Early Nutritional Education in the Prevention of Childhood Obesity
Abstract
1. Introduction
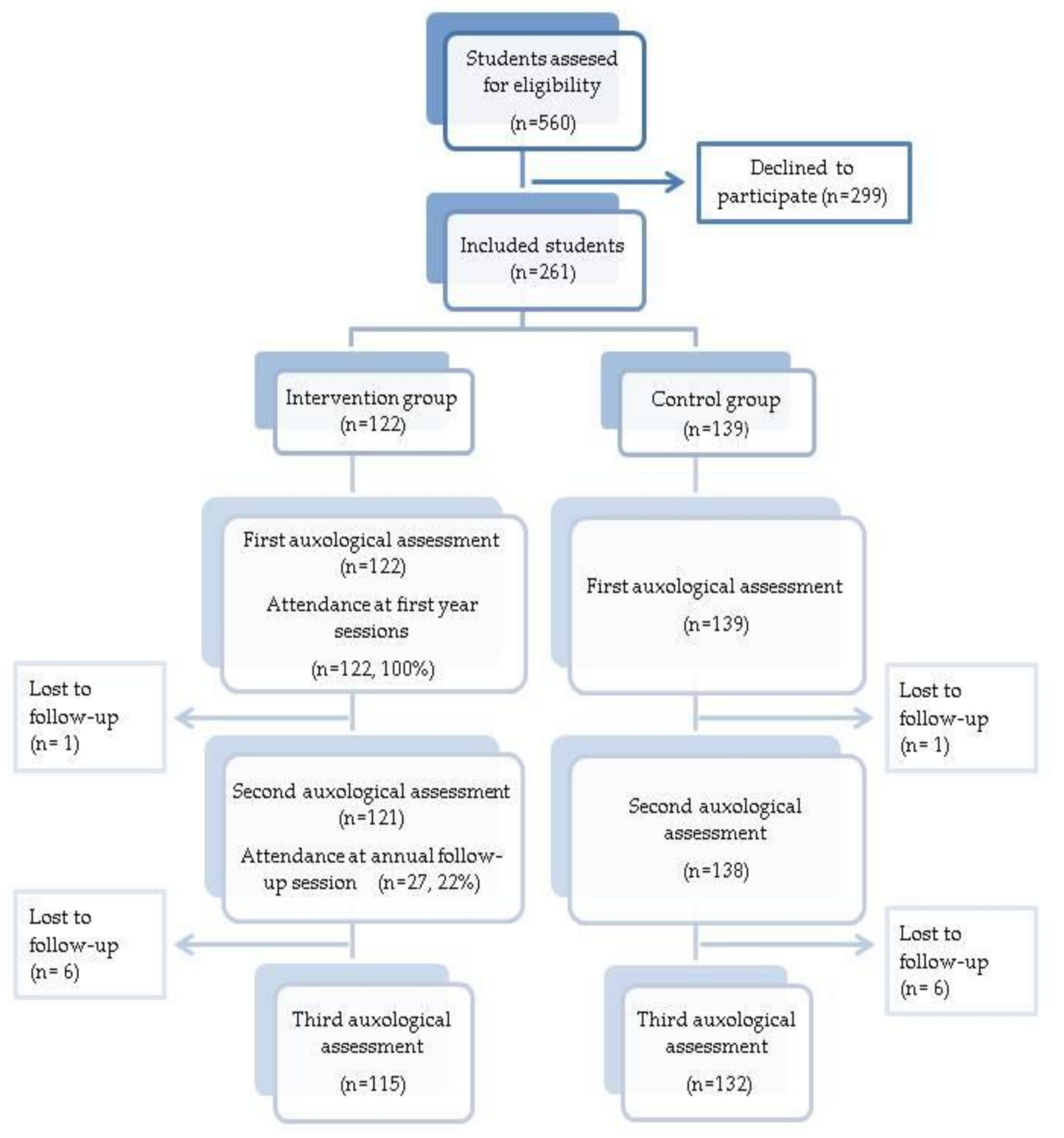
2. Materials and Methods
2.1. Variables
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Nutrition and Physical Activity Education Program
- 1st group session: Introduction to nutrition. Duration: 2 h. Activities:
- ○
- Knowledge of basic concepts: Nourishment and eating habits, Nutrition, Foods, Diet, Diet therapy.
- ○
- Understanding the concept of obesity and overweight, its various causes and possible consequences.
- ○
- Learn the different nutrients and their function in the human body: macronutrients, carbohydrates and sugars (starches), proteins, lipids, fats, micronutrients, vitamins and minerals.
- 2nd group session: Healthy eating habits. Duration: 2 h. Activities:
- ○
- Recognizing one’s own eating habits and which factors could be modified.
- ○
- Assessing the importance of good eating habits for health.
- ○
- Recognizing the social importance of food and nutrition in all its dimensions, which influence and establish the eating patterns of populations.
- 3rd group session: Keys to improving nutrition and eating habits. Duration: 2 h. Activities:
- ○
- Learn the 7 food groups and become familiar with the main nutrients provided by each of them.
- ○
- Analyze, understand and develop skills associated with behavior at the table at mealtime.
- ○
- Become aware of the uses of eating in different situations: calming anxiety, compensating frustration, comfort.
- ○
- Ten principles of a diet.
- 4th group session: Designing a healthy menu. Duration: 2 h. Activities:
- ○
- Understand the concept of food servings and how to adapt the criteria for a balanced diet such as servings of the different food groups.
- ○
- Recognize the importance of food choice, frequency, serving size and volume over a period of time to maintain good health.
- ○
- Describe your own diet, assessing the possibilities of defining it as healthy based on your own knowledge about Nutrition—Health.
- ○
- Understand the most important aspects to be considered when designing a meal plan.
- ○
- Learn to use food servings with new recipes.
- 5th group session: Food labeling. Duration: 2 h. Activities:
- ○
- Understand the meanings of terms used on food labels.
- ○
- Learn to recognize the healthiest foods by reading the ingredients and the nutritional information of the label.
- 6th group session: Physical activity. Duration: 2 h. Activities:
- ○
- Learn how sports can be beneficial on a physical, psychological and emotional level.
- ○
- Simple ways to encourage physical activity.
- Annual follow-up session. Duration: 3 h. Activities:
- ○
- Review the different nutrients and their importance in the diet.
- ○
- Review the preparation of a healthy menu.
- ○
- Review the benefits of physical activity and how to stimulate it.
References
- NCD Risk Factor Collaboration. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- WHO. Consideration of the Evidence on Childhood Obesity for the Commission on Ending Childhood Obesity: Report of the Ad Hoc Working Group on Science and Evidence for Ending Childhood Obesity; World Health Organization: Geneva, Switzerland, 2016; pp. 1–219. [Google Scholar]
- Cunningham, S.A.; Kramer, M.R.; Narayan, K.M.V. Incidence of childhood obesity in the United States. N. Engl. J. Med. 2014, 370. [Google Scholar] [CrossRef] [PubMed]
- Agencia Española de Seguridad Alimentaria y Nutrición. Estudio ALADINO 2019: Estudio de Vigilancia del Crecimiento, Alimentación, Actividad Física, Desarrollo Infantil y Obesidad en España. 2019. Available online: https://www.aesan.gob.es/AECOSAN/docs/documentos/nutricion/observatorio/Informe_Aladino_2019.pdf (accessed on 17 June 2021).
- López-Siguero, J.P.; Fernández García, J.M.F.; Castillo, J.D.D.L.; Moreno, J.A.M.; Cosano, C.R.; Ortiz, A.J. Cross-sectional study of height and weight in the population of Andalusia from age 3 to adulthood. BMC Endocr. Disord. 2008, 8, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Shah, B.; Cost, K.T.; Fuller, A.; Birken, C.S.; Anderson, L.N. Sex and gender differences in childhood obesity: Contributing to the research agenda. BMJ Nutr. Prev. Health 2020. [Google Scholar] [CrossRef]
- Dev, D.A.; McBride, B.A.; Fiese, B.H.; Jones, B.L.; Cho, H. On behalf of the STRONG Kids Research Team. Risk factors for overweight/obesity in preschool children: An ecological approach. Child. Obes. 2013, 9, 399–408. [Google Scholar] [CrossRef]
- Qiao, Y.; Ma, J.; Wang, Y.; Li, W.; Katzmarzyk, P.T.; Chaput, J.P.; Hu, G. Birth weight and childhood obesity: A 12-country study. Int. J. Obes. Suppl. 2015, 5, S74–S79. [Google Scholar] [CrossRef]
- Bergmann, K.E.; Bergmann, R.L.; Von Kries, R.; Böhm, O.; Richter, R.; Dudenhausen, J.W.; Wahn, U. Early determinants of childhood overweight and adiposity in a birth cohort study: Role of breast-feeding. Int. J. Obes. 2003, 27, 162–172. [Google Scholar] [CrossRef]
- Tang, M. Protein intake during the first two years of life and its association with growth and risk of overweight. Int. J. Environ. Res. Public Health 2018, 15, 1742. [Google Scholar] [CrossRef]
- Rolland-Cachera, M.F.; Deheeger, M.; Maillot, M.; Bellisle, F. Early adiposity rebound: Causes and consequences for obesity in children and adults. Int. J. Obes. 2006, 30. [Google Scholar] [CrossRef]
- Gil, J.M.; Takourabt, S. Socio-economics, food habits and the prevalence of childhood obesity in Spain. Child. Care. Health Dev. 2017, 43, 250–258. [Google Scholar] [CrossRef]
- Gortmaker, S.L.; Taveras, E.M. Who becomes obese during childhood—Clues to prevention. N. Engl. J. Med. 2014, 370, 475–476. [Google Scholar] [CrossRef]
- Weihrauch-Blüher, S.; Wiegand, S. Risk factors and implications of childhood obesity. Curr. Obes. Rep. 2018, 7, 254–259. [Google Scholar] [CrossRef]
- Sahoo, K.; Sahoo, B.; Choudhury, A.K.; Sofi, N.Y.; Kumar, R.; Bhadoria, A.S. Childhood obesity: Causes and consequences. J. Fam. Med. Prim. Care 2015, 4, 187. [Google Scholar]
- Quek, Y.H.; Tam, W.W.S.; Zhang, M.W.B.; Ho, R.C.M. Exploring the association between childhood and adolescent obesity and depression: A meta-analysis. Obes. Rev. 2017, 18, 742–754. [Google Scholar] [CrossRef] [PubMed]
- González-Muniesa, P.; Mártinez-González, M.A.; Hu, F.B.; Després, J.P.; Matsuzawa, Y.; Loos, R.J.F.; Moreno, L.A.; Bray, G.A.; Martinez, J.A. Obesity. Nat. Rev. Dis. Prim. 2017, 3. [Google Scholar] [CrossRef] [PubMed]
- Baidal, J.A.W.; Taveras, E.M. Childhood obesity: Shifting the focus to early prevention. Arch. Pediatr. Adolesc. Med. 2012, 166. [Google Scholar] [CrossRef] [PubMed]
- Skinner, A.C.; Perrin, E.M.; Moss, L.A.; Skelton, J.A. Cardiometabolic risks and severity of obesity in children and young adults. N. Engl. J. Med. 2015, 373, 1307–1317. [Google Scholar] [CrossRef]
- Lanigan, J. Prevention of overweight and obesity in early life. Proc. Nutr. Soc. 2018, 77, 247–256. [Google Scholar] [CrossRef]
- Notario-Barandiaran, L.; Valera-Gran, D.; Gonzalez-Palacios, S.; Garcia-de-la-Hera, M.; Fernández-Barrés, S.; Pereda-Pereda, E.; Fernández-Somoano, A.; Guxens, M.; Iñiguez, C.; Romaguera, D.; et al. High adherence to a Mediterranean diet at age 4 reduces overweight, obesity and abdominal obesity incidence in children at the age of 8. Int. J. Obes. 2020, 4, 1906–1917. [Google Scholar] [CrossRef]
- Ariza, C.; Ortega-Rodríguez, E.; Sánchez-Martínez, F.; Valmayor, S.; Juárez, O.; Pasarín, M.I. La prevención de la obesidad infantil desde una perspectiva comunitaria. Aten. Primaria 2015, 47, 246–255. [Google Scholar] [CrossRef]
- Arai, L.; Panca, M.; Morris, S.; Curtis-Tyler, K.; Lucas, P.J.; Roberts, H.M. Time, monetary and other costs of participation in family-based child weight management interventions: Qualitative and systematic review evidence. PLoS ONE 2015, 10, 1–12. [Google Scholar] [CrossRef]
- Flodmark, C.E. Prevention models of childhood obesity in Sweden. Obes. Facts 2018, 11, 257–262. [Google Scholar] [CrossRef]
- Brown, T.; Moore, T.H.; Hooper, L.; Gao, Y.; Zayegh, A.; Ijaz, S.; Elwenspoek, M.; Foxen, S.C.; Magee, L.; O’Malley, C.; et al. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2019, 7. [Google Scholar] [CrossRef]
- Lavelle, H.V.; MacKay, D.F.; Pell, J.P. Systematic review and meta-analysis of school-based interventions to reduce body mass index. J. Public Heal. UK 2012, 34. [Google Scholar] [CrossRef]
- Krystia, O.; Ambrose, T.; Darlington, G.; Ma, D.W.L.; Buchholz, A.C.; Haines, J. A randomized home-based childhood obesity prevention pilot intervention has favourable effects on parental body composition: Preliminary evidence from the Guelph Family Health Study. BMC Obes. 2019, 6, 1–9. [Google Scholar] [CrossRef]
- Carrascosa, A.; Fernández, J.; Ferrández, A.; López-Siguero, J.; López, D.; Sánchez, E. Estudios Españoles de Crecimiento 2010. Rev. Esp. Endocrinol. Pediatr. 2011, 2, 59–62. [Google Scholar]
- Styne, D.M.; Arslanian, S.A.; Connor, E.L.; Farooqi, I.S.; Murad, M.H.; Silverstein, J.H.; Yanovski, J.A. Pediatric obesity-assessment, treatment, and prevention: An endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 2017, 102. [Google Scholar] [CrossRef]
- Pérez Solís, D.; Díaz Martín, J.J.; Álvarez Caro, F.; Suárez Tomás, I.; Suárez Menéndez, E.; Riaño Galán, I. Efectividad de una intervención escolar contra la obesidad. An. Pediatr. 2015, 83, 19–25. [Google Scholar] [CrossRef]
- Slusser, W.; Frankel, F.; Robison, K.; Fischer, H.; Cumberland, W.G.; Neumann, C. Pediatric overweight prevention through a parent training program for 2–4-year-old Latino children. Child. Obes. 2012, 8, 52–59. [Google Scholar] [CrossRef]
- Murimi, M.W.; Moyeda-Carabaza, A.F.; Nguyen, B.; Saha, S.; Amin, R.; Njike, V. Factors that contribute to effective nutrition education interventions in children: A systematic review. Nutr. Rev. 2018, 76, 553–580. [Google Scholar] [CrossRef] [PubMed]
- Gardner, D.S.L.; Hosking, J.; Metcalf, B.S.; Jeffery, A.N.; Voss, L.D.; Wilkin, T.J. Contribution of early weight gain to childhood overweight and metabolic health: A longitudinal study (EarlyBird 36). Pediatrics 2009, 123, e67–e73. [Google Scholar] [CrossRef] [PubMed]
- Ong, K.K.; Petry, C.J.; Emmett, P.M.; Saradhu, M.S.; Kiess, W.; Hales, C.N.; Ness, A.R.; Dunger, D.B. Insulin sensitivity and secretion in normal children related to size at birth, postnatal growth, and plasma insulin-like growth factor-I levels. Diabetologia 2004, 47, 1064–1070. [Google Scholar] [CrossRef] [PubMed]
- Ljungkrantz, M.; Ludvigsson, J.; Samuelsson, U. Type 1 diabetes: Increased height and weight gains in early childhood. Pediatr. Diabetes 2008, 9, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Nader, P.R.; O’Brien, M.; Houts, R.; Bradley, R.; Belsky, J.; Crosnoe, R.; Friedman, S.; Mei, Z.; Susman, E.J. Identifying risk for obesity in early childhood. Pediatrics 2006, 118, e594–e601. [Google Scholar] [CrossRef]
- Morgan, P.J.; Collins, C.E.; Plotnikoff, R.C.; Callister, R.; Burrows, T.; Fletcher, R.; Okely, A.D.; Young, M.D.; Miller, A.; Lloyd, A.B.; et al. The “Healthy dads, healthy kids” community randomized controlled trial: A community-based healthy lifestyle program for fathers and their children. Prev. Med. Baltim. 2014, 61, 90–99. [Google Scholar] [CrossRef]
| Variable | Control | Intervention | p |
|---|---|---|---|
| n | 139 | 122 | |
| Female, % | 43.90 | 49.20 | 0.392 |
| Age (months) | 43.81 ± 3.93 | 45.70 ± 5.41 | 0.002 * |
| zBMI | 0.17 ± 0.82 | 0.23 ± 1.18 | 0.640 |
| zWeight | 0.04 ± 0.82 | 0.12 ± 1.2 | 0.645 |
| zHeight | −0.16 ± 0.92 | −0.12 ± 1.03 | 0.761 |
| zBMI > 0 (median), % | 51.10 | 48.40 | 0.661 |
| Overweight, % | 5.8 | 7.4 | 0.867 |
| Obesity, % | 6.5 | 6.6 | 0.867 |
| Overweight and obesity, % | 12.2 | 14 | 0.683 |
| zBMI | Control | Intervention | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Baseline | Final | Change | p | n | Baseline | Final | Change | p | |
| 1st year | 138 | 0.17 ± 0.82 | 0.14 ± 0.96 | −0.03 | 0.261 | 121 | 0.23 ± 1.18 | 0.10 ± 0.99 | −0.13 | 0.002 * |
| 2nd year | 132 | 0.16 ± 0.83 | 0.17 ± 1.03 | 0.01 | 0.423 | 115 | 0.24 ± 1.21 | 0.14 ±1.05 | −0.10 | 0.021 * |
| Subgroup | zBMI | Control | Intervention | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Baseline | Final | Change | p | n | Baseline | Final | Change | p | ||
| zBMI < 0 | 1st year | 68 | −0.47 ± 0.33 | −0.52 ± 0.42 | −0.05 | 0.296 | 63 | −0.48 ± 0.31 | −0.48 ± 0.45 | 0.00 | 0.401 |
| 2nd year | 67 | −0.47 ± 0.33 | −0.50 ± 0.41 | −0.03 | 0.511 | 59 | −0.49 ± 0.32 | −0.43 ± 0.52 | 0.06 | 0.764 | |
| zBMI > 0 | 1st year | 70 | 0.80 ± 0.65 | 0.78 ± 0.89 | −0.02 | 0.64 | 58 | 1.00 ± 1.30 | 0.72 ± 1.05 | −0.28 | 0.001 * |
| 2nd year | 65 | 0.83 ± 0.66 | 0.86 ± 1.03 | 0.03 | 0.694 | 56 | 1.01 ± 1.32 | 0.73 ± 1.15 | −0.28 | 0.002 * | |
| Control | Intervention | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | Final | Change | p | Baseline | Final | Change | p | ||
| Overweight and obesity % | 1st year | 12.2 | 15.8 | 3.6 | 0.227 | 13.9 | 13.9 | 0 | 1 |
| 2nd year | 12.2 | 20.1 | 7.9 | 0.027 * | 13.9 | 18 | 4.1 | 0.302 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gato-Moreno, M.; Martos-Lirio, M.F.; Leiva-Gea, I.; Bernal-López, M.R.; Vegas-Toro, F.; Fernández-Tenreiro, M.C.; López-Siguero, J.P. Early Nutritional Education in the Prevention of Childhood Obesity. Int. J. Environ. Res. Public Health 2021, 18, 6569. https://doi.org/10.3390/ijerph18126569
Gato-Moreno M, Martos-Lirio MF, Leiva-Gea I, Bernal-López MR, Vegas-Toro F, Fernández-Tenreiro MC, López-Siguero JP. Early Nutritional Education in the Prevention of Childhood Obesity. International Journal of Environmental Research and Public Health. 2021; 18(12):6569. https://doi.org/10.3390/ijerph18126569
Chicago/Turabian StyleGato-Moreno, Mario, María F. Martos-Lirio, Isabel Leiva-Gea, M. Rosa Bernal-López, Fernando Vegas-Toro, María C. Fernández-Tenreiro, and Juan P. López-Siguero. 2021. "Early Nutritional Education in the Prevention of Childhood Obesity" International Journal of Environmental Research and Public Health 18, no. 12: 6569. https://doi.org/10.3390/ijerph18126569
APA StyleGato-Moreno, M., Martos-Lirio, M. F., Leiva-Gea, I., Bernal-López, M. R., Vegas-Toro, F., Fernández-Tenreiro, M. C., & López-Siguero, J. P. (2021). Early Nutritional Education in the Prevention of Childhood Obesity. International Journal of Environmental Research and Public Health, 18(12), 6569. https://doi.org/10.3390/ijerph18126569







