Virtual Experience of Perioperative Patients: Walking in the Patients’ Shoes Using Virtual Reality and Blended Learning
Abstract
1. Introduction
2. Methods
2.1. Research Design
2.1.1. Research Participants and Researcher Preparation
2.1.2. VR Blended Learning Program
2.1.3. Research Procedure and Data Collection
2.2. Data Analysis
2.3. Research Rigor
2.4. Ethical Considerations
3. Results
3.1. Categories and Theme Clusters
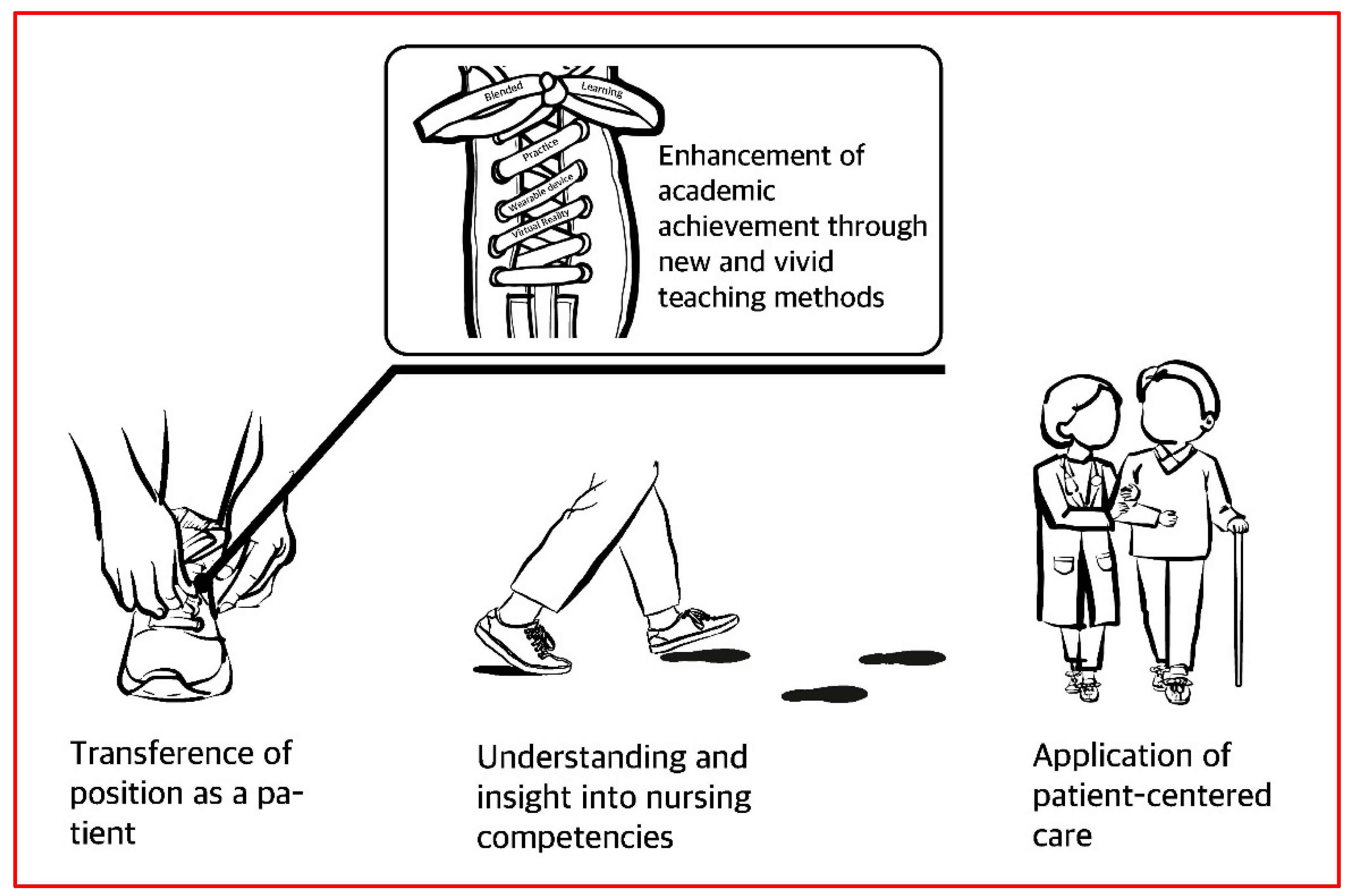
3.1.1. Category 1: Transference into the Position of a Patient Who Receives Nursing Care
Being Placed in a Passive Position
“When I was being transferred, lying on the stretcher, I felt like I could not even move, though I was not actually sick … I felt like I was perhaps on my way to death, on my way to the grave. It was scary. I felt helpless.”
“I was looking at the ceiling with my arms out, and I felt I could not do anything … There was nothing that could be done (during urinary catheterization) … Even when I am watching the animation (VR) I am (really) looking at the ceiling … (I felt) pressure(d) from the feeling of being surrounded.”
Facing the Limits of Communication
“So, for me, I could not say some things to the medical staff when I was the patient. I felt that it could make the atmosphere harsh … because I am speaking with that person one on one. It made me think that if I say anything along the lines of “This does not sound right”, then they may not be so nice to me.”
“When I was being transferred on the stretcher, I felt conscious of (my own) weight, and I felt that if I said that whenever they moved me (made me uncomfortable), then they may not like me, and (they might) intentionally not do (the) things they should be doing for me.”
3.1.2. Category 2: Understanding of and Insights into Nursing Competencies
Thinking about Developing and Improving One’s Competency as a Nurse
“During procedures, I was always busy, but being in the patient’s position, I felt quite strongly that even just saying a (kind) word could make them much less anxious.”
“It (was an opportunity for me to realize that perioperative patients are family members. The experience of being a patient encouraged me to think quite frequently about the term “responsibility.”
“If I consider the patients as my family, would I make a mistake? Wouldn’t I double check? That is what I was thinking. I want to provide better care.”
Recognizing the Importance of Interacting with Patients
“Honestly, I felt very different from when I (was the one doing) the procedures. I thought that I could be a politer nurse, if I remember that the patient is also a human being, like me.”
“I guess it is like respecting (the patient) as a human being. I never thought about (being) compassionate, but through this experience, I realized that patients need compassion, and it helped me consider them, once again, as human beings.”
“I thought, “Maybe patients need to know that they have right to ask questions and things like that.” That is because they are all patients for the first time, they are undergoing procedures for the first time, so they would not be able to speak properly due to fear and anxiety.”
3.1.3. Category 3: Enhancement of Academic Achievement through New and Vivid Teaching Methods
Learning Vividly through Experience
“Oh, the operation theater (in VR) was darker than I thought. I thought it would be brighter.”
“(The experience) made me realize that patients feel very uncomfortable in (ways) I had never thought about. I had to go to the toilet with an IV pole … and getting dressed was also uncomfortable … I felt a lot of (unexpected) discomfort (while doing) things I had never (thought much about before).”
“The hips should be pulled forward as far as possible. That posture was very difficult. It was so embarrassing when I had to wear the equipment. And when they inserted the IV, it really hurt.”
Engaging in a New Type of Participatory Learning
“People were crowded on both side of the chairs (in VR)… There were many people on my way to the operation theater, and I felt I would become more anxious … That was (the) most memorable. Dramas and movies only depict scenes during surgery; (they don’t) quite show what the theater looks like, but I was able to see 360 degrees around, and there were things like a kidney basin and gauze with blood on it. I saw timers with anesthesia time and operation time. I also saw medical devices. So, it was interesting.”
“I thought there would probably be things like the surgical lights or Bovies, which are the basic items, but I never knew that they check the time. (I learned that during) the VR, and it felt like the timer was quite an important device, so that was interesting.”
3.1.4. Category 4: Application of Patient-Centered Care
Designing Nursing Knowledge
“I came to think that (understanding the emotions involved) in the patient’s experience is very important for medical staff. Things like posture were very difficult to rectify. I think it would be easier for the patient and the staff if there is (a) marking to show where to enter. Maybe something like, “Please lower your backside until the red point.”
“(Since) the patients I care for can be (either) males or females, it was an opportunity for me to make a sensitive consideration, as I gained experience and (thought) about those things in advance.”
“I felt worse than I expected when I was being moved onto the bed. I had severe nausea when I was being moved and when they were using the bed sheet (because) the staff could not control their strength very well.”
“So, I thought that during urinary catheterization, (rather than undressing), it would be better to cover everything (and) just use the insertion point … so that’s the only part that’s visible to cover and let it be seen or cover it to help the patient feel better.”
“I think there must be medical staff to (attend to) the (patient’s) psychological aspects.”
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Epstein, R.M.; Street, R.L. The values and value of patient-centered care. Ann. Fam. Med. 2011, 9, 100–103. [Google Scholar] [CrossRef] [PubMed]
- Epstein, R.M.; Fiscella, K.; Lesser, C.S.; Stange, K.C. Why the nation needs a policy push on patient-centered health care. Health Aff. 2010, 29, 1489–1495. [Google Scholar] [CrossRef] [PubMed]
- Do, Y.K.; Kim, J.E.; Lee, J.Y.; Lee, H.Y.; Cho, M.W.; Kim, E.N.; Ok, M.S. Research on Development of Patient-Centered Evaluation Model; Report No.: G000E70-2015-87; Health Insurance Review & Assessment Service: Seoul, Korea, 2015. [Google Scholar]
- Seo, S.Y. Introduction of patient experience evaluation for measuring patient-centeredness. Policy Trend Health Insur. Rev. Assess. Serv. 2017, 11, 25–28. [Google Scholar]
- Wolf, P.h.D.C.; Jason, A. Defining patient experience. Patient Exp. J. 2014, 1, 7–19. [Google Scholar]
- Ahmed, F.; Burt, J.; Roland, M. Measuring patient experience: Concepts and methods. Patient-Patient-Cent. Outcomes Res. 2014, 7, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Kim, U.-N. Reporting Heterogeneity in Patient Experience: Applying the Anchoring Vignette Method; The Graduate School, Seoul National University: Seoul, Korea, 2015. [Google Scholar]
- Lee, N.K. A Study on the Developmental Implications of Clinical Practice through the Patient Experience narratives of Nurses. Asia Pac. J. Multimed. Serv. Converg. Art Humanit. Sociol. 2019, 9, 675–688. [Google Scholar]
- Song, J.; Kim, M. Study on clinical education for nursing in hospitals in Korea. J. Korean Acad. Soc. Nurs. Educ. 2013, 19, 251–264. [Google Scholar] [CrossRef]
- Sanchez-Vives, M.V.; Slater, M. From presence to consciousness through virtual reality. Nat. Rev. Neurosci. 2005, 6, 332–339. [Google Scholar] [CrossRef]
- Consorti, F.; Mancuso, R.; Nocioni, M.; Piccolo, A. Efficacy of virtual patients in medical education: A meta-analysis of randomized studies. Comput. Educ. 2012, 59, 1001–1008. [Google Scholar] [CrossRef]
- Pottle, J. Virtual reality and the transformation of medical education. Future Healthc. J. 2019, 6, 181. [Google Scholar] [CrossRef]
- Kim, I.-O.; Yeom, G.J.; Kim, M.J. Development and effects of a sex education program with blended learning for university students. Child Health Nurs. Res. 2018, 24, 443–453. [Google Scholar] [CrossRef]
- Kim, M.; Kim, S.; Lee, W.S. Effects of a virtual reality simulation and a blended simulation of care for pediatric patient with asthma. Child Health Nurs. Res. 2019, 25, 496–506. [Google Scholar] [CrossRef]
- Chen, F.-Q.; Leng, Y.-F.; Ge, J.-F.; Wang, D.-W.; Li, C.; Chen, B.; Sun, Z.-L. Effectiveness of Virtual Reality in Nursing Education: Meta-Analysis. J. Med. Internet Res. 2020, 22, e18290. [Google Scholar] [CrossRef] [PubMed]
- Park, E.-H.; Hwang, S.-Y. Effects of a web-based learning contents in operating room nursing for nursing students. J. Korea Contents Assoc. 2011, 11, 384–394. [Google Scholar]
- Kang, Y.-K.; Kim, K.-M.; Kim, Y.-Y.; Park, H.-O.; Seo, K.-H.; Song, S.; Lee, H.-S.; Cho, E.-Y. Analysis of Anesthesia and Recovery Room Nurses’s Activities. J. Korean Acad. Nurs. Adm. 2006, 12, 63–75. [Google Scholar]
- Kim, J.-S.; Kim, M.-S.; Hwang, S.-K. Development of an e-learning education program for preventing nursing errors and adverse events of operating room nurses. Korean J. Adult Nurs. 2005, 17, 697–708. [Google Scholar]
- Koh, D.-H. Participation of New Nurses in Simulation-Based Educaiton; The Graduate School of Nursing and Health Professons, Chung-Ang University: Seoul, Korea, 2017. [Google Scholar]
- Lee, J.-H.; Kim, S.-S.; Yeo, K.-S.; Cho, S.-J.; Kim, H.-L. Experiences among undergraduate nursing students on high-fidelity simulation education: A focus group study. J. Korean Acad. Soc. Nurs. Educ. 2009, 15, 183–193. [Google Scholar] [CrossRef]
- Deming, W.E. Sample Design in Business Research; John Wiley & Sons: New York, NY, USA, 1990. [Google Scholar]
- Colaizzi, P.F. Psychological Research as the Phenomenologist Views It. In Existential Phenomenological Alternatives for Psychology; Valle, R.S., King, M., Eds.; Open University Press: New York, NY, USA, 1978. [Google Scholar]
- Lincoln, Y.S.; Guba, E.G. But is it rigorous? Trustworthiness and authenticity in naturalistic evaluation. New Dir. Program Eval. 1986, 1986, 73–84. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Song, M.-K.; Hong, S.-U. A survey of students’ satisfaction on participation learning using role-play in clerkship. J. Korean Med. Ophthalmol. Otolaryngol. Dermatol. 2012, 25, 65–77. [Google Scholar] [CrossRef]
- Jenkinson, C.; Coulter, A.; Bruster, S. The Picker Patient Experience Questionnaire: Development and validation using data from in-patient surveys in five countries. Int. J. Qual. Health Care 2002, 14, 353–358. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.H.; Kim, N.H. Relationships among nursing professionalism, nurse image, and core elements of nursing professionalism that nursing students perceive. J. Korean Acad. Soc. Nurs. Educ. 2014, 20, 548–557. [Google Scholar] [CrossRef][Green Version]
- Kang, S.; Kim, C.; Lee, H.S.; Nam, J.-W.; Park, M.S. Integrative Review on Nursing education Adopting Virtual Reality Convergence Simulation. J. Converg. Inf. Technol. 2020, 10, 60–74. [Google Scholar]
- Dyer, E.; Swartzlander, B.J.; Gugliucci, M.R. Using virtual reality in medical education to teach empathy. J. Med. Libr. Assoc. JMLA 2018, 106, 498. [Google Scholar] [CrossRef]
- Woon, A.P.N.; Mok, W.Q.; Chieng, Y.J.S.; Zhang, H.M.; Ramos, P.; Mustadi, H.B.; Lau, Y. Effectiveness of virtual reality training in improving knowledge among nursing students: A systematic review, meta-analysis and meta-regression. Nurse Educ. Today 2021, 98, 104655. [Google Scholar] [CrossRef] [PubMed]
- Grilo, A.M.; Santos, M.C.; Rita, J.S.; Gomes, A.I. Assessment of nursing students and nurses’ orientation towards patient-centeredness. Nurse Educ. Today 2014, 34, 35–39. [Google Scholar] [CrossRef]
- Rye, E.K. Merlot-Ponty’s Concept of Sensory Experience Phenomenology and Contemporary Philosoph; Sechang-Media: Seoul, Korea, 2003; pp. 5–114. [Google Scholar]
| Category | Theme Cluster | Theme |
|---|---|---|
| Transference of position as a patient | Placed in a passive position | Complains of helplessness and anxiety |
| Becomes sensitive to even minor stimuli | ||
| Feels shame and embarrassment | ||
| Experiences pressure | ||
| Facing the limits of communication | Wants the minimum amount of consideration as the patient | |
| Experiences a feeling of dejection due to one-way and limited communication | ||
| Understanding and insight into nursing competencies | Thinking of developing and improving competency as a nurse | Comes to understand and pursue evidence-based nursing as a nurse |
| Thinks about nurses’ attitudes | ||
| Is determined to become a better nurse | ||
| Recognizing the importance of interacting with their patients | Experiences what it is like to be a patient | |
| Comes to view the patients as human beings who need care | ||
| Thinks seriously about the interaction between the patient and medical staff | ||
| Enhancement of academic achievement through new and vivid teaching methods | Learning vividly through experience | Learns the surgery process realistically rather than abstractly |
| Faces unexpected an nursing field in a new and powerful way | ||
| Learning is motivated, and curiosity is spiked | ||
| Engaging in a new type of participatory learning | Experiences VR | |
| Experiences VR through a wearable device | ||
| Application of patient-centered care | Designing nursing knowledge | Is keenly aware of the need for patient experience |
| Thinks about gender-perspective sensitivity | ||
| Comes up with creative and effective nursing service ideas | ||
| Devises a plan for patient-centered care |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.-Y.; Lee, J.-H.; Lee, E.-H. Virtual Experience of Perioperative Patients: Walking in the Patients’ Shoes Using Virtual Reality and Blended Learning. Int. J. Environ. Res. Public Health 2021, 18, 6457. https://doi.org/10.3390/ijerph18126457
Kim H-Y, Lee J-H, Lee E-H. Virtual Experience of Perioperative Patients: Walking in the Patients’ Shoes Using Virtual Reality and Blended Learning. International Journal of Environmental Research and Public Health. 2021; 18(12):6457. https://doi.org/10.3390/ijerph18126457
Chicago/Turabian StyleKim, Hyeon-Young, Ji-Hye Lee, and Eun-Hye Lee. 2021. "Virtual Experience of Perioperative Patients: Walking in the Patients’ Shoes Using Virtual Reality and Blended Learning" International Journal of Environmental Research and Public Health 18, no. 12: 6457. https://doi.org/10.3390/ijerph18126457
APA StyleKim, H.-Y., Lee, J.-H., & Lee, E.-H. (2021). Virtual Experience of Perioperative Patients: Walking in the Patients’ Shoes Using Virtual Reality and Blended Learning. International Journal of Environmental Research and Public Health, 18(12), 6457. https://doi.org/10.3390/ijerph18126457







