Institute of Medicine Recommendations on the Rate of Gestational Weight Gain and Perinatal Outcomes in Rural Bangladesh
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
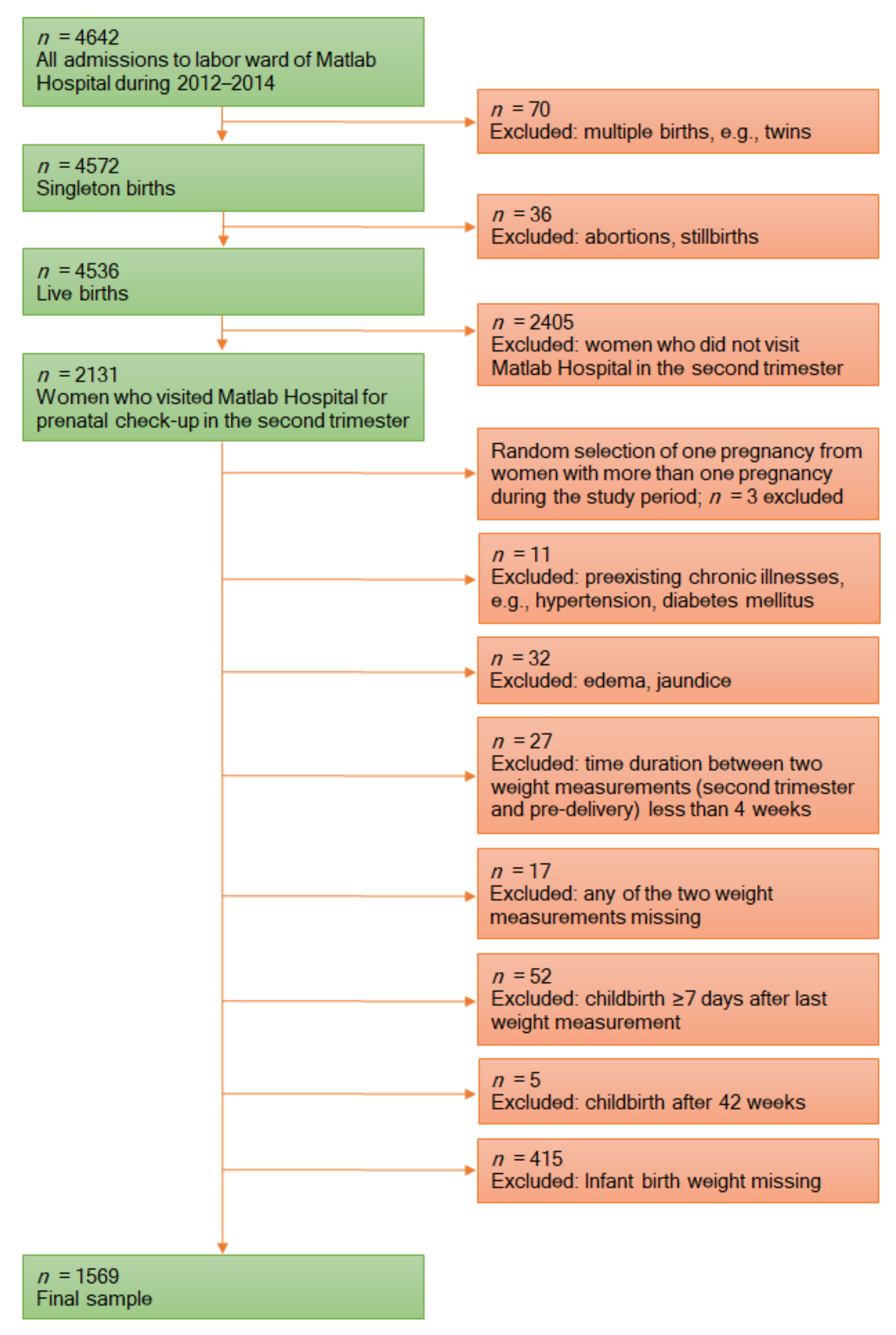
2.2. Study Population and Data Source
2.3. Prepregnancy BMI
2.4. Rate of Weight Gain during the Second and Third Trimester
2.5. Outcomes
2.6. Statistical Analysis
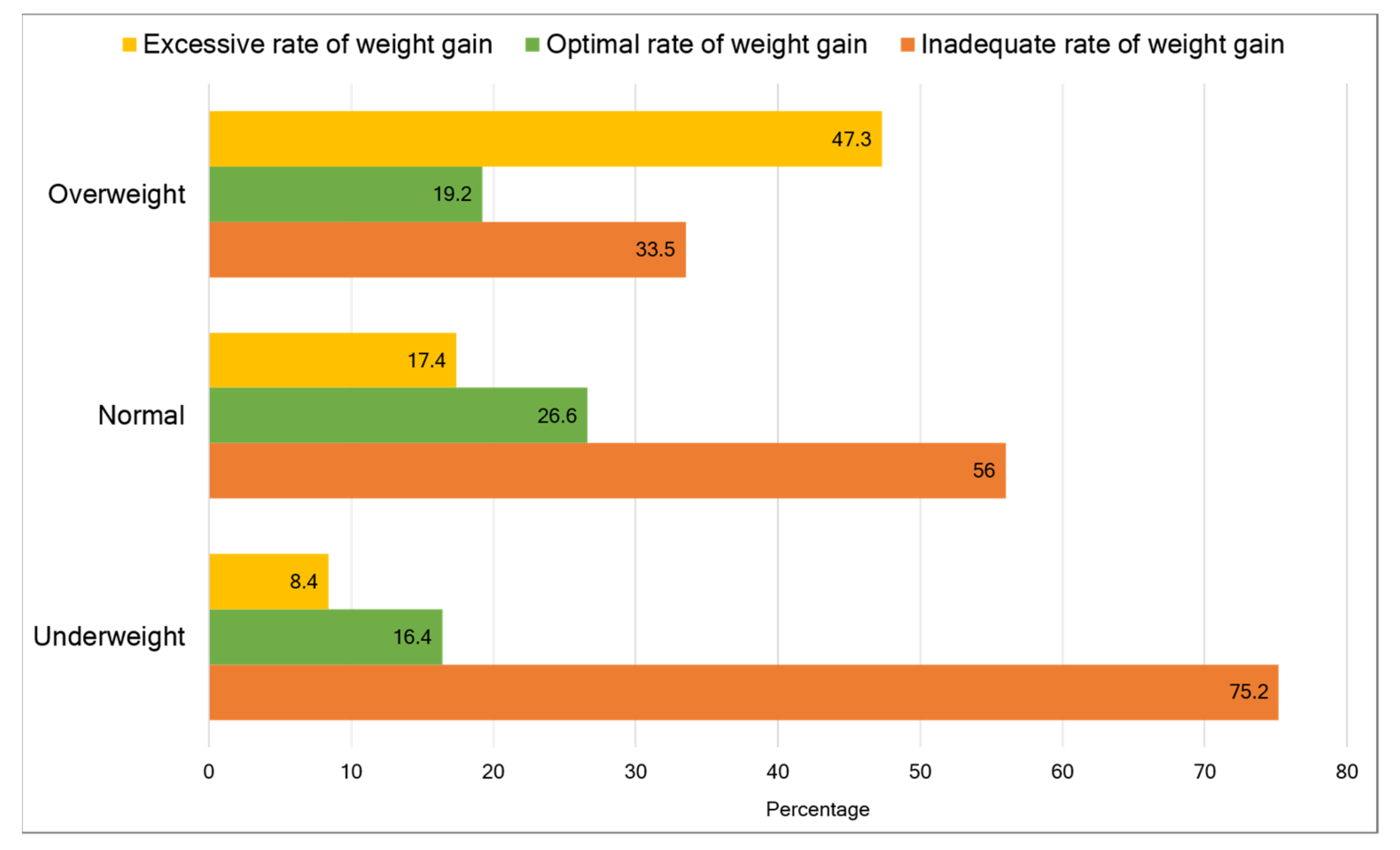
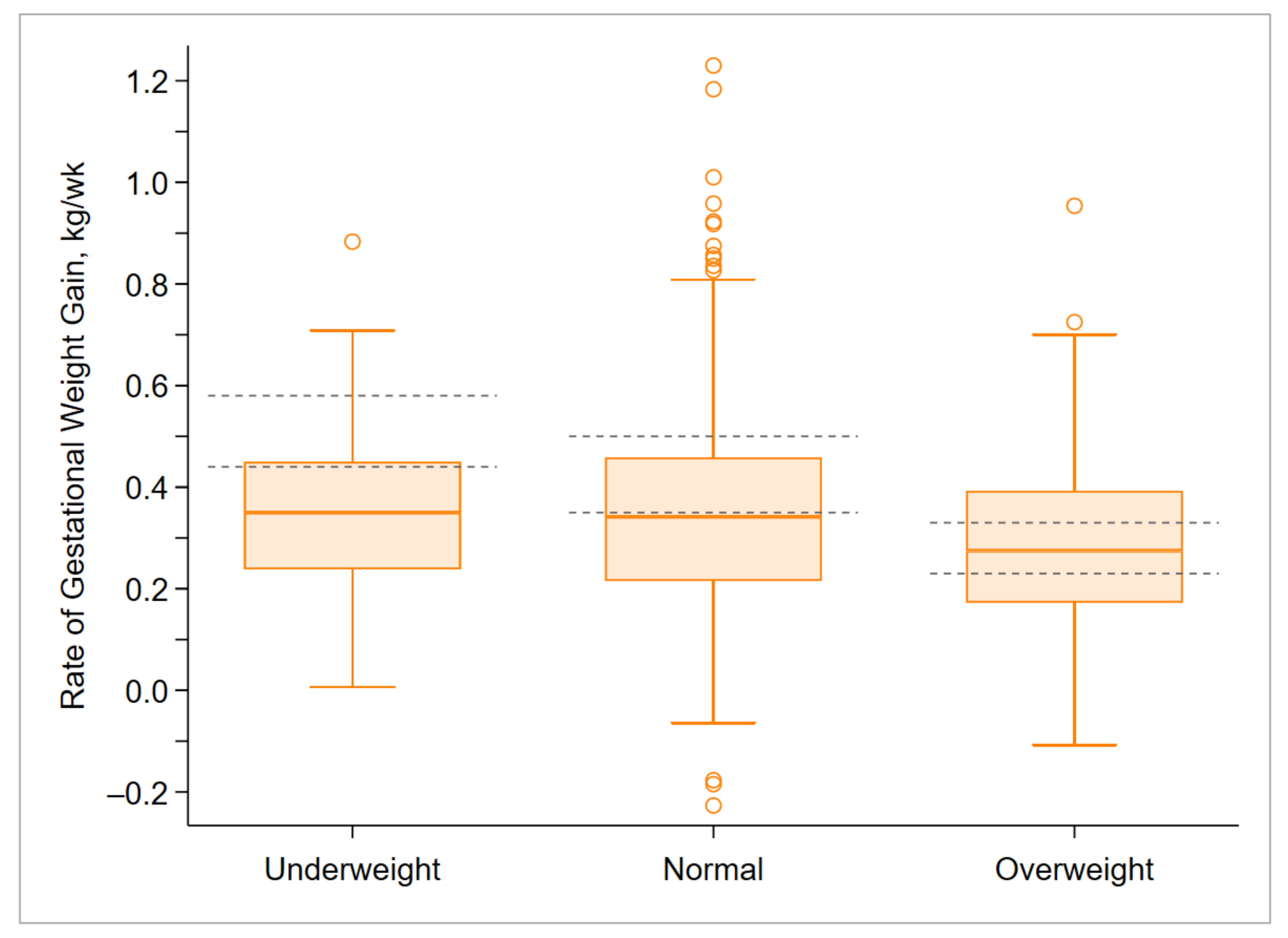
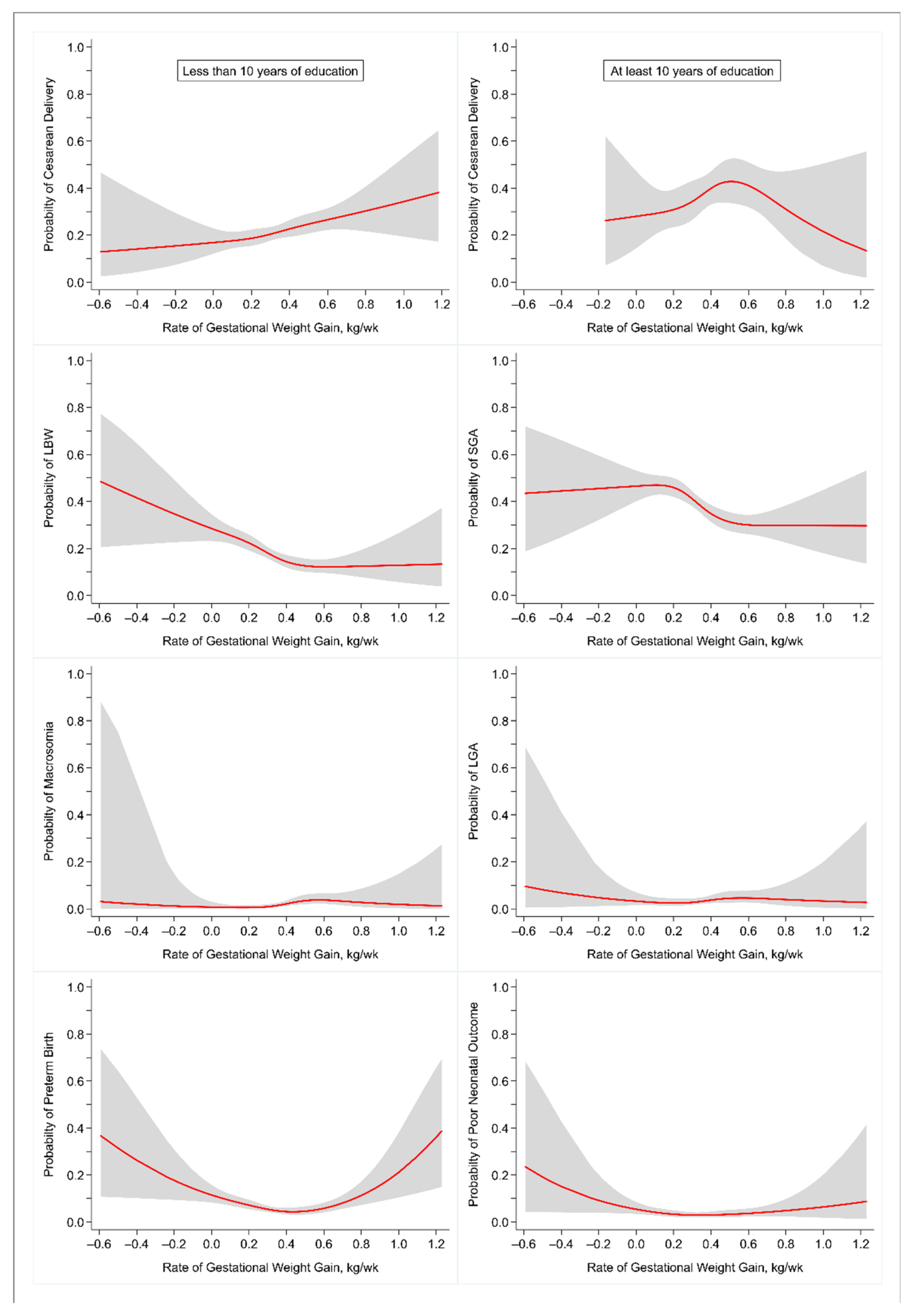
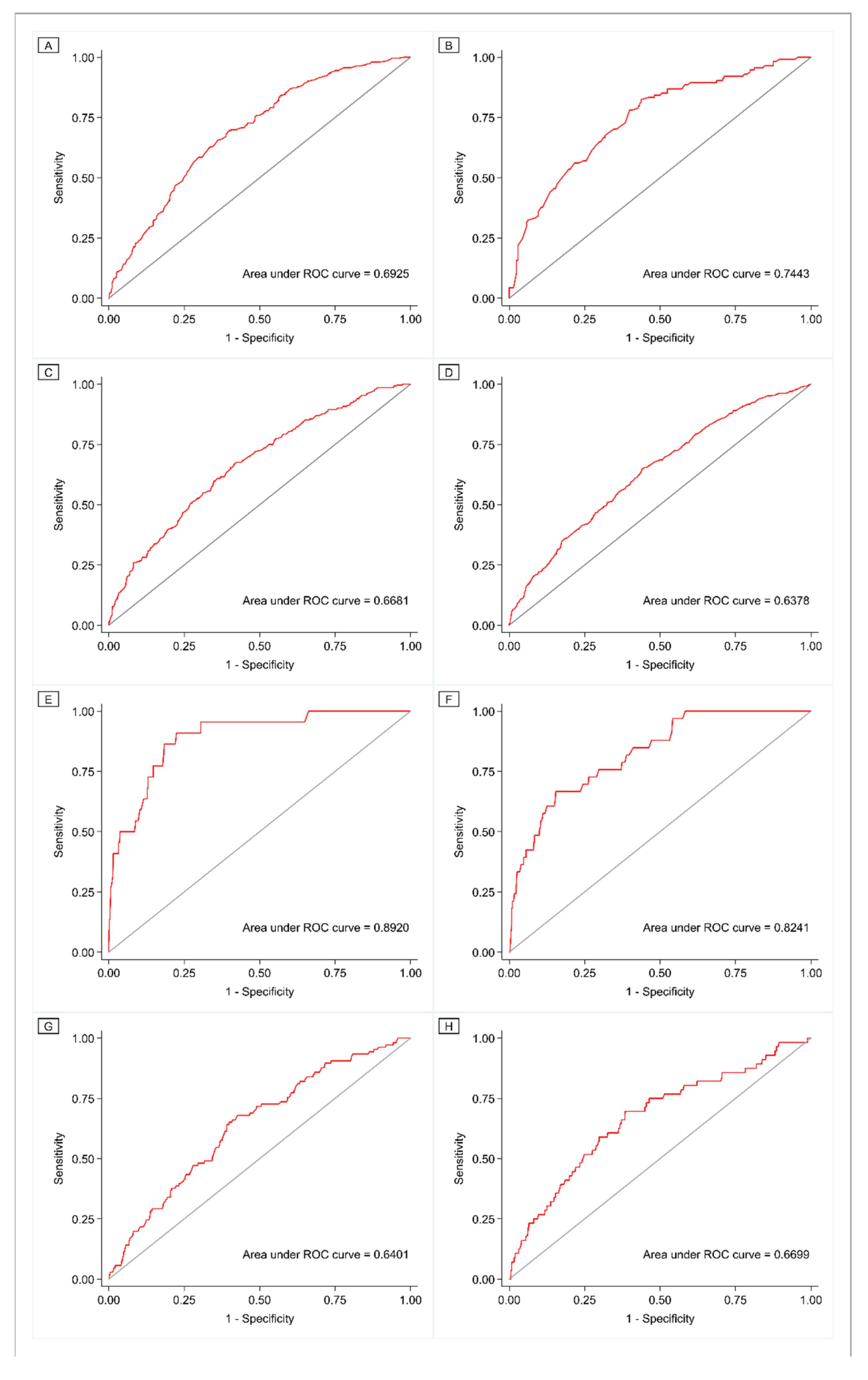
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Goldstein, R.F.; Abell, S.K.; Ranasinha, S.; Misso, M.L.; Boyle, J.A.; Harrison, C.L.; Black, M.H.; Li, N.; Hu, G.; Corrado, F.; et al. Gestational weight gain across continents and ethnicity: Systematic review and meta-analysis of maternal and infant outcomes in more than one million women. BMC Med. 2018, 16, 153. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Wang, M.; Darling, A.M.; Perumal, N.; Liu, E.; Danaei, G.; Fawzi, W.W. Gestational weight gain in low-income and middle-income countries: A modelling analysis using nationally representative data. BMJ Glob. Health 2020, 5, e003423. [Google Scholar] [CrossRef] [PubMed]
- Zhao, R.; Xu, L.; Wu, M.; Huang, S.; Cao, X. Maternal pre-pregnancy body mass index, gestational weight gain influence birth weight. Women Birth 2018, 31, e20–e25. [Google Scholar] [CrossRef] [PubMed]
- Simko, M.; Totka, A.; Vondrova, D.; Samohyl, M.; Jurkovicova, J.; Trnka, M.; Cibulkova, A.; Stofko, J.; Argalasova, L. Maternal Body Mass Index and Gestational Weight Gain and Their Association with Pregnancy Complications and Perinatal Conditions. Int. J. Environ. Res. Public Health 2019, 16, 1751. [Google Scholar] [CrossRef]
- Kominiarek, M.A.; Saade, G.; Mele, L.; Bailit, J.; Reddy, U.M.; Wapner, R.; Varner, M.W.; Thorp, J.M.; Caritis, S.N.; Prasad, M.; et al. Association Between Gestational Weight Gain and Perinatal Outcomes. Obstet. Gynecol. 2018, 132, 875–881. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, X.; Zhou, M.; Juan, J.; Wang, X. Association of prepregnancy body mass index, rate of gestational weight gain with pregnancy outcomes in Chinese urban women. Nutr. Metab. 2019, 16, 1–9. [Google Scholar] [CrossRef]
- Ukah, U.V.; Bayrampour, H.; Sabr, Y.; Razaz, N.; Chan, W.-S.; Lim, K.I.; Lisonkova, S. Association between gestational weight gain and severe adverse birth outcomes in Washington State, US: A population-based retrospective cohort study, 2004–2013. PLoS Med. 2019, 16, e1003009. [Google Scholar] [CrossRef]
- Durie, D.E.; Thornburg, L.L.; Glantz, J.C. Effect of Second-Trimester and Third-Trimester Rate of Gestational Weight Gain on Maternal and Neonatal Outcomes. Obstet. Gynecol. 2011, 118, 569–575. [Google Scholar] [CrossRef]
- Institute of Medicine. Weight Gain during Pregnancy: Reexamining the Guidelines; National Academies Press: Washington, DC, USA, 2009. [Google Scholar]
- Hasan, S.M.T.; Khan, A.; Ahmed, T. Inadequate maternal weight gain in the third trimester increases the risk of intrauterine growth restriction in rural Bangladesh. PLoS ONE 2019, 14, e0212116. [Google Scholar] [CrossRef]
- Ahmed, T.; Roy, S.K.; Alam, N.; Ahmed, A.M.S.; Ara, G.; Bhuiya, A.U.; El Arifeen, S.; Barkat-e-Khuda; Farida Khatun, U.H.; Harun-ur-Rashid; et al. National Nutrition Programme: Baseline Survey Report; International Centre for Diarrhoeal Disease Research, Bangladesh: Dhaka, Bangladesh, 2005; Available online: http://dspace.icddrb.org/jspui/handle/123456789/4057 (accessed on 12 April 2021).
- Aune, D.; Saugstad, O.D.; Henriksen, T.; Tonstad, S. Maternal Body Mass Index and the Risk of Fetal Death, Stillbirth, and Infant Death. JAMA 2014, 311, 1536–1546. [Google Scholar] [CrossRef]
- Yu, Z.; Han, S.; Zhu, J.; Sun, X.; Ji, C.; Guo, X. Pre-Pregnancy Body Mass Index in Relation to Infant Birth Weight and Offspring Overweight/Obesity: A Systematic Review and Meta-Analysis. PLoS ONE 2013, 8, e61627. [Google Scholar] [CrossRef]
- International Centre for Diarrhoeal Disease Research, Bangladesh. Health and Demographic Surveillance System–Matlab, v. Registration of Health and Demographic Events 2016; Scientific Report No. 138; International Centre for Diarrhoeal Disease Research, Bangladesh: Dhaka, Bangladesh, 2018. [Google Scholar]
- Ahmed, S.I.; Hasan, S.M.T.; Khan, A.; Ahmed, T. Effect of Maternal Exposure to Seasons during the Second and Third Trimesters of Pregnancy on Infant Birth Weight in Rural Bangladesh. Curr. Dev. Nutr. 2020, 4, nzaa016. [Google Scholar] [CrossRef]
- Hasan, S.M.T.; Rahman, S.; Locks, L.M.; Rahman, M.; Hore, S.K.; Saqeeb, K.N.; Khan, A.; Ahmed, T. Magnitude and determinants of inadequate third-trimester weight gain in rural Bangladesh. PLoS ONE 2018, 13, e0196190. [Google Scholar] [CrossRef]
- Abubakari, A.; Kynast-Wolf, G.; Jahn, A. Maternal Determinants of Birth Weight in Northern Ghana. PLoS ONE 2015, 10, e0135641. [Google Scholar] [CrossRef]
- Asefa, F.; Nemomsa, D. Gestational weight gain and its associated factors in Harari Regional State: Institution based cross-sectional study, Eastern Ethiopia. Reprod. Health 2016, 13, 101. [Google Scholar] [CrossRef] [PubMed]
- Weir, C.B.; Jan, A. BMI Classification Percentile and Cut off Points. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- American College of Obstetricians and Gynecologists. ACOG Practice bulletin no. 134: fetal growth restriction. Obstet. Gynecol. 2013, 121, 1122–1133. [Google Scholar] [CrossRef] [PubMed]
- De Onis, M.; Habicht, J.P. Anthropometric reference data for international use: Recommendations from a World Health Organization Expert Committee. Am. J. Clin. Nutr. 1996, 64, 650–658. [Google Scholar] [CrossRef] [PubMed]
- Villar, J.; Ismail, L.C.; Victora, C.G.; Ohuma, E.O.; Bertino, E.; Altman, D.G.; Lambert, A.; Papageorghiou, A.T.; Carvalho, M.; Jaffer, Y.A.; et al. International standards for newborn weight, length, and head circumference by gestational age and sex: The Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet 2014, 384, 857–868. [Google Scholar] [CrossRef]
- Wardlaw, T.; World Health Organization; UNICEF (Eds.) Low Birthweight: Country Regional and Global Estimates; WHO: Geneva, Switzerland, 2004. [Google Scholar]
- Alberico, S.; for the Multicentre Study Group on Mode of Delivery in Friuli Venezia Giulia; Montico, M.; Barresi, V.; Monasta, L.; Businelli, C.; Soini, V.; Erenbourg, A.; Ronfani, L.; Maso, G. The role of gestational diabetes, pre-pregnancy body mass index and gestational weight gain on the risk of newborn macrosomia: Results from a prospective multicentre study. BMC Pregnancy Childbirth 2014, 14, 23. [Google Scholar] [CrossRef]
- World Health Organization. WHO Libr. In Neonatal and Perinatal Mortality: Country, Regional and Global Estimates; WHO: Geneva, Switzerland, 2006. [Google Scholar]
- Liu, Y.; Dai, W.; Dai, X.; Li, Z. Prepregnancy body mass index and gestational weight gain with the outcome of pregnancy: A 13-year study of 292,568 cases in China. Arch. Gynecol. Obstet. 2012, 286, 905–911. [Google Scholar] [CrossRef] [PubMed]
- Olusanya, B.; Solanke, O. Correlates of birth asphyxia using two Apgar score classification methods. Niger. Q. J. Hosp. Med. 2011, 20, 153–161. [Google Scholar]
- Kashyap, H.; Sharma, D.; Gala, A.; Pratap, O.T.; Murki, S. Effect of second trimester and third trimester weight gain on immediate outcomes in neonates born to mothers with gestational diabetes: A retrospective observational study from India. J. Matern. Neonatal Med. 2018, 32, 4133–4138. [Google Scholar] [CrossRef] [PubMed]
- Firth, D. Bias Reduction of Maximum Likelihood Estimates. Biometrika 1993, 80, 27–38. [Google Scholar] [CrossRef]
- LifeCycle Project-Maternal Obesity and Childhood Outcomes Study Group; Voerman, E.; Santos, S.; Inskip, H.; Amiano, P.; Barros, H.; Charles, M.A.; Chatzi, L.; Chrousos, G.P.; Corpeleijn, E.; et al. Association of Gestational Weight Gain With Adverse Maternal and Infant Outcomes. JAMA 2019, 321, 1702–1715. [Google Scholar] [CrossRef]
- Begum, T.; Rahman, A.; Nababan, H.; Hoque, D.M.E.; Khan, A.F.; Ali, T.; Anwar, I. Indications and determinants of caesarean section delivery: Evidence from a population-based study in Matlab, Bangladesh. PLoS ONE 2017, 12, e0188074. [Google Scholar] [CrossRef]
- Sosale, S.; Asaduzzaman, T.M.; Ramachandran, D. Girls’ Education in Bangladesh: A Promising Journey. End Poverty in South Asia. World Bank Blogs. Available online: https://blogs.worldbank.org/endpovertyinsouthasia/girls-education-bangladesh-promising-journey (accessed on 14 April 2021).
- Schurmann, A.T. Review of the Bangladesh female secondary school stipend project using a social exclusion framework. J. Health Popul. Nutr. 2009, 27, 505–517. [Google Scholar] [CrossRef]
- International Centre for Diarrhoeal Disease Research, Bangladesh. Health and Demographic Surveillance System–Matlab, v. Household Socio-Economic Census Dhaka; International Centre for Diarrhoeal Disease Research, Bangladesh: Dhaka, Bangladesh, 2016. [Google Scholar]
- Strauss, R.S.; Dietz, W.H. Low Maternal Weight Gain in the Second or Third Trimester Increases the Risk for Intrauterine Growth Retardation. J. Nutr. 1999, 129, 988–993. [Google Scholar] [CrossRef]
- Toh-Adam, R.; Srisupundit, K.; Tongsong, T. Short stature as an independent risk factor for cephalopelvic disproportion in a country of relatively small-sized mothers. Arch. Gynecol. Obstet. 2012, 285, 1513–1516. [Google Scholar] [CrossRef]
- Vogel, J.P.; Lee, A.C.C.; Souza, J.P. Maternal morbidity and preterm birth in 22 low- and middle-income countries: A secondary analysis of the WHO Global Survey dataset. BMC Pregnancy Childbirth 2014, 14, 56. [Google Scholar] [CrossRef]
- Simas, T.A.M.; Liao, X.; Garrison, A.; Sullivan, G.M.T.; Howard, A.E.; Hardy, J.R. Impact of Updated Institute of Medicine Guidelines on Prepregnancy Body Mass Index Categorization, Gestational Weight Gain Recommendations, and Needed Counseling. J. Women’s Health 2011, 20, 837–844. [Google Scholar] [CrossRef]
- Institute of Medicine. Nutrition during Pregnancy; National Academies Press: Washington, DC, USA, 1990; pp. 1–435. [Google Scholar]
- Dude, A.M.; Grobman, W.; Haas, D.; Mercer, B.M.; Parry, S.; Silver, R.M.; Wapner, R.; Wing, D.; Saade, G.; Reddy, U.; et al. Gestational Weight Gain and Pregnancy Outcomes among Nulliparous Women. Am. J. Perinatol. 2021, 38, 182–190. [Google Scholar] [CrossRef]
- Kac, G.; Arnold, C.D.; Matias, S.L.; Mridha, M.K.; Dewey, K.G. Gestational weight gain and newborn anthropometric outcomes in rural Bangladesh. Matern. Child. Nutr. 2019, 15, e12816. [Google Scholar] [CrossRef]
- Huang, A.; Ji, Z.; Zhao, W.; Hu, H.; Yang, Q.; Chen, D. Rate of gestational weight gain and preterm birth in relation to prepregnancy body mass indices and trimester: A follow-up study in China. Reprod. Health 2016, 13, 1–7. [Google Scholar] [CrossRef]
- Bouvier, D.; Forest, J.-C.; Dion-Buteau, E.; Bernard, N.; Bujold, E.; Pereira, B.; Giguère, Y. Association of Maternal Weight and Gestational Weight Gain with Maternal and Neonate Outcomes: A Prospective Cohort Study. J. Clin. Med. 2019, 8, 2074. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Population Research and Training (NIPORT). Mitra and Associates, and ICF International; Bangladesh Demographic and Health Survey: Dhaka, Bangladesh; Rockville, MA, USA, 2016.
- Begum, T.; Ellis, C.; Sarker, M.; Rostoker, J.-F.; Rahman, A.; Anwar, I.; Reichenbach, L. A qualitative study to explore the attitudes of women and obstetricians towards caesarean delivery in rural Bangladesh. BMC Pregnancy Childbirth 2018, 18, 368. [Google Scholar] [CrossRef] [PubMed]
- Rebelo, F.; Da Rocha, C.M.M.; Cortes, T.; Dutra, C.L.; Kac, G. High cesarean prevalence in a national population-based study in Brazil: The role of private practice. Acta Obstet. Gynecol. Scand. 2010, 89, 903–908. [Google Scholar] [CrossRef]
- Teguete, I.; Traore, Y.; Sissoko, A.; Djire, M.Y.; Thera, A.; Dolo, T.; Mounkoro, M.; Traore, M.; Dolo, A. Determining Factors of Cesarean Delivery Trends in Developing Countries: Lessons from Point G National Hospital (Bamako-Mali); INTECH Open Access Publisher: Rijeka, Croatia, 2012. [Google Scholar]
- Hussain, A.M.Z.; Hussain, A.T. National Low Birth Weight Survey (NLBWS) Bangladesh, Report; Institute of Public Health Nutrition (IPHN): Dhaka, Bangladesh, 2017.
- WHO. WHO Guidelines Approved by the Guidelines Review Committee. In WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Schneeweiss, S.; Avorn, J. A review of uses of health care utilization databases for epidemiologic research on therapeutics. J. Clin. Epidemiol. 2005, 58, 323–337. [Google Scholar] [CrossRef] [PubMed]
- Bohensky, M.; Jolley, D.; Sundararajan, V.; Evans, S.; Pilcher, D.V.; Scott, I.; Brand, C. Data Linkage: A powerful research tool with potential problems. BMC Health Serv. Res. 2010, 10, 346. [Google Scholar] [CrossRef]
- Thomas, D.M.; Oken, E.; Rifas-Shiman, S.L.; Rojo, M.T.; Just, A.; Svensson, K.; Deierlein, A.L.; Chandler-Laney, P.C.; Miller, R.C.; McNamara, C.; et al. Do Women Know Their Prepregnancy Weight? Obesity 2019, 27, 1161–1167. [Google Scholar] [CrossRef]
| Characteristics | n (%) |
|---|---|
| Maternal characteristics | |
| Age | |
| ≤19 years | 319 (20.3) |
| 20–34 years | 1149 (73.2) |
| ≥35 years | 101 (6.4) |
| Height, ≤145 cm | 235 (15.0) |
| Prepregnancy BMI | |
| Underweight (<18.5 kg/m2) | 238 (15.2) |
| Normal (18.5–24.9 kg/m2) | 1128 (71.9) |
| Overweight (25–29.9 kg/m2) | 185 (11.8) |
| Obese (≥30 kg/m2) | 18 (1.2) |
| Parity | |
| Nulliparous | 660 (42.1) |
| 1 previous birth | 436 (27.8) |
| 2 previous births | 307 (19.6) |
| ≥3 previous birth | 166 (10.6) |
| Previous cesarean delivery | 14 (0.9) |
| Education, years | |
| ≤5 | 367 (23.4) |
| 6–9 | 878 (56.0) |
| ≥10 | 324 (20.7) |
| Wealth quintile | |
| Lowest | 249 (15.9) |
| Second | 269 (17.1) |
| Middle | 303 (19.3) |
| Fourth | 327 (20.8) |
| Highest | 421 (26.8) |
| Rate of weight gain | |
| Inadequate | 879 (56.0) |
| Optimal | 378 (24.1) |
| Excessive | 312 (19.9) |
| Preterm labor | 106 (6.8) |
| Cesarean delivery | 381 (24.3) |
| Offspring characteristics | |
| Sex, Female | 773 (49.3) |
| LBW | 284 (18.1) |
| SGA | 602 (38.4) |
| Macrosomia | 22 (1.4) |
| LGA | 33 (2.1) |
| Severe neonatal morbidity | 42 (2.7) |
| Neonatal death | 19 (1.2) |
| Poor neonatal outcome | 56 (3.6) |
| Adverse Outcome | OR (95% CI) | p | AOR (95% CI) 1 | p |
|---|---|---|---|---|
| Maternal | ||||
| Cesarean delivery in women who received less than 10 years of education | 0.9 (0.6, 1.3) | 0.502 | 0.9 (0.6, 1.3) | 0.452 |
| Cesarean delivery in women who completed at least 10 years of education | 0.6 (0.3, 1.1) | 0.080 | 0.6 (0.3, 1.1) | 0.105 |
| Fetal | ||||
| LBW | 1.6 (1.1, 2.2) | 0.006 | 1.4 (1.03, 2.0) | 0.034 |
| SGA | 1.5 (1.2, 1.9) | 0.002 | 1.3 (1.04, 1.7) | 0.023 |
| Macrosomia | 0.5 (0.1, 2.1) | 0.314 | 0.6 (0.1, 2.5) | 0.450 |
| LGA | 3.0 (0.8, 11.4) | 0.116 | 3.2 (0.8, 12.5) | 0.094 |
| Preterm birth | 2.1 (1.2, 3.7) | 0.013 | 2.0 (1.1, 3.6) | 0.017 |
| Neonatal | ||||
| Poor neonatal outcome | 2.5 (1.1, 5.8) | 0.035 | 2.4 (1.03, 5.6) | 0.043 |
| Adverse Outcome | OR (95% CI) | p | AOR (95% CI) 1 | p |
|---|---|---|---|---|
| Maternal | ||||
| Cesarean delivery in women who received less than 10 years of education | 1.8 (1.2, 2.8) | 0.003 | 1.7 (1.1, 2.6) | 0.023 |
| Cesarean delivery in women who completed at least 10 years of education | 1.3 (0.7, 2.4) | 0.395 | 0.9 (0.5, 1.8) | 0.753 |
| Fetal | ||||
| LBW | 0.6 (0.4, 1.02) | 0.060 | 0.7 (0.4, 1.2) | 0.183 |
| SGA | 0.7 (0.5, 0.96) | 0.029 | 0.8 (0.5, 1.1) | 0.110 |
| Macrosomia | 5.6 (1.8, 18.1) | 0.004 | 3.3 (1.0, 10.9) | 0.051 |
| LGA | 7.9 (2.1, 30.3) | 0.002 | 5.9 (1.5, 23.1) | 0.010 |
| Preterm birth | 1.8 (0.9, 3.6) | 0.077 | 2.2 (1.1, 4.4) | 0.023 |
| Neonatal | ||||
| Poor neonatal outcome | 2.8 (1.1, 7.1) | 0.032 | 2.7 (1.04, 7.0) | 0.041 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hasan, S.M.T.; Khan, M.A.; Ahmed, T. Institute of Medicine Recommendations on the Rate of Gestational Weight Gain and Perinatal Outcomes in Rural Bangladesh. Int. J. Environ. Res. Public Health 2021, 18, 6519. https://doi.org/10.3390/ijerph18126519
Hasan SMT, Khan MA, Ahmed T. Institute of Medicine Recommendations on the Rate of Gestational Weight Gain and Perinatal Outcomes in Rural Bangladesh. International Journal of Environmental Research and Public Health. 2021; 18(12):6519. https://doi.org/10.3390/ijerph18126519
Chicago/Turabian StyleHasan, S. M. Tafsir, Md Alfazal Khan, and Tahmeed Ahmed. 2021. "Institute of Medicine Recommendations on the Rate of Gestational Weight Gain and Perinatal Outcomes in Rural Bangladesh" International Journal of Environmental Research and Public Health 18, no. 12: 6519. https://doi.org/10.3390/ijerph18126519
APA StyleHasan, S. M. T., Khan, M. A., & Ahmed, T. (2021). Institute of Medicine Recommendations on the Rate of Gestational Weight Gain and Perinatal Outcomes in Rural Bangladesh. International Journal of Environmental Research and Public Health, 18(12), 6519. https://doi.org/10.3390/ijerph18126519






