Influencing Factors of Psychosocial Stress among Korean Adults during the COVID-19 Outbreak
Abstract
1. Introduction
2. Materials and Methods
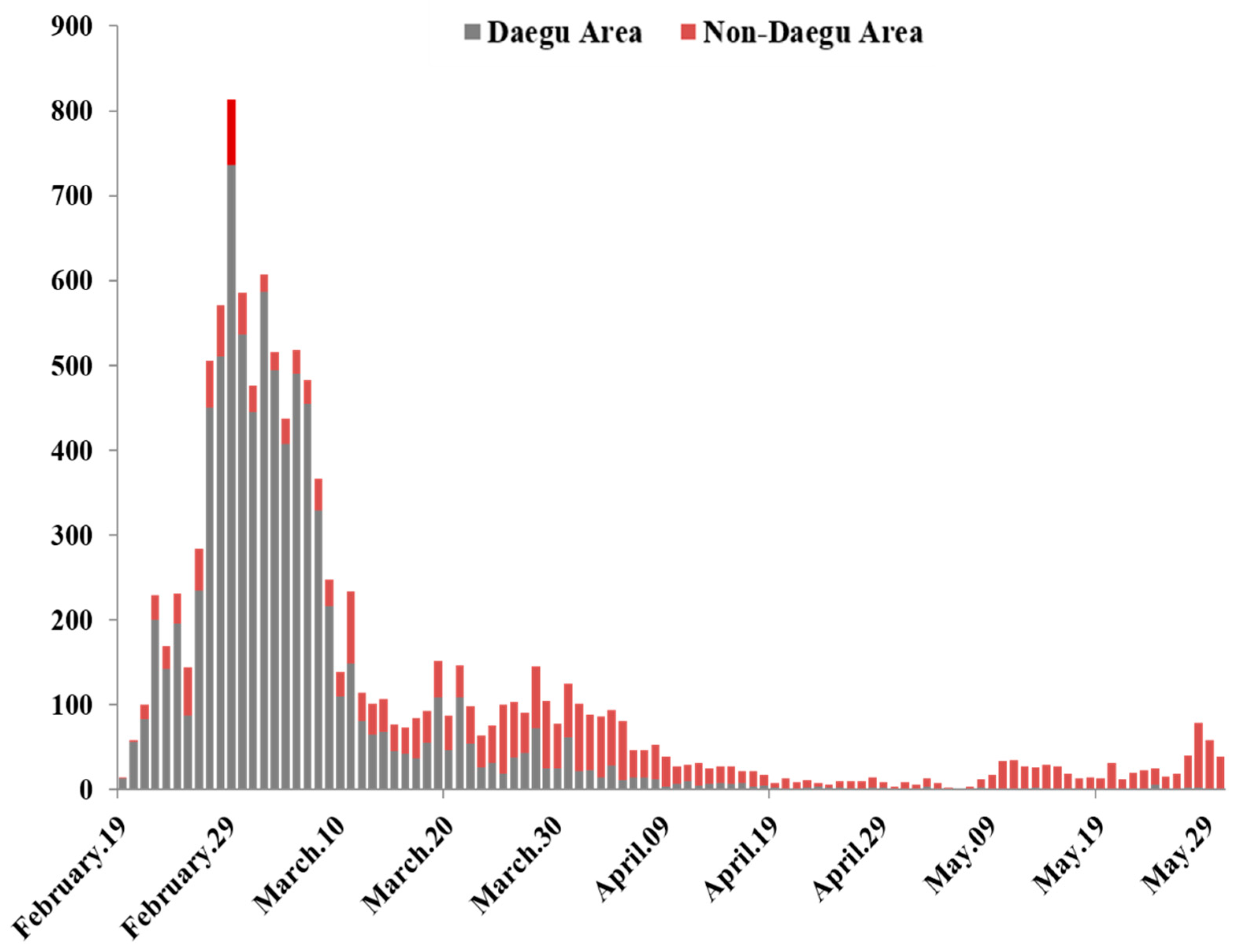
2.1. Design and Participants
2.2. Data Collection
2.3. Measures
2.3.1. Knowledge of COVID-19
2.3.2. Health Belief
2.3.3. Resilience
2.3.4. Psychosocial Stress
2.4. Ethical Considerations
2.5. Analysis
3. Results
3.1. Sociodemographic Characteristics
3.2. Knowledge of COVID-19, Health Belief, Resilience, and Psychosocial Stress
3.3. Differences in Knowledge of COVID-19, Health Beliefs, Resilience, and Psychosocial Stress by Sociodemographic Characteristics
3.4. Correlations between Variables
3.5. Influencing Factors of Psychosocial Stress
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO Announces COVID-19 Outbreak a Pandemic 2020. Issue Newspaper. Available online: https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic (accessed on 26 March 2021).
- Dubey, S.; Biswas, P.; Ghosh, R.; Chatterjee, S.; Dubey, M.J.; Chatterjee, S.; Dubey, J.M.; Chatterjee, S.; Lahiri, D.; Lavie, C.J. Psychosocial impact of COVID-19. Diabetes Metab. Syndr. 2020, 14, 779–788. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Siddique, R.; Li, H.; Ali, A.; Shereen, M.A.; Bashir, N.; Xue, M. Impact of coronavirus outbreak on psychological health. J. Glob. Health 2020, 10. [Google Scholar] [CrossRef] [PubMed]
- Quadri, S.A. COVID-19 and religious congregations: Implications for spread of novel pathogens. Int. J. Inf. Dis. 2020, 96, 219–221. [Google Scholar] [CrossRef] [PubMed]
- Hashmi, F.K.; Iqbal, Q.; Haque, N.; Saleem, F. Religious cliché and stigma: A brief response to overlooked barriers in COVID-19 management. J. Relig. Health 2020, 59, 2697–2700. [Google Scholar] [CrossRef]
- Park, K.S.; Kim, Y.H.; Yeom, H.S.; Hwang, I.S.; Kwon, J.W.; Park, Y.J.; Gwak, J.; Park, O. Coronavirus Disease-19 (COVID-19) 6-month outbreak infection report as of July 19, 2020, in the Republic of Korea. Public Health Wkly. Rep. 2020, 13, 2662–2669. [Google Scholar]
- Korea Center for Disease Control and Prevention. Daily Brief Report. Available online: http://www.kdca.go.kr/board/board.es?mid=a20501000000&bid=0015 (accessed on 26 March 2021).
- Serafini, G.; Parmigiani, B.; Amerio, A.; Aguglia, A.; Sher, L.; Amore, M. The psychological impact of COVID-19 on the mental health in the general population. QJM 2020, 113, 531–537. [Google Scholar] [CrossRef]
- Luo, M.; Guo, L.; Yu, M.; Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public: A systematic review and meta-analysis. Psychiatry Res. 2020, 291, 1–17. [Google Scholar] [CrossRef]
- Setiawati, Y.; Wahyuhadi, J.; Joestandari, F.; Maramis, M.M.; Atika, A. Anxiety and resilience of healthcare workers during COVID-19 pandemic in Indonesia. J. Multidiscip. Healthc. 2020, 14, 1–8. [Google Scholar] [CrossRef]
- Saqib, M.A.; Siddiqui, S.; Qasim, M.; Jamil, M.A.; Rafique, I.; Awan, U.A.; Ahmad, H.; Afzal, M.S. Effect of COVID-19 lockdown on patients with chronic diseases. Diabetes Metab. Syndr. 2020, 14, 1621–1623. [Google Scholar] [CrossRef]
- Kwon, H.M.; Kim, T.H.; Choi, M.R.; Kim, B.J.; Kim, H.W.; Song, O.S.; Eun, H.J. The effects of MERS (Middle East Respiratory Syndrome) event on the psychosocial wellbeing of healthcare workers and the public with the mediating effect of resilience. Korean J. Psychosom. Med. 2017, 25, 111–119. [Google Scholar] [CrossRef]
- Jose, R.; Narendran, M.; Bindu, A.; Beevi, N.; Manju, L.; Benny, P. Public perception and preparedness for the pandemic COVID 19: A health belief model approach. Clin. Epidemiol. Glob. Health 2021, 9, 41–46. [Google Scholar] [CrossRef]
- Roy, D.; Tripathy, S.; Kar, S.K.; Sharma, N.; Verma, S.K.; Kaushal, V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J. Psychiatr. 2020, 291, 1–9. [Google Scholar] [CrossRef]
- Holingue, C.; Badillo-Goicoechea, E.; Riehm, K.E.; Veldhuis, C.B.; Thrul, J.; Johnson, R.M.; Fallin, M.D.; Kreuter, F.; Stuart, E.A.; Kalb, L.G. Mental distress during the COVID-19 pandemic among US adults without a pre-existing mental health condition: Findings from American trend panel survey. Prev. Med. 2020, 139, 1–8. [Google Scholar] [CrossRef]
- Kimhi, S.; Marciano, H.; Eshel, Y.; Adini, B. Resilience and demographic characteristics predicting distress during the COVID-19 crisis. Soc. Sci. Med. 2020, 265, 113389. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Cho, J.H. Correlation between preventive health behaviors and psycho-social health on the activities of South Koreans in the COVID-19 crisis. Int. J. Environ. Res. Public Health 2020, 17, 4066. [Google Scholar] [CrossRef]
- Bonanno, G.A.; Galea, S.; Bucciarelli, A.; Vlahov, D. What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. J. Consult. Clin. Psychol. 2007, 75, 671–682. [Google Scholar] [CrossRef]
- Paredes, M.R.; Apaolaza, V.; Fernandez-Robin, C.; Hartmann, P.; Yañez-Martinez, D. The impact of the COVID-19 pandemic on subjective mental well-being: The interplay of perceived threat, future anxiety and resilience. Pers. Individ. Dif. 2021, 170, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Erkin, Ö.; Özsoy, S. Validity and reliability of health belief model applied to influenza. Acad. Res. Int. 2012, 2, 31. [Google Scholar]
- Shin, S.H. Relationships between health promoting lifestyle, health belief about emerging infectious disease and hygiene behavior of college students. J. Korea Converg. Soc. 2019, 10, 285–293. [Google Scholar] [CrossRef]
- Yıldırım, M.; Güler, A. COVID-19 severity, self-efficacy, knowledge, preventive behaviors, and mental health in Turkey. Death Stud. 2020, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Ye, Y.; Wang, R.; Feng, D.; Wu, R.; Li, Z.; Long, C.; Feng, Z.; Tang, S. The recommended and excessive preventive behaviors during the COVID-19 pandemic: A community-based online survey in China. Int. J. Environ. Res. Public Health 2020, 17, 6953. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.U.; Shah, S.; Ahmad, A.; Fatokun, O. Knowledge and attitude of healthcare workers about middle east respiratory syndrome in multispecialty hospitals of Qassim, Saudi Arabia. BMC Public Health 2014, 14, 1–7. [Google Scholar] [CrossRef]
- Lee, M.; You, M. Psychological and behavioral responses in South Korea during the early stages of coronavirus disease 2019 (COVID-19). Int. J. Environ. Res. Public Health 2020, 17, 2977. [Google Scholar] [CrossRef] [PubMed]
- Shahnazi, H.; Ahmadi-Livani, M.; Pahlavanzadeh, B.; Rajabi, A.; Hamrah, M.S.; Charkazi, A. Assessing preventive health behaviors from COVID-19: A cross sectional study with health belief model in Golestan Province, Northern of Iran. Infect. Dis. Poverty 2020, 9, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Korea Center for Disease Control and Prevention. Response Guidance for Local Government to Prevent and Control the Spread of COVID-19, 7th ed. Available online: http://www.kdca.go.kr/menu.es?mid=a20507020000 (accessed on 26 March 2021).
- Connor, K.M.; Davidson, J.R. Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC). Depress. Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Baek, H.S.; Lee, K.U.; Joo, E.J.; Lee, M.Y.; Choi, K.S. Reliability and validity of the Korean version of the Connor-Davidson Resilience Scale. Psychiatry Investig. 2010, 7, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.J. Standardization of Collection and Measurement for Heath Data; Kyechukmunhwasa: Seoul, Korea, 2000; pp. 121–159. [Google Scholar]
- Park, J.H.; Chang, S.J.; Choi, S. Correlation between knowledge, attitude, and compliance of preventive behaviors regarding Middle East Respiratory Syndrome among nursing students. J. Korean Biol. Nurs. Sci. 2018, 20, 252–260. [Google Scholar] [CrossRef][Green Version]
- Tedeschi, R.G.; Cann, A.; Taku, K.; Senol, D.E.; Calhoun, L.G. The posttraumatic growth inventory: A revision integrating existential and spiritual change. J. Trauma. Stress 2017, 30, 11–18. [Google Scholar] [CrossRef]
- Torrente, F.; Yoris, A.; Low, D.M.; Lopez, P.; Bekinschtein, P.; Manes, F.; Cetkovich, M. Sooner than you think: A very early affective reaction to the COVID-19 pandemic and quarantine in Argentina. J. Affect. Disord 2021, 282, 495–503. [Google Scholar] [CrossRef]
- Milstein, G. Disasters, Psychological Traumas, and Religions: Resiliencies Examined. Psychol. Trauma 2019, 11, 559–662. [Google Scholar] [CrossRef] [PubMed]
- Korean Statistical. Information Service. Available online: https://kosis.kr/index/index.do (accessed on 11 April 2021).
- Kim, Y.J.; Kang, S.W. The quality of life, psychological health, and occupational calling of Korean workers: Differences by the new classes of occupation emerging amid the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2020, 17, 5689. [Google Scholar] [CrossRef] [PubMed]
- Babore, A.; Lombardi, L.; Viceconti, M.L.; Pignataro, S.; Marino, V.; Crudele, M.; Candelori, C.; Bramanti, M.; Trumello, C. Psychological effects of the COVID-2019 pandemic: Perceived stress and coping strategies among healthcare professionals. Psychiatry Res. 2020, 293, 113366. [Google Scholar] [CrossRef] [PubMed]
| Variables | Total | Daegu (n = 152) | Non-Daegu (n = 186) | t(p) |
|---|---|---|---|---|
| Mean ± SD | ||||
| Knowledge of COVID-19 | 9.40 ± 1.19 | 9.32 ± 1.15 | 9.46 ± 1.23 | −1.03 (0.302) |
| Health belief | 3.45 ± 0.34 | 3.50 ± 0.37 | 3.41 ± 0.31 | 2.34 (0.020) |
| Susceptibility | 3.66 ± 0.64 | 3.91 ± 0.71 | 3.44 ± 0.48 | 6.97 (<0.001) |
| Seriousness | 4.31 ± 0.60 | 4.39 ± 0.56 | 4.23 ± 0.61 | 2.38 (0.018) |
| Benefits | 3.85 ± 0.66 | 3.77 ± 0.76 | 3.92 ± 0.57 | −2.12 (0.034) |
| Barriers | 2.72 ± 0.63 | 2.66 ± 0.57 | 2.77 ± 0.64 | −1.69 (0.093) |
| Cue to Actions | 2.87 ± 0.84 | 2.88 ± 0.92 | 2.87 ± 0.77 | 0.05 (0.962) |
| Resilience | 63.42 ± 11.23 | 62.43 ± 11.51 | 64.23 ± 10.96 | −1.47 (0.143) |
| Hardness | 2.41 ± 0.53 | 2.38 ± 0.52 | 2.44 ± 0.53 | −1.01 (0.312) |
| Persistence | 2.63 ± 0.49 | 2.56 ± 0.49 | 2.69 ± 0.48 | −2.40 (0.017) |
| Optimism | 2.58 ± 0.60 | 2.60 ± 0.62 | 2.57 ± 0.58 | 0.40 (0.689) |
| Support | 2.88 ± 0.61 | 2.79 ± 0.67 | 2.96 ± 0.54 | −2.57 (0.011) |
| Spirituality | 2.28 ± 0.75 | 2.28 ± 0.76 | 2.29 ± 0.74 | −0.07 (0.948) |
| Psychosocial stress | 33.45 ± 8.23 | 33.03 ± 9.44 | 33.79 ± 7.10 | −0.83 (0.410) |
| Severity | n (%) | n (%) | n (%) | |
| Healthy group (≤8) | 4 (1.2) | 3 (2.0) | 1 (0.5) | |
| Potential stress group (9–26) | 57 (16.9) | 32 (21.0) | 25 (13.5) | |
| High-risk stress group (≥27) | 277 (82.0) | 117 (77.0) | 160 (86.0) |
| Characteristic | Category | n (%) | Knowledge of COVID-19 | Health Belief | Resilience | Psychosocial Stress | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| M ± SD | t/F(p) Sheffé | M ± SD | t/F(p) Sheffé | M ± SD | t/F(p) Sheffé | M ± SD | t/F(p) Sheffé | |||
| Sex | Male | 127 (37.6) | 9.32 ± 1.22 | −1.48 (0.141) | 3.42 ± 0.32 | −2.01 (0.045) | 63.03 ± 11.67 | −0.82 (0.413) | 33.95 ± 7.97 | 0.88 (0.381) |
| Female | 211 (62.4) | 9.52 ± 1.13 | 3.50 ± 0.37 | 64.06 ± 10.45 | 33.14 ± 8.39 | |||||
| Age | 20–29 a | 65 (19.2) | 9.15 ± 1.29 | 2.98 (0.019) n.s | 3.39 ± 0.32 | 3.72 (0.006) a,b,c < e | 62.25 ± 14.44 | 0.30 (0.879) | 31.85 ± 9.21 | 1.69 (0.152) |
| 30–39 b | 134 (39.6) | 9.63 ± 1.21 | 3.45 ± 0.33 | 63.59 ± 10.46 | 33.17 ± 7.44 | |||||
| 40–49 c | 61 (18.1) | 9.33 ± 1.21 | 3.40 ± 0.30 | 63.51 ± 11.62 | 33.66 ± 8.70 | |||||
| 50–59 d | 47 (13.9) | 9.40 ± 1.17 | 3.45 ± 0.33 | 63.53 ± 8.49 | 33.83 ± 8.24 | |||||
| 60–65 e | 31 (9.2) | 9.00 ± 0.58 | 3.66 ± 0.47 | 64.77 ± 9.99 | 33.97 ± 8.04 | |||||
| Marital status | Unmarried | 98 (29.0) | 9.32 ± 1.22 | −0.79 (0.438) | 3.46 ± 0.36 | 1.16 (0.245) | 62.73 ± 11.17 | 0.64 (0.525) | 32.33 ± 8.47 | −1.60 (0.110) |
| Married | 240 (71.0) | 9.43 ± 1.18 | 3.41 ± 0.31 | 63.70 ± 9.26 | 33.90 ± 8.11 | |||||
| Education level | High school a | 111 (32.8) | 9.14 ± 0.96 | 7.07 (0.001) a,b < c | 3.54 ± 0.37 | 6.76 (0.001) b,c < a | 63.37 ± 12.09 | 0.31 (0.737) | 36.43 ± 0.71 | 1.68 (0.188) |
| College/university b | 204 (60.4) | 9.46 ± 1.26 | 3.41 ± 0.33 | 63.25 ± 10.93 | 33.33 ± 7.43 | |||||
| Graduate school c | 23 (6.8) | 10.09 ± 1.28 | 3.32 ± 0.29 | 65.17 ± 9.63 | 33.04 ± 9.73 | |||||
| Religious affiliation | Yes | 119 (35.2) | 9.21 ± 1.06 | −2.23 (0.026) | 3.47 ± 0.36 | 0.73 (0.465) | 67.34 ± 10.61 | 4.90 (0.001) | 32.44 ± 8.31 | −3.09 (0.002) |
| No | 219 (64.8) | 9.50 ± 1.25 | 3.44 ± 0.34 | 61.28 ± 10.10 | 35.30 ± 7.79 | |||||
| Number of family members | 1 | 25 (7.4) | 9.39 ± 1.19 | −0.54 (0.591) | 3.68 ± 0.40 | 3.52 (0.055) | 64.84 ± 8.65 | 0.66 (0.511) | 31.88 ± 6.43 | −1.24 (0.226) |
| ≥2 | 313 (92.6) | 9.52 ± 1.26 | 3.43 ± 0.33 | 63.30 ± 11.41 | 33.57 ± 8.36 | |||||
| Occupation | Yes | 224 (66.3) | 9.54 ± 1.04 | 1.63 (0.105) | 3.42 ± 0.32 | −1.74 (0.083) | 62.95 ± 11.78 | −1.13 (0.261) | 33.46 ± 8.88 | .044 (0.965) |
| No | 114 (33.7) | 9.33 ± 1.26 | 3.49 ± 0.39 | 64.33 ± 10.04 | 33.42 ± 6.83 | |||||
| Monthly household income (won/month) | <3 million a | 84 (24.9) | 9.20 ± 1.23 | 1.50 (0.225) | 3.46 ± 0.34 | 0.56 (0.573) | 66.25 ± 9.20 | 13.53 (<0.001) c < b < a | 29.49 ± 8.51 | 20.92(<0.001) a < b < c |
| 3–5 million b | 112 (33.1) | 9.45 ± 1.23 | 3.46 ± 0.34 | 63.51 ± 12.26 | 32.78 ± 8.37 | |||||
| >5 million c | 142 (42.0) | 9.47 ± 1.13 | 3.41 ± 0.35 | 58.50 ± 11.43 | 36.32 ± 6.80 | |||||
| Subjective health status | Healthy | 292 (86.4) | 9.43 ± 1.15 | 1.05 (0.296) | 3.48 ± 0.37 | 0.62 (0.535) | 64.04 ± 10.71 | 2.40 (0.020) | 27.24 ± 7.91 | −5.73 (0.001) |
| Unhealthy | 46 (13.6) | 9.20 ± 1.42 | 3.44 ± 0.34 | 59.48 ± 12.13 | 34.42 ± 7.86 | |||||
| Channel of COVID-19 information | Mass media | 205 (60.6) | 9.70 ± 0.71 | 0.36 (0.698) | 3.34 ± 0.24 | 0.62 (0.538) | 62.13 ± 8.68 | 0.10 (0.908) | 33.50 ± 7.53 | 0.62 (0.539) |
| Internet/SNS | 125 (37.0) | 9.39 ± 1.20 | 3.47 ± 0.34 | 63.68 ± 12.51 | 33.57 ± 9.21 | |||||
| Acquaintances/hospitals | 8 (2.4) | 9.39 ± 1.20 | 3.44 ± 0.35 | 63.31 ± 10.50 | 30.25 ± 8.23 | |||||
| Variable | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| 1. Knowledge of COVID-19 | 1 | |||
| 2. Health belief | −0.057 (0.294) | 1 | ||
| 3. Resilience | 0.034 (0.537) | 0.218 (<0.001) | 1 | |
| 4. Psychosocial stress | −0.059 (0.227) | −0.103 (0.060) | −0.578 (<0.001) | 1 |
| Variables | B | SE | β | t | p |
|---|---|---|---|---|---|
| (Constant) | 11.95 | 2.23 | 5.36 | <0.001 | |
| Resilience | −0.37 | 0.03 | −0.51 | −11.16 | <0.001 |
| Religion * | −0.05 | 0.76 | −0.01 | 0.07 | 0.943 |
| Subjective health status ** | −4.77 | 1.04 | −0.20 | −4.59 | <0.001 |
| Monthly household income *** | |||||
| <3 million | −3.22 | 0.92 | −0.17 | −3.48 | 0.001 |
| 3~5 million | −2.01 | 0.82 | −0.12 | −2.45 | 0.015 |
| R2 = 0.368, Adj R2 = 0.398, F = 45.50, p < 0.001, Durbin–Watson = 1.98 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.; Lee, O. Influencing Factors of Psychosocial Stress among Korean Adults during the COVID-19 Outbreak. Int. J. Environ. Res. Public Health 2021, 18, 6153. https://doi.org/10.3390/ijerph18116153
Kim J, Lee O. Influencing Factors of Psychosocial Stress among Korean Adults during the COVID-19 Outbreak. International Journal of Environmental Research and Public Health. 2021; 18(11):6153. https://doi.org/10.3390/ijerph18116153
Chicago/Turabian StyleKim, Jina, and Ogcheol Lee. 2021. "Influencing Factors of Psychosocial Stress among Korean Adults during the COVID-19 Outbreak" International Journal of Environmental Research and Public Health 18, no. 11: 6153. https://doi.org/10.3390/ijerph18116153
APA StyleKim, J., & Lee, O. (2021). Influencing Factors of Psychosocial Stress among Korean Adults during the COVID-19 Outbreak. International Journal of Environmental Research and Public Health, 18(11), 6153. https://doi.org/10.3390/ijerph18116153






