1. Introduction
Since the early 2000s, emerging developments in online technology have offered increasing opportunities to support remotely delivered healthcare [
1,
2,
3]. Telehealth refers to all health services provided remotely and tele-rehabilitation, more specifically, refers to the use of information and communication technologies (ICT) to provide rehabilitation services to people remotely in their homes or other environments [
4,
5]. The goal of tele-rehabilitation is to improve client access to care by receiving therapy beyond the physical walls of a traditional healthcare facility, thus expanding the continuity of rehabilitation care [
6,
7,
8,
9]. The technology used by rehabilitation professionals is diverse, ranging from simple day-to-day applications such as phone calls, emails, photos or videos, to more sophisticated technologies such as secured video conferencing, sensor-based monitoring, and virtual gaming. These can be used to increase the accessibility and the cost-effectiveness of rehabilitation [
10,
11].
As demonstrated by numerous systematic reviews and meta-analyses that examined more than 250 studies of tele-rehabilitation published in the past 20 years, the majority have focused on adult populations with diverse diagnoses (e.g., stroke, multiple sclerosis (MS), diabetes, heart failure, chronic obstructive pulmonary disease, cancer) [
10,
12,
13,
14]. The studies did not report any negative effects of tele-rehabilitation on the participants or statistically significant differences between conventional care to telehealth. In McFarland’s et al. [
14] systematic review and meta-analysis, additional qualitative data were provided. Participants reported peace of mind, reassurance, patient ownership and an overall feeling of better access to health care.
Prior to the COVID-19 pandemic, the use of this approach for pediatric rehabilitation had been reported with far less frequency. Camden et al.’s [
3] systematic review summarized the results of 23 studies of children from birth to the age of 12 years including diagnoses such as autism, cerebral palsy (CP), acquired brain injury (ABI) and other developmental disabilities and the effectiveness of tele-rehabilitation. The majority of studies (18/23) were carried out since 2015 and most focused more on behavioral issues than on physical or functional goals. None of the studies reported in this systematic review documented any advantage of in-person sessions over tele-rehabilitation, concluding that, in many cases, tele-rehabilitation appears to be as beneficial as in-person therapy. Indeed, in applications of coaching and behavioral therapy, tele-rehabilitation appeared to be more effective than physical therapy via tele-rehabilitation.
Yet, the use of tele-rehabilitation was not widespread in the great majority of clinical settings until the necessity arose of providing therapy via remote means due to the COVID-19 pandemic. Previously, concerns regarding data security as well as disruption of the patient-clinician relationship led some rehabilitation professionals to resist adoption of these tools [
15]. Moreover, many therapists were reluctant to embrace what they perceived to be the burden of coping with online technologies [
15,
16]. Remote rehabilitation had mainly been used as a means to provide services to those living in the periphery who have less access to services [
17]. A systematic review of 44 studies of allied health care professionals providing remote services in Australia between the years 2004–2015 found that the majority concentrated on speech pathology (64%). Thirty-three studies reported on trials and interventions with the remainder focusing on the client’s perception of the service. None of the studies reported a deterioration or negative results, but the authors did report that, in general, there was no noticeable increase in the use of remote therapy and that the therapists remained hopeful that upcoming improvements in technology will improve the use of such services.
Gladwell’s “tipping point” [
18] was achieved with the onset of the COVID-19 pandemic crisis where the need to expand the delivery of online pediatric rehabilitation services became of paramount importance. Conventional healthcare services were unable to adequately cope with therapeutic interventions such as medication monitoring and dietary supervision, nor to provide cognitive and motor therapy as well as psychological support [
4]. Children with disabilities who did not have acute, life-threatening medical needs were recommended to avoid hospital visits and in-person contact with clinicians; the ability to access therapy remotely became the option of choice, indeed the only available alternative [
19].
The approach of the Mayo Clinic team [
20] illustrates this response. To prepare children, families and therapists for tele-rehabilitation consultations necessitated by the COVID-19 pandemic social distancing requirements, they developed checklists and guidelines that were specific for medical diagnoses and types of intervention. The checklists included the items that therapists and patients needed to prepare prior to therapy in the home setting such as tools or equipment and any technological requirements for a successful online visit. A wide range of concerns related to how to execute specific assessments and provide treatment in a home setting, the type of equipment needed to record clinical outcomes, and how to build rapport from a distance. They concluded that remote interactions were generally suitable for pediatric rehabilitation services and that the pandemic crisis should be used to “try out” best practices for the future. Tanner [
21,
22] reported on tele-rehabilitation services provided to children in general and oncology departments; within two weeks of the COVID-19 pandemic outbreak, protocols were developed, and within the first month, more than 1000 tele-rehabilitation sessions were provided.
In summary, the potential of online technologies for pediatric rehabilitation has been demonstrated in a range of clinical interventions with children and their families. They appear to encourage greater physical activity, promote a healthier lifestyle, help manage chronic conditions and, indeed, to be viable alternatives to traditional one-on-one interventions [
3,
23,
24]. Nevertheless, despite initial promising research results, the adoption of these technologies has been limited, and even waned after the first wave of excitement [
25]. Additional evidence is required to identify “best practices” for maintaining viable clinician–patient interactions that promote activity and participation, while supporting families in their efforts to manage their children’s health condition and psychological well-being.
In light of the COVID-19 pandemic, ALYN Pediatric Rehabilitation Hospital responded immediately by providing a broad range of rehabilitation services to young people via online therapy. Until that point ALYN provided tele-rehabilitation services only within the framework of pilot studies and research [
24]. Widespread reservations among therapists, reimbursement difficulties and lack of Health Insurance Portability and Accountability Act (HIPAA) [
26]-accredited infrastructure prevented the inclusion of tele-rehabilitation into the regular program offered by the hospital. However, once COVID-related health regulations forced abrupt cessation of on-site ambulatory services and brought treatment protocols to a halt, every single one of these barriers was quickly overcome. Similar to other countries, the Israel Ministry of Health (IMOH) issued the needed provisions, recognizing tele-rehabilitation therapy as equivalent to in-person sessions reimbursement-wise. This paved the way to a combination of on-site and off-site patients and therapists. For example, in-patients could be treated remotely by therapists who were either quarantined themselves or in lock-down, and ambulatory multidisciplinary clinics could be held as long as enough data could be obtained without physical examination.
Within one week of the IMOH’s regulations mandating an enforcement of social distancing, ALYN responded by implementing medical and allied health online support including speech and language, physical and occupational therapy, psychology treatments and more. In keeping with the well-known adage “Necessity is the mother of invention”, our goal was to implement the use of a HIPAA accredited online platform (Zoom) that is widely available, user-friendly and that supports the implementation of realistic therapy protocols via real-time interactions between one or more patients and therapists.
For young people in the critical period of rehabilitation, such as those recovering from brain injury or following orthopedic and neurosurgical interventions, Zoom-based online therapy was adopted without delay by ALYN, provided that the young people’s parents or guardians consented in writing to this method. At the same time, the hospital administrators, clinicians and research personnel made a key decision to fully document the process in order to determine its feasibility, effectiveness and acceptance by the various stakeholders. Thus, although the adoption of online therapy was an ad hoc response to a crisis, documentation of the experience was expected to support future decision- making regarding the advantages and limitations of its continued use after COVID-19. We expected online therapy monitoring would provide information as to which patients and treatment goals are most amenable to remote interaction, and that we could use the data to develop patient selection criteria. An additional goal included identification of appropriate treatment goals that take into account the flexibility needed in treatment approaches since, in some cases, online tasks differ greatly from those suitable for conventional in-person therapy. Thus, the objectives of this naturalistic study were: (1) to monitor usage of and attitudes toward online rehabilitation provided to young people receiving out-patient sessions of physical, occupational, speech and language therapy and psychology and (2) to determine whether this model of online treatment should be retained in full or in part post-COVID-19.
4. Discussion
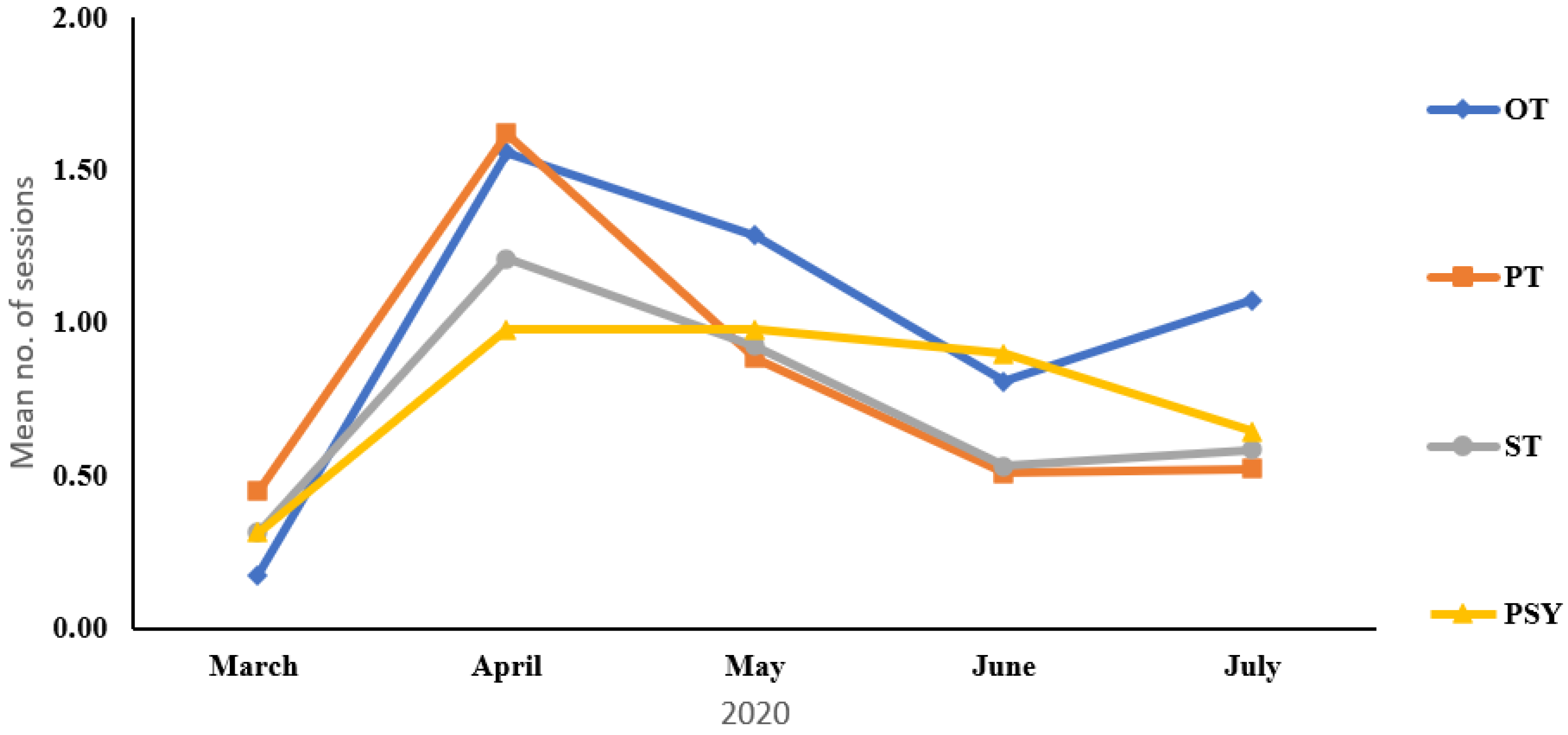
The demographic and statistical results highlighted differences over time that varied significantly across therapeutic disciplines: following the sudden significant surge between March 2020 to April 2020 of all therapies, the disciplines responded differently. PT and ST similarly showed an initial increase and then decline in the use of online therapy. The characteristics of therapy, with the desire for more intensive handling (the PTs were eager to position and support the child and stimulate balance reactions; the STs felt the need to provide hands-on oral-motor stimulation) led to the return of patients as soon as possible. Online therapy sessions in psychology remained high until June 2020, due to the primary reliance on verbal interactions with less need of physical contact. Indeed, the psychologists reported that online therapy was, in many cases, more beneficial by facilitating flexibility which led to increased parental involvement in the process. Occupational therapy was the only discipline that decreased between April to June 2020 and then increased during July 2020. This is attributed to the reluctance of parents to send children back to the hospital school; the majority of children in the school are respiratory dependent and need mainly OT and PSY (not PT).
The ensuing discussion will relate to two main topics that emerged from the literature review and study results from global, national and local perspectives: (1) the use of telehealth and tele-rehabilitation before and during the COVID-19 pandemic and 2) “lessons learned” to work towards implementation of “best practices” of tele-rehabilitation. This topic will be examined with reference to a framework for implementing telehealth in pediatrics, known by the acronym VIRTUAL (for Viewing, Information, Relationships, Technology, Unique, Accessible, Legal), proposed by Camden and Silva [
11] following a May 2020 e-Summit.
Prior to the COVID-19 pandemic, telehealth was not widely used in pediatric rehabilitation settings despite numerous studies supporting its use as a feasible alternative to conventional in-person healthcare [
3,
31,
32]. A World Health Organization (WHO) report “Global diffusion of eHealth” from 2016 [
33] documented the use of telehealth services in different countries based on a survey sent to their member states. One hundred and twenty-two countries (out of 194) responded, with only 22% of the countries reporting the use of telehealth services. In a similar report, Camden and Silva [
11] surveyed 76 countries in 2019 and found that only 4% used telehealth prior to COVID-19. It appears that technical, logistical and training challenges deterred therapists from using tele-rehabilitation. However, in May 2020, just three months since the global awareness of COVID-19, the same polled countries reported an increase of 70% [
11].
In the United States, extensive use of telehealth was hindered by restrictions related to state-to-state reciprocity in professional licensing and medical insurance coverage [
34]. In 2010 only 12 states allowed insurance coverage for these services compared to 2017 where 33 states and the District of Columbia passed laws to enable adoption of telehealth services [
35]. The American Academy of Pediatrics recognized that each state and specialty addressed telehealth differently and in 2015 initiated Supporting Pediatric Research on Outcomes and Utilization of Telehealth (SPROUT), a multi-centered research network devoted to establishing evidence for pediatric telehealth. Their first report mapped out telehealth services based on survey responses from 52 programs in 30 states [
35]. Considerably more telehealth programs were available in neurology, psychiatry and cardiology (23–25/52) compared to rehabilitation (3/52). The most substantial barrier to growing pediatric telehealth and tele-rehabilitation among the 52 surveyed programs was reimbursement (30/52).
Similar to global trends, Israel also changed its use of telehealth services. A study carried out by a pediatric rehabilitation hospital in Israel [
23] demonstrated how the number of tele-rehabilitation sessions increased to 110 over a five-week period in late March to the end of April 2020. They reported that although both children (mean age = 11 years) and therapists were able to maintain a therapeutic “connection” during this period, other rehabilitation goals were perceived to be less achievable, specifically in physical and occupational therapy. Several barriers affected the process including a decline in the children’s focus and attention, problems with technology, and a distracting home environment.
Prior to the COVID-19 pandemic, the experience at rehabilitation facilities around the world and in Israel had, in many cases, supported telehealth services via pilot studies [
24]. However, previous concerns regarding the feasibility and acceptance of tele-rehabilitation changed dramatically in many locations, including at ALYN Hospital, as rehabilitation professionals around the world responded rapidly in March 2020 and overcame many barriers. The most prominent barriers were therapist’s hesitation to adopt technology, funding through the health management organizations (HMO) and a concern that many key therapeutic goals could not be obtained.
In 2020, an “info-demiological” evaluation [
36], calculated the Relative Search Volume (RSV) and information and the Communications Technology Infrastructure Availability index (ICT) from the World Economic Forum report for the 50 countries most effected by COVID-19. The RSV was calculated by aggregating the information collected from each country, either through Google Trends or the local search engine in Russia and China. Search terms were defined for each of the 50 countries in English, Spanish and the local language. RSV levels were also calculated according to the countries COVID-19 timeline (China January 2020 and all other countries 11 March 2020, in accordance with the WHO announcement of COVID-19 as a pandemic). Although such searches do not necessarily translate to the utilization of telehealth services, they do reflect its perceived significance in each country. Countries with the highest infection and death rates had the highest RSV levels. RSV levels decreased in June and July 2020 (periods with fewer lockdowns) but remained somewhat higher than pre-COVID-19.
The key issue of relevance is whether the tele-rehabilitation experience imposed due to COVID-19 can be harnessed to support future implementations of this approach. Camden & Silva’s [
11] VIRTUAL framework, proposed following the May 2020 eHealth Summit for Pediatric Therapists, provides a convenient tool for interpreting the data presented in this paper. In the context of the ALYN experience,
viewing relates to the insights that the therapists gained by becoming more aware of the patient’s home setting; this can help in modifying the environment, for example, for better training opportunities and compliance. At the beginning of the therapy process, the child or parent provided a virtual tour of the home environment so that an appropriate treatment setting could be selected. Most focus group therapists and parents commented that the opportunity to view the child’s home environment was beneficial in designing between-treatment session exercises that were best suited to overcome setting-specific constraints (e.g., safety concerns in small dwellings). Indeed, this approach is now used even in the case of in-person therapy in order to ensure continuity of therapeutic goals, treatment protocols and home exercise. These findings are in line with the results of Camden et al.’s systematic review [
3] of tele-rehabilitation for young people with disabilities and effective intervention characteristics.
Information relates to how we provided the information (regarding the therapeutic process) to the patients and families with respect to their preferences and technological abilities. The focus groups related to the benefit of having both parents present when sharing therapeutic information as was often the case during the pandemic. Information was also received from the parents and young people as to how to improve the tele-rehabilitation process. For example, in the second focus group, teenagers participating in online therapy said they preferred to have therapy early in the morning or later in the day so that they did not miss scheduled school sessions via Zoom. Another aspect that emerged in the therapist’s focus group was the challenge in sharing information about the patient between therapists to benefit the overall therapeutic process. Many therapists were providing therapy while they themselves were at home and did not meet the other therapists during breaks. Pre-COVID, a lot of key information was shared between therapists during those breaks, information that was not necessarily documented in the electronic medical record. Similar to other global and local tele-rehabilitation settings [
22,
23] particular attention is now focused on how information is documented and shared between therapists and with families to better meet their needs for both remote and in-person therapy.
Relationships were very important to facilitate the tele-rehabilitation process. Therapists stated that having initial in-person time with the young people provided a better base for the development of the relationship during remote sessions, compared to their connection with patients that they never physically met. In both focus groups, participants related to the difference between a therapy session with a therapist/child they had worked prior to the pandemic. Parents of young people in ALYN’s daycare shared the challenge they faced when participating in therapy- how their role in the triad relationship changed from an observational position to a more “hands on” position. Their role as a parent/ therapist changed the dynamics of the relationship. Parents that were primarily involved in the care for the child with special needs also commented on the impact of this on their relationships with other family members. This aspect remains a major goal for implementing future tele-rehabilitation programs. Other tele-rehabilitation settings also reported the patient-therapist rapport challenge. In some cases [
23], therapists noted a positive effect between prior acquaintanceship and online treatment effectiveness. In other cases [
17] satisfaction with the tele-rehabilitation services was reported even when the child-clinician relationship developed only during tele-rehabilitation sessions.
Technology options were explored by the ALYN information technology team to identify the best option that complied with IMOH’s security regulations. As a hospital, strict regulations were needed, although some of the children were in the hospital’s daycare program, where less strict regulations were required. It was a challenge to match the technology to the patients’
unique backgrounds. Due to the moderate number of patients from families without access to the Internet or smartphones, traditional technology such as phone calls were used in some cases. In other cases, at the onset of the pandemic, a simple text, phone and video application was used with the younger children, although it was not approved by the IMOH. As soon as feasible, these patients transferred to the approved technology. The therapists used Zoom functions to facilitate the therapeutic process. For example, “remote control” was granted to the children during therapy. The goal was two-fold: first, to enable interaction similar to that experienced when interacting in-person; second, to give the child some mastery over their own actions during such a restrictive period. Some of the second focus group participants (parents and young people) shared their preference for the familiar technology, such as WhatsApp, LLC, and others indicated that Zoom was too difficult to operate. Going forward, ALYN is considering additional, user-friendly online platforms to better serve the patients and their families during tele-rehabilitation services. Wiederhold [
37] remarked on the ramifications that COVID-19 has had on at-home technology usage, for both work and recreational purposes. Whereas approximately 10 million people regularly attended meetings held on Zoom in 2019, this number had greatly expanded to 300 million by April 2020. Although far from ideal, communication technologies such as Zoom supported the continuation of many work-related activities, including rehabilitation, during the quarantine.
One of the key limitations in wider use of online, remote technologies is the lack of inexpensive tools that can provide data comparable to the types of objective, quantitative outcomes needed by some of the healthcare professions. This was particularly noted by the physical therapists who lacked the ability to assess joint range of motion and muscle strength as well as a range of functional abilities such as gait, posture and balance via online treatment. Indeed, the insufficient availability of reliable and valid high-tech devices (e.g., joint position sensors, force transducers) reduce the type of assessments that can be performed via tele-rehabilitation [
3,
38]. Although still limited, technologies in this field are rapidly developing as demonstrated by tools such as TytoCare, a remote device consisting of a camera, microphone, screen and wireless communication unit. It is equipped with an infrared basal thermometer, digital stethoscope, digital otolaryngoscope and tongue depressors [
39]. Although not designed to provide data to support tele-rehabilitation, TytoCare demonstrates the ability of a small, inexpensive medical device to support healthcare providers in the diagnosis and treatment of common ailments (e.g., ear infections, sore throats, fever, allergies, pink eye, nausea, respiratory infections, and common skin conditions) [
40]. Meditouch’s ArmTutor and 3D Tutor systems provide feedback of elbow range of motion to treat upper limb function post-elbow fractures via a tele-rehabilitation protocol similar to conventional rehabilitation [
41]. The hardware includes wireless electro-optical sensors which detect and display joint movement. The system measures passive and active ROM and movement accuracy in relation to presented virtual targets. It is anticipated that both observational and quantitative assessment of joint range of motion and muscle strength will improve within the next two to five years [
42,
43].
Access to in-person services was limited due to a series of COVID-19 lockdowns. Although patients could return to in-person therapy by July 2020, some families preferred to continue online sessions because of the ease of access to therapy without the need to physically come to the hospital. ALYN continued to provide access to these services when it was apparent that some of the families needed to stay home (e.g., to care for their other children) or because they were afraid to take their respiratory dependent child out of the house. ALYN recognized that some families had access issues and facilitated a donation of computers and game consoles through Microsoft, Inc. [
44] to ensure that the children’s therapeutic process would not be interrupted. Parents in the focus group shared that they appreciated that access to therapy was not discontinued. ALYN is committed to providing access to therapy for all patients as an in-person service or online therapy. In countries such as Australia, with many rural areas, access to tele-rehabilitation services is a challenge regardless of COVID-19 [
17] and they had already accumulated considerable practice in using these tools. Nevertheless, even for such experienced users, lessons were learned from the world’s response during COVID-19.
Finally,
legal aspects of tele-rehabilitation were addressed at the commencement of the process and covered privacy and medico-legal aspects. In a systematic review [
45] of 30 articles on barriers to the adoption of telehealth services, 33 barriers were identified. Legal liability, security and privacy concerns comprised 11 percent of the barriers identified. In March 2020, the only national policy to substantiate the legal stance of tele-rehabilitation at ALYN hospital was the IMOH published guidelines from 2019 (IMOH 6/2019 directive). The guidelines established that the Israel’s four main HMOs would share responsibility for defining best practices, training and insurance coverage. It also stated that citizens had the right to refuse telehealth services, and that the HMOs could not decrease conventional, in-person services. During the pandemic, in-person services were seriously limited by the HMOs. At the onset of the pandemic, all families under treatment at ALYN were asked if they wanted tele-rehabilitation services. Only those that signed a consent form received services. For others, treatment was stopped abruptly. Some families stated that they wanted to wait and see how long the lock-down would last. After a month, ALYN reached out again to the families that originally declined tele-rehabilitation service. A large number of families decided to permit their children to commence online therapy.
In June 2020, in response to the pandemic and as part of the hospital’s experience, hospital representatives participated in the writing of a position paper on telehealth services in occupational therapy [
46]. The paper was accepted by the IMOH. It outlined how remote occupational therapy services should be rendered. For example, choosing the therapy setting at home, parent’s/care giver’s role, security regulations and ethical dilemmas posed to the team during tele-rehabilitation. The IMOH further updated their guidelines in December 2020 (direct communication from IMOH to HMO’s and hospital directors) with specific instructions about reimbursement and consent to online therapy. Further lessons are being documented through IMOH’s special telehealth interest groups including a group of allied health professional working with children with special needs. ALYN has recently updated its policies to include a tele-rehabilitation protocol based on the IMOH occupational therapy position paper [
43]. Some countries (e.g., the USA, Australia) had policies on telehealth services in place pre-COVID-19. For example, the American Telemedicine Association has practice guidelines for remote care on a range of different topics including rehabilitation, mental health and dermatology.
Limitations
It is important to recognize the limitations in this study. As a naturalistic study that started immediately with the onset of the online therapy sessions due to COVID-19, the participants could not be divided into cohorts to compare online and in-person therapies. Data were collected as part of the therapy sessions. In most cases, standard clinical assessments during online sessions could not be performed due to the lack of reliability and validity of these tools for online use. Evaluation of any improvement of function was therefore achieved only through observation of the participant. Future studies of online therapy need to include baseline evaluations, online interventions and follow-up evaluations.




_Weiss.png)


