Relationship between Physical Activity and Cardiovascular Risk Factors: A Cross-Sectional Study among Low-Income Housewives in Kuala Lumpur
Abstract
1. Introduction
2. Materials and Methods
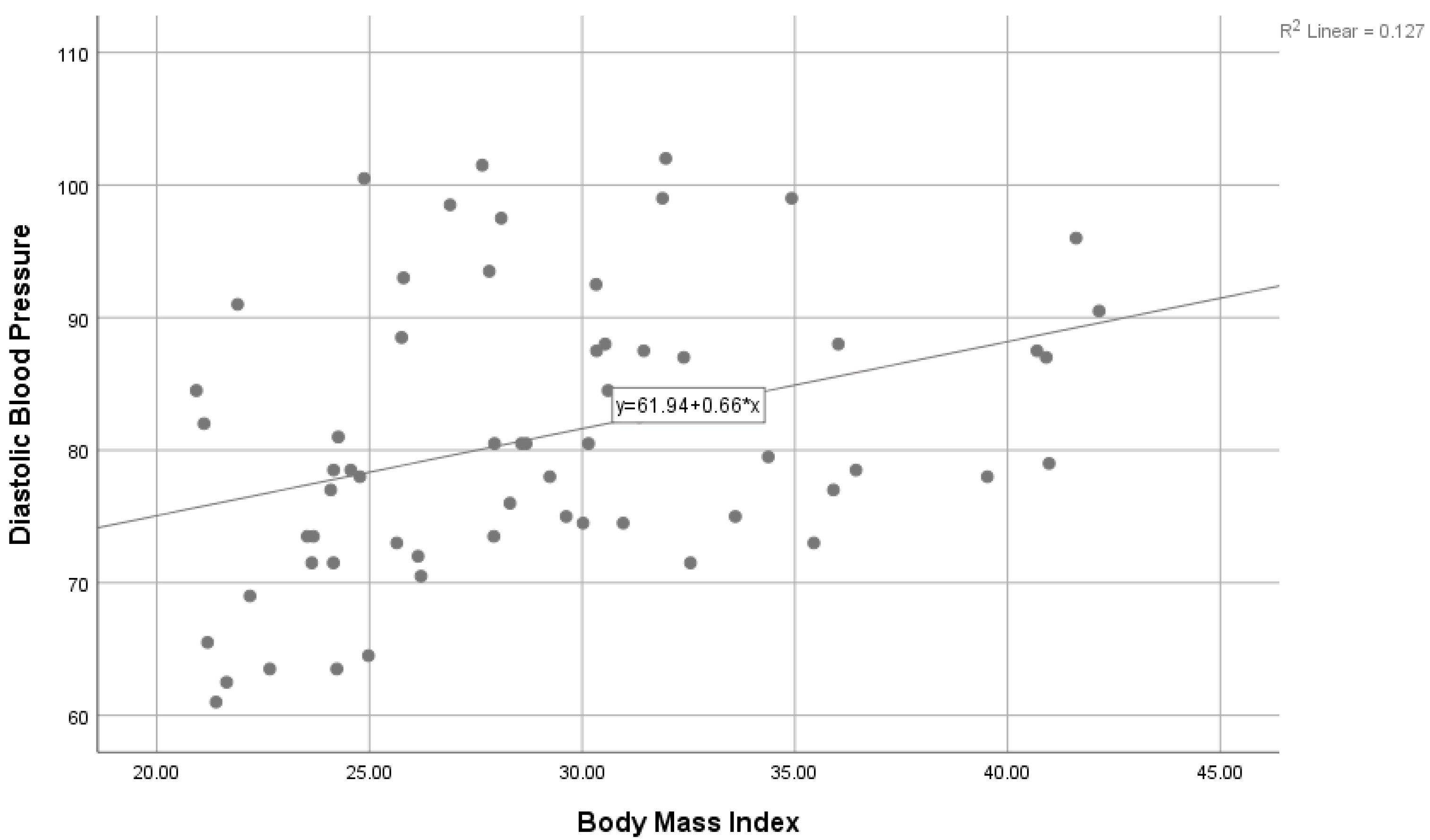
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mensah, G.A.; Roth, G.A.; Fuster, V. The global burden of cardiovascular diseases and risk factors: 2020 and beyond. J. Am. Coll. Cardiol. 2019, 74, 2529–2532. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Cardiovascular Diseases (CVDs). 2017. Available online: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 23 September 2019).
- World Health Organization. Noncommunicable Diseases (NCD) Country Profiles. 2018. Available online: https://www.who.int/nmh/countries/mys_en.pdf (accessed on 11 December 2019).
- Ghazali, S.M.; Seman, Z.; Cheong, K.C.; Hock, L.K.; Manickam, M.; Kuay, L.K.; Yusoff, A.F.; Mustafa, F.I.; Mustafa, A.N. Sociodemographic factors associated with multiple cardiovascular risk factors among Malaysian adults. BMC Public Health 2015, 15, 68. [Google Scholar] [CrossRef] [PubMed]
- Mohammadnezhad, M.; Mangum, T.; May, W.; Lucas, J.J.; Ailson, S. Common modifiable and non-modifiable risk factors of cardiovascular disease (CVD) among Pacific countries. World J. Cardiovasc. Surg. 2016, 6, 153–170. [Google Scholar] [CrossRef]
- Bahagian Pendidikan Kesihatan, Kementerian Kesihatan Malaysia. Garis Panduan Aktiviti Fizikal Malaysia. 2017. Available online: https://mdes.org.my/wp-content/uploads/2017/07/garis-panduan-aktiviti-fizikal-2017.pdf (accessed on 10 October 2019).
- Kim, H.C.; Oh, S.M. Noncommunicable diseases: Current status of major modifiable risk factors in Korea. J. Prev. Med. Public Health 2013, 46, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Colberg, S.R.; Sigal, R.J.; Yardley, J.E.; Riddell, M.C.; Dunstan, D.W.; Dempsey, P.C.; Horton, E.S.; Castorino, K.; Tate, D.F. Physical activity/exercise and diabetes: A position statement of the American Diabetes Association. Diabetes Care 2016, 39, 2065–2079. [Google Scholar] [CrossRef] [PubMed]
- Chan, Y.Y.; Lim, K.K.; Lim, K.H.; Teh, C.H.; Kee, C.C.; Cheong, S.M.; Khoo, Y.Y.; Baharudin, A.; Ling, M.Y.; Omar, M.A.; et al. Physical activity and overweight/obesity among Malaysian adults: Findings from the 2015 National Health and morbidity survey (NHMS). BMC Public Health 2017, 17, 733. [Google Scholar] [CrossRef]
- Hornbuckle, L.M.; Liu, P.Y.; Ilich, J.Z.; Kim, J.S.; Arjmandi, B.H.; Panton, L.B. Effects of resistance training and walking on cardiovascular disease risk in African-American women. Med. Sci. Sports Exerc. 2012, 44, 525–533. [Google Scholar] [CrossRef]
- Anil, O.M.; Yadav, R.S.; Shrestha, N.; Koirala, S.; Shrestha, S.; Nikhil, O.M.; Baidar, M.; Chaudhary, N.; Jaishwal, C.; Yadav, N.S.; et al. Prevalence of cardiovascular risk factors in apparently healthy urban adult population of Kathmandu. J. Nepal Health Res. Counc. 2019, 16, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Moniruzzaman, M.; Ahmed, M.M.; Zaman, M.M. Physical activity levels and associated socio-demographic factors in Bangladeshi adults: A cross-sectional study. BMC Public Health 2017, 17, 59. [Google Scholar] [CrossRef]
- Najafipour, H.; Moazenzadeh, M.; Afshari, M.; Nasri, H.R.; Khaksari, M.; Forood, A.; Mirzazadeh, A. The prevalence of low physical activity in an urban population and its relationship with other cardiovascular risk factors: Findings of a community-based study (KERCADRS) in southeast of Iran. ARYA Atheroscler. 2016, 12, 212–219. [Google Scholar]
- Omar, A.; Husain, M.N.; Jamil, A.T.; Mohamad Nor, N.S.; Ambak, R.; Fazliana, M.; Ahamad Zamri, N.L.; Aris, T. Effect of physical activity on fasting blood glucose and lipid profile among low income housewives in the MyBFF@ home study. BMC Women’s Health 2018, 18, 79–98. [Google Scholar] [CrossRef]
- Prihartono, N.A.; Fitriyani, F.; Riyadina, W. Cardiovascular disease risk factors among blue and white-collar workers in Indonesia. Acta Med. Indones. 2018, 50, 96–103. [Google Scholar] [PubMed]
- Nakhaie, M.R.; Koor, B.E.; Salehi, S.O.; Karimpour, F. Prediction of cardiovascular disease risk using framingham risk score among office workers, Iran, 2017. Saudi J. Kidney Dis. Transpl. 2018, 29, 608–614. [Google Scholar]
- Martínez, S.M.A.; Leiva, O.A.M.; Sotomayor, C.C.; Victoriano, R.T.; Von Chrismar, P.A.M.; Pineda, B.S. Cardiovascular risk factors among university students. Rev. Med. Chil. 2012, 140, 426–435. [Google Scholar]
- Scheuch, K.; Haufe, E.; Seibt, R. Teachers’ health. Dtsch. Ärzteblatt Int. 2015, 112, 347–356. [Google Scholar] [CrossRef] [PubMed]
- Chu, A.H.Y.; Moy, F.M. Reliability and validity of the Malay International Physical Activity Questionnaire (IPAQ-M) among a Malay population in Malaysia. Asia Pac. J. Public Health 2015, 27, NP2381–NP2389. [Google Scholar] [CrossRef] [PubMed]
- IPAQ. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ)—Short and Long Forms, Revised on November 2005. 2005. Available online: https://docs.google.com/viewer?a=v&pid=sites&srcid=ZGVmYXVsdGRvbWFpbnxaGVpcGFxfGd4OjE0NDgxMDk3NDU1YWRlZTM (accessed on 15 October 2019).
- Craig, E.; Bland, R.; Reilly, J. Objectively measured physical activity levels of children and adolescents in rural South Africa: High volume of physical activity at low intensity. Appl. Physiol. Nutr. Metab. 2013, 38, 81–84. [Google Scholar] [CrossRef]
- IDF. The IDF Consensuses Worldwide Definition of The Metabolic Syndrome; International Diabetes Federation: Brussels, Belgium, 2006.
- Institute for Public Health. National Health and Morbidity Survey (NHMS) 2019: Vol. I: NCDs–Non-Communicable Diseases: Risk Factors and Other Health Problems; Institute for Public Health: Kuala Lumpur, Malaysia, 2019. [Google Scholar]
- Institute for Public Health. National Health and Morbidity Survey NHMS. Summary on NHMS Report on Disease Prevalence; National Health and Morbidity Survey: Kuala Lumpur, Malaysia, 2015.
- Cochran, W.G. Sampling Techniques, 2nd ed.; John Wiley and Sons, Inc.: New York, NY, USA, 1963. [Google Scholar]
- WHO. Obesity and Overweight; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 11 December 2019).
- Aranceta-Bartrina, J.; Pérez-Rodrigo, C.; Alberdi-Aresti, G.; Ramos-Carrera, N.; Lázaro-Masedo, S. Prevalence of general obesity and abdominal obesity in the Spanish adult population (aged 25–64 years) 2014–2015: The ENPE study. Rev. Española Cardiol. 2016, 69, 579–587. [Google Scholar] [CrossRef]
- Harbuwono, D.S.; Pramono, L.A.; Yunir, E.; Subekti, I. Obesity and central obesity in Indonesia: Evidence from a national health survey. Med. J. Indones. 2018, 27, 114–120. [Google Scholar] [CrossRef]
- Ahmad, N.; Adam, S.I.; Nawi, A.M.; Hassan, M.R.; Ghazi, H.F. Abdominal obesity indicators: Waist circumference or waist-to-hip ratio in Malaysian adults population. Int. J. Prev. Med. 2016, 7, 82. [Google Scholar]
- Amiri, M.; Majid, H.A.; Hairi, F.; Thangiah, N.; Bulgiba, A.; Su, T.T. Prevalence and determinants of cardiovascular disease risk factors among the residents of urban community housing projects in Malaysia. BMC Public Health 2014, 14, S3. [Google Scholar] [CrossRef]
- Harris, H.; Ooi, Y.B.; Lee, J.S.; Matanjun, P. Non-communicable diseases among low income adults in rural coastal communities in Eastern Sabah, Malaysia. BMC Public Health 2019, 19, 554. [Google Scholar] [CrossRef]
- Su, T.T.; Amiri, M.; Mohd Hairi, F.; Thangiah, N.; Bulgiba, A.; Majid, H.A. Prediction of cardiovascular disease risk among low-income urban dwellers in metropolitan Kuala Lumpur, Malaysia. Biomed. Res. Int. 2015, 2015, 516984. [Google Scholar] [CrossRef] [PubMed]
- Mamani-Ortiz, Y.; San Sebastián, M.; Armaza, A.X.; Luizaga, J.M.; Illanes, D.E.; Ferrel, M.; Mosquera, P.A. Prevalence and determinants of cardiovascular disease risk factors using the WHO STEPS approach in Cochabamba, Bolivia. BMC Public Health 2019, 19, 786. [Google Scholar] [CrossRef]
- Mirzaei, M.; Mirzaei, M.; Sarsangi, A.R.; Bagheri, N. Prevalence of modifiable cardiovascular risk factors in Yazd inner-city municipalities. BMC Public Health 2020, 20, 134. [Google Scholar] [CrossRef]
- Aisyah Waheeda, R.; Rheshara, S.; Nik Nasreen, N.K.; Sabariah, A.H. Physical Activity Status of Community in Kg Hulu Chuchoh, Sungai Pelek, Sepang, Selangor, Malaysia. Int. Educ. Res. J. 2018, 6, 37–46. [Google Scholar]
- Cheah, Y.K.; Poh, B.K. The determinants of participation in physical activity in Malaysia. Osong Public Health Res. Perspect. 2014, 5, 20–27. [Google Scholar] [CrossRef] [PubMed]
- The, C.H.; Lim, K.K.; Chan, Y.Y.; Lim, K.H.; Azahadi, O.; Akmar, A.H.; Nadiah, Y.U.; Syafinaz, M.S.; Kee, C.C.; Yeo, P.S.; et al. The prevalence of physical activity and its associated factors among Malaysian adults: Findings from the National Health and Morbidity Survey 2011. Public Health 2014, 128, 416–423. [Google Scholar]
- Moschny, A.; Platen, P.; Klaaßen-Mielke, R.; Trampisch, U.; Hinrichs, T. Barriers to physical activity in older adults in Germany: A cross-sectional study. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 121. [Google Scholar] [CrossRef] [PubMed]
- Mathews, A.E.; Laditka, S.B.; Laditka, J.N.; Wilcox, S.; Corwin, S.J.; Liu, R.; Friedman, D.B.; Hunter, R.; Tseng, W.; Logsdon, R.G. Older adults’ perceived physical activity enablers and barriers: A multicultural perspective. J. Aging Phys. Act. 2010, 18, 119–140. [Google Scholar] [CrossRef]
- Jurakić, D.; Pedišić, Ž.; Andrijašević, M. Physical Activity of Croatian Population: Cross-Sectional Study Using International Physical Activity Questionnaire. Croat. Med. J. 2009, 50, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Beenackers, M.A.; Kamphuis, C.B.; Giskes, K.; Brug, J.; Kunst, A.E.; Burdorf, A.; Van Lenthe, F.J. Socioeconomic inequalities in occupational, leisure-time, and transport related physical activity among European adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 116. [Google Scholar] [CrossRef]
- Kari, J.T.; Pehkonen, J.; Hirvensalo, M.; Yang, X.; Hutri-Kähönen, N.; Raitakari, O.T.; Tammelin, T.H. Income and physical activity among adults: Evidence from self-reported and pedometer-based physical activity measurements. PLoS ONE 2015, 10, e0135651. [Google Scholar] [CrossRef]
- Chu, A.H.; Moy, F.M. Association between physical activity and metabolic syndrome among Malay adults in a developing country, Malaysia. J. Sci. Med. Sport 2014, 17, 195–200. [Google Scholar] [CrossRef]
- Jamil, A.T.; Ismail, A.; Idris, I.B.; Soo, K.C.; Teng, A.J.; Bahaman, N.A.; Fadzil, M.F. Levels of physical activity and its associated factors among health care workers. Malays. J. Public Health Med. 2016, 16, 127–133. [Google Scholar]
- Saat, N.Z.M.; Nor Farah, M.F.; Hanawi, S.A.; Mohd Radhi, S. The associations between daily steps and cardiovascular risk factors among female teachers. Malays J. Mov. Health Exerc. 2020, 9, 113. [Google Scholar]
- Zulkepli, Z.; Saat, N.Z.M.; Nor Farah, M.F.; Hanawi, S.A.; Zin, N.M. Relationship between physical activity level and cardiovascular risk factors among teachers. Asian J. Epidemiol. 2019, 12, 1–8. [Google Scholar] [CrossRef]
- Abdullah, M.; Saat, N.Z.M.; Nor Farah, M.F.; Hui, C.Y.; Kamaralzaman, S. Association between Walking and Cardiovascular Risk Factors in University Employees. J. Med. Sci. 2015, 15, 105. [Google Scholar] [CrossRef]
- Pang, Y.; Kartsonaki, C.; Du, H.; Millwood, I.Y.; Guo, Y.; Chen, Y.; Bian, Z.; Yang, L.; Walters, R.; Bragg, F.; et al. Physical activity, sedentary leisure time, circulating metabolic markers, and risk of major vascular diseases. Circ. Genom. Precis. Med. 2019, 12, e002527. [Google Scholar] [CrossRef]
- Earnest, C.P.; Artero, E.G.; Sui, X.; Lee, D.C.; Church, T.S.; Blair, S.N. Maximal estimated cardiorespiratory fitness, cardiometabolic risk factors, and metabolic syndrome in the aerobics center longitudinal study. In Mayo Clinic Proceedings; Elsevier: Amsterdam, The Netherlands, 2013; Volume 88, pp. 259–270. [Google Scholar]

| Characteristics | n (%) |
|---|---|
| Age | |
| 21–30 | 4 (6.3) |
| 31–40 | 14 (22.2) |
| 41–50 | 19 (30.2) |
| 51–60 | 26 (41.3) |
| Duration of Being a Housewife (years) | |
| 10 | 26 (41.3) |
| 11–20 | 9 (14.3) |
| >20 | 28 (44.4) |
| Number of Children | |
| 2 | 10 (15.9) |
| 3–4 | 30 (47.6) |
| 5 | 23 (36.5) |
| Education Level | |
| Primary | 9 (14.3) |
| Lower secondary | 11 (17.5) |
| Upper secondary | 41 (65.1) |
| Certificate and above | 2 (3.1) |
| Household Income | |
| RM 1000 | 10 (15.9) |
| RM 1001–RM 2000 | 29 (46.0) |
| >RM 2000 | 24 (38.1) |
| CVD Risk Factors | n (%) | Mean ± SD |
|---|---|---|
| BMI (kg m−2) | ||
| Underweight | 0 (0) | 29.10 ± 5.67 |
| Normal | 8 (12.7) | |
| Overweight | 18 (28.6) | |
| Obesity | 37 (58.7) | |
| WC (cm) | ||
| Normal (80 cm) | 12 (19.0) | 92.74 ± 16.40 |
| Obesity (>80 cm) | 51 (81.0) | |
| Systolic Blood Pressure (mm Hg) | ||
| Normal | 33 (52.4) | 122.90 ± 19.05 |
| Prehypertension | 21 (33.3) | |
| Hypertension stage I | 5 (7.9) | |
| Hypertension stage II | 4 (6.4) | |
| Diastolic Blood Pressure (mm Hg) | ||
| Normal | 32 (50.8) | 81.04 ± 10.43 |
| Prehypertension | 18 (28.6) | |
| Hypertension stage I | 10 (15.9) | |
| Hypertension stage II | 3 (4.7) | |
| FBG level (mmol L−1) | ||
| Normal | 31 (49.2) | 6.48 ± 2.81 |
| Prediabetes | 20 (31.7) | |
| Diabetes | 12 (19.1) | |
| TC Level (mmol L−1) | ||
| Normal | 58 (92.1) | 4.15 ± 0.72 |
| Borderline high | 4 (6.3) | |
| High | 1 (1.6) |
| Age Group A | Mean ± SD | ||
|---|---|---|---|
| 21–40 (n = 18) | 41–50 (n = 19) | 51–60 (n = 26) | |
| BMI (kg m−2) | 28.28 ± 6.37 | 30.30 ± 5.89 | 28.79 ± 5.13 |
| WC (cm) | 88.17 ± 11.29 | 95.35 ± 23.66 | 93.98 ± 10.68 |
| SBP (mm Hg) | 112.14 ± 11.29 | 123.74 ± 14.99 | 129.73 ± 22.78 |
| DBP (mm Hg) | 76.19 ± 9.14 | 84.24 ± 10.43 | 82.06 ± 10.44 |
| FBG level (mmol L−1) | 5.26 ± 0.61 | 7.00 ± 3.08 | 6.93 ± 3.32 |
| TC level (mmol L−1) | 3.98 ± 0.59 | 4.07 ± 0.64 | 4.33 ± 0.82 |
| Education Level | Mean ± SD | ||
| Primary and Lower Secondary (n = 20) | Upper Secondary and Above (n = 43) | ||
| BMI (kg m−2) | 28.09 ± 5.30 | 29.57 ± 5.83 | |
| WC (cm) | 92.63 ± 22.42 | 92.78 ± 13.02 | |
| SBP (mm Hg) | 122.05 ± 18.62 | 123.29 ± 19.45 | |
| DBP (mm Hg) | 79.30 ± 8.66 | 81.85 ± 11.16 | |
| FBG level (mmol L−1) | 6.32 ± 2.47 | 6.54 ± 2.97 | |
| TC level (mmol L−1) | 4.19 ± 0.99 | 4.13 ± 0.55 | |
| CVD Risk Factor | Mean ± SD | ||||
|---|---|---|---|---|---|
| ≤RM 1000 (n = 10) | RM 1001–RM 2000 (n = 29) | >RM 2000 (n = 24) | F | p-Value | |
| BMI (kg m−2) | 26.25 ± 5.83 | 29.59 ± 5.55 | 29.71 ± 5.63 | 1.54 | 0.22 |
| WC (cm) | 86.24 ± 8.20 | 92.55 ± 12.46 | 95.67 ± 21.96 | 1.18 | 0.32 |
| SBP (mm Hg) | 120.35 ± 17.23 | 123.38 ± 16.38 | 123.38 ± 23.06 | 0.10 | 0.90 |
| DBP (mm Hg) | 77.20 ± 8.35 | 83.24 ± 10.30 | 79.98 ± 11.09 | 1.47 | 0.24 |
| FBG level (mmol L−1) | 7.16 ± 4.63 | 6.50 ± 2.67 | 6.16 ± 1.97 | 0.44 | 0.67 |
| TC level (mmol L−1) | 4.02 ± 0.83 | 4.04 ± 0.54 | 4.34 ± 0.84 | 1.35 | 0.27 |
| Parameter | n (%) | Mean ± SD |
|---|---|---|
| Category of Physical Activity Level | ||
| Low | 57 (90.5) | - |
| Moderate | 4 (6.3) | - |
| High | 2 (3.2) | - |
| Physical Activity Level | ||
| Total physical activity level (MET-min/week) | - | 451.35 ± 617.78 |
| MVPA (MET-min/week) | - | 70.48 ± 282.36 |
| Sitting (h/day) | - | 2.92 ± 1.49 |
| Factors | Physical Activity Level | |||||
|---|---|---|---|---|---|---|
| n | Mean | Median | IQR | H | p-Value | |
| Age | ||||||
| 21–40 | 18 | 452 | 347 | 260 | ||
| 41–50 | 19 | 604.05 | 297 | 396 | ||
| >50 | 26 | 321.35 | 198 | 355 | 4.70 a | >0.05 |
| Education Level | ||||||
| Primary and lower secondary | 20 | 294.5 | 264 | 247 | ||
| Upper secondary and others | 43 | 513.56 | 240 | 445 | 393.00 b | >0.05 |
| Household Income | ||||||
| ≤RM 1000 | 10 | 250.90 | 214.50 | 334 | ||
| RM 1001–2000 | 29 | 352.14 | 198.00 | 256 | ||
| >RM 2000 | 24 | 635.50 | 396.00 | 656 | 3.62 a | >0.05 |
| Parameter | Coefficients | Std Error | 95% Confidence Interval | p-Value | |
|---|---|---|---|---|---|
| Intercept | 30.902 | 4.3320 | 22.412 | 39.393 | 0.000 |
| WC | 0.050 | 0.0737 | −0.094 | 0.195 | 0.495 |
| BMI | −0.092 | 0.1625 | −0.410 | 0.226 | 0.571 |
| FBG | −0.570 | 0.1360 | −0.836 | −0.303 | <0001 * |
| TC | −3.687 | 0.5994 | −4.862 | −2.512 | <0001 * |
| SBP | 0.090 | 0.0294 | 0.033 | 0.148 | 0.002 |
| DBP | −0.268 | 0.0489 | 22.412 | 39.393 | <0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohd Saat, N.Z.; Hanawi, S.A.; M. F. Farah, N.; Mohd Amin, H.; Hanafiah, H.; Shamsulkamar, N.S. Relationship between Physical Activity and Cardiovascular Risk Factors: A Cross-Sectional Study among Low-Income Housewives in Kuala Lumpur. Int. J. Environ. Res. Public Health 2021, 18, 6090. https://doi.org/10.3390/ijerph18116090
Mohd Saat NZ, Hanawi SA, M. F. Farah N, Mohd Amin H, Hanafiah H, Shamsulkamar NS. Relationship between Physical Activity and Cardiovascular Risk Factors: A Cross-Sectional Study among Low-Income Housewives in Kuala Lumpur. International Journal of Environmental Research and Public Health. 2021; 18(11):6090. https://doi.org/10.3390/ijerph18116090
Chicago/Turabian StyleMohd Saat, Nur Zakiah, Siti Aishah Hanawi, Nor M. F. Farah, Hazilah Mohd Amin, Hazlenah Hanafiah, and Nur Shazana Shamsulkamar. 2021. "Relationship between Physical Activity and Cardiovascular Risk Factors: A Cross-Sectional Study among Low-Income Housewives in Kuala Lumpur" International Journal of Environmental Research and Public Health 18, no. 11: 6090. https://doi.org/10.3390/ijerph18116090
APA StyleMohd Saat, N. Z., Hanawi, S. A., M. F. Farah, N., Mohd Amin, H., Hanafiah, H., & Shamsulkamar, N. S. (2021). Relationship between Physical Activity and Cardiovascular Risk Factors: A Cross-Sectional Study among Low-Income Housewives in Kuala Lumpur. International Journal of Environmental Research and Public Health, 18(11), 6090. https://doi.org/10.3390/ijerph18116090






