The Risk of Hospitalization in COVID-19 Patients Can Be Predicted by Lung Ultrasound in Primary Care
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
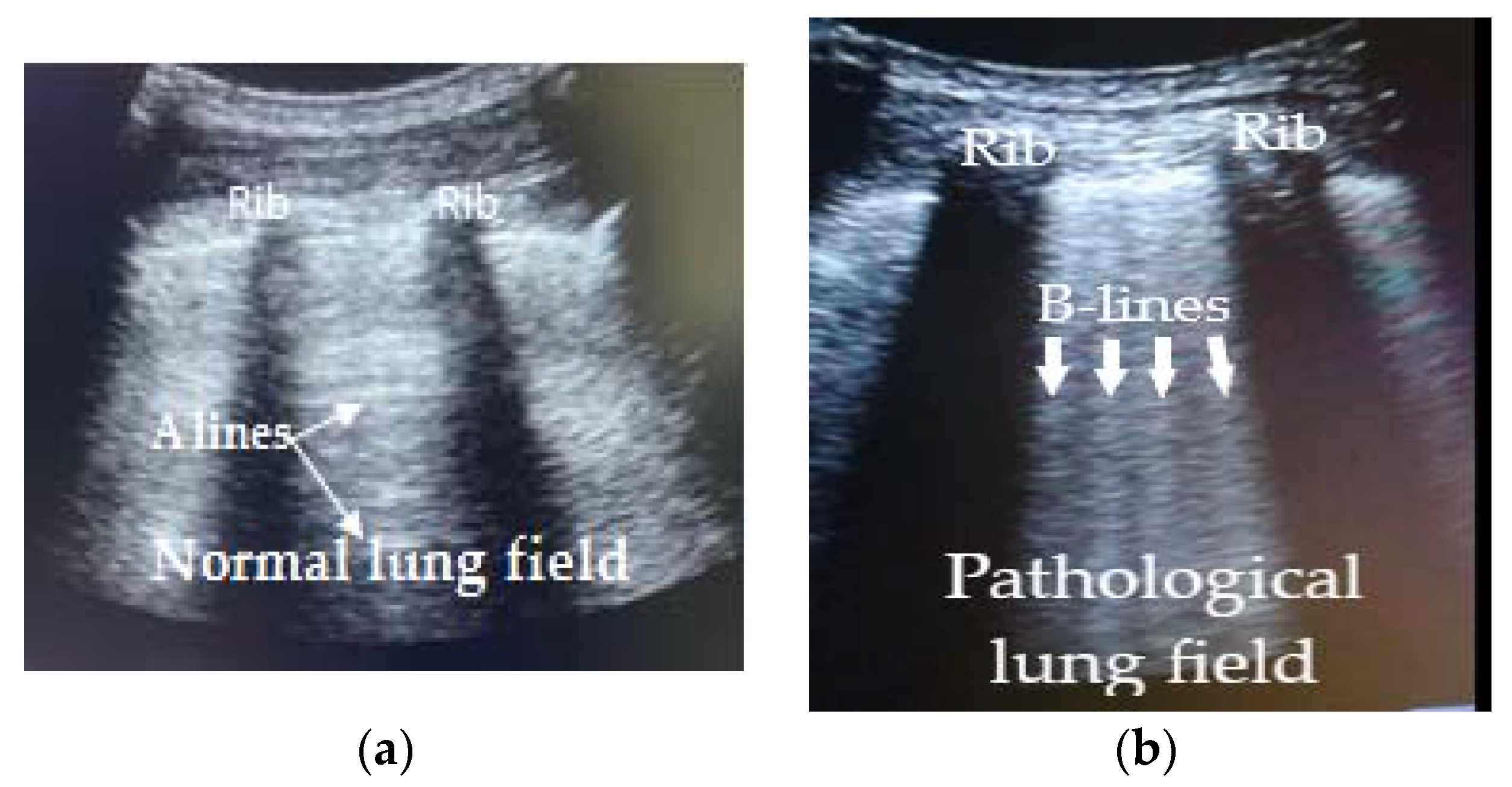
2.2. Imaging Protocol and Interpretation
2.3. Ethical Approval
2.4. Statistical Analysis
3. Results
3.1. Patient Demographics and Analysis of Symptoms
3.1.1. Symptom Distribution
3.1.2. Ultrasound Patterns Observed According to the Presence and Arrangement of the B Lines in Patients with Positive RT-PCR
3.1.3. Evolution of LUS Patterns in Patients with Positive RT-PCR
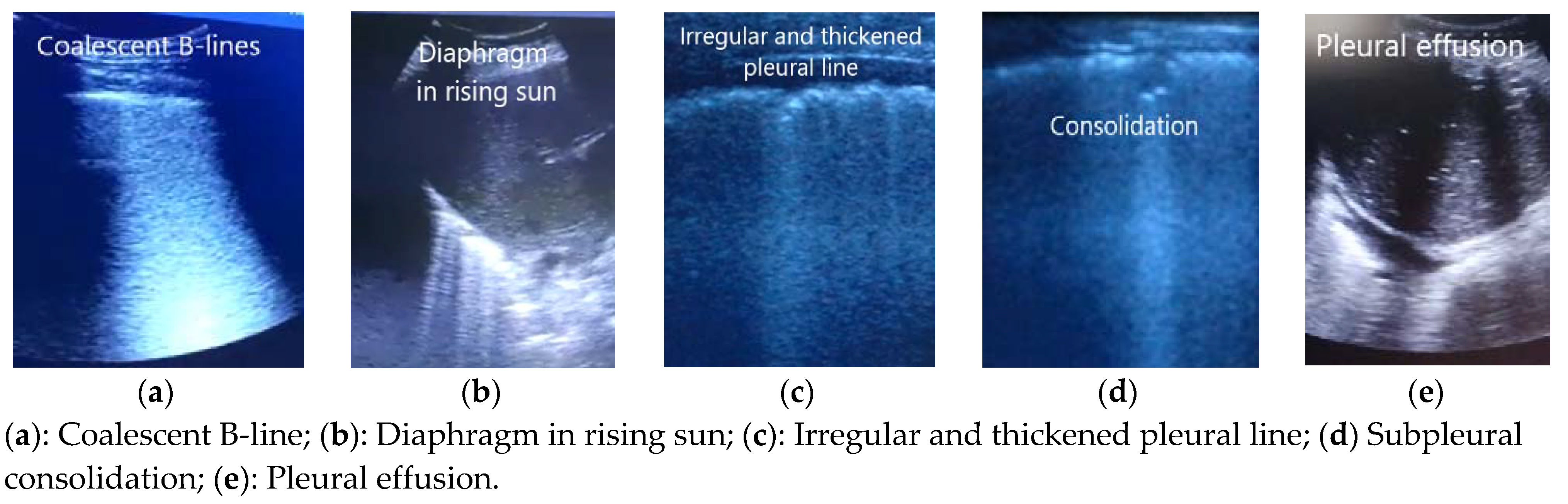
3.1.4. Other Ultrasound Findings in Patients with Positive RT-PCR
3.1.5. LUS Findings as Either Risk or Protector Factors, for Hospital Admission of Patients with Positive RT-PCR
3.1.6. Distribution of Other Diagnoses According LUS Pattern in Patients with Negative RT-PCR
4. Discussion
4.1. Summary
4.2. Strengths and Limitations
4.3. Comparison with Existing Literature
4.4. Implications for Research and Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19–11 March 2020. 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19–11-march-2020 (accessed on 20 January 2021).
- Spain Ministry of Health. Informe Sobre la Situación de COVID-19 en España. Informe COVID-19 nº8. 11 de Marzo de 2020. Available online: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/INFORMES/Informes%20COVID-19/Informe%20COVID-19.%20N%c2%ba%208_11marzo2020_ISCIII.pdf (accessed on 20 January 2021).
- Spain Ministry of Health. COVID-19 Update Number 60. 31 March 2020. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/Actualizacion_61_COVID-19.pdf (accessed on 20 January 2021).
- Xu, X.W.; Wu, X.X.; Jiang, X.G.; Xu, K.J.; Ying, L.J.; Ma, C.L.; Li, S.B.; Wang, H.Y.; Zhang, S.; Gao, H.N.; et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: Retrospective case series. BMJ 2020, 368, 32075786. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Pan, F.; Tianhe, Y.; Sun, P.; Gui, S.; Liang, B.; Li, L.; Zheng, D.; Wang, J.; Hesketh, R.L.; Yang, L. Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19). Radiology 2020, 295, 715–721. [Google Scholar] [CrossRef] [PubMed]
- Peng, Q.Y.; Wang, X.T.; Zhang, L.N. Findings of lung ultrasonography of novel corona virus pneumonia during the 2019–2020 epidemic. Intensive Care Med. 2020, 46, 849–850. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Wang, S.; Liu, Y.; Zhang, Y.; Zheng, C.; Zheng, Y.; Zhang, C.; Min, W.; Yu, M.; Hu, M. A Preliminary Study on the Ultrasonic Manifestations of Peripulmonary Lesions of Non-Critical Novel Coronavirus Pneumonia (COVID-19). SSRN. 2020. Available online: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3544750 (accessed on 5 April 2021). [CrossRef]
- Volpicelli, G.; Elbarbary, M.; Blaivas, M.; Lichtenstein, D.A.; Mathis, G.; Kirkpatrick, A.W.; Melniker, L.; Gargani, L.; Noble, V.E.; Via, G.; et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012, 38, 577–591. [Google Scholar] [CrossRef] [PubMed]
- Ma, I.W.Y.; Hussain, A.; Wagner, M.; Walker, B.; Chee, A.; Arishenkoff, S.; Buchanan, B.; Liu, R.B.; Gregory, M.; Wong, T.; et al. Canadian Internal Medicine Ultrasound (CIMUS) Expert Consensus Statement on the Use of Lung Ultrasound for the Assessment of Medical Inpatients with Known or Suspected Coronavirus Disease 2019. J. Ultrasound Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Ji, L.; Cao, C.; Gao, Y.; Zhang, W.; Xie, Y.; Duan, Y.; Kong, S.; You, M.; Ma, R.; Jiang, L.; et al. Prognostic value of bedside lung ultrasound score in patients with COVID-19. Crit. Care 2020, 24, 700. [Google Scholar] [CrossRef] [PubMed]
- Lichter, Y.; Topilsky, Y.; Taieb, P.; Banai, A.; Hochstadt, A.; Merdler, I.; Oz, A.G.; Vine, J.; Goren, O.; Cohen, B.; et al. Lung ultrasound predicts clinical course and outcomes in COVID-19 patients. Intensive Care Med. 2020, 46, 1873–1883. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Yu, K.; Zhao, Q.; Tian, R.; Xie, H.; Xie, L.; Deng, P.; Xie, G.; Bao, A.; Du, J. Lung Ultrasound Score in Evaluating the Severity of Coronavirus Disease 2019 (COVID-19) Pneumonia. Ultrasound Med. Biol. 2020, 46, 2938–2944. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, M.; Al-Shokri, S.; Yousaf, Z.; Danjuma, M.; Parambil, J.; Mohamed, S.; Mubasher, M.; Dauleh, M.M.; Hasanain, B.; AlKahlout, M.A. Frequency of Abnormalities Detected by Point-of-Care Lung Ultrasound in Symptomatic COVID-19 Patients: Systematic Review and Meta-Analysis. Am. J. Trop. Med. Hyg. 2020, 103, 815–821. [Google Scholar] [CrossRef] [PubMed]
- De Alencar, J.; Marchini, J.; Marino, L.O.; da Costa Ribeiro, S.C.; Bueno, C.G.; da Cunha, V.P.; Lazar Neto, F.; Brandão Neto, R.A.; Souza, H.P.; COVID U. S. P. Registry Team. Lung ultrasound score predicts outcomes in COVID-19 patients admitted to the emergency department. Ann. Intensive Care 2021, 11, 6. [Google Scholar] [CrossRef] [PubMed]
- Rubio-Gracia, J.; Giménez-López, I.; Garcés-Horna, V.; López-Delgado, D.; Sierra-Monzón, J.L.; Martínez-Lostao, L.; Josa-Laorden, C.; Ruiz-Laiglesia, F.; Pérez-Calvo, J.I.; Crespo-Aznarez, S.; et al. Point-of-care lung ultrasound assessment for risk stratification and therapy guiding in COVID-19 patients. A prospective non-interventional study. Eur. Respir. J. 2021, 2004283. [Google Scholar] [CrossRef] [PubMed]
- Martínez Redondo, J.; Comas Rodríguez, C.; Pujol Salud, J.; Crespo Pons, M.; García Serrano, C.; Ortega Bravo, M.; Palacín Peruga, J.M. Higher accuracy of lung ultrasound over chest X-ray for early diagnosis of COVID-19 pneumonia. Int. J. Environ. Res. Public Health 2021, 18, 3481. [Google Scholar] [CrossRef] [PubMed]
- Calvo-Cebrián, A.; Alonso-Roca, R.; Rodriguez-Contreras, F.J.; Rodríguez-Pascual, M.N.; Calderín-Morales, M.P. Usefulness of Lung Ultrasound Examinations Performed by Primary Care Physicians in Patients with Suspected COVID-19. J. Ultrasound Med. 2020, 40, 741–750. [Google Scholar] [CrossRef] [PubMed]
- Guan, W.; Ni, Z.; Hu, Y.; Liang, W.; Ou, C.; He, J.; Liu, L.; Shan, H.; Lei, C.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Lu, W.; Zhang, S.; Chen, B.; Chen, J.; Xian, J.; Lin, Y.; Shan, H.; Su, Z.Z. A Clinical Study of Noninvasive Assessment of Lung Lesions in Patients with Coronavirus Disease-19 (COVID-19) by Bedside Ultrasound. Ultraschall Med. 2020, 41, 300–307. [Google Scholar] [CrossRef] [PubMed]
- Trauer, M.M.; Matthies, A.; Mani, N.; Mcdermott, C.; Jarman, R. Utility of Lung Ultrasound in COVID-19: A Systematic Scoping Review. Ultrasound 2020, 28, 208–222. [Google Scholar] [CrossRef]
- Zieleskiewicz, L.; Markarian, T.; Lopez, A.; Taguet, C.; Mohammedi, N.; Boucekine, M.; Baumstarck, K.; Besch, G.; Mathon, G.; Duclos, G.; et al. Comparative study of lung ultrasound and chest computed tomography scan in the assessment of severity of confirmed COVID-19 pneumonia. Intensive Care Med. 2020, 46, 1707–1713. [Google Scholar] [CrossRef] [PubMed]
- Volpicelli, G.; Gargani, L.; Perlini, S.; Spinelli, S.; Barbieri, G.; Lanotte, A.; Casasola, G.G.; Nogué-Bou, R.; Lamorte, A.; Agricola, E.; et al. Lung ultrasound for the early diagnosis of COVID-19 pneumonia: An international multicenter study. Intensive Care Med. 2021, 47, 444–454. [Google Scholar] [CrossRef] [PubMed]
- Solanes Cabus, M.; Pujol Salud, J.; Alonso Aliaga, J.; Mayench Ariza, F.; Marsal Mora, J.R.; Sabaté Navarro, A.; Gòdia López, S.; Florensa Piró, C.; Abellana Sangrà, M.; Marín Muñoz, M.; et al. Inter-rater agreement and reliability among General Practitioners and Radiologists on Ultrasound examinations after specialized Training Program. J. Prim. Health Care Gen. Pr. 2019, 3, 026. [Google Scholar]
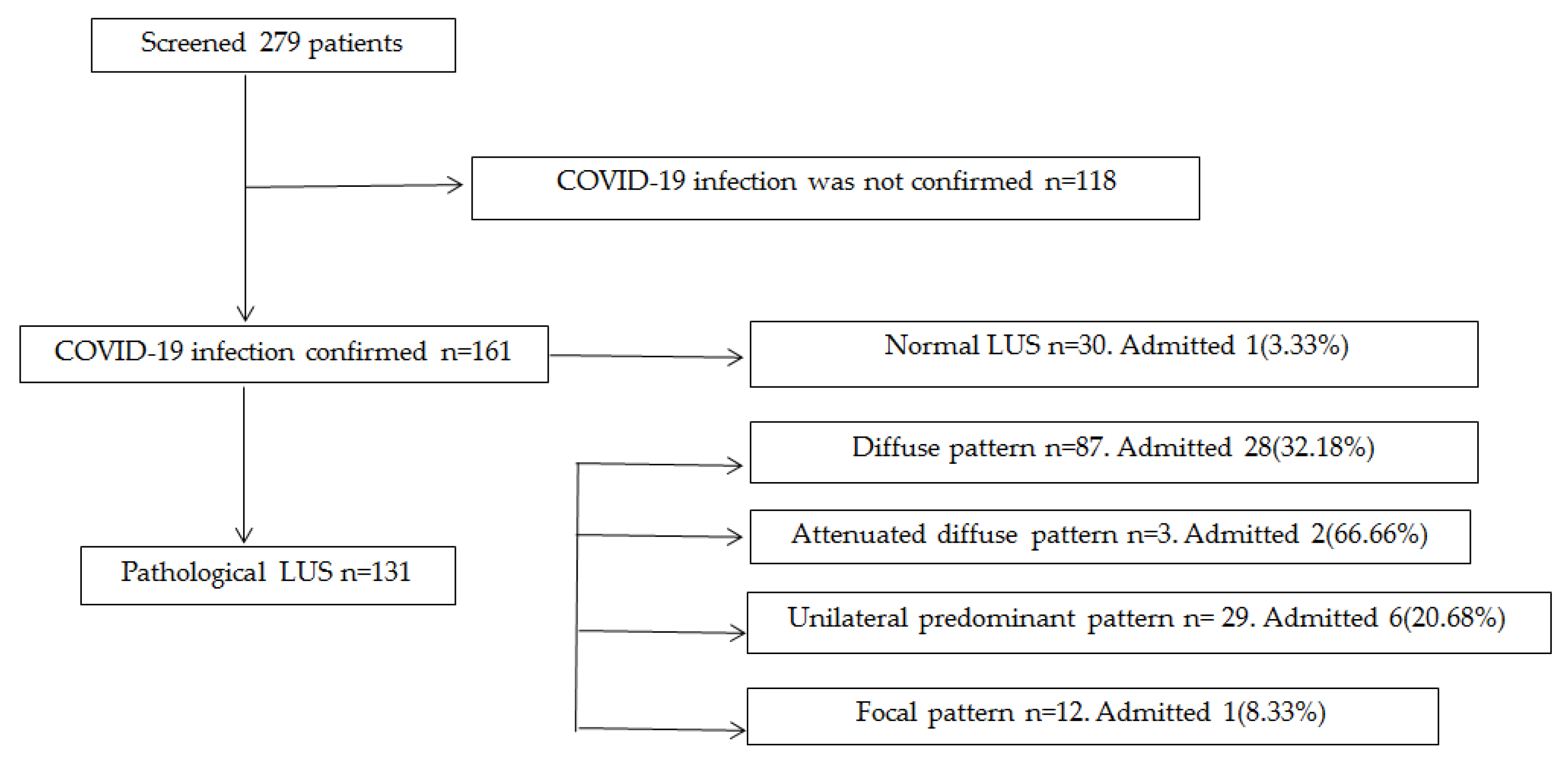
| Interstitial Pattern | Description | n = 172 |
|---|---|---|
| Diffuse | Three or more B-lines in two or more lung fields in a longitudinal section between two ribs (bat sign) and bilaterally. | 87 |
| Attenuated diffuse | More than 8 B-lines distributed in an erratic bilateral inhomogeneous manner. | 3 |
| Unilateral predominant | Three or more B-lines in two or more lung fields in a longitudinal section between two ribs. This pattern was sometimes associated with isolated, erratically arranged B-lines (less than 8) or with a single contralateral field with 3 or more B-lines. | 29 |
| Focal | Three or more B-lines in a single lung field in a longitudinal section between two ribs and unilaterally, sometimes with isolated and associated B-lines (less than 8). | 12 |
| Normal | Absence of B-lines or, in some cases, B-lines (less than 8 and no more than 2 in a single lung field) erratically scattered. | 30 |
| LUS Findings | Diffuse Interstitial Pattern n = 87 | Attenuated Diffuse Interstitial Pattern n = 3 | Unilateral Predominant Interstitial Pattern n = 29 | Focal Interstitial pattern n = 12 |
|---|---|---|---|---|
| Coalescence of B-lines | 15 | 0 | 1 | 2 |
| Diaphragm in rising sun | 6 | 0 | 0 | 0 |
| Irregular and/or thickened pleura | 20 | 0 | 1 | 0 |
| Decreased sliding | 2 | 0 | 0 | 0 |
| Consolidations | 21 | 0 | 0 | 0 |
| Pleural Effusion | 3 | 0 | 0 | 0 |
| Diffuse Interstitial Pattern n = 87 | Attenuated Diffuse Interstitial Pattern n = 3 | Unilateral Predominant Interstitial Pattern n = 29 | Focal Interstitial Pattern n = 12 | |
|---|---|---|---|---|
| Distribution of hospital admission according LUS pattern | 28(32.18%) | 2(66.66%) | 6(20.68%) | 1(8.33%) |
| Association between hospital admission and LUS pattern | p = 0.0016 | p = 0.0002 | p = 0.039 | p = 0.4918 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Redondo, J.; Comas, C.; Pujol Salud, J.; Crespo-Pons, M.; García-Serrano, C.; Bravo, M.O.; Peruga, J.M.P. The Risk of Hospitalization in COVID-19 Patients Can Be Predicted by Lung Ultrasound in Primary Care. Int. J. Environ. Res. Public Health 2021, 18, 6083. https://doi.org/10.3390/ijerph18116083
Martínez-Redondo J, Comas C, Pujol Salud J, Crespo-Pons M, García-Serrano C, Bravo MO, Peruga JMP. The Risk of Hospitalization in COVID-19 Patients Can Be Predicted by Lung Ultrasound in Primary Care. International Journal of Environmental Research and Public Health. 2021; 18(11):6083. https://doi.org/10.3390/ijerph18116083
Chicago/Turabian StyleMartínez-Redondo, Javier, Carles Comas, Jesús Pujol Salud, Montserrat Crespo-Pons, Cristina García-Serrano, Marta Ortega Bravo, and Jose María Palacín Peruga. 2021. "The Risk of Hospitalization in COVID-19 Patients Can Be Predicted by Lung Ultrasound in Primary Care" International Journal of Environmental Research and Public Health 18, no. 11: 6083. https://doi.org/10.3390/ijerph18116083
APA StyleMartínez-Redondo, J., Comas, C., Pujol Salud, J., Crespo-Pons, M., García-Serrano, C., Bravo, M. O., & Peruga, J. M. P. (2021). The Risk of Hospitalization in COVID-19 Patients Can Be Predicted by Lung Ultrasound in Primary Care. International Journal of Environmental Research and Public Health, 18(11), 6083. https://doi.org/10.3390/ijerph18116083






