Resuscitation in Community Healthcare Facilities in Israel
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.1.1. Analysis of Reported Resuscitations
2.1.2. The Questionnaire
2.2. Statistical Analysis
3. Results
3.1. BLS/ACLS Training
3.2. Previous CPR Experience
3.3. Resuscitation Guideline Knowledge
3.4. Confidence in Ability to Perform BLS and to Work as a Member of a Resuscitation Team
3.5. Confidence in Performing Resuscitation Skills
3.6. Work Settings
3.7. Previous Resuscitation Training
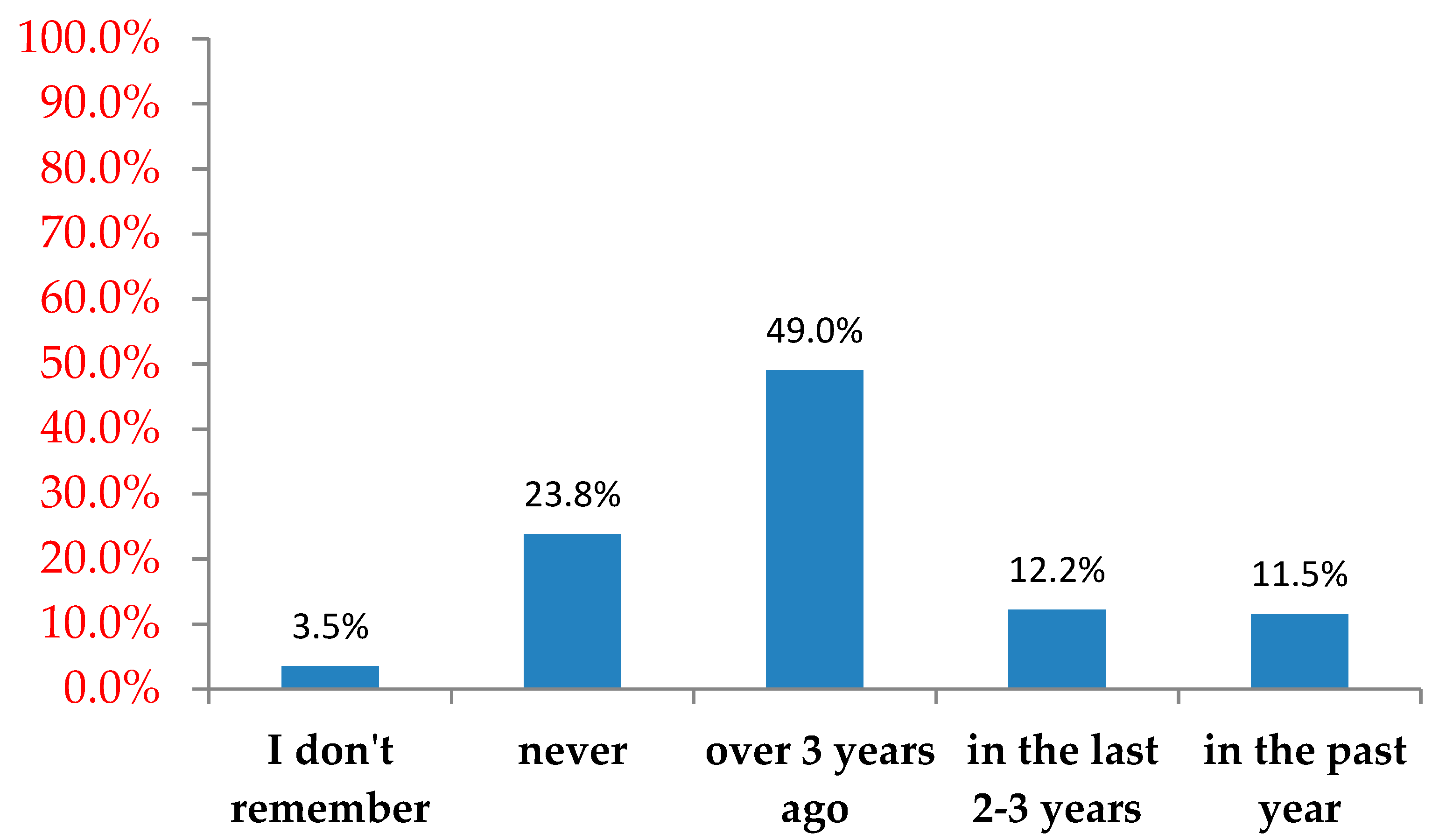
3.8. Resuscitation Experience
3.9. Prediction of Level of Confidence
4. Discussion
5. Conclusions
Implications for Practice
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
- 1.
- Gender: 1. Male 2. Female
- 2.
- Year of birth: _____________
- 3.
- Profession: 1. Physician 2. Nurse
- 4.
- Years of work experience: ___________
- 5.
- What is your main work setting?
- Primary (nursing) care clinics
- Community specialty center
- Urgent care center
- Other: _______
- 6.
- Additional work setting in a hospital:
- yes
- no
- 7.
- Have you been instructed on the use of an automatic defibrillator?
- In the past year
- In the last 2–3 years
- Over 3 years ago
- Never
- I don’t remember
- 8.
- Have you undergone Basic Life Support (BLS) training? When?
- In the past year
- In the last 2–3 years
- Over 3 years ago
- Never
- I don’t remember
- 9.
- Have you undergone Advanced Cardiovascular Life Support (ACLS)? When?
- In the past year
- In the last 2–3 years
- Over 3 years ago
- Never
- I don’t remember
- 10.
- Have you had previous experience in resuscitation?
- In the past year
- In the last 2–3 years
- Over 3 years ago
- Never
- I don’t remember
- 11.
- In how many resuscitation were you involved as a caregiver?
- 1–3 events
- 4–10 events
- More than 10 events
- I don’t remember
- 12.
- Would you be interested in additional resuscitation training and if so what type of training? (a number of answers can be marked)
- No, I don’t feel the need for additional training.
- Yes, more frequently than once every three years.
- Yes, I would like to undergo a resuscitation workshop at the medical center where I work in conjunction with fellow co-workers and the clinic’s resuscitation equipment.
- Yes, online course.
| Completely Agree 5 | Somewhat Agree 4 | Slightly Agree 3 | Neither Disagree nor Agree 2 | Somewhat Disagree 1 | Completely Disagree 0 | ||
| 1 | I believe that I have enough resuscitation knowledge | ||||||
| 2 | I believe I have undergone adequate training in resuscitation | ||||||
| 3 | I feel confident in operating the resuscitation equipment in the clinic | ||||||
| 4 | I feel experienced in performing CPR | ||||||
| 5 | I am confident that I can recognize the cardiac rhythm correctly | ||||||
| 6 | I might hesitate to perform defibrillation, due to fear of harming the patient | ||||||
| 7 | I feel competent to lead a resuscitation team | ||||||
| 8 | I feel competent to work as part of a resuscitation team | ||||||
| 9 | I might hesitate before commencing CPR |
- 1.
- You are in your clinic (equipped with an AED). Which of the following actions would you perform to an adult patient who collapses in front of you and is pulseless:A. Chest compressions should first be performed for two minutes and then a defibrillator should be connected.B. The defibrillator should be connected and given an electric shock as early as possible.C. We have to wait for the Emergency Medical Services (EMS) team to arrive.D. None of the above.
- 2.
- Which of the following rhythm disturbance would you expect in an adult patient who suddenly collapses in front of you and is pulseless on evaluation?A. Ventricular Fibrillation (VF).B. Supra-Ventricular Tachycardia (SVT).C. Atrial Fibrillation (AF).D. COMPLETE AV BLOCK.
- 3.
- Which of the following is correct regarding the defibrillation of a patient in ventricular fibrillation?A. Defibrillation should be delayed until spontaneous cardiac activity returns.B. Intravenous amiodarone administration is as effective as performing defibrillation to achieve Return Of Spontaneous Circulation (ROSC).C. Survival from cardio-pulmonary arrest is highly dependent on early defibrillation, when indicated.D. It is important to give at least one dose of adrenaline before defibrillation.
- 4.
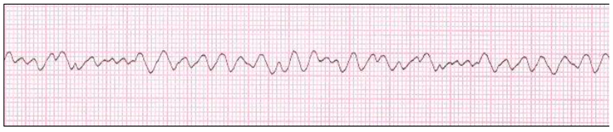
- A 62-year-old patient presented to your clinic and collapsed while waiting to be evaluated. You have connected the patient to the monitor—what is his cardiac rhythm?Which of the following treatment options is immediate treatment?A. Search for reversible causes (5T’S & 5H’S).B. Perform immediate 200J defibrillation with a biphasic defibrilator and then perform chest compressions.C. Perform chest compressions for at least two minutes and then give a defibrillation of intensity 200J.D. Achieve IV (Intravenous) access and administer adrenaline by rapid injection.
- 5.
- Which of the following is the major immediate risk in an adult who becomes unconscious?A. AW obstruction.B. Myocardial infarction (MI).C. Fatal arrhythmias.D. Decreased perfusion of the heart muscle.
References
- Hasselqvist-Ax, I.; Riva, G.; Herlitz, J.; Rosenqvist, M.; Hollenberg, J.; Nordberg, P.; Svensson, L. Early Cardiopulmonary Resuscitation in Out-of-Hospital Cardiac Arrest. N. Engl. J. Med. 2015, 372, 2307–2315. [Google Scholar] [CrossRef]
- Nishiyama, C.; Iwami, T.; Kawamura, T.; Kitamura, T.; Tanigawa, K.; Sakai, T.; Hayashida, S.; Nishiuchi, T.; Hayashi, Y.; Hiraide, A. Prodromal symptoms of out-of-hospital cardiac arrests: A report from a large-scale population-based cohort study. Resuscitation 2013, 84, 558–563. [Google Scholar] [CrossRef]
- Guyette, F.X.; Reynolds, J.C.; Frisch, A. Cardiac Arrest Resuscitation. Emerg. Med. Clin. North Am. 2015, 33, 669–690. [Google Scholar] [CrossRef]
- Berdowski, J.; Berg, R.A.; Tijssen, J.G.; Koster, R.W. Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation 2010, 81, 1479–1487. [Google Scholar] [CrossRef]
- Masterson, S.; Cullinan, J.; McNally, B.; Deasy, C.; Murphy, A.; Wright, P.; O’Reilly, M.; Vellinga, A. Out-of-hospital cardiac arrest attended by ambulance services in Ireland: First 2 years’ results from a nationwide registry. Emerg. Med. J. 2016, 33, 776–781. [Google Scholar] [CrossRef]
- Myerburg, R.J. Sudden Cardiac Death: Exploring the Limits of Our Knowledge. J. Cardiovasc. Electrophysiol. 2001, 12, 369–381. [Google Scholar] [CrossRef]
- Ong, M.E.H.; Yap, S.; Chan, K.P.; Sultana, P.; Anantharaman, V. Knowledge and attitudes towards cardiopulmonary Resuscitation and defibrillation amongst Asian primary health care physicians. Open Access Emerg. Med. 2009. [Google Scholar] [CrossRef]
- Einav, S.; Wacht, O.; Kaufman, N.; Alkalay, E. Cardiopulmonary arrest in primary care clinics: More holes than cheese: A survey of the knowledge and attitudes of primary care physicians regarding resuscitation. Isr. J. Health Policy Res. 2017, 6, 22. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Passali, C.; Pantzopoulos, I.; Dontas, I.; Patsaki, A.; Barouxis, D.; Troupis, G.; Xanthos, T. Evaluation of nurses’ and doctors’ knowledge of basic & advanced life support resuscitation guidelines. Nurse Educ. Pract. 2011, 11, 365–369. [Google Scholar] [CrossRef] [PubMed]
- McNally, B.; Robb, R.; Mehta, M.; Vellano, K.; Valderrama, A.L.; Yoon, P.W.; Kellerman, A. Out- of- hospital Cardiac Arrest Surveillance–Cardiac Arrest Registry to Enhance Survival (CARES), United State, October 1, 2005–December 31. MMWR Surveille Summ. 2011, 60, 1–19. Available online: http://www.cdc.gov/mmwr/preview/mmwrhtml/ss6008a1.htm (accessed on 29 July 2011).
- Lin, S.; Smith, N.; Gray, D. The place of general practitioners in the management of out- of- hospital cardiopulmonary resuscitation. Resuscitation 1999. [Google Scholar] [CrossRef]
- Ginsberg, G.M.; Kark, J.D.; Einav, S. Cost-utility analysis of treating out of hospital cardiac arrests in Jerusalem. Resuscitation 2015, 86, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Ong, M.E.; Yan, X.; Lau, G.; Tan, E.H.; Panchalingham, A.; Leong, B.S.; Venkataramah, A. Out-of-hospital cardiac arrests occurring in primary health care facilities in Singapore. Resuscitation 2007, 74, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Siobhán Masterson, S.; Vellinga, A.; Wright, P.; Dowling, J.; Bury, G.; Murphy, A.W. General practitioner contribution to out-of-hospital cardiac arrest outcome: A national registry study. Eur. J. Gen. Pract. 2015, 21, 1–7. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Colquhoun, M.C. Defibrillation by general practitioners. Resuscitation 2002, 52, 143–148. [Google Scholar] [CrossRef]
- Peberdy, M.A.; Callaway, C.W.; Neumar, R.W.; Geocadin, R.G.; Zimmerman, J.L.; Donnino, M.; Kronick, S.L. Post cardiac arrest care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010, 122, 768–786. [Google Scholar] [CrossRef]
- Hamilton, R. Nurses’ knowledge and skill retention following cardiopulmonaryresuscitation training: A review of the literature. J. Adv. Nurs. 2004, 51, 288–297. [Google Scholar] [CrossRef]
- Abolfotouh, M.A.; Alnasser, M.A.; Berhanu, A.N.; Al-Turaif, D.A.; Alfayez, A.I. Impact of basic life-support training on the attitudes of health-care workers toward cardiopulmonary resuscitation and defibrillation. BMC Health Serv. Res. 2017, 17, 674. [Google Scholar] [CrossRef]
- Available online: http://www.health.gov.il/hozer/mr04_2012.pdf (accessed on 12 February 2019).
- Bahr, J.; Berg, R.A.; Billi, J.E.; Bossaert, L.; Cassan, P.; Coovadia, A.; D’Este, K.; Finn, J.; Halperin, H.; Handley, A.; et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update and simplification of the Utstein templates for resuscitation registries: A statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, Inter American Heart Foundation, Resuscitation Councils of Southern Africa). Circulation 2004, 110, 3385–3397. [Google Scholar] [CrossRef]
- Eubank, B.H.; Mohtadi, N.G.; Lafave, M.R.; Wiley, J.P.; Bois, A.J.; Boorman, R.S.; Sheps, D.V. Using the modified Delphi method to establish clinical consensus for the diagnosis and treatment of patients with rotator cuff pathology. BMC Med. Res. Methodol. 2016, 16, 56. [Google Scholar] [CrossRef]
- Ong, M.E.; Chan, Y.H.; Ang, H.Y.; Lim, S.H.; Tan, K.L. Resuscitation of out-of-hospital cardiac arrest by Asian primary health-care physicians. Resuscitation 2005, 65, 191–195. [Google Scholar] [CrossRef]
- Ahna, K.O.; Shinb, S.D.; Suhb, G.J.; Chac, W.C.; Songd, K.J.; Kime, S.J.; Leeb, E.J.; Hock Ongf, M.E. Epidemiology and outcomes from non-traumatic out-of-hospital cardiac arrest inKorea: A nationwide observational study. Resuscitation 2010, 81, 974–981. [Google Scholar] [CrossRef] [PubMed]
- Hock Onga, M.E.; Shinc, S.D.; Amatullah De Souza, N.N.; Tanaka, H.T.; Nishiuchif, T.; Songc, K.J.; Chow-In Kog, P.; Leongi, B.S.; Khunkhlai, N.; Narook, G.Y.; et al. Outcomes for out-of-hospital cardiac arrests across 7 countries in Asia: The Pan Asian Resuscitation Outcomes Study (PAROS). Resuscitation 2015, 96, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Gräsner, J.T.; Leferingc, R.; Koster, R.W.; Masterson, S.; Böttiger, B.W.; Herlitz, J.; Wnent, J.; Tjelmeland, I.B.; Ortiz, F.R.; Maurer, H.; et al. EuReCa ONE—27 Nations, ONE Europe, ONE Registry, A prospective one month analysis of out-of-hospital cardiac arrestoutcomes in 27 countries in Europe. Resuscitation 2016, 105, 188–195. [Google Scholar] [CrossRef]
- Żuratyński, P.; Ślęzak, D.; Dąbrowski, S.; Krzyżanowski, K.; Mędrzycka-Dąbrowska, W.; Rutkowski, P. Use of Public Automated External Defibrillators in Out-of-Hospital Cardiac Arrest in Poland. Medicina 2021, 57, 298. [Google Scholar] [CrossRef] [PubMed]
- Kozamani, A.; Kapadochos, T.; Kadda, A. Factors that influence nursing staff attitudes towards initiating CPR and in using an automatic external defibrillator when outside of a hospital. Health Sci. J. 2012, 6, 88–101. [Google Scholar]
| Chest Compression Characteristics | Female Patients | Male Patients | Total |
|---|---|---|---|
| Physician led Chest compressions | 6 (27.3%) | 2 (25.0%) | 4 (28.6%) |
| Nurse led chest compressions | 9 (40.9%) | 4 (40.0%) | 5 (35.7%) |
| Leading chest compression provider not listed | 1 (4.5%) | 0 | 1 (7.1%) |
| Chest Compressions not performed by HMO staff | 1 (4.5%) | 1 (12.5%) | 2 (14.3%) |
| Nurses | Physicians | |||
|---|---|---|---|---|
| Respondents | Target Group | Respondents | Target Group | |
| N-149 | N-1300 | N-126 | N-1500 | |
| Age (years) | 43.4 | 44.33 | 52 | 54.49 |
| Mean (SD) | (9.87) | (8.59) | (10.6) | (12.3) |
| Experience (years) | 15.6 | 11.03 | 21.2 | 12.56 |
| Mean (SD) | (8.63) | (9.46) | (11.7) | (10.8) |
| Gender | ||||
| Female, n (%) | 143 (95.9%) | (93.80%) | 59 (48%) | 579 (38.6%) |
| Male, n (%) | 6 (4.1%) | (6.20%) | 64 (52%) | 921 (61.4%) |
| Question | N (%) |
|---|---|
| Q1. A 62-year-old patient presented to your clinic and collapsed while waiting to be evaluated. You have connected the patient to the monitor—what is his cardiac rhythm (participants were presented with a rhythm strip of ventricular fibrillation and asked to identify the rhythm). | 218 (75.7%) |
| Q2. Which of the following rhythm disturbances would you expect in an adult patient who suddenly collapses in front of you and is pulseless on evaluation? | 253 (87.8%) |
| Q3. Which of the following is the major immediate risk in an adult unconscious patient? | 202 (70.1%) |
| Q4. You are in your clinic (equipped with an Automated External Defibrilator). Which of the following actions would you perform on an adult patient who collapsed in front of you and is pulseless. | 162 (56.3%) |
| Q5. Which of the following is correct regarding the defibrillation of a patient in ventricular fibrillation? | 266 (92.4%) |
| Predictive Variables First Level | Coefficients | |||||
|---|---|---|---|---|---|---|
| R2 | p | t | B | SE | ||
| Gender (1 = male) | 0.33 | 0.14 | 1.46 | 0.16 | 0.11 | 0.10 |
| Age | 0.85 | −0.18 | −0.01 | 0.01 | −0.02 | |
| Professional experience | 0.28 | 1.06 | 0.01 | 0.01 | 0.12 | |
| Profession (1 = doctor) | 0.14 | −1.48 | −0.15 | 0.10 | −0.10 | |
| Work settings (1 = primary care clinics) | 0.01 | −2.53 * | −0.25 | 0.10 | −0.14 | |
| Additional work setting in a hospital (1 = yes) | 0.01 | 2.37 * | 0.36 | 0.15 | 0.14 | |
| Experience in CPR | 0.00 | 4.51 ** | 0.21 | 0.04 | 0.33 | |
| cardiac arrests in the past (1 = yes) | 0.16 | 1.39 | 0.16 | 0.12 | 0.10 | |
| Previous resuscitation training | 0.00 | −3.14 ** | −0.24 | 0.07 | −0.18 | |
| Second level | ||||||
| Level of knowledge | 0.33 | 0.40 | 0.89 | 0.04 | 0.00 | 0.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zherebovich, I.; Goldberg, A.; Ben Tov, A.; Schwartz, D. Resuscitation in Community Healthcare Facilities in Israel. Int. J. Environ. Res. Public Health 2021, 18, 6612. https://doi.org/10.3390/ijerph18126612
Zherebovich I, Goldberg A, Ben Tov A, Schwartz D. Resuscitation in Community Healthcare Facilities in Israel. International Journal of Environmental Research and Public Health. 2021; 18(12):6612. https://doi.org/10.3390/ijerph18126612
Chicago/Turabian StyleZherebovich, Irena, Avishay Goldberg, Amir Ben Tov, and Dagan Schwartz. 2021. "Resuscitation in Community Healthcare Facilities in Israel" International Journal of Environmental Research and Public Health 18, no. 12: 6612. https://doi.org/10.3390/ijerph18126612
APA StyleZherebovich, I., Goldberg, A., Ben Tov, A., & Schwartz, D. (2021). Resuscitation in Community Healthcare Facilities in Israel. International Journal of Environmental Research and Public Health, 18(12), 6612. https://doi.org/10.3390/ijerph18126612