The Effect of Ambient Environmental Conditions on COVID-19 Mortality: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
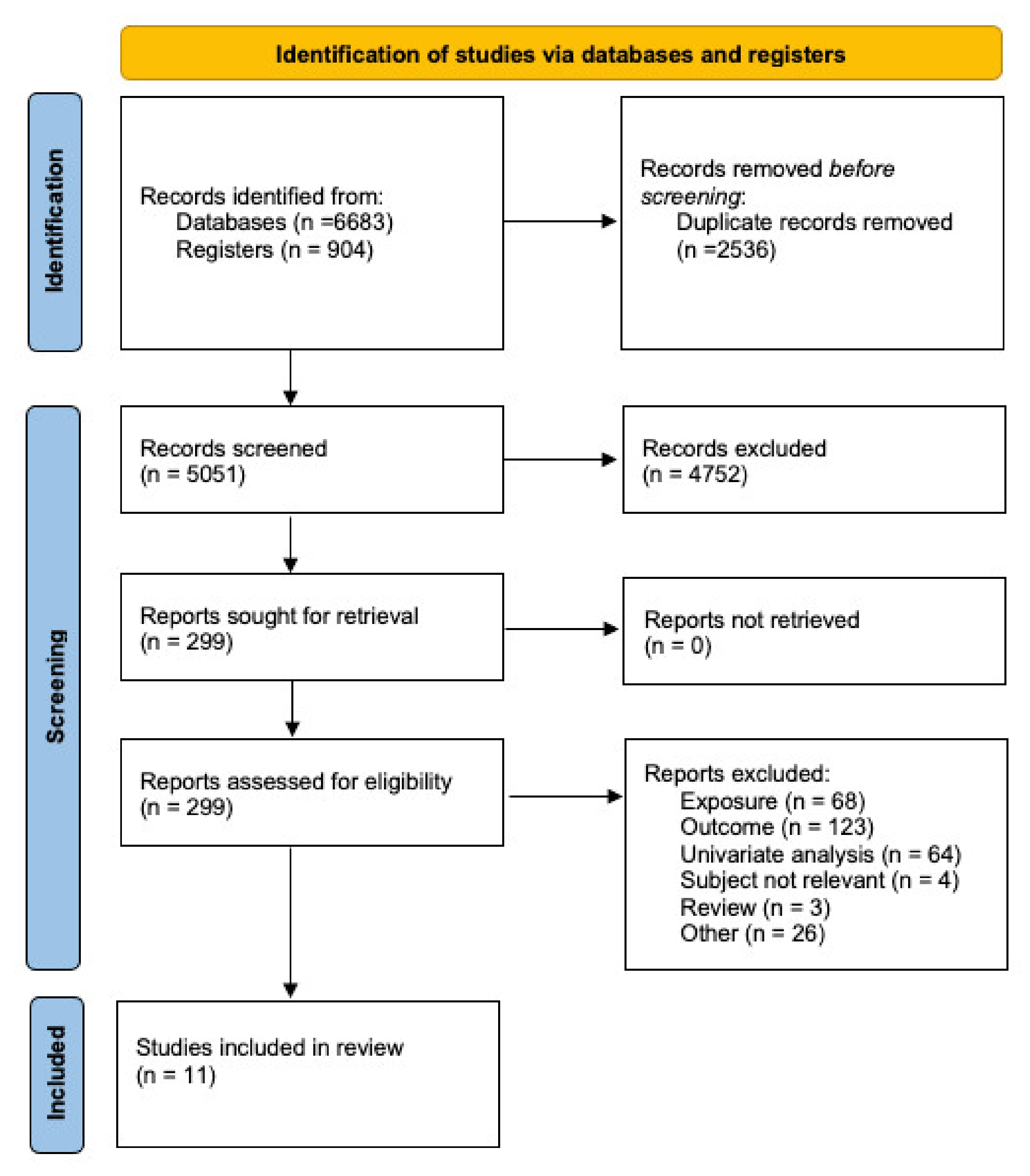
2.2. Selection Process
2.3. Data Collection Process
2.4. Risk of Bias Evaluation
2.4.1. Recruitment Procedure
2.4.2. Exposure Assessment
2.4.3. Outcome Source and Validations
2.4.4. Confounding
2.4.5. Analysis Methods
2.4.6. Chronology
2.4.7. Funding
2.4.8. Conflict of Interest
2.4.9. Overall Risk of Bias
2.5. Data Synthesis
3. Results
3.1. Overview of the Studies
3.2. Quality of the Studies
3.3. Effect of Temperature on Mortality
3.4. Effect of Relative Humidity and Precipitation on Mortality
3.5. Effect of Wind on Mortality
3.6. Quantitative Analysis
4. Discussion
4.1. Summary of Results
4.2. Strengths and Limitations of Our Review
4.3. Risk of Bias of Included Studies and Recommendations for Future Work
4.4. Public Policy Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Coronavirus Disease (COVID-19). Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 5 August 2020).
- Ji, Y.; Qian, H.; Ye, J.; Zheng, X. The impact of ambient humidity on the evaporation and dispersion of exhaled breathing droplets: A numerical investigation. J. Aerosol Sci. 2018, 115, 164–172. [Google Scholar] [CrossRef]
- Haslbeck, K.; Schwarz, K.; Hohlfeld, J.; Seume, J.R.; Koch, W. Submicron droplet formation in the human lung. J. Aerosol. Sci. 2010, 41, 429–438. [Google Scholar] [CrossRef]
- Asbach, C.; Held, A.; Kiendler-Scharr, A.; Scheuch, G.; Schmid, H.-J.; Schmitt, S.; Schumacher, S.; Wehner, B.; Weingartner, E.; Weinzierl, B. Position paper of the Gesellschaft für Aerosolforschung on understanding the role of aerosol particles in SARS-CoV-2 infection. Ges. Für Aerosolfoschung 2020, 17. [Google Scholar] [CrossRef]
- Chan, K.H.; Peiris, J.S.M.; Lam, S.Y.; Poon, L.L.M.; Yuen, K.Y.; Seto, W.H. The Effects of Temperature and Relative Humidity on the Viability of the SARS Coronavirus. Adv. Virol. 2011, 2011, 734690. [Google Scholar] [CrossRef]
- Moriyama, M.; Hugentobler, W.J.; Iwasaki, A. Seasonality of Respiratory Viral Infections. Annu. Rev. Virol. 2020, 7, 83–101. [Google Scholar] [CrossRef]
- Ianevski, A.; Zusinaite, E.; Shtaida, N.; Kallio-Kokko, H.; Valkonen, M.; Kantele, A.; Telling, K.; Lutsar, I.; Letjuka, P.; Metelitsa, N.; et al. Low Temperature and Low UV Indexes Correlated with Peaks of Influenza Virus Activity in Northern Europe during 2010–2018. Viruses 2019, 11, 207. [Google Scholar] [CrossRef] [Green Version]
- Tamerius, J.D.; Shaman, J.; Alonso, W.J.; Bloom-Feshbach, K.; Uejio, C.K.; Comrie, A.; Viboud, C. Environmental Predictors of Seasonal Influenza Epidemics across Temperate and Tropical Climates. PLoS Pathog. 2013, 9, e1003194. [Google Scholar] [CrossRef]
- Yuan, J.; Yun, H.; Lan, W.; Wang, W.; Sullivan, S.; Jia, S.; Bittles, A.H. A climatologic investigation of the SARS-CoV outbreak in Beijing, China. Am. J. Infect. Control 2006, 34, 234–236. [Google Scholar] [CrossRef]
- Tan, J.; Mu, L.; Huang, J.; Yu, S.; Chen, B.; Yin, J. An initial investigation of the association between the SARS outbreak and weather: With the view of the environmental temperature and its variation. J. Epidemiol. Commun. Health 2005, 59, 186–192. [Google Scholar] [CrossRef] [Green Version]
- Byun, W.S.; Heo, S.W.; Jo, G.; Kim, J.W.; Kim, S.; Lee, S.; Park, H.E.; Baek, J.-H. Is coronavirus disease (COVID-19) seasonal? A critical analysis of empirical and epidemiological studies at global and local scales. Environ. Res. 2021, 196, 110972. [Google Scholar] [CrossRef]
- Paraskevis, D.; Kostaki, E.G.; Alygizakis; Thomaidis, N.S.; Cartalis, C.; Tsiodras, S.; Dimopoulos, M.A. A review of the impact of weather and climate variables to COVID-19: In the absence of public health measures high temperatures cannot probably mitigate outbreaks. Sci. Total Environ. 2021, 768, 144578. [Google Scholar] [CrossRef]
- McClymont, H.; Hu, W. Weather Variability and COVID-19 Transmission: A Review of Recent Research. Int. J. Environ. Res. Public Health 2021, 18, 396. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Ijaz, S.I.; Verbeek, J.; Seidler, A.; Lindbohm, M.-L.; Ojajärvi, A.; Orsini, N.; Costa, G.; Neuvonen, K. Night-shift work and breast cancer—A systematic review and meta-analysis. Scand. J. Work. Environ. Health 2013, 39, 431–447. [Google Scholar] [CrossRef]
- Petereit-Haack, G.; Bolm-Audorff, U.; Starke, K.R.; Seidler, A. Occupational Risk for Post-Traumatic Stress Disorder and Trauma-Related Depression: A Systematic Review with Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 9369. [Google Scholar] [CrossRef]
- Starke, K.R.; Petereit-Haack, G.; Schubert, M.; Kämpf, D.; Schliebner, A.; Hegewald, J.; Seidler, A. The Age-Related Risk of Severe Outcomes Due to COVID-19 Infection: A Rapid Review, Meta-Analysis, and Meta-Regression. Int. J. Environ. Res. Public Health 2020, 17, 5974. [Google Scholar] [CrossRef]
- Starke, K.R.; Kofahl, M.; Freiberg, A.; Schubert, M.; Groß, M.L.; Schmauder, S.; Hegewald, J.; Kämpf, D.; Stranzinger, J.; Nienhaus, A.; et al. Are Daycare Workers at a Higher Risk of Parvovirus B19 Infection? A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 1392. [Google Scholar] [CrossRef] [Green Version]
- Starke, K.R.; Kofahl, M.; Freiberg, A.; Schubert, M.; Groß, M.L.; Schmauder, S.; Hegewald, J.; Kämpf, D.; Stranzinger, J.; Nienhaus, A.; et al. The risk of cytomegalovirus infection in daycare workers: A systematic review and meta-analysis. Int. Arch. Occup. Environ. Health 2019, 93, 11–28. [Google Scholar] [CrossRef]
- Khalili, M.; Karamouzian, M.; Nasiri, N.; Javadi, S.; Mirzazadeh, A.; Sharifi, H. Epidemiological Characteristics of COVID-19; A Systemic Review and Meta-Analysis. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Ma, Y.; Zhao, Y.; Liu, J.; He, X.; Wang, B.; Fu, S.; Yan, J.; Niu, J.; Zhou, J.; Luo, B. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci. Total Environ. 2020, 724, 138226. [Google Scholar] [CrossRef]
- Sobral, M.F.F.; Duarte, G.B.; Sobral, A.I.G.D.P.; Marinho, M.L.M.; Melo, A. Association between climate variables and global transmission of SARS-CoV-2. Sci. Total Environ. 2020, 729, 138997. [Google Scholar] [CrossRef]
- Dai Su, Y.C.; He, K.; Zhang, T.; Tan, M.; Zhang, Y.; Zhang, X. Influence of socio-ecological factors on COVID-19 risk: A cross-sectional study based on 178 countries/regions worldwide. medRxiv 2020. [Google Scholar] [CrossRef]
- Wu, Y.; Jing, W.; Liu, J.; Ma, Q.; Yuan, J.; Wang, Y.; Du, M.; Liu, M. Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries. Sci. Total Environ. 2020, 729, 139051. [Google Scholar] [CrossRef]
- Rehman, Y.; Rehman, N. Association of climatic factors with COVID-19 in Pakistan. AIMS Public Health 2020, 7, 854–868. [Google Scholar] [CrossRef] [PubMed]
- Guo, C.; Bo, Y.; Lin, C.; Li, H.B.; Zeng, Y.; Zhang, Y.; Hossain, S.; Chan, J.W.; Yeung, D.W.; Kwok, K.-O.; et al. Meteorological factors and COVID-19 incidence in 190 countries: An observational study. Sci. Total Environ. 2021, 757, 143783. [Google Scholar] [CrossRef]
- Islam, A.R.; Hasanuzzaman, M.; Shammi, M.; Salam, R.; Bodrud-Doza, M.; Rahman, M.M.; Mannan, M.A.; Huq, S. Are meteorological factors enhancing COVID-19 transmission in Bangladesh? Novel findings from a compound Poisson generalized linear modeling approach. Environ. Sci. Pollut. Res. Int. 2020, 28, 11245–11258. [Google Scholar] [CrossRef]
- Jiang, Y.; Xu, J. The association between COVID-19 deaths and short-term ambient air pollution/meteorological condition exposure: A retrospective study from Wuhan, China. Air Qual. Atmosphere Health 2021, 14, 1–5. [Google Scholar] [CrossRef]
- Sun, Y.; Hu, X.; Xie, J. Spatial inequalities of COVID-19 mortality rate in relation to socioeconomic and environmental factors across England. Sci. Total Environ. 2021, 758, 143595. [Google Scholar] [CrossRef]
- Tzampoglou, P.; Loukidis, D. Investigation of the Importance of Climatic Factors in COVID-19 Worldwide Intensity. Int. J. Environ. Res. Public Health 2020, 17, 7730. [Google Scholar] [CrossRef]
- Fernández, D.; Giné-Vázquez, I.; Liu, I.; Yucel, R.; Ruscone, M.N.; Morena, M.; García, V.G.; Haro, J.M.; Pan, W.; Tyrovolas, S. Are environmental pollution and biodiversity levels associated to the spread and mortality of COVID-19? A four-month global analysis. Environ. Pollut. 2021, 271, 116326. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Son, W.; Ryu, Y.; Choi, S.B.; Kwon, O.; Ahn, I. Effects of temperature, humidity, and diurnal temperature range on influenza incidence in a temperate region. Influ. Other Respir. Viruses 2020, 14, 11–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Y.; Feng, C.; Ma, C.; Yang, P.; Tang, S.; Lau, A.; Sun, W.; Wang, Q. The impact of temperature and humidity measures on influenza A (H7N9) outbreaks—evidence from China. Int. J. Infect. Dis. 2015, 30, 122–124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dai, Q.; Ma, W.; Huang, H.; Xu, K.; Qi, X.; Yu, H.; Deng, F.; Bao, C.; Huo, X. The effect of ambient temperature on the activity of influenza and influenza like illness in Jiangsu Province, China. Sci. Total Environ. 2018, 645, 684–691. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| Population | General human populations (both sexes, all ages) | All others |
| Exposure(s) | Temperature, humidity *, wind | All other exposures |
| Comparator/control | Not applicable | Not applicable |
| Outcomes | Mortality due to COVID-19 or excess mortality compared to a previous time frame | Other outcomes |
| Study design ** | Ecological studies, case series, cross-sectional, case-control, and cohort studies | RCTs, qualitative studies, ecological studies, case reports, experiments |
| Author, Year Reference | Study Design | Study Area and Climatic Zone | Time Period of Study | Exposures and Source of Data | Outcome Definition and Source of Data | Confounders/Covariates | Analysis, Lags, and Results |
|---|---|---|---|---|---|---|---|
| Ma, 2020 [22] | Ecological study | Study area: Wuhan, China Climatic zone: Humid subtropical climate | 20 January–29 February 2020 | Exposures: Daily average temperature, diurnal temperature range (DTR), and relative humidity Source of data: Shanghai Meteorological Bureau and Data Center of Ministry of Ecology and Environment of the People’s Republic of China | Outcome; COVID-19 deaths Source of data: Official website of Health Commission of Hubei Province | Air pollutants, date of the week, time trends | Analysis: Generalized additive model (GAM) to analyze associations, with a quasi-Poisson link function. Used smoothed spline functions of times to accommodate nonlinear and nonmonotonic patterns between mortality and time. Lag: Examined single day lag and multiple-day average lag effects (0–5 lag) of weather conditions Results: % change of COVID-19 mortality (based on Figures 2 and 3 of the text in Ma et al. 2020 [22])—no quantitative figures could be obtained. |
| Sobral, 2020 [23] | Ecological study | Study area: World (249 countries) | 1 December 2019–30 March 2020 | Exposures: Average temperature, maximum temperature, minimum temperature, and precipitation Source of data: National Oceanic and Atmospheric Administration (NOAA) database | Outcome: Daily death rates Source of data: World Health Organization reports | Population density, dummy month (specific month effects), country’s time of exposure to the epidemic (temporal distance, in days, between the first case registered in the territory and the time of study) | Analysis: Multivariate linear regression Lag: No lag effect included Results: Model 1 (average temperature only): ß = 0.053 (p < 0.01) Model 2 (average temperature, maximum temperature, minimum temperature, precipitation, exposure time): Death: Average temperature: ß = −0.10 Maximum temperature: ß = 0.01 Minimum temperature: ß = 0.01 Precipitation: ß = 0.34 Model 3 (average temperature, maximum temperature, minimum temperature, precipitation, exposure time, population density, dummy month): Death: Average temperature: ß = −0.10 Maximum temperature: ß = 0.02 Minimum temperature: ß = 0.001 |
| Su, 2020 [24] | Ecological study | Study area: 178 countries/regions (excluding countries/region without COVID-19 cases and some unmatched countries/region (i.e., Taiwan)) | 22 January–6 April 2020 | Exposures: Mean temperature, relative humidity, and precipitation Source of data: Global Surface Summary of the 183 Day (GSOD) via The Integrated Surface Hourly (ISH) dataset (includes global data obtained from the USAF Climatology Center | Outcome: Cumulative mortality rate (CMR) Source of data: John Hopkins University dashboard from Center for Systems Science and Engineering | World Development Indicators dataset (World Bank), urban development (% urban population, population growth, population density), GDP per capita, health, infrastructure (railways, passengers carried), poverty (poverty headcount ratio), science and technology (researchers in R&D) , social protection and labor (cover of social insurance programs, unemployment), mean wind speed | Analysis: Negative binomial regression Lag: No consideration of time (no lag) Results: Cumulative mortality rate Mean temperature (°C): IRR = 0.975 (95% CI 0.887–1.071) Relative humidity (%): IRR = 1.025 (95% CI 0.995–1.056) Mean wind speed (.1 knots): IRR = 1.155 (95% CI 0.951–1.403) Precipitation (0.01 inches) IRR = 0.019 (95% CI 0.001–0.377) |
| Wu, 2020 [25] | Ecological study | Study area: Worldwide (166 countries excluding China) | December–27 March 2020 | Exposures: Temperature and relative humidity Source of data: National Oceanic and Atmospheric Administration Center | Outcome: Daily new deaths Source of data: WHO daily situation reports | Wind speed, median age of national population, Global Health Security Index, Human Development Index, population density, controlling for countries, date of the week and date of the observation to control time trend and cycle | Analysis: Log-linear generalized additive model (GAM) Lag: Single lag days (lag 0, 1, 2, 3). Cumulative effects of average exposure over multiple days assessed using additional analyses (lag 01, 02, 03) Results: Changes in daily new deaths (% change) associated with each 1-unit increase: Temperature (°C): ß = −0.65% (95% CI −1.40% to 0.099%) Relative humidity (%) ß = −0.46% (95% CI −0.63% to −0.29%) Sensitivity analyses: Over 10 days since the first reported case: Temperature (°C): ß = −1.22% (95% CI −2.00% to −0.45%) Relative humidity (%) ß = −0.51% (95% CI -0.68% to −0.34%) Over 100 cumulative cases: Temperature (°C): ß = −1.25% (95% CI −2.16% to −0.34%) Relative humidity (%) ß = −0.53% (95% CI −0.73% to −0.33%) |
| Rehman, 2020 [26] | Ecological study | Study area: Provinces of Pakistan Climatic zone: Lies in temperate zone with wide variations depending on location | 10 March–10 July 2020 | Exposures: Daily mean humidity and wind, daily and minimum temperature Source of data: Pakistan Meteorological Department (http://www.pmd.gov.pk/en/), https://www.timeanddate.com/weather/pakistan, https://www.accuweather.com, | Outcome: COVID-19 deaths Source of data: Government of Pakistan http://covid.gov.pk/stats/pakistan and Worldometer Coronavirus cases https://www.worldometers.info/coronavirus/country/pakistan/ | Sun status | Analysis: Negative binomial log linear mixed model Lag: No lag Results: Due to lack of space, results summarized in Table S3 |
| Guo, 2020 [27] | Ecological study | 415 sites comprising 235 cities from 10 countries and 180 countries | 23 January–13 April 2020 | Hourly meteorological data (temperature, relative humidity, wind speed) aggregated as daily average meteorological data. Ground-based monitoring network of the World Meteorological Organization global telecommunications system | COVID-19 mortality Johns Hopkins University Center for Systems Science and Engineering (JHU VSSE) The Wind Financial databases (WFD) for detailed information on COVID-19 at city/stae level in Australia, Canada, USA, China, Germany, Italy, Japan, Korea, Norway, and Spain | Date of first reported cases, population density, median age, Global Health Security Index (GHSI), latitude, longitude, intervention policies implemented | Analysis: Negative binomial log linear mixed model Results: Lag 0–14 days Temperature (Reference = 11 °C) 5 °C: RR 1.35 (95% CI: 1.21, 1.51) 22oC: RR = 0.51 (95%CI: 0.39, 0.67) Relative humidity (Reference = 71%) 59%: RR = 0.98 (95% CI: 0.92–1.05) 79%: RR = 0.86 (95% CI: 0.80–0.92) Wind speed (Reference = 3 m/s) 2 m/s: RR = 1.31 (95% CI: 1.16, 1.48) 4 m/s: RR = 0.76 (95% CI: 0.70, 0.82) Lag 14 days Temperature (Reference = 11 °C) 5 °C: RR 1.02 (95% CI: 0.99, 1.06) 22oC: RR = 0.92 (95%CI: 0.84, 1.01) Relative humidity (Reference = 71%) 59%: RR = 1.00 (95% CI: 0.98–1.02) 79%: RR = 1.00 (95% CI: 0.98–1.02) Wind speed (Reference = 3 m/s) 2 m/s: RR = 1.03 (95% CI: 1.00, 1.05) 4 m/s: RR = 0.98 (95% CI: 0.96, 0.99) |
| Islam, 2020 [28] | Ecological study | Study area: Bangladesh Climatic zone: Humid monsoon sub-tropical climate | 8 March–30 April 2020 | Exposures: Night relative humidity (NRH), rainfall, diurnal temperature (TDN), mean temperature (MT), mean relative humidity (MRH), and absolute humidity (AH) Source of data: Bangladesh Meteorological Department (BMD) weather stations | Outcome: COVID-19 death cases Source of data: Bangladeshi government site | None besides the weather parameters shown in results (NRH, TDN, MT, MRH, AH) | Analysis: Compound Poisson generalized linear model, along with a Monte-Carlo method and random forest model Lag: Single and multiple day lags Results: no effect numbers (Figures 5 and 6 in the text in Islam et al. 2020 [28] show a depiction) |
| Jiang and Xu, 2021 [29] | Ecological study | Study area: Wuhan, China Climatic zone: Humid sub-tropical climate | 25 Jan–7 April 2020 | Exposure: Daily temperature, relative humidity, and diurnal temperature range Source of data: Weather Channel (www.weather.com) | Outcome: COVID-19 deaths Source of data: Health Commission of Hubei China | No further confounders in the analysis model and no government interventions were included because the whole study period was under strict lockdown | Analysis: Poisson generalized linear model Lag: 18 days Results: Daily temperature ß = −0.149 RR = 0.861 (95% CI: 0.851, 0.872) Relative humidity ß = −0.005 RR = 0.995 (95% CI: 0.989, 1) Diurnal temperature range ß = 0.014 RR = 1.014 (95% CI: 1.003, 1.025) |
| Sun 2020 [30] | Ecological study | Study area: 317 local authority districts (LADs) in England Climatic zone: Temperate climate | March–May 2020 | Exposure: 3-month mean monthly relative humidity and monthly air temperature (from 2019) Source of data: Met Office HadUK-Grid, Gridded Climate Observations on a 1 km Grid over the UK | Outcome: Aggregated three-month England-wide COVID-19 mortality rate. Spatial patterns of COVID-19 mortality compared with non-COVID-19 mortality Source of data: Office for National Statistics | First model: sex, ethnicity (percent Asians, percent blacks), percent of households in poverty, unemployment rate, population density, hospital density annual mean PM2.5 | Analysis: Variable selection: Lasso technique, spatial autoregressive model (MESS-SAR), Eigenvector spatial filtering model (RES-ESF) Lag: No consideration of time (no lag) Results: First model: OLS Model: Humidity: ß = −8.521 (p < 0.001) Air temperature: ß = −0.795 MESS-SAR model: Humidity: ß = −3.715 (p < 0.01) Air temperature: ß = 1.512 RE-ESF model: Humidity: ß = −4.793 (p < 0.001) Air temperature: ß = 3.852 |
| Tzampoglou and Dimitrios, 2020 [31] | Ecological study | Study area: Worldwide 101 countries (countries with Human Development Index (HDI) < 0.7 excluded from analysis) | March–3 May 2020 | Exposures: Monthly average atmospheric temperature (°C), monthly average relative humidity (%), and cumulative precipitation (mm) Source of data: Collected from the Copernicus Program database, estimated from climate reanalysis ERA-Interim and ERA5 Spatial analysis tool of the ArcGIS software was employed to derive the spatial average of variables across the entire territory of each country. After spatial averaging, temporal average values were computed for the March 2020 to May 2020 period. | Outcome: Total deaths per million due to COVID-19 Source of data: European Commission (EC), OurWorldInData.org, and COVID-19 Government Response Tracker, Blavatnik School of Government | Cloud cover (CC), population density (PD), median age (MA), stringency index (SI), delay in first case (FC) and stay at-home order measures (SH) | Analysis: Linear model, variable selection: Lasso and forward stepwise Lag: No lag (no consideration of time) Results: Only two models shown, other models in Table S3 Model A Temperature: ß = −108.9 (95% CI: −307.2, 89.4) Relative humidity: ß = 82.2 (95% CI −125.1, 289.5) Precipitation: ß = 13.4 (95% CI −258.8, 285.6) confounders: CC, PD, MA, SI, FC, SH Model B Temperature: ß = −88.9 (95% CI −259.2, 81.5) Relative humidity: ß = 79.1 (95% CI −126.5, 284.8) Precipitation: ß = −17.9 (95% CI −239.6. 203.8) Confounders: PD, MA, SI, FC, SH |
| Fernández 2021 [32] | Ecological study | Study area: Worldwide 218 countries | 21 January–18 May 2020 | Exposures: Maximum, miniumum, and average daily temperature and precipitation Source of data: Downloaded from NASA’s Goddard Earth Sciences Data and Information Services Center (GES DISC). Integrated Multi-satellite Retrievals for Global Precipitation Measurement (IMERG), MERRA-2 (a Modern-Era Retrospective analysis for Research and Applications version 2) | Outcome: Daily confirmed deaths and the total amount of confirmed deaths Source of data: Population-level information (per country), reported by WHO | National Biodiversity Index (NBI), population density, days since last case, days since first case reported in country, country income level, government intervention level | Analysis: Generalized linear mixed models Lag: 14 days Results: Results of Bayesian spatio-temporal regression analysis: All countries Precipitation: ß = 0.000 (95% CI: −0.002, 0.001) Maximum temperature: ß = −0.003 (95% CI: −0.010, 0.005) |
| Study ID | Major Domains | Minor Domains | OVERALL | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Recruitment Procedure | Exposure Assessment | Outcome Source and Validation | Confounding | Analysis Method | Chronology | Funding | Conflict of Interest | ||
| Ma et al. 2020 [22] |  |  |  |  |  |  |  |  |  |
| Sobral et al. 2020 [23] |  |  |  |  |  |  |  |  |  |
| Su et al. 2020 ** [24] |  |  |  |  |  |  |  |  |  |
| Wu et al. 2020 [25] |  |  |  |  |  |  |  |  |  |
| Rehman et al. 2020 [26] |  |  |  |  |  |  |  |  |  |
| Guo et al. 2020 [27] |  |  |  |  |  |  |  |  |  |
| Islam et al. 2020 [28] |  |  |  |  |  |  |  |  |  |
| Jiang and Xu et al. 2021 [29] |  |  |  |  |  |  |  |  |  |
| Sun et al. 2020 ** [30] |  |  |  |  |  |  |  |  |  |
| Tzampoglou and Dimitrios et al. 2020 [31] |  |  |  |  |  |  |  |  |  |
| Fernandez et al. 2020 [32] |  |  |  |  |  |  |  |  |  |
 : low risk;
: low risk;  : unclear risk;
: unclear risk;  : high risk.
: high risk.Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romero Starke, K.; Mauer, R.; Karskens, E.; Pretzsch, A.; Reissig, D.; Nienhaus, A.; Seidler, A.L.; Seidler, A. The Effect of Ambient Environmental Conditions on COVID-19 Mortality: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 6665. https://doi.org/10.3390/ijerph18126665
Romero Starke K, Mauer R, Karskens E, Pretzsch A, Reissig D, Nienhaus A, Seidler AL, Seidler A. The Effect of Ambient Environmental Conditions on COVID-19 Mortality: A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(12):6665. https://doi.org/10.3390/ijerph18126665
Chicago/Turabian StyleRomero Starke, Karla, René Mauer, Ethel Karskens, Anna Pretzsch, David Reissig, Albert Nienhaus, Anna Lene Seidler, and Andreas Seidler. 2021. "The Effect of Ambient Environmental Conditions on COVID-19 Mortality: A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 12: 6665. https://doi.org/10.3390/ijerph18126665
APA StyleRomero Starke, K., Mauer, R., Karskens, E., Pretzsch, A., Reissig, D., Nienhaus, A., Seidler, A. L., & Seidler, A. (2021). The Effect of Ambient Environmental Conditions on COVID-19 Mortality: A Systematic Review. International Journal of Environmental Research and Public Health, 18(12), 6665. https://doi.org/10.3390/ijerph18126665








