MoSIoT: Modeling and Simulating IoT Healthcare-Monitoring Systems for People with Disabilities
Abstract
:1. Introduction
2. Background
2.1. The Existing HMS Solutions for People with Disabilities
2.2. Necessity and Existing IoT Simulators
2.3. Model-Driven Engineering for Developing IoT Systems
- Specifying the system model, in which the heterogeneous elements are precisely identified, defining an automation process to obtain the final solution;
- The application’s complexity to be addressed;
- Facilitating communication between the application stakeholders.
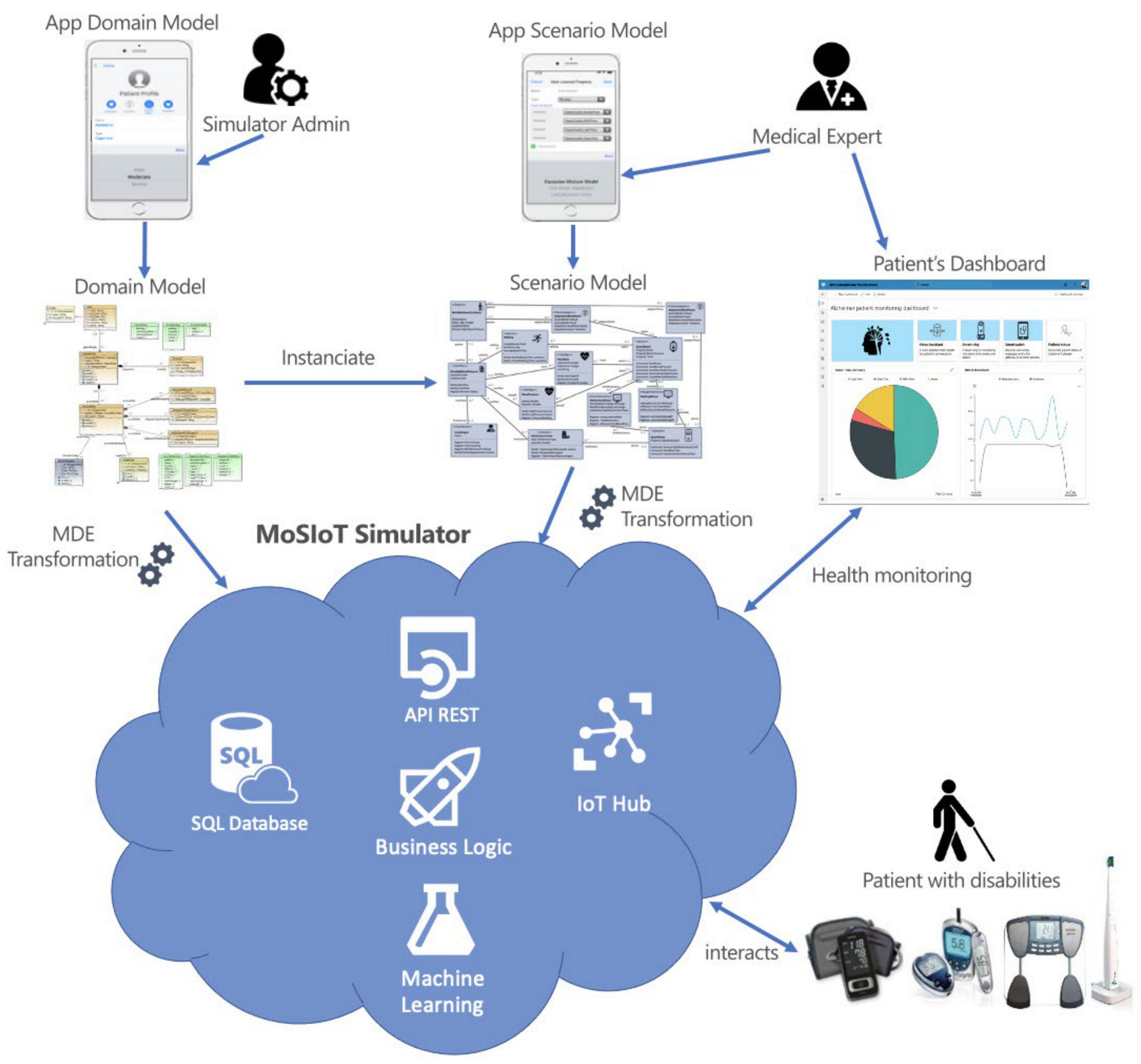
3. MoSIoT: A MDE Framework for IoT Healthcare-Monitoring Systems for People with Disabilities
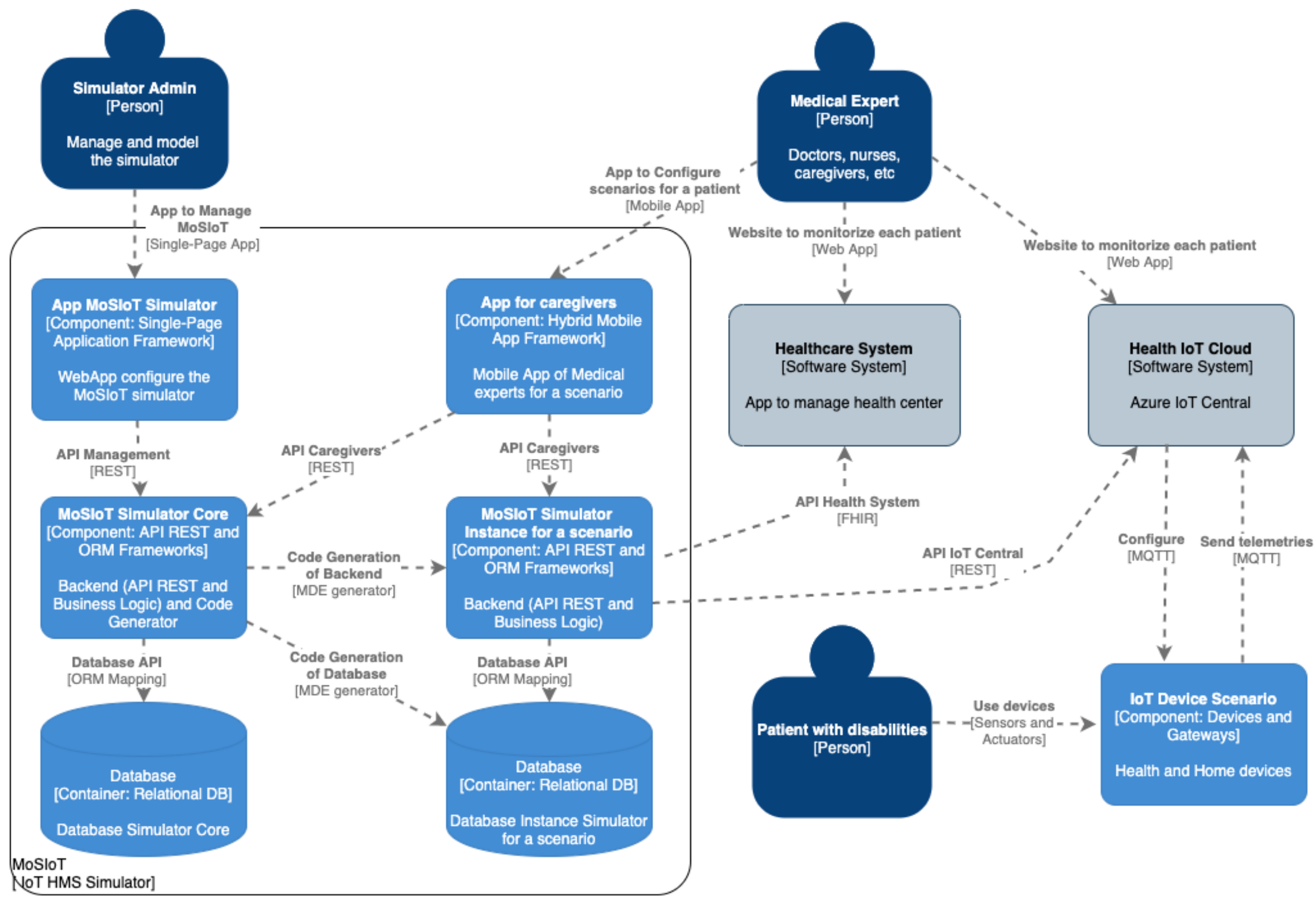
3.1. The Software Architecture of the MoSIoT Framework
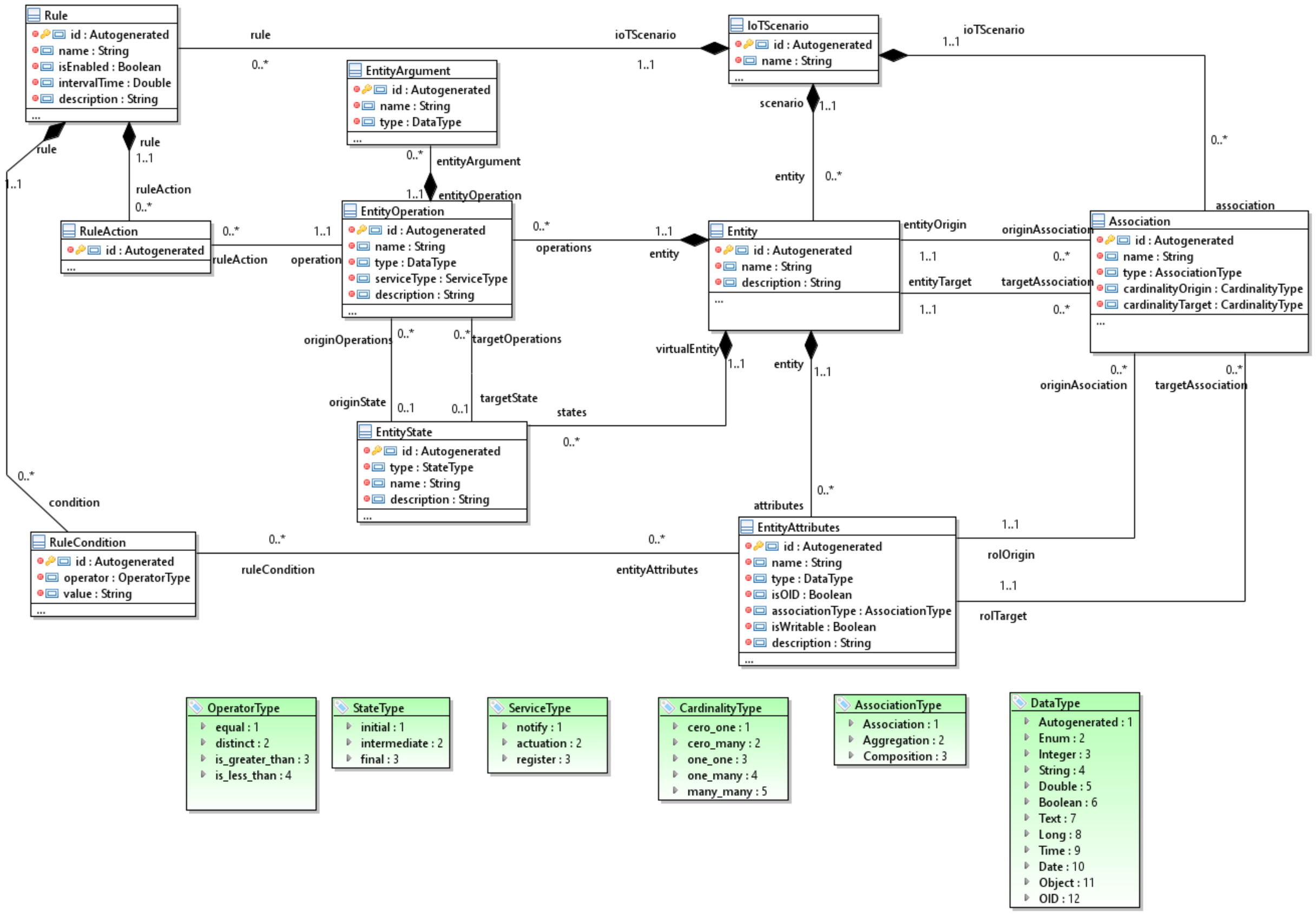
- Entity operations that the simulator has enriched with a typology to improve the generation;
- The state machine models to represent the internal states of complex entities;
- Trigger–action programming to define a set of recipes that configure the behavior of the scenario.
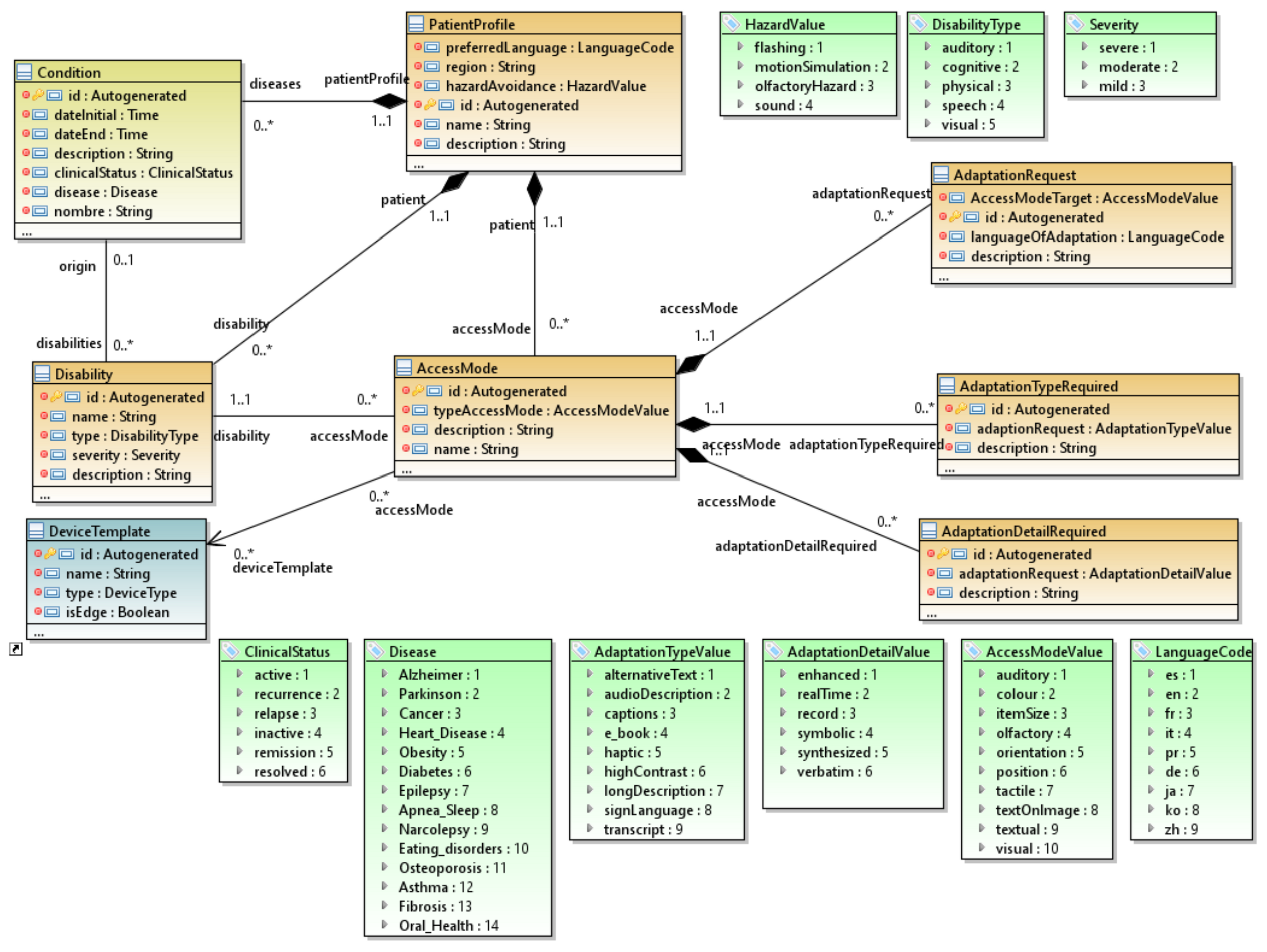
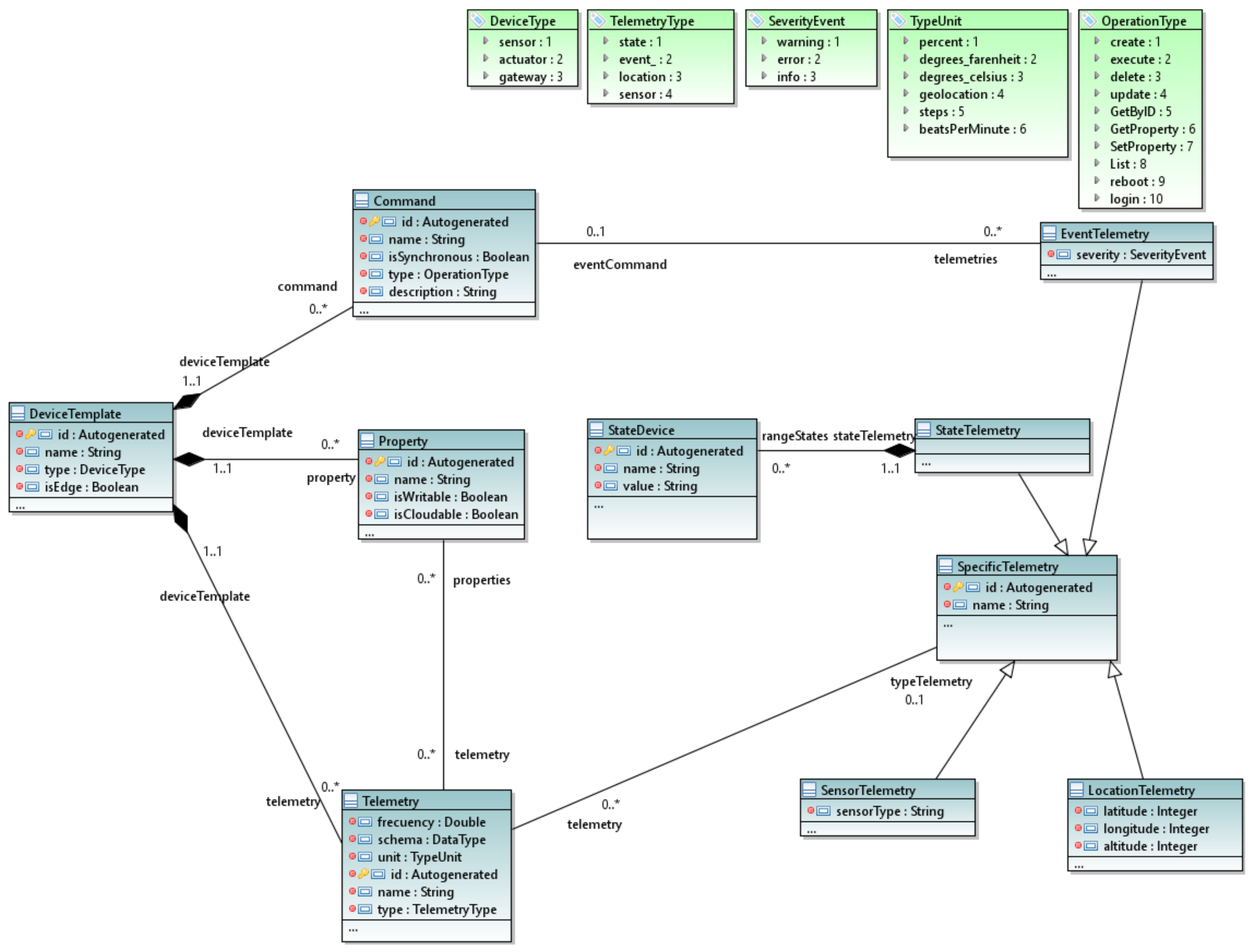
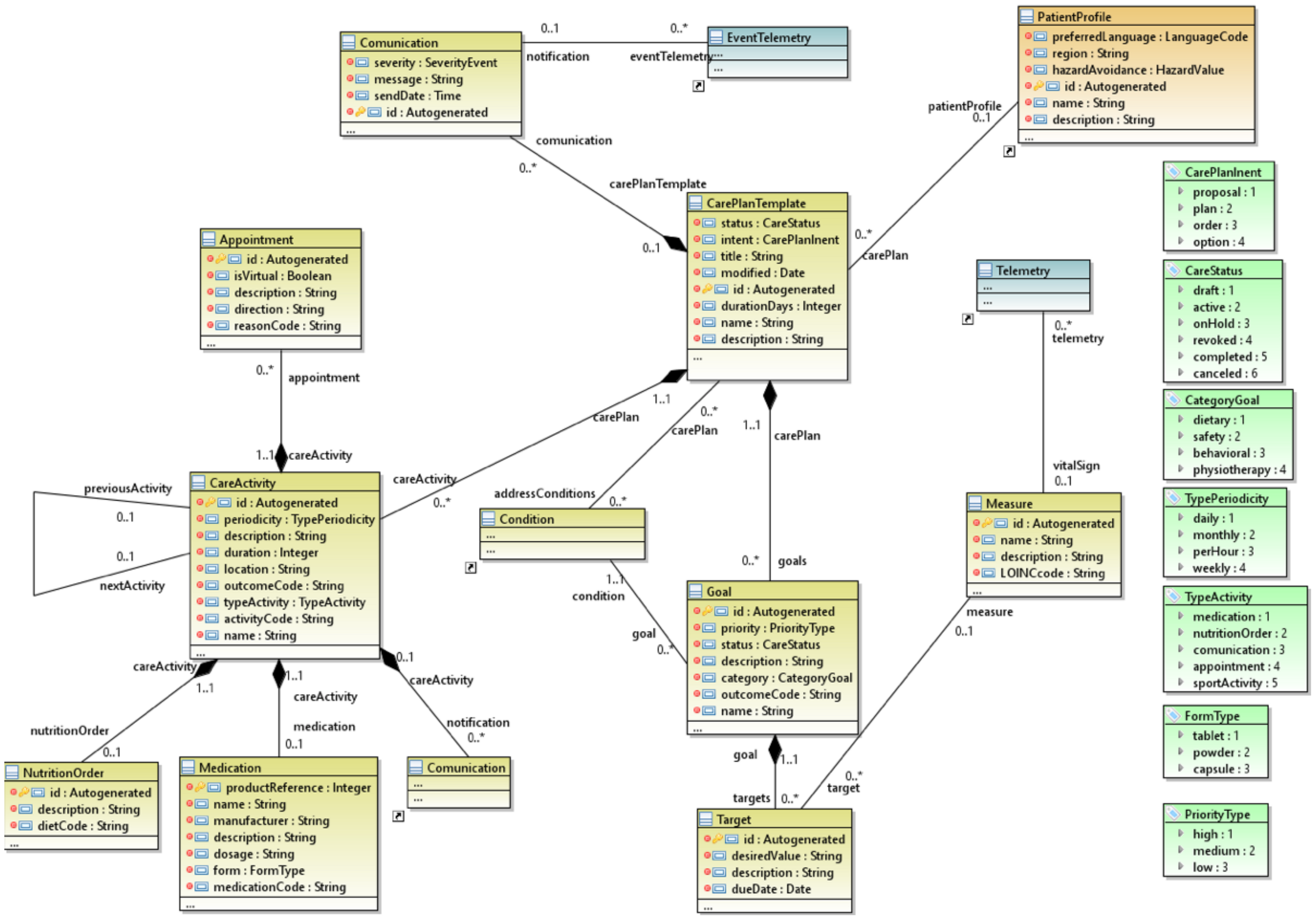
3.2. The MoSIoT Domain Model
- The patient profile package, which allows for the definition of the adaptation profiles of patients based on the types of disabilities and conditions;
- The device package, which defines the device templates or types of devices used in these systems with their characteristics and the types of telemetries;
- The healthcare package, which proposes different care plan templates with activities, goals, and communications for patients with specific conditions and disability types.
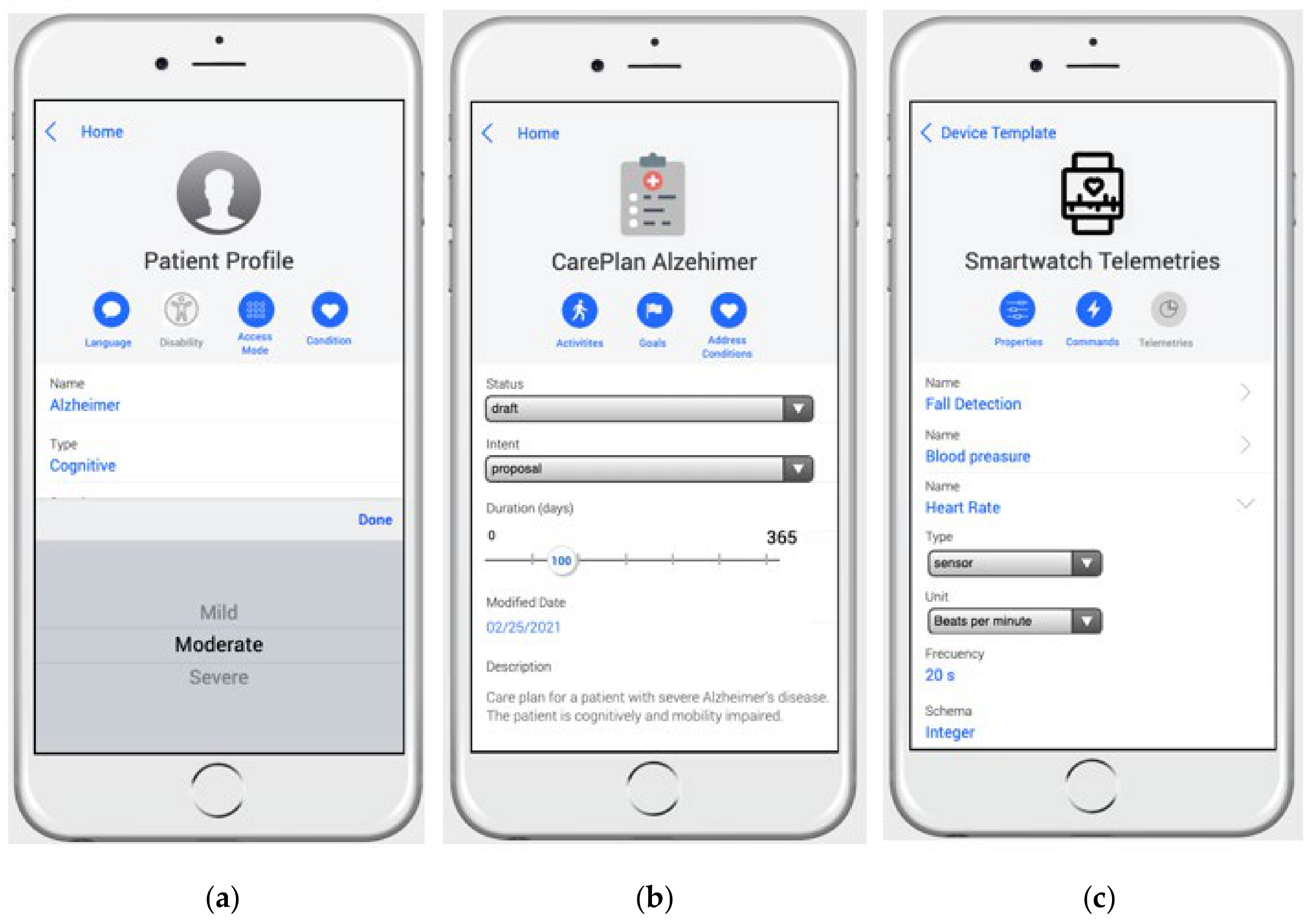
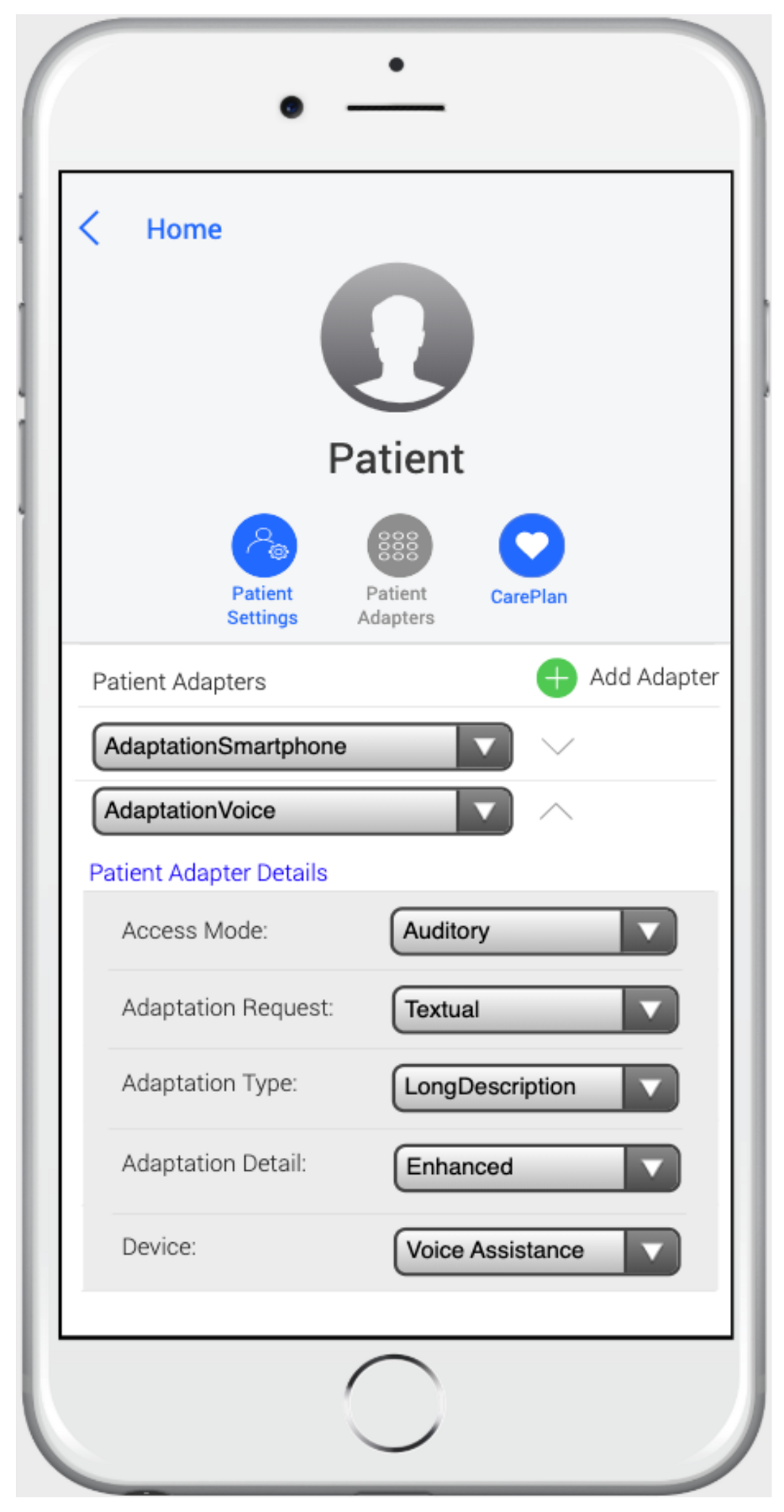
3.2.1. The Patient Profile Package
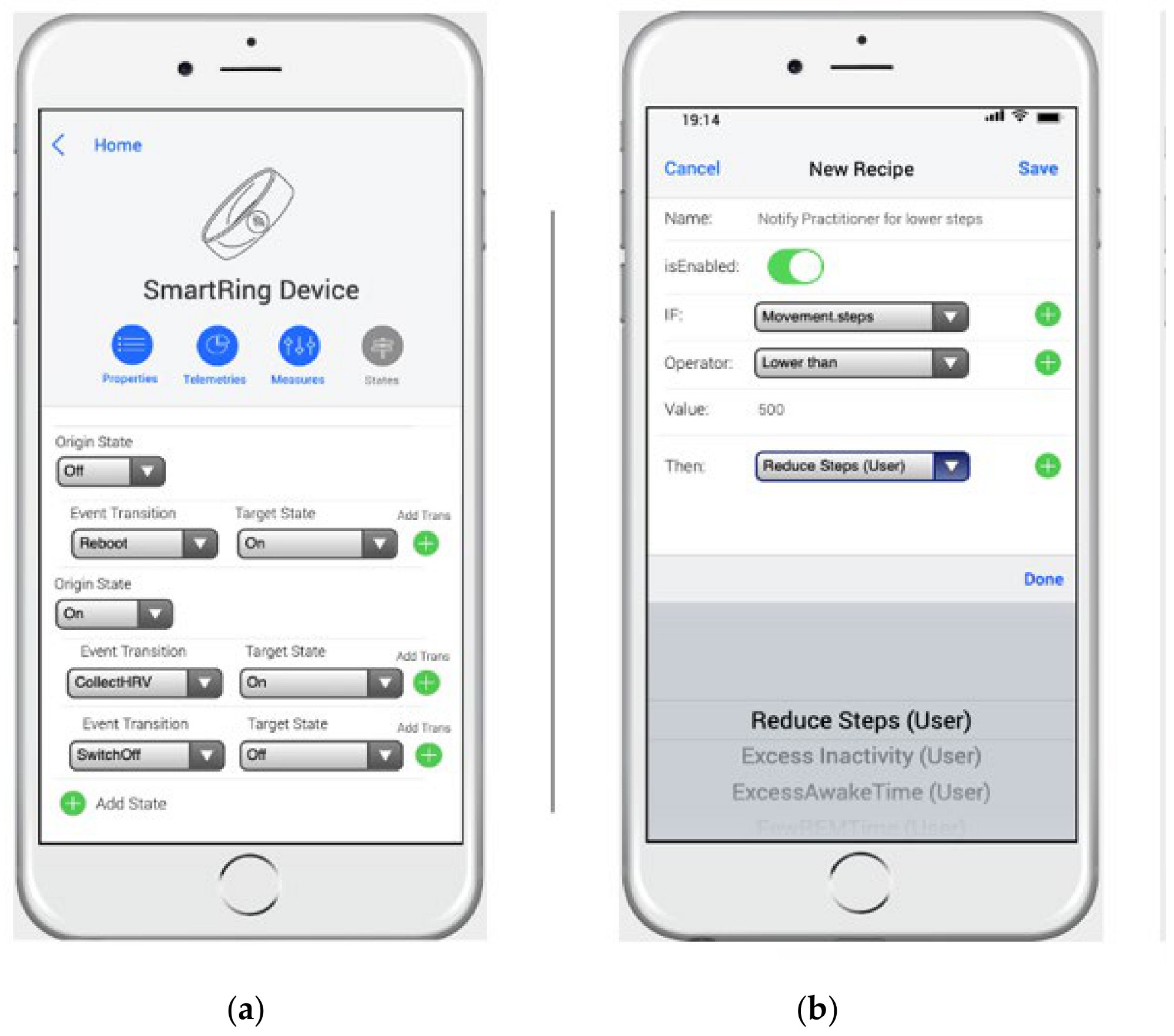
3.2.2. The Device Package
3.2.3. The Healthcare Package
3.3. The MoSIoT Scenario Metamodel
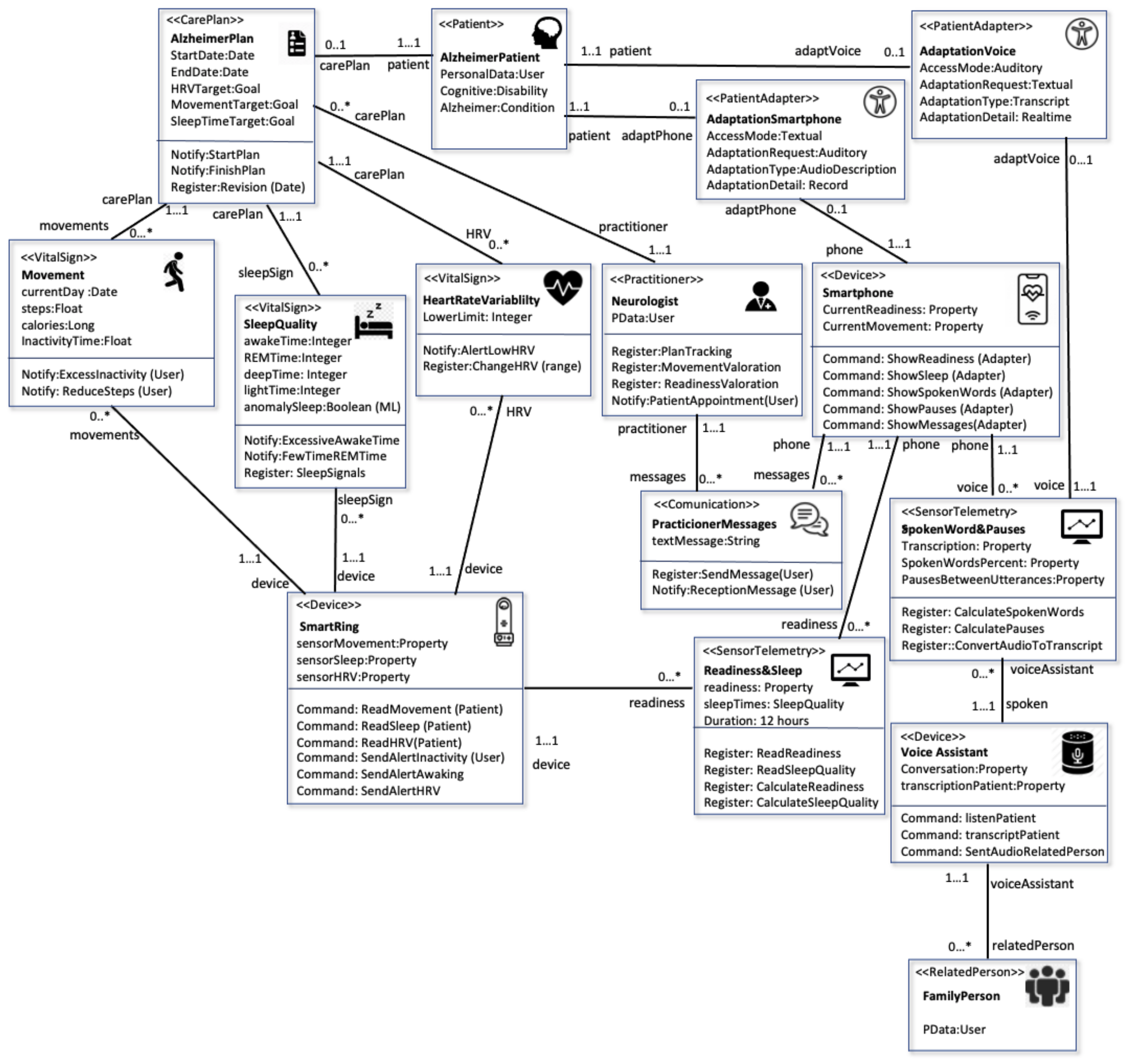
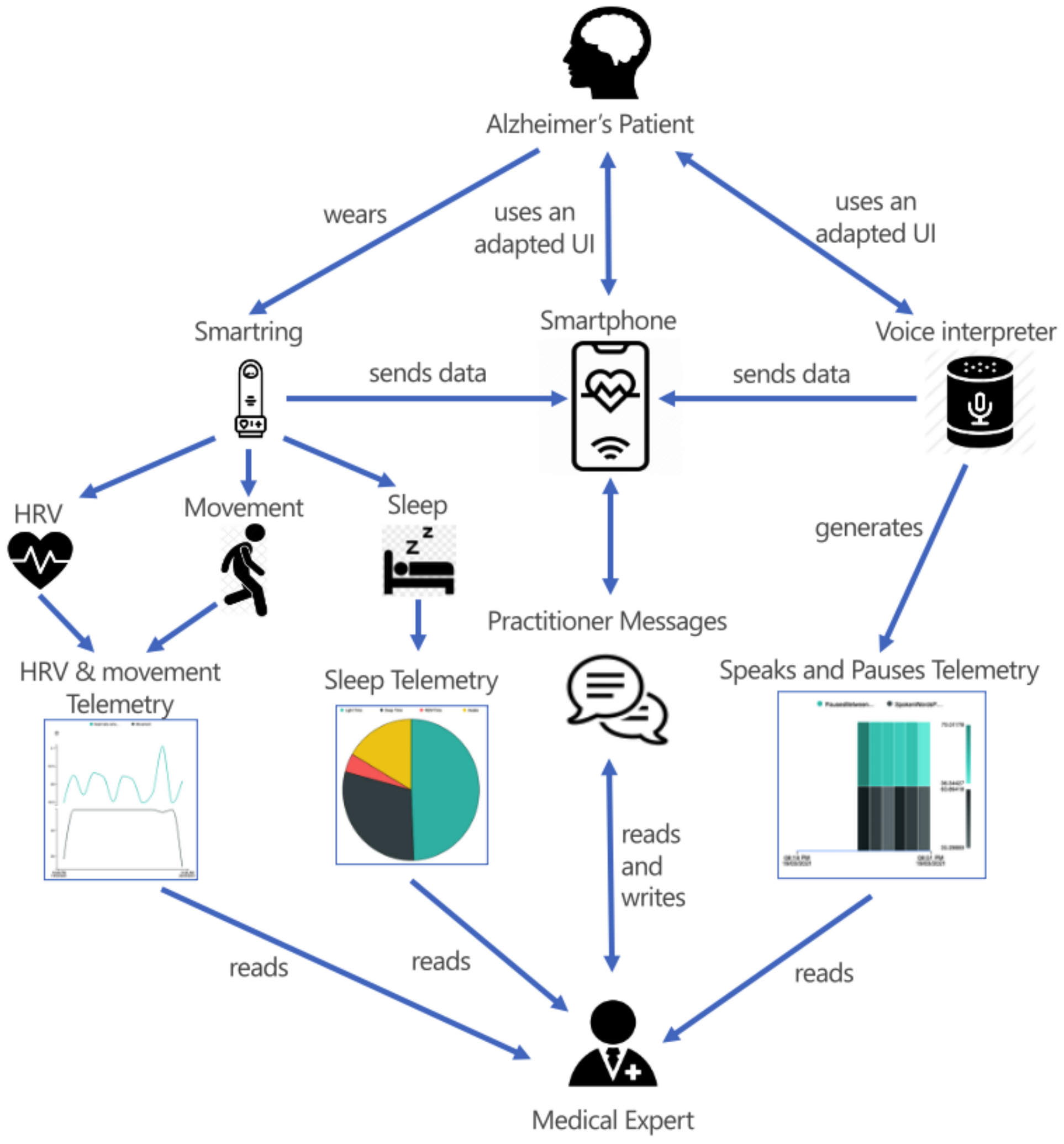
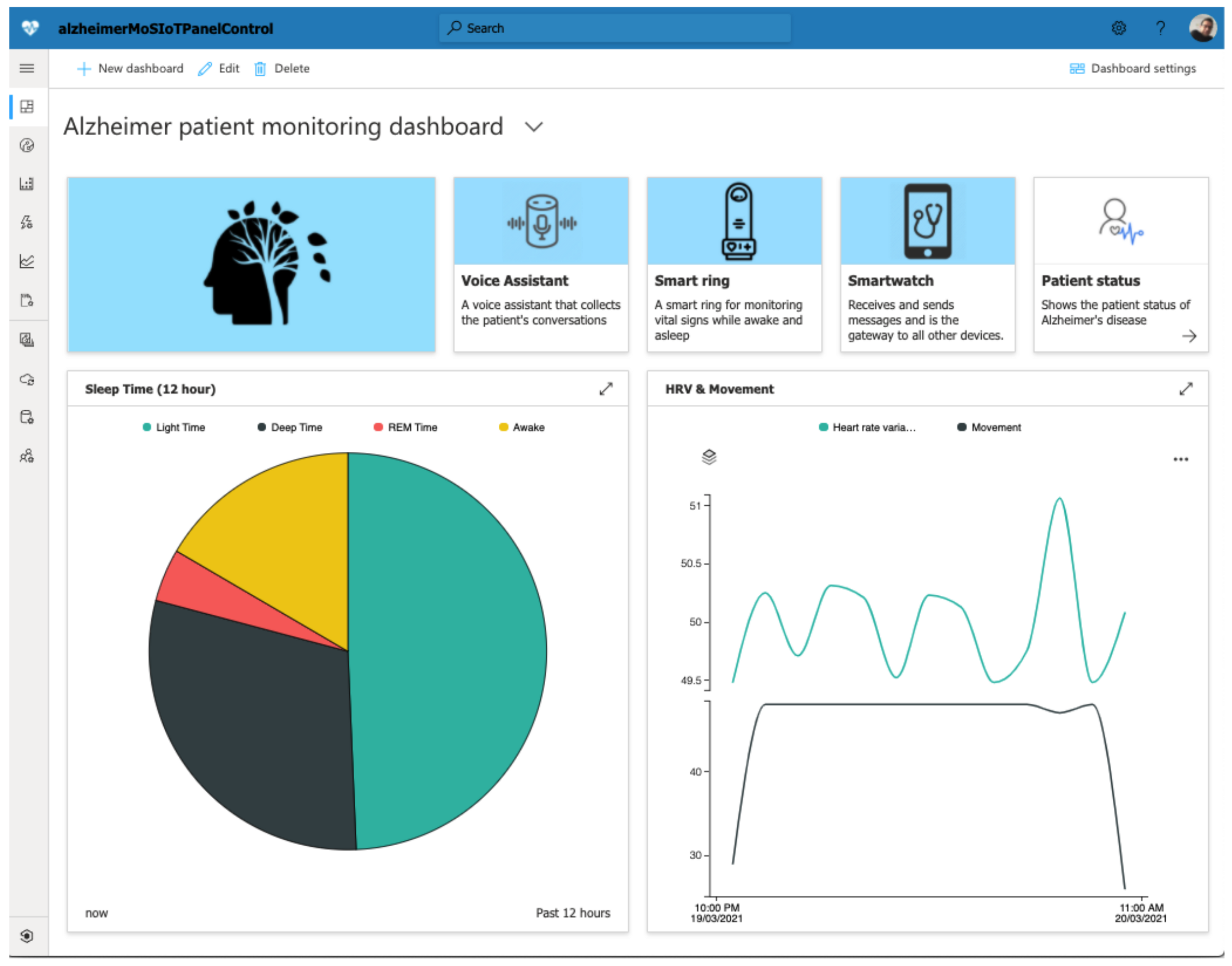
4. A Case Study of the MoSIoT Scenario Model: A Patient with Alzheimer’s Disease
4.1. The MoSIoT Scenario Model
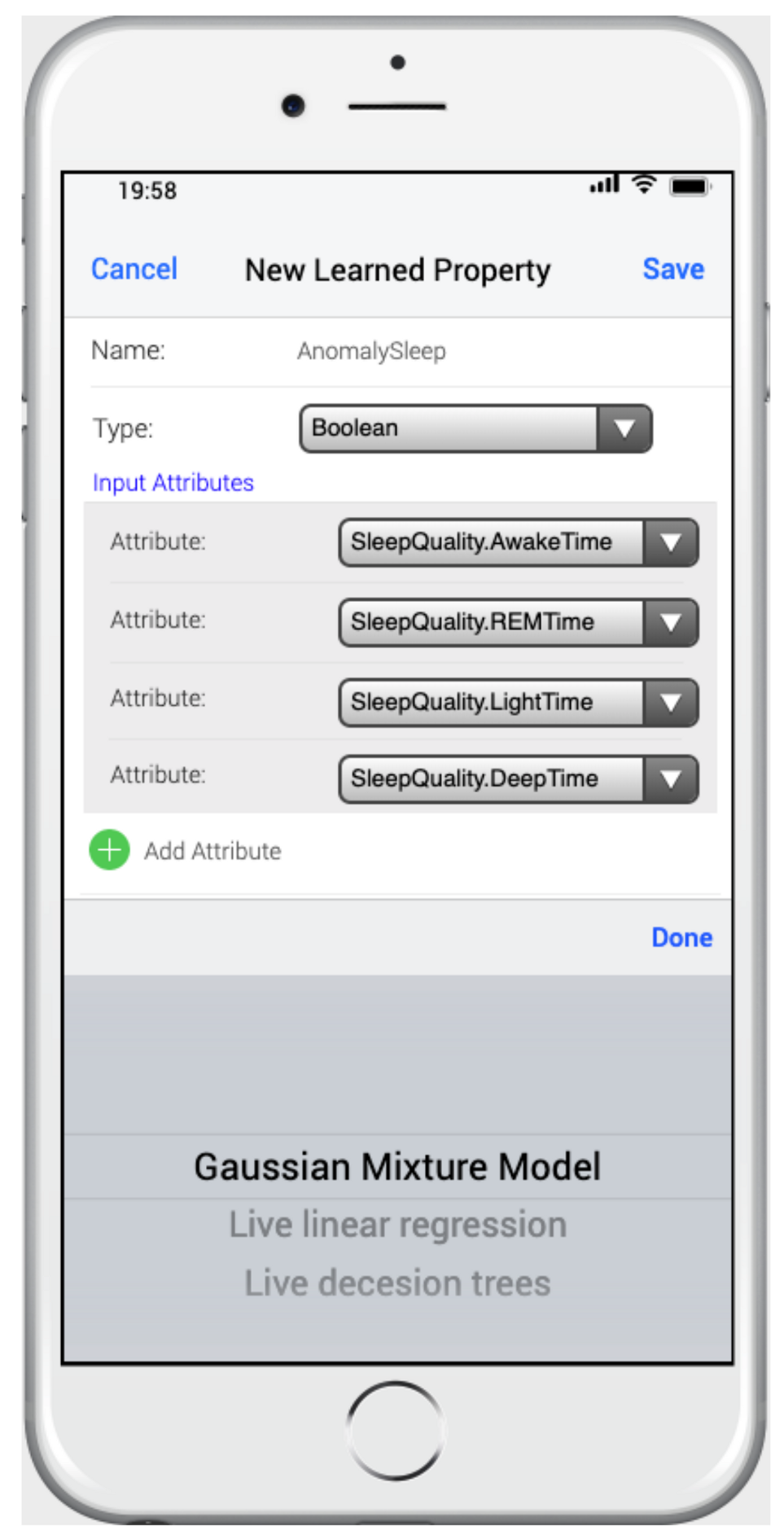
4.2. The Prediction Module of MoSIoT Simulator
4.3. The IoT Hub Integration
5. Discussion
6. Conclusions
Future Work
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- World Health Organization. Disability and Health. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/disability-and-health (accessed on 5 January 2021).
- Gentry, T. Smart homes for people with neurological disability: State of the art. NeuroRehabilitation 2009, 25, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Neßelrath, R.; Haupert, J.; Frey, J.; Brandherm, B. Supporting persons with special needs in their daily life in a smart home. In Proceedings of the 2011 Seventh International Conference on Intelligent Environments, Nottingham, UK, 25–28 July 2011; pp. 370–373. [Google Scholar]
- Stefanov, D.H.; Bien, Z.; Bang, W.C. The smart house for older persons and persons with physical disabilities: Structure, technology arrangements, and perspectives. IEEE Trans. Neural Syst. Rehabil. Eng. 2004, 12, 228–250. [Google Scholar] [CrossRef] [PubMed]
- Aburukba, R.; Al-Ali, A.R.; Kandil, N.; AbuDamis, D. Configurable ZigBee-based control system for people with multiple disabilities in smart homes. In 2016 International Conference on Industrial Informatics and Computer Systems (CIICS); IEEE: Piscataway, NJ, USA, 2016; pp. 1–5. [Google Scholar]
- D’Angelo, G.; Ferretti, S.; Ghini, V. Simulation of the Internet of Things. In Proceedings of the 2016 International Conference on High Performance Computing & Simulation (HPCS), Innsbruck, Austria, 18–22 July 2016; pp. 1–8. [Google Scholar]
- Ojie, E.; Pereira, E. Simulation tools in internet of things: A review. In Proceedings of the 1st International Conference on Internet of Things and Machine Learning, Liverpool, UK, 17–18 October 2017; pp. 1–7. [Google Scholar]
- Bézivin, J. In search of a basic principle for model driven engineering. Novatica J. 2004, 5, 21–24. [Google Scholar]
- Bauer, M.; Bui, N.; De Loof, J.; Magerkurth, C.; Nettsträter, A.; Stefa, J.; Walewski, J.W. IoT reference model. In Enabling Things to Talk; Springer: Berlin/Heidelberg, Germany, 2013; pp. 113–162. [Google Scholar]
- Stackowiak, R. IoT Central and Solution Accelerators. In Azure Internet of Things Revealed; Apress: Berkeley, CA, USA, 2019. [Google Scholar]
- Kourtis, L.C.; Regele, O.B.; Wright, J.M.; Jones, G.B. Digital biomarkers for Alzheimer’s disease: The mobile/wearable devices opportunity. Nat. Partn. J. Digit. Med 2019, 2, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Avci, A.; Bosch, S.; Marin-Perianu, M.; Marin-Perianu, R.; Havinga, P. Activity recognition using inertial sensing for healthcare, wellbeing and sports applications: A survey. In Proceedings of the 23th International Conference on Architecture of Computing Systems, Hannover, Germany, 22–25 February 2010; pp. 1–10. [Google Scholar]
- Campos, W.; Martínez, A.; Sanchez, W.; Estrada, H.; Castro-Sánchez, N.A.; Mujica, D. A systematic review of proposals for the social integration of elderly people using ambient intelligence and social networking sites. Cogn. Comput. 2016, 8, 529–542. [Google Scholar] [CrossRef]
- Sodhro, A.H.; Sangaiah, A.K.; Sodhro, G.H.; Lohano, S.; Pirbhulal, S. An Energy-Efficient Algorithm for Wearable Electrocardiogram Signal Processing in Ubiquitous Healthcare Application. Sensors 2018, 3, 923. [Google Scholar] [CrossRef] [Green Version]
- Magsi, H.; Sodhro, A.H.; Al-Rakhami, M.S.; Zahid, N.; Pirbhulal, S.; Wang, L. A Novel Adaptive Battery-Aware Algorithm for Data Transmission in IoT-Based Healthcare Applications. Electronics 2021, 10, 367. [Google Scholar] [CrossRef]
- Yang, G.; Xie, L.; Mäntysalo, M.; Zhou, X.; Pang, Z.; Da Xu, L.; Zheng, L.R. A health-IoT platform based on the integration of intelligent packaging, unobtrusive bio-sensor, and intelligent medicine box. IEEE Trans. Ind. Inform. 2014, 10, 2180–2191. [Google Scholar] [CrossRef] [Green Version]
- Ahmed, E.; Islam, A.; Sarker, F.; Huda, M.N.; Abdullah-Al-Mamun, K. A road to independent living with smart homes for people with disabilities. In Proceedings of the 2016 5th International Conference on Informatics, Electronics and Vision (ICIEV), Dhaka, Bangladesh, 13–14 May 2016; pp. 472–477. [Google Scholar]
- The Network Simulator NS-2. Available online: http://www.isi.edu/nsnam/ns/ (accessed on 15 December 2020).
- Henderson, T.R.; Lacage, M.; Riley, G.F.; Dowell, C.; Kopena, J. Network simulations with the ns-3 simulator. SIGCOMM Demonstr. 2008, 14, 527. [Google Scholar]
- Brambilla, G.; Picone, M.; Cirani, S.; Amoretti, M.; Zanichelli, F. A simulation platform for large-scale internet of things scenarios in urban environments. In Proceedings of the First International Conference on IoT in Urban Space, Rome, Italy, 27–28 October 2014; pp. 50–55. [Google Scholar]
- Silva, I.; Leandro, R.; Macedo, D.; Guedes, L.A. A dependability evaluation tool for the Internet of Things. Comput. Electr. Eng. 2013, 39, 2005–2018. [Google Scholar] [CrossRef]
- Sotiriadis, S.; Bessis, N.; Asimakopoulou, E.; Mustafee, N. Towards simulating the internet of things. In Proceedings of the 2014 28th International Conference on Advanced Information Networking and Applications Workshops, Victoria, BC, Canada, 13–16 May 2014; pp. 444–448. [Google Scholar]
- Costa, B.; Pires, P.F.; Delicato, F.C.; Li, W.; Zomaya, A.Y. Design and analysis of IoT applications: A model-driven approach. In Proceedings of the 2016 IEEE (DASC/PiCom/DataCom/CyberSciTech), Auckland, New Zealand, 8–12 August 2016; pp. 392–399. [Google Scholar]
- Patel, P.; Cassou, D. Enabling high-level application development for the Internet of Things. J. Syst. Softw. 2015, 103, 62–84. [Google Scholar] [CrossRef]
- Ciccozzi, F.; Spalazzese, R. Mde4iot: Supporting the internet of things with model-driven engineering. In International Symposium on Intelligent and Distributed Computing; Springer: Cham, Switzerland, 2016; pp. 67–76. [Google Scholar]
- Kecskemeti, G.; Casale, G.; Jha, D.N.; Lyon, J.; Ranjan, R. Modelling and simulation challenges in internet of things. IEEE Cloud Comput. 2017, 4, 62–69. [Google Scholar] [CrossRef] [Green Version]
- Johann, S. Software architecture for developers. IEEE Softw. 2015, 5, 93–96. [Google Scholar] [CrossRef]
- Meliá, S.; Gómez, J.; Pérez, S.; Díaz, O. Architectural and Technological Variability in Rich Internet Applications. IEEE Internet Comput. 2010, 14, 24–32. [Google Scholar] [CrossRef]
- Golfarelli, M.; Rizzi, S. UML-based modeling for what-if analysis. In Proceedings of the International Conference on Data Warehousing and Knowledge Discovery, Turin, Italy, 1–5 September 2008; pp. 1–12. [Google Scholar]
- IMS Global Learning Consortium, Inc. IMS Access For All Version 3.0. Available online: http://imsglobal.org/accessibility (accessed on 12 February 2021).
- WAI W3C: Web Accessibility Initiative. Diverse Abilities and Barriers. Available online: https://www.w3.org/WAI/people-use-web/abilities-barriers/ (accessed on 12 February 2021).
- HL7 FHIR: Fast Healthcare Interoperability Resources. Available online: http://hl7.org/implement/standards/fhir/ (accessed on 11 February 2021).
- Guinard, D.D.; Trifa, V.M. Building the Web of Things; Manning Publications: Hong Kong, China, 2016; Volume 3. [Google Scholar]
- ISO 13606. Health Informatics. Available online: https://www.iso.org/standard/40784.html (accessed on 8 May 2021).
- Kalra, D.; Beale, T.; Heard, S. The openEHR foundation. Stud. Health Technol. Inform. 2005, 115, 153–173. [Google Scholar]
- Dolin, R.H.; Alschuler, L.; Beebe, C.; Biron, P.V.; Boyer, S.L.; Essin, D.; Mattison, J.E. The HL7 clinical document architecture. J. Am. Med Inform. Assoc. 2001, 8, 552–569. [Google Scholar] [CrossRef] [Green Version]
- Elkin, P.L.; Brown, S.H.; Husser, C.S.; Bauer, B.A.; Wahner-Roedler, D.; Rosenbloom, S.T.; Speroff, T. Evaluation of the content coverage of SNOMED CT: Ability of SNOMED clinical terms to represent clinical problem lists. In Mayo Clinic Proceedings; Elsevier: Philadelphia, PA, USA, 2016; Volume 81, pp. 741–748. [Google Scholar]
- International Classifications of Diseases (ICD) Version 10. Available online: https://www.cdc.gov/nchs/icd/index.htm (accessed on 10 May 2021).
- International Standard for Indentifying Health Measurements, Observations and Documents (LOINC). Available online: https://loinc.org/ (accessed on 13 May 2021).
- Ur, B.; Pak Yong Ho, M.; Brawner, S.; Lee, J.; Mennicken, S.; Picard, N.; Schulze, D.; Littman, M.L. Trigger-action programming in the wild: An analysis of 200,000 IFTTT recipes. In Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems, San Jose, CA, USA, 7–12 May 2016; pp. 3227–3231. [Google Scholar]
- De Zambotti, M.; Rosas, L.; Colrain, I.M.; Baker, F.C. The sleep of the ring: Comparison of the ŌURA sleep tracker against polysomnography. Behav. Sleep. Med. 2017, 17, 124–136. [Google Scholar] [CrossRef]
- Thayer, J.F.; Hansen, A.L.; Saus-Rose, E.; Johnsen, B.H. Heart rate variability, prefrontal neural function, and cognitive performance: The neurovisceral integration perspective on self-regulation, adaptation, and health. Ann. Behav. Med. 2009, 37, 141–153. [Google Scholar] [CrossRef]
- Kluge, A.; Kirschner, M.; Hager, O.M.; Bischof, M.; Habermeyer, B.; Seifritz, E.; Walther, S.; Kaiser, S. Combining actigraphy, ecological momentary assessment and neuroimaging to study apathy in patients with schizophrenia. Schizophr. Res. 2018, 195, 176–182. [Google Scholar] [CrossRef]
- Goldberg, T.E.; Harvey, P.D.; Wesnes, K.A.; Snyder, P.J.; Schneider, L.S. Practice effects due to serial cognitive assessment: Implications for preclinical Alzheimer’s disease randomized controlled trials. Alzheimer’s Dement. Diagn. Assess. Dis. Monit. 2015, 1, 103–111. [Google Scholar] [CrossRef] [Green Version]
- Hartmann, T.; Moawad, A.; Fouquet, F.; Le Traon, Y. The next evolution of MDE: A seamless integration of machine learning into domain modeling. Softw. Syst. Model. 2019, 18, 1285–1304. [Google Scholar] [CrossRef] [Green Version]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meliá, S.; Nasabeh, S.; Luján-Mora, S.; Cachero, C. MoSIoT: Modeling and Simulating IoT Healthcare-Monitoring Systems for People with Disabilities. Int. J. Environ. Res. Public Health 2021, 18, 6357. https://doi.org/10.3390/ijerph18126357
Meliá S, Nasabeh S, Luján-Mora S, Cachero C. MoSIoT: Modeling and Simulating IoT Healthcare-Monitoring Systems for People with Disabilities. International Journal of Environmental Research and Public Health. 2021; 18(12):6357. https://doi.org/10.3390/ijerph18126357
Chicago/Turabian StyleMeliá, Santiago, Shahabadin Nasabeh, Sergio Luján-Mora, and Cristina Cachero. 2021. "MoSIoT: Modeling and Simulating IoT Healthcare-Monitoring Systems for People with Disabilities" International Journal of Environmental Research and Public Health 18, no. 12: 6357. https://doi.org/10.3390/ijerph18126357
APA StyleMeliá, S., Nasabeh, S., Luján-Mora, S., & Cachero, C. (2021). MoSIoT: Modeling and Simulating IoT Healthcare-Monitoring Systems for People with Disabilities. International Journal of Environmental Research and Public Health, 18(12), 6357. https://doi.org/10.3390/ijerph18126357






