Modelling the Reallocation of Time Spent Sitting into Physical Activity: Isotemporal Substitution vs. Compositional Isotemporal Substitution
Abstract
1. Introduction
2. Materials and Methods
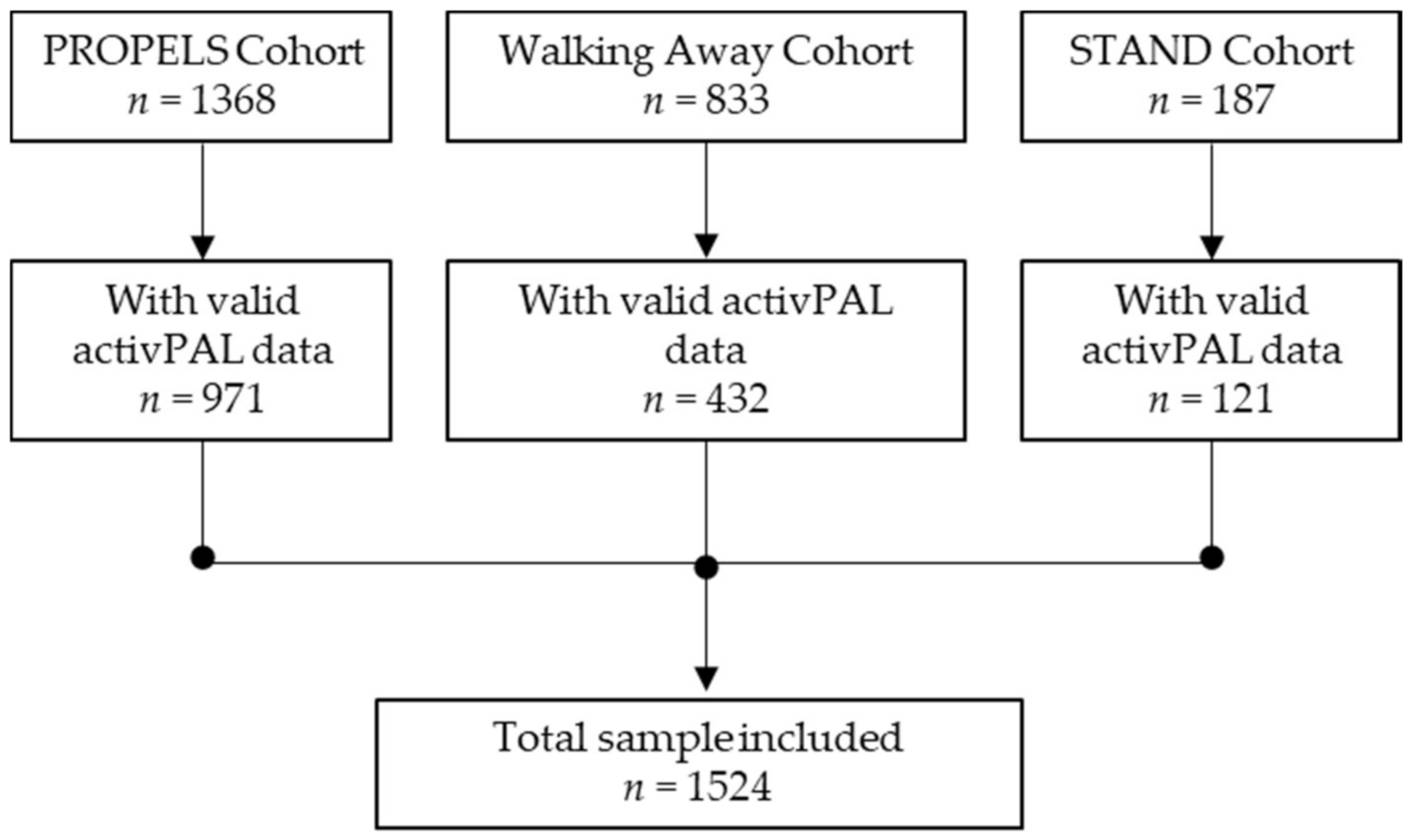
2.1. Participants
2.1.1. PROPELS
2.1.2. Walking Away from Diabetes (WA)
2.1.3. STAND
2.2. Sedentary Behaviour and Physical Activity Measurement
2.3. Anthropometric and Blood Pressure Measurement
2.4. Cardiometabolic Biomarker Measurement
2.5. Covariates
2.6. Statistical Analysis
2.6.1. Isotemporal Substitution Modelling
2.6.2. Compositional Isotemporal Substitution Modelling
2.6.3. Incremental Comparison
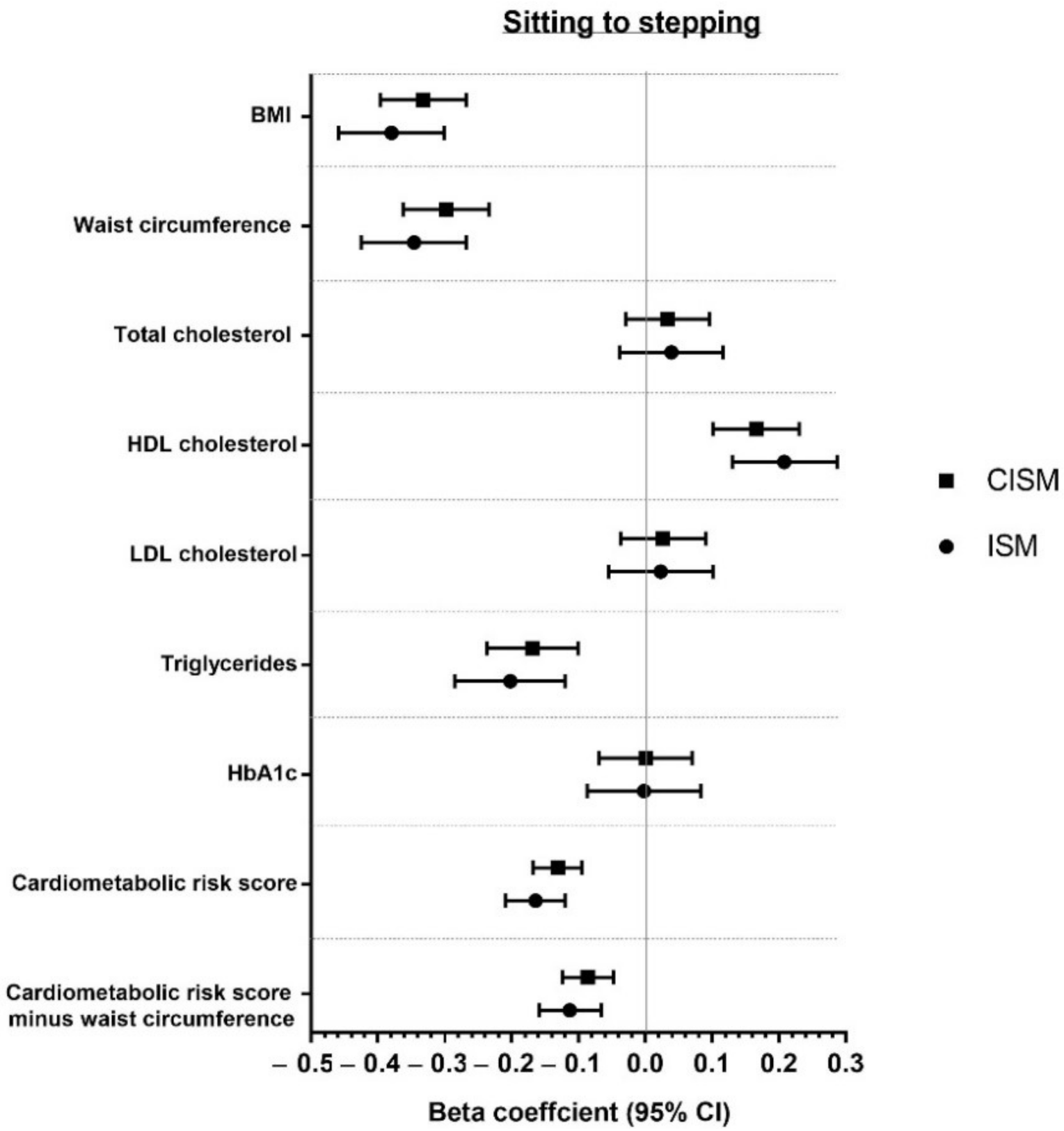
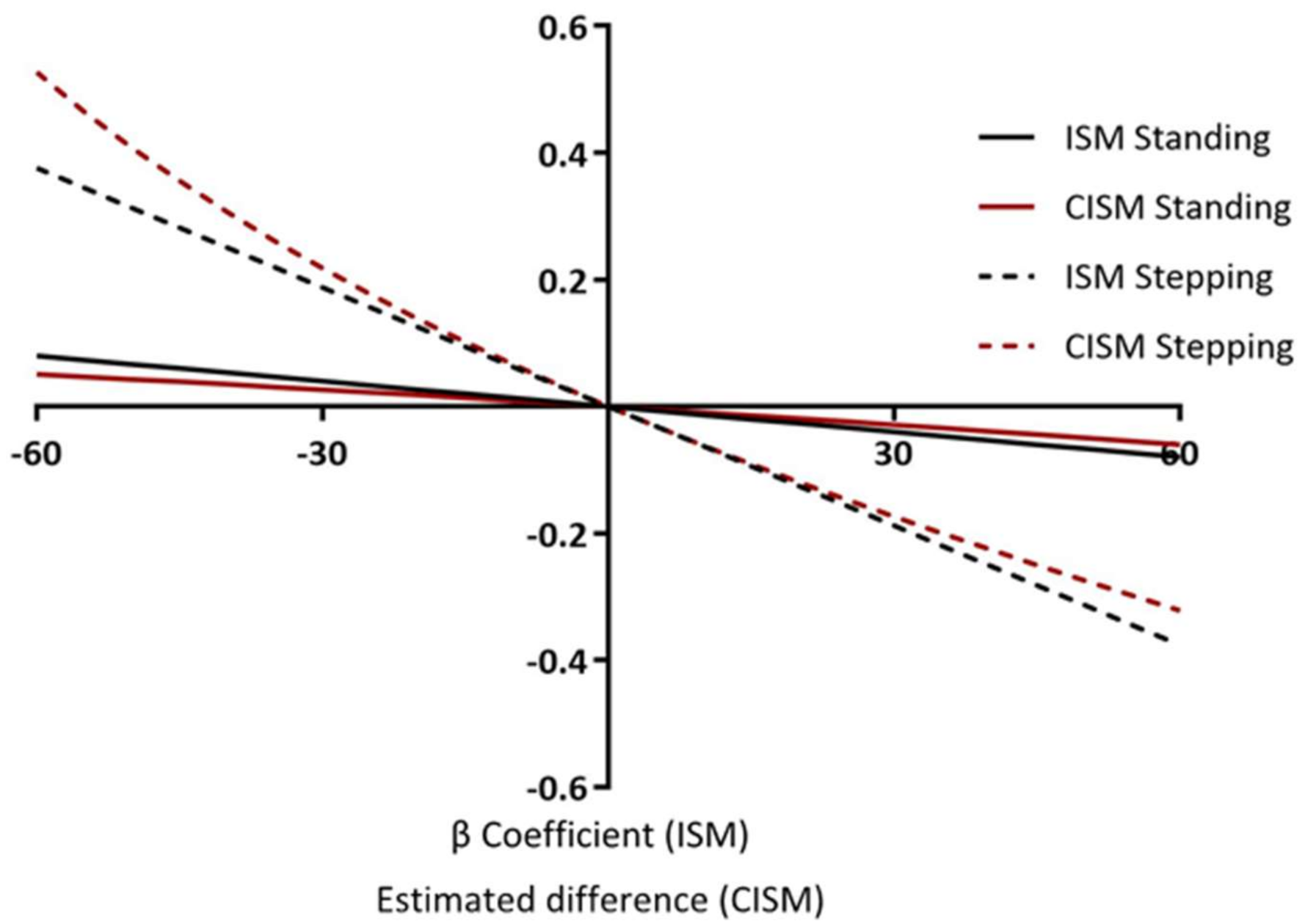
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Biswas, A.; Oh, P.I.; Faulkner, G.E.; Bajaj, R.R.; Silver, M.A.; Mitchell, M.S. Sedentary Time and Its Association with Risk for Disease Incidence, Mortality, and Hospitalization in Adults: A Systematic Review and Meta-Analysis. Ann. Intern. Med. 2015, 162, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Patterson, R.; McNamara, E.; Tainio, M.; de Sa, T.H.; Smith, A.D.; Sharp, S.J.; Edwards, P.; Woodcock, J.; Brage, S.; Wijndaele, K. Sedentary Behaviour and Risk of All-Cause, Cardiovascular and Cancer Mortality, and Incident Type 2 Diabetes: A Systematic Review and Dose Response Meta-Analysis. Eur. J. Epidemiol. 2018, 33, 811–829. [Google Scholar] [CrossRef] [PubMed]
- Wilmot, E.G.; Edwardson, C.L.; Achana, F.A.; Davies, M.J.; Gorely, T.; Gray, L.J.; Khunti, K.; Yates, T.; Biddle, S.J.H. Sedentary Time in Adults and the Association with Diabetes, Cardiovascular Disease and Death: Systematic Review and Meta-Analysis. Diabetologia 2012, 55, 2895–2905. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T. Effect of Physical Inactivity on Major Non-Communicable Diseases Worldwide: An Analysis of Burden of Disease and Life Expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef]
- Ku, P.-W.; Steptoe, A.; Liao, Y.; Hsueh, M.-C.; Chen, L.-J. A Cut-Off of Daily Sedentary Time and All-Cause Mortality in Adults: A Meta-Regression Analysis Involving More than 1 Million Participants. BMC Med. 2018, 16, 74. [Google Scholar] [CrossRef] [PubMed]
- Ekelund, U.; Brown, W.J.; Steene-Johannessen, J.; Fagerland, M.W.; Owen, N.; Powell, K.E.; Bauman, A.E.; Lee, I.-M. Do the Associations of Sedentary Behaviour with Cardiovascular Disease Mortality and Cancer Mortality Differ by Physical Activity Level? A Systematic Review and Harmonised Meta-Analysis of Data From 850 060 Participants. Br. J. Sports Med. 2018. [Google Scholar] [CrossRef]
- Ekelund, U.; Steene-Johannessen, J.; Brown, W.J.; Fagerland, M.W.; Owen, N.; Powell, K.E.; Bauman, A.; Lee, I.M. Does Physical Activity Attenuate, or Even Eliminate, the Detrimental Association of Sitting Time with Mortality? A Harmonised Meta-Analysis of Data from More Than 1 Million Men and Women. Lancet 2016, 388, 1302–1310. [Google Scholar] [CrossRef]
- Ekelund, U.; Tarp, J.; Steene-Johannessen, J.; Hansen, B.H.; Jefferis, B.; Fagerland, M.W.; Whincup, P.; Diaz, K.M.; Hooker, S.P.; Chernofsky, A.; et al. Dose-Response Associations Between Accelerometry Measured Physical Activity and Sedentary Time and All Cause Mortality: Systematic Review and Harmonised Meta-Analysis. BMJ 2019, 366, l4570. [Google Scholar] [CrossRef]
- Biddle, G.J.H.; Edwardson, C.L.; Henson, J.; Davies, M.J.; Khunti, K.; Rowlands, A.V.; Yates, T. Associations of Physical Behaviours and Behavioural Reallocations with Markers of Metabolic Health: A Compositional Data Analysis. Int. J. Environ. Res. Public Health 2018, 15, 2280. [Google Scholar] [CrossRef] [PubMed]
- Buman, M.P.; Winkler, E.A.H.; Kurka, J.M.; Hekler, E.B.; Baldwin, C.M.; Owen, N.; Ainsworth, B.E.; Healy, G.N.; Gardiner, P.A. Reallocating Time to Sleep, Sedentary Behaviors, or Active Behaviors: Associations with Cardiovascular Disease Risk Biomarkers, NHANES 2005–2006. Am. J. Epidemiol. 2014, 179, 323–334. [Google Scholar] [CrossRef]
- Dumuid, D.; Pedisic, Z.; Stanford, T.E.; Martin-Fernadez, J.-A.; Hron, K.; Maher, C.A.; Lewis, L.K.; Olds, T. The Compositional Isotemporal Substitution Model: A Method for Estimating Changes in a Health Outcome for Reallocation of Time Between Sleep, Physical Activity and Sedentary Behaviour. Stat. Methods Med Res. 2017, 3, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Edwardson, C.L.; Henson, J.; Bodicoat, D.H.; Bakrania, K.; Khunti, K.; Davies, M.J.; Yates, T. Associations of Reallocating Sitting Time into Standing or Stepping with Glucose, Insulin and Insulin Sensitivity: A Cross-Sectional Analysis of Adults at Risk of Type 2 Diabetes. BMJ Open 2017, 7. [Google Scholar] [CrossRef] [PubMed]
- Falconer, C.L.; Page, A.S.; Andrews, R.C.; Cooper, A.R. The Potential Impact of Displacing Sedentary Time in Adults with Type 2 Diabetes. Med. Sci. Sports Exerc. 2015, 47, 2070–2075. [Google Scholar] [CrossRef] [PubMed]
- Hamer, M.; Stamatakis, E.; Steptoe, A. Effects of Substituting Sedentary Time with Physical Activity on Metabolic Risk. Med. Sci. Sports Exerc. 2014, 46, 1946–1950. [Google Scholar] [CrossRef]
- Healy, G.N.; Winkler, E.A.H.; Owen, N.; Anuradha, S.; Dunstan, D.W. Replacing Sitting Time with Standing or Stepping: Associations with Cardio-Metabolic Risk Biomarkers. Eur. Heart J. 2015, 36, 2643–2649. [Google Scholar] [CrossRef] [PubMed]
- Henson, J.; Edwardson, C.L.; Bodicoat, D.H.; Bakrania, K.; Davies, M.J.; Khunti, K.; Talbot, D.C.S.; Yates, T. Reallocating Sitting Time to Standing or Stepping Through Isotemporal Analysis: Associations with Markers of Chronic Low-Grade Inflammation. J. Sports Sci. 2017, 1–8. [Google Scholar] [CrossRef]
- Mekary, R.A.; Ding, E.L. Isotemporal Substitution as the Gold Standard Model for Physical Activity Epidemiology: Why It Is the Most Appropriate for Activity Time Research. Int. J. Environ. Res. Public Health 2019, 16, 797. [Google Scholar] [CrossRef]
- Stamatakis, E.; Rogers, K.; Ding, D.; Berrigan, D.; Chau, J.; Hamer, M.; Bauman, A. All-Cause Mortality Effects of Replacing Sedentary Time with Physical Activity and Sleeping Using an Isotemporal Substitution Model: A Prospective Study of 201,129 Mid-Aged and Older Adults. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 121. [Google Scholar] [CrossRef]
- Varela-Mato, V.; O’Shea, O.; King, J.A.; Yates, T.; Stensel, D.J.; Biddle, S.J.; Nimmo, M.A.; Clemes, S.A. Cross-Sectional Surveillance Study to Phenotype Lorry Drivers’ Sedentary Behaviours, Physical Activity and Cardio-Metabolic Health. BMJ Open 2017, 7, e013162. [Google Scholar] [CrossRef]
- Yates, T.; Henson, J.; Edwardson, C.; Dunstan, D.; Bodicoat, D.H.; Khunti, K. Objectively Measured Sedentary Time and Associations with Insulin Sensitivity: Importance of Reallocating Sedentary Time to Physical Activity. Prev. Med. 2015, 76, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Ryan, D.J.; Wullems, J.A.; Stebbings, G.K.; Morse, C.I.; Stewart, C.E.; Onambele-Pearson, G.L. Using Isotemporal Substitution to Predict the Effects of Changing Physical Behaviour on Older Adults’ Cardio-Metabolic Profiles. PLoS ONE 2019, 14, e0224223. [Google Scholar] [CrossRef]
- Dumuid, D.; Stanford, T.E.; Pedisic, Z.; Maher, C.; Lewis, L.K.; Martin-Fernandez, J.A.; Katzmarzyk, P.T.; Chaput, J.P.; Fogelholm, M.; Standage, M.; et al. Adiposity and the Isotemporal Substitution of Physical Activity, Sedentary Time and Sleep Among School-Aged Children: A Compositional Data Analysis Approach. BMC Public Health 2018, 18, 311. [Google Scholar] [CrossRef]
- van der Ploeg, H.P.; Chey, T.; Korda, R.J.; Banks, E.; Bauman, A. Sitting Time and All-Cause Mortality Risk in 222 497 Australian Adults. Arch. Intern. Med. 2012, 172, 494–500. [Google Scholar] [CrossRef]
- van der Ploeg, H.P.; Chey, T.; Ding, D.; Chau, J.Y.; Stamatakis, E.; Bauman, A.E. Standing Time and All-Cause Mortality in a Large Cohort of Australian Adults. Prev. Med. 2014, 69, 187–191. [Google Scholar] [CrossRef] [PubMed]
- Bakrania, K.; Edwardson, C.L.; Khunti, K.; Bandelow, S.; Davies, M.J.; Yates, T. Associations Between Sedentary Behaviours and Cognitive Function: Cross-Sectional and Prospective Findings from the UK Biobank. Am. J. Epidemiol. 2017, 187, 441–454. [Google Scholar] [CrossRef]
- Henson, J.; Yates, T.; Biddle, S.J.; Edwardson, C.L.; Khunti, K.; Wilmot, E.G. Associations of Objectively Measured Sedentary Behaviour and Physical Activity with Markers of Cardiometabolic Health. Diabetologia 2013, 56, 1012–1020. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.F.M.; Altenburg, T.M.; Chinapaw, M.J.M. Sedentary Behavior Research Network (SBRN)—Terminology Consensus Project Process and Outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 75. [Google Scholar] [CrossRef]
- Biddle, G.J.H.; Edwardson, C.L.; Henson, J.; Rowlands, A.V.; Yates, T. Reply to Mekary, R.A.; Ding, E.L. Isotemporal Substitution as the Gold Standard Model for Physical Activity Epidemiology: Why It Is the Most Appropriate for Activity Time Research. Int. J. Environ. Res. Public Health 2019, 16, 797. Int. J. Environ. Res. Public Health 2019, 16, 2885. [Google Scholar] [CrossRef] [PubMed]
- Chastin, S.F.M.; Palarea-Albaladejo, J.; Dontje, M.L.; Skelton, D.A. Combined Effects of Time Spent in Physical Activity, Sedentary Behaviors and Sleep on Obesity and Cardio-Metabolic Health Markers: A Novel Compositional Data Analysis Approach. PLoS ONE 2015, 10, e0139984. [Google Scholar] [CrossRef]
- Mekary, R.A.; Willett, W.C.; Hu, F.B.; Ding, E.L. Isotemporal Substitution Paradigm for Physical Activity Epidemiology and Weight Change. Am. J. Epidemiol. 2009, 170, 519–527. [Google Scholar] [CrossRef]
- Atkin, A.J.; Gorely, T.; Clemes, S.A.; Yates, T.; Edwardson, C.; Brage, S.; Salmon, J.; Marshall, S.J.; Biddle, S.J. Methods of Measurement in Epidemiology: Sedentary Behaviour. Int. J. Epidemiol. 2012, 41, 1460–1471. [Google Scholar] [CrossRef]
- Healy, G.N.; Clark, B.K.; Winkler, E.A.H.; Gardiner, P.A.; Brown, W.J.; Matthews, C.E. Measurement of Adults’ Sedentary Time in Population-Based Studies. Am. J. Prev. Med. 2011, 41, 216–227. [Google Scholar] [CrossRef]
- Stamatakis, E.; Ekelund, U.; Ding, D.; Hamer, M.; Bauman, A.E.; Lee, I.-M. Is the Time Right for Quantitative Public Health Guidelines on Sitting? A Narrative Review of Sedentary Behaviour Research Paradigms and Findings. Br. J. Sports Med. 2018, 53, 377–382. [Google Scholar] [CrossRef]
- Wilmot, E.G.; Davies, M.J.; Edwardson, C.L.; Gorely, T.; Khunti, K.; Nimmo, M.; Yates, T.; Biddle, S.J. Rationale And Study Design For A Randomised Controlled Trial To Reduce Sedentary Time in Adults at Risk of Type 2 Diabetes Mellitus: Project Stand (Sedentary Time And Diabetes). BMC Public Health 2011, 11, 908. [Google Scholar] [CrossRef]
- Yates, T.; Davies, M.J.; Henson, J.; Troughton, J.; Edwardson, C.; Gray, L.J.; Khunti, K. Walking Away from Type 2 Diabetes: Trial Protocol of a Cluster Randomised Controlled Trial Evaluating a Structured Education Programme in Those at High Risk of Developing Type 2 Diabetes. BMC Fam. Pract. 2012, 13, 46. [Google Scholar] [CrossRef] [PubMed]
- Yates, T.; Griffin, S.; Bodicoat, D.H.; Brierly, G.; Dallosso, H.; Davies, M.J.; Eborall, H.; Edwardson, C.; Gillett, M.; Gray, L.; et al. PRomotion of Physical Activity Through Structured Education with Differing Levels of Ongoing Support for People at High Risk of Type 2 Diabetes (PROPELS): Study Protocol for a Randomized Controlled Trial. Trials 2015, 16, 289. [Google Scholar] [CrossRef][Green Version]
- National Institute for Health and Care Excellence. Type 2 Diabetes: Prevention in People at High Risk. Available online: https://www.nice.org.uk/guidance/ph38 (accessed on 20 January 2020.).
- Gray, L.J.; Davies, M.J.; Hiles, S.; Taub, N.A.; Webb, D.R.; Srinivasan, B.T.; Khunti, K. Detection of Impaired Glucose Regulation and/or Type 2 Diabetes Mellitus, Using Primary Care Electronic Data, in a Multiethnic UK Community Setting. Diabetologia 2012, 55, 959–966. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycemia: Report of a WHO/IDF Consultation; World Health Organisation: Geneva, Switzerland, 2006. [Google Scholar]
- Edwardson, C.L.; Winkler, E.A.H.; Bodicoat, D.H.; Yates, T.; Davies, M.J.; Dunstan, D.W.; Healy, G.N. Considerations when Using the Activpal Monitor in Field-Based Research with Adult Populations. J. Sport Health Sci. 2016. [Google Scholar] [CrossRef] [PubMed]
- Edwardson, C.L.; Rowlands, A.V.; Bunnewell, S.; Sanders, J.; Esliger, D.W.; Gorely, T.; O’Connell, S.; Davies, M.J.; Khunti, K.; Yates, T. Accuracy of Posture Allocation Algorithms for Thigh- and Waist-Worn Accelerometers. Med. Sci. Sports Exerc. 2016, 48, 1085–1090. [Google Scholar] [CrossRef]
- GitHub. ProcessingPAL. Available online: https://github.com/UOL-COLS/ProcessingPAL (accessed on 1 May 2019).
- Winkler, E.A.; Bodicoat, D.H.; Healy, G.N.; Bakrania, K.; Yates, T.; Owen, N.; Dunstan, D.W.; Edwardson, C.L. Identifying Adults’ Valid Waking Wear Time by Automated Estimation in Activpal Data Collected with A 24 H Wear Protocol. Physiol. Meas. 2016, 37, 1653. [Google Scholar] [CrossRef] [PubMed]
- Wijndaele, K.; Orrow, G.; Ekelund, U.; Sharp, S.J.; Brage, S.; Griffin, S.J.; Simmons, R.K. Increasing Objectively Measured Sedentary Time Increases Clustered Cardiometabolic Risk: A 6 Year Analysis of the Proactive Study. Diabetologia 2014, 57, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Viitasalo, A.; Lakka, T.A.; Laaksonen, D.E.; Savonen, K.; Lakka, H.M.; Hassinen, M.; Komulainen, P.; Tompuri, T.; Kurl, S.; Laukkanen, J.A.; et al. Validation of Metabolic Syndrome Score by Confirmatory Factor Analysis in Children and Adults and Prediction of Cardiometabolic Outcomes in Adults. Diabetologia 2014, 57, 940–949. [Google Scholar] [CrossRef] [PubMed]
- Yates, T.; Edwardson, C.L.; Henson, J.; Zaccardi, F.; Khunti, K.; Davies, M.J. Prospectively Reallocating Sedentary Time: Associations with Cardiometabolic Health. Med. Sci. Sports Exerc. 2020, 52, 844–850. [Google Scholar] [CrossRef] [PubMed]
- Dumuid, D.; Maher, C.; Lewis, L.K.; Stanford, T.E.; Martin Fernandez, J.A.; Ratcliffe, J.; Katzmarzyk, P.T.; Barreira, T.V.; Chaput, J.P.; Fogelholm, M.; et al. Human Development Index, Children’s Health-Related Quality of Life and Movement Behaviors: A Compositional Data Analysis. Qual. Life Res. 2018, 27, 1473–1482. [Google Scholar] [CrossRef] [PubMed]
- Henson, J.; Davies, M.J.; Bodicoat, D.H.; Edwardson, C.L.; Gill, J.M.R.; Stensel, D.J.; Tolfrey, K.; Dunstan, D.W.; Khunti, K.; Yates, T. Breaking Up Prolonged Sitting with Standing or Walking Attenuates the Postprandial Metabolic Response in Postmenopausal Women: A Randomized Acute Study. Diabetes Care 2016, 39, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Dempsey, P.C.; Larsen, R.N.; Sethi, P.; Sacre, J.W.; Straznicky, N.E.; Cohen, N.D.; Cerin, E.; Lambert, G.W.; Owen, N.; Kingwell, B.A.; et al. Benefits for Type 2 Diabetes of Interrupting Prolonged Sitting with Brief Bouts of Light Walking or Simple Resistance Activities. Diabetes Care 2016, 39, 964–972. [Google Scholar] [CrossRef] [PubMed]
- Dunstan, D.W.; Kingwell, B.A.; Larsen, R.; Healy, G.N.; Cerin, E.; Hamilton, M.T.; Shaw, J.E.; Bertovic, D.A.; Zimmet, P.Z.; Salmon, J.; et al. Breaking Up Prolonged Sitting Reduces Postprandial Glucose and Insulin Responses. Diabetes Care 2012, 35, 976–983. [Google Scholar] [CrossRef] [PubMed]
- Pelclova, J.; Stefelova, N.; Dumuid, D.; Pedisic, Z.; Hron, K.; Gaba, A.; Olds, T.; Pechova, J.; Zajac-Gawlak, I.; Tlucakova, L. Are Longitudinal Reallocations of Time Between Movement Behaviours Associated with Adiposity Among Elderly Women? A Compositional Isotemporal Substitution Analysis. Int. J. Obes. 2020, 44, 857–864. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | All (n = 1524) | PROPELS (n = 971) | WA (n = 432) | STAND (n = 121) |
|---|---|---|---|---|
| Age (years) | 59.8 (11.9) | 59.9 (9.0) | 66.8 (7.4) | 32.8 (5.7) |
| Male (%) | 51.7 | 49.9 | 61.8 | 29.9 |
| White European (%) | 72.9 | 70.5 | 89.1 | 75.2 |
| Body mass index (kg/m2) | 30.3 (5.7) | 29.3 (5.7) | 31.4 (5.3) | 34.4 (5.1) |
| Waist circumference (cm) | 100 (14) | 98 (14) | 103 (13) | 103 (13) |
| Using blood pressure medication (%) | 40.2 | 38.2 | 48.6 | 3.3 |
| Using lipid-lowering medication (%) | 27.9 | 28.3 | 30.1 | 0.8 |
| Current smokers (%) | 9.1 | 8.9 | 7.2 | 19.0 |
| HbA1c (unit %) | 5.8 (0.4) | 5.8 (0.3) | 5.7 (0.5) | 5.5 (0.3) |
| Sitting (min/day) | 548 (112) | 542 (113) | 568 (109) | 530 (107) |
| Standing (min/day) | 286 (96) | 296 (97) | 268 (89) | 277 (91) |
| Stepping (min/day) | 107 (40) | 111 (40) | 101 (38) | 103 (37) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Biddle, G.J.H.; Henson, J.; Biddle, S.J.H.; Davies, M.J.; Khunti, K.; Rowlands, A.V.; Sutton, S.; Yates, T.; Edwardson, C.L. Modelling the Reallocation of Time Spent Sitting into Physical Activity: Isotemporal Substitution vs. Compositional Isotemporal Substitution. Int. J. Environ. Res. Public Health 2021, 18, 6210. https://doi.org/10.3390/ijerph18126210
Biddle GJH, Henson J, Biddle SJH, Davies MJ, Khunti K, Rowlands AV, Sutton S, Yates T, Edwardson CL. Modelling the Reallocation of Time Spent Sitting into Physical Activity: Isotemporal Substitution vs. Compositional Isotemporal Substitution. International Journal of Environmental Research and Public Health. 2021; 18(12):6210. https://doi.org/10.3390/ijerph18126210
Chicago/Turabian StyleBiddle, Gregory J. H., Joseph Henson, Stuart J. H. Biddle, Melanie J. Davies, Kamlesh Khunti, Alex V. Rowlands, Stephen Sutton, Thomas Yates, and Charlotte L. Edwardson. 2021. "Modelling the Reallocation of Time Spent Sitting into Physical Activity: Isotemporal Substitution vs. Compositional Isotemporal Substitution" International Journal of Environmental Research and Public Health 18, no. 12: 6210. https://doi.org/10.3390/ijerph18126210
APA StyleBiddle, G. J. H., Henson, J., Biddle, S. J. H., Davies, M. J., Khunti, K., Rowlands, A. V., Sutton, S., Yates, T., & Edwardson, C. L. (2021). Modelling the Reallocation of Time Spent Sitting into Physical Activity: Isotemporal Substitution vs. Compositional Isotemporal Substitution. International Journal of Environmental Research and Public Health, 18(12), 6210. https://doi.org/10.3390/ijerph18126210







