The Co-Evolution of Network Structure and PrEP Adoption among a Large Cohort of PrEP Peer Leaders: Implications for Intervention Evaluation and Community Capacity-Building
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Site and Population
2.2. Study Design and Data Collection
2.3. Measures
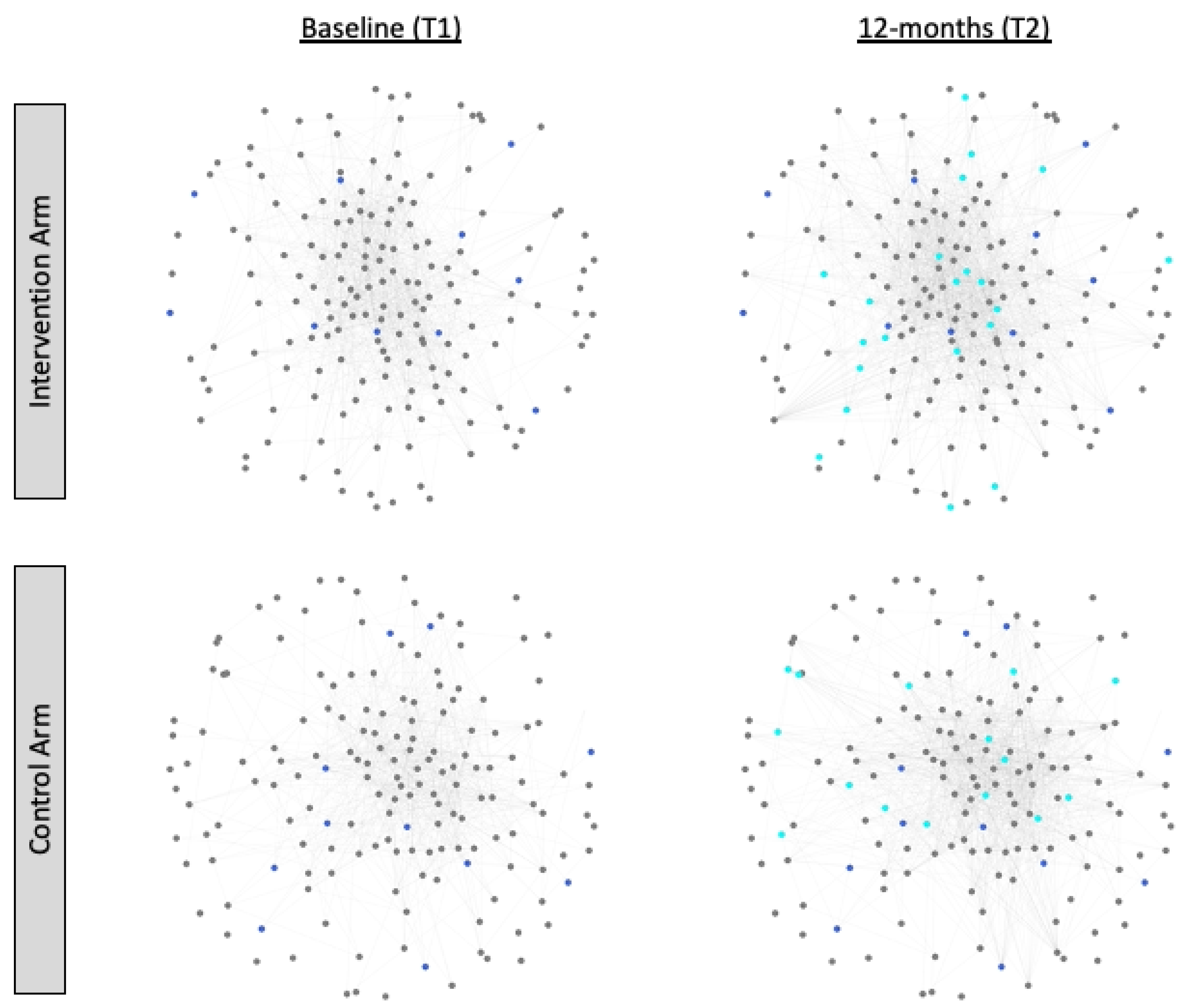
2.3.1. Facebook Friendship Networks
2.3.2. PrEP Adoption
2.3.3. Study Participation Effect
2.3.4. Actor Covariate Attributes
2.3.5. Dyadic Covariate Attributes
2.4. Data Analysis
2.4.1. Analytic Sample
2.4.2. Actor-Based Models for Diffusion of Innovations in Dynamic Networks
2.4.3. Model Specification
2.4.4. Network Dynamics
2.4.5. Adoption Process
3. Results
3.1. Descriptives
3.2. Actor-Based Models for the Diffusion of PrEP in Dynamic Facebook Networks
3.2.1. Model 1: Intervention Arm
3.2.2. Model 2: Control Arm
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
The Logic of Stochastic Actor-Based Models
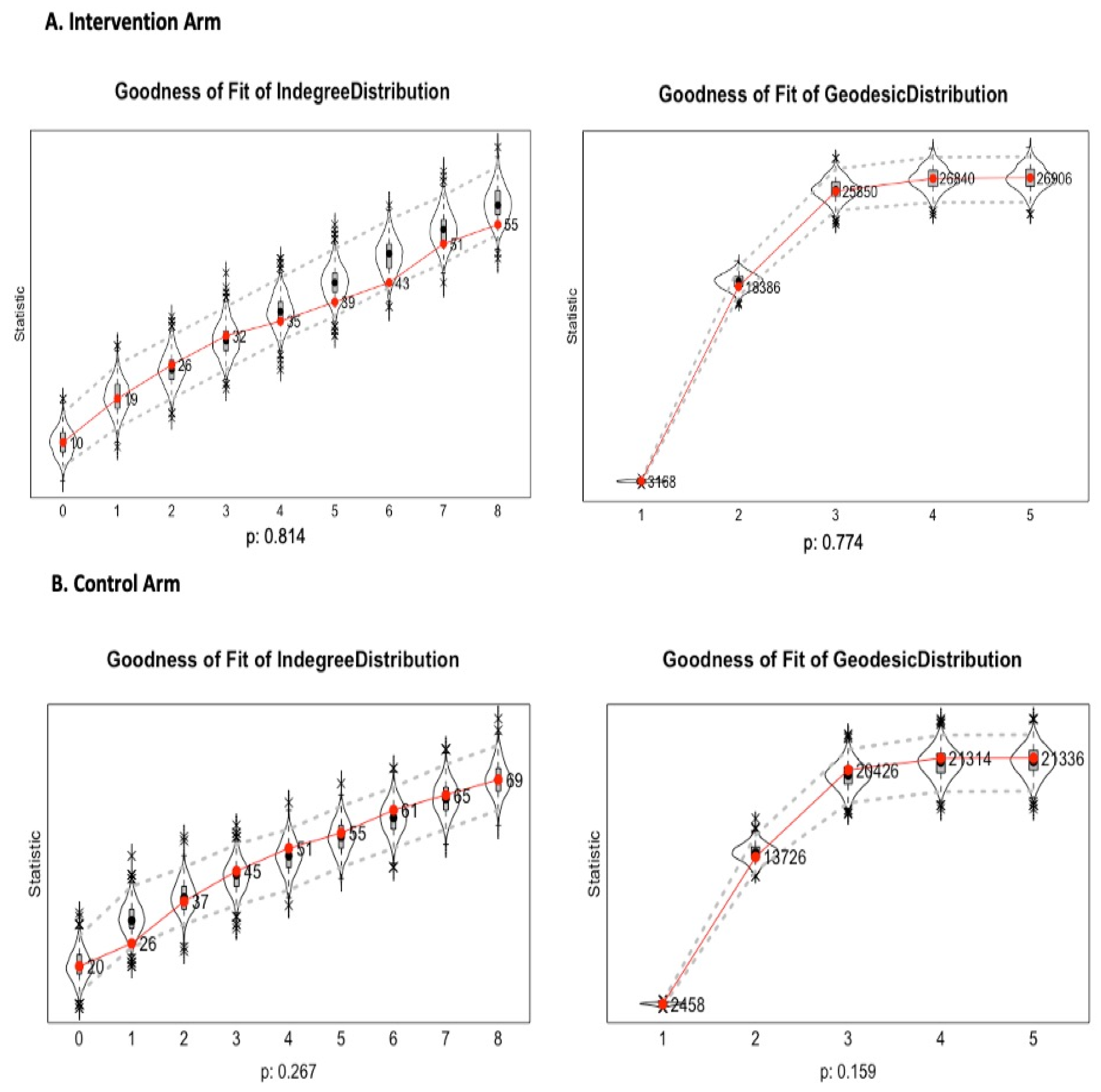
Appendix B
Model Goodness of Fit
References
- Kelley, C.F.; Kahle, E.; Siegler, A.; Sanchez, T.; Del Rio, C.; Sullivan, P.S.; Rosenberg, E.S. Applying a PrEP continuum of care for men who have sex with men in Atlanta, GA. Clin. Infect. Dis. 2015, 6, civ664. [Google Scholar]
- Rusie, L.K.; Orengo, C.; Burrell, D.; Ramachandran, A.; Houlberg, M.; Keglovitz, K.; Munar, D.; Schneider, J.A. Preexposure Prophylaxis Initiation and Retention in Care Over 5 Years, 2012–2017: Are Quarterly Visits Too Much? Clin. Infect. Dis. 2018, 67, 283–287. [Google Scholar] [CrossRef]
- Khanna, A.S.; Michaels, S.; Skaathun, B.; Morgan, E.; Green, K.; Young, L.E.; Schneider, J.A. Preexposure Prophylaxis Awareness and Use in a Population-Based Sample of Young Black Men Who Have Sex with Men. JAMA Intern. Med. 2016, 176, 136–138. [Google Scholar] [CrossRef]
- Hess, K.L.; Hu, X.; Lansky, A.; Mermin, J.; Hall, H.I. Lifetime risk of a diagnosis of HIV infection in the United States. Ann. Epidemiol. 2017, 27, 238–243. [Google Scholar] [CrossRef]
- Cohen, S.E.; Vittinghoff, E.; Bacon, O.; Doblecki-Lewis, S.; Postle, B.S.; Feaster, D.J.; Matheson, T.; Trainor, N.; Blue, R.W.; Estrada, Y. High Interest in Pre-exposure Prophylaxis Among Men Who Have Sex with Men at Risk for HIV-Infection: Baseline Data from the US PrEP Demonstration Project. J. Acquir. Immune Defic. Syndr. 2015, 68, 439–448. [Google Scholar] [CrossRef] [PubMed]
- Stevens, L. Pre-Exposure Prophylaxis: Policy and Implementation. In Proceedings of the United States Conference on AIDS (USCA), San Diego, CA, USA, 3–5 October 2014. [Google Scholar]
- Furukawa, N.W.; Schneider, J.A.; Coleman, M.E.; Wiener, J.B.; Shrestha, R.K.; Smith, D.K. Out-of-pocket costs and HIV pre-exposure prophylaxis persistence in a US multicity demonstration project. Health Serv. Res. 2020, 55, 524–530. [Google Scholar] [CrossRef] [PubMed]
- Eaton, L.A.; Driffin, D.D.; Bauermeister, J.; Smith, H.; Conway-Washington, C. Minimal Awareness and Stalled Uptake of Pre-Exposure Prophylaxis (PrEP) Among at Risk, HIV-Negative, Black Men Who Have Sex with Men. AIDS Patient Care STDS 2015, 29, 423–429. [Google Scholar] [CrossRef]
- Bauermeister, J.A.; Meanley, S.; Pingel, E.; Soler, J.H.; Harper, G.W. PrEP awareness and perceived barriers among single young men who have sex with men. Curr. HIV Res. 2013, 11, 520–527. [Google Scholar] [CrossRef] [PubMed]
- Mutchler, M.G.; McDavitt, B.; Ghani, M.A.; Nogg, K.; Winder, T.J.A.; Soto, J.K. Getting PrEPared for HIV prevention navigation: Young black gay men talk about HIV prevention in the biomedical era. AIDS Patient Care STDs 2015, 29, 490–502. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.K.; Toledo, L.; Smith, D.J.; Adams, M.A.; Rothenberg, R. Attitudes and program preferences of African-American urban young adults about pre-exposure prophylaxis (PrEP). AIDS Educ. Prev. 2012, 24, 408. [Google Scholar] [CrossRef]
- Purdie-Vaughns, V.; Eibach, D.R.P. Intersectional invisibility: The distinctive advantages and disadvantages of multiple subordi-nate-group identities. Sex Roles 2008, 59, 377–391. [Google Scholar] [CrossRef]
- Arnold, E.; Rebchook, G.M.; Kegeles, S.M. ‘Triply cursed’: Racism, homophobia and HIV-related stigma are barriers to regular HIV testing, treatment adherence and disclosure among young Black gay men. Cult. Health Sex. 2014, 16, 710–722. [Google Scholar] [CrossRef]
- Peterson, J.L.; Jones, K.T. HIV prevention for black men who have sex with men in the United States. Am. J. Public Health 2009, 99, 976–980. [Google Scholar] [CrossRef] [PubMed]
- Rogers, E.M. Diffusion of Innovations; Simon and Schuster: New York, NY, USA, 2010. [Google Scholar]
- Valente, T.W. Network interventions. Science 2012, 337, 49–53. [Google Scholar] [CrossRef]
- Ghosh, D.; Krishnan, A.; Gibson, B.; Brown, S.-E.; Latkin, C.A.; Altice, F.L. Social Network Strategies to Address HIV Prevention and Treatment Continuum of Care Among At-risk and HIV-infected Substance Users: A Systematic Scoping Review. AIDS Behav. 2017, 21, 1183–1207. [Google Scholar] [CrossRef] [PubMed]
- Heckathorn, D.D.; Broadhead, R.S.; Anthony, D.L.; Weakliem, D.L. Aids and Social Networks: HIV Prevention Through Network Mobilization. Sociol. Focus 1999, 32, 159–179. [Google Scholar] [CrossRef]
- Kelly, J.A.; St Lawrence, J.S.; Diaz, Y.E.; Stevenson, L.Y.; Hauth, A.C.; Brasfield, T.L.; Kalichman, S.C.; Smith, J.E.; Andrew, M.E. HIV risk behavior reduction following intervention with key opinion leaders of population: An experimental analysis. Am. J. Public Health 1991, 81, 168–171. [Google Scholar] [CrossRef] [PubMed]
- Walsh, T.; Schneider, J.A.; Ardestani, B.M.; Young, L.E. Individual and Social Network Structure Characteristics Associated with Peer Change Agent Engagement and Impact in a PrEP Intervention. AIDS Behav. 2020, 24, 3385–3394. [Google Scholar] [CrossRef]
- Kelly, J.A.; Amirkhanian, Y.A.; Walsh, J.L.; Brown, K.D.; Quinn, K.G.; Petroll, A.E.; Pearson, B.M.; Rosado, A.N.; Ertl, T. Social network intervention to increase pre-exposure prophylaxis (PrEP) awareness, interest, and use among African American men who have sex with men. AIDS Care 2020, 32 (Suppl. 2), 40–46. [Google Scholar] [CrossRef] [PubMed]
- Schneider, J.A.; Young, L.E.; Ramachandran, A.; Michaels, S.; Cohen, H.; Robinson, I.; Alon, L.; Hill, B.; Nakasone, S.; Balenciaga, M.; et al. A Pragmatic Randomized Controlled Trial to Increase Pre-Exposure Prophylaxis Uptake for HIV prevention: 55-week results from PrEPChicago. J Acquir. Immune Defic. Syndr. 2021, 86, 31–37. [Google Scholar] [CrossRef]
- Patel, V.V.; Ginsburg, Z.; Golub, S.A.; Horvath, K.J.; Rios, N.; Mayer, K.H.; Kim, R.S.; Arnsten, J.H. Empowering with PrEP (ePrEP)-a peer-delivered online social network intervention for PrEP adoption among young Black and Latinx men who have sex with men: Cluster randomized controlled trial. In Proceedings of the 2019 International AIDS Society Annual Conference, Mexico City, Mexico, 21–24 July 2019; pp. 64–65. [Google Scholar]
- Kelly, J.A.; St Lawrence, J.S.; Stevenson, L.Y.; Hauth, A.C.; Kalichman, S.; Diaz, Y.E.; Brasfield, T.L.; Koob, J.J.; Morgan, M.G. Community AIDS/HIV risk reduction: The effects of endorsements by popular people in three cities. Am. J. Public Health 1992, 82, 1483–1489. [Google Scholar] [CrossRef]
- Mosack, K.E.; Patterson, L.; Brouwer, A.M.; Wendorf, A.R.; Ertl, K.; Eastwood, D.; Morzinski, J.; Fletcher, K.; Whittle, J. Evaluation of a peer-led hypertension intervention for veterans: Impact on peer leaders. Health Educ. Res. 2013, 28, 426–436. [Google Scholar] [CrossRef]
- Rhee, H.; McQuillan, B.E.; Belyea, M.J. Evaluation of a Peer-Led Asthma Self-Management Program and Benefits of the Pro-gram for Adolescent Peer Leaders. Respir. Care 2012, 57, 2082–2089. [Google Scholar] [CrossRef]
- Sheppard, C.S.; Golonka, M.; Costanzo, P.R. Evaluating the Impact of a Substance Use Intervention Program on the Peer Status and Influence of Adoles-cent Peer Leaders. Prev. Sci. 2012, 13, 75–85. [Google Scholar] [CrossRef]
- Green, G.; Haines, A. The Role of Assets in Community-Based Development. In Asset Building & Community Development; SAGE Publications, Inc.: New York, NY, USA, 2016; pp. 1–31. [Google Scholar]
- Putnam, R.D.; Pharr, S.J.; Dalton, R.J. Introduction: What’s Troubling the Trilateral Democracies? In Disaffected Democracies; Putnam, R.D., Pharr, S.J., Eds.; Princeton University Press: Princeton, NJ, USA, 2000; pp. 3–28. [Google Scholar]
- Beeker, C.; Guenther-Grey, C.; Raj, A. Community empowerment paradigm drift and the primary prevention of HIV/AIDS. Soc. Sci. Med. 1998, 46, 831–842. [Google Scholar] [CrossRef]
- Trickett, E.J.; Beehler, S.; Deutsch, C.; Green, L.W.; Hawe, P.; McLeroy, K.; Miller, R.L.; Rapkin, B.D.; Schensul, J.J.; Schulz, A.J. Advancing the science of community-level interventions. Am. J. Public Health 2011, 101, 1410–1419. [Google Scholar] [CrossRef]
- Singh, A.A. Understanding Trauma and Supporting Resilience with LGBT People of Color. In Trauma, Resilience, and Health Pro-motion in LGBT Patients: What Every Healthcare Provider Should Know; Eckstrand, K.L., Potter, J., Eds.; Springer International Publishing: Cham, Switzerland, 2017; pp. 113–119. [Google Scholar]
- Monica, M.W. Community Connections: Social Capital and Community Success. Sociol. Forum 2012, 27, 441–457. [Google Scholar]
- Musso, J.A.; Weare, C.; Oztas, N.; Loges, W.E. Neighborhood Governance Reform and Networks of Community Power in Los Angeles. Am. Rev. Public Adm. 2006, 36, 79–97. [Google Scholar] [CrossRef]
- Sharp, J.S. Locating the Community Field: A Study of Interorganizational Network Structure and Capacity for Community Action. Rural Sociol. 2001, 66, 403–424. [Google Scholar] [CrossRef]
- Snijders, T.A.B.; van de Bunt, G.G.; Steglich, C.E.G. Introduction to stochastic actor-based models for network dynamics. Soc. Netw. 2010, 32, 44–60. [Google Scholar] [CrossRef]
- Snijders, T.A.B.; Steglich, C.; Schweinberger, M. Modeling the co-evolution of networks and behavior. In Longitudinal Models in the Behavioral and Related Sciences; van Montfort, K., Oud, H., Satorra, A., Eds.; Lawrence Erlbaum: Mahwah, NJ, USA, 2007; pp. 41–71. [Google Scholar]
- Steglich, C.; Snijders, T.A.B.; Pearson, M. Dynamic networks and behavior: Separating selection from influence. Sociol. Methodol. 2010, 40, 329–393. [Google Scholar] [CrossRef]
- Kalton, G.; Anderson, D.W. Sampling rare populations. J. R. Stat. Soc. Ser. A 1986, 149, 65–82. [Google Scholar] [CrossRef]
- Heckathorn, D.D. Respondent-Driven Sampling: A New Approach to the Study of Hidden Populations. Soc. Probl. 1997, 44, 174. [Google Scholar] [CrossRef]
- Heckathorn, D.D. Respondent-Driven Sampling II: Deriving Valid Population Estimates from Chain-Referral Samples of Hidden Populations. Soc. Probl. 2002, 49, 11. [Google Scholar] [CrossRef]
- Johnston, L.G.; Sabin, K. Sampling hard-to-reach populations with respondent driven sampling. Methodol. Innov. Online 2010, 5, 38–48. [Google Scholar] [CrossRef]
- Khanna, A.S.; Schumm, L.P.; Schneider, J. Facebook network structure and awareness of preexposure prophylaxis among young men who have sex with men. Ann. Epidemiol. 2017, 27, 176–180. [Google Scholar] [CrossRef]
- Young, L.E.; Schumm, L.P.; Alon, L.; Bouris, A.; Ferreira, M.; Hill, B.; Khanna, A.S.; Valente, T.W.; Schneider, J.A. PrEP Chicago: A randomized controlled peer change agent intervention to promote the adoption of pre-exposure prophylaxis for HIV prevention among young Black men who have sex with men. Clin. Trials 2018, 15, 44–52. [Google Scholar] [CrossRef]
- Latkin, C.A.; Donnell, D.; Liu, T.Y.; Davey-Rothwell, M.; Celentano, D.; Metzger, D. The dynamic relationship between social norms and behaviors: The results of an HIV prevention network inter-vention for injection drug users. Addiction 2013, 108, 934–943. [Google Scholar] [CrossRef]
- Mihailovic, A.; Tobin, K.; Latkin, C.A. The Influence of a Peer-Based HIV Prevention Intervention on Conversation About HIV Prevention Among People Who Inject Drugs in Baltimore, Maryland. AIDS Behav. 2015, 19, 1792–1800. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lindquist, R.; Wyman, J.F.; Talley, K.; Findorff, M.J.; Gross, C.R. Design of control-group conditions in clinical trials of behavioral interventions. J. Nurs. Scholarsh. 2007, 39, 214–221. [Google Scholar] [CrossRef]
- Young, L.E.; Fujimoto, K. The Co-evolution of online social networks and syphilis incidence among young black men who have sex with men. Soc. Sci. Med. 2021, 272, 113764. [Google Scholar] [CrossRef]
- Brooks, R.A.; Landovitz, R.J.; Regan, R.; Lee, S.-J.; Allen, V.C. Perceptions of and intentions to adopt HIV pre-exposure prophylaxis among black men who have sex with men in Los Angeles. Int. J. STD AIDS 2015, 26, 1040–1048. [Google Scholar] [CrossRef] [PubMed]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Dubov, A.; Altice, F.L.; Fraenkel, L. An Information–Motivation–Behavioral Skills Model of PrEP Uptake. AIDS Behav. 2018, 22, 3603–3616. [Google Scholar] [CrossRef]
- Dehlin, J.M.; Issema, R.; Eavou, R.; Pickett, J.; Alon, L.; Brewer, R.; Schneider, J.A. The Motivational PrEP Cascade Guides Interpretation of Early PrEP Linkage to Care for Young Black Men Who Have Sex with Men: The Case of Chicago’s PrEPLine. AIDS Educ. Prev. 2019, 31, 491–504. [Google Scholar] [CrossRef] [PubMed]
- Greenan, C.C. Diffusion of innovations in dynamic networks. J. R. Stat. Soc. Ser. A 2015, 178, 147–166. [Google Scholar] [CrossRef]
- The R Development Core Team. R: A Language Environment for Statistical Computing; R Foundation for Statistical Computing: Viena, Austria, 2020. [Google Scholar]
- Ripley, R.M.; Snijders, T.A.B.; Boda, Z.; Voros, A.; Preciado, P. Manual for RSiena; Department of Statistics University of Oxford: Oxford, UK; Nuffield College, Department of Sociology University of Groningen: Groningen, The Netherlands, 2020. [Google Scholar]
- O’Quigley, J. Proportional Hazards Regression; Springer: Berlin/Heidelberg, Germany, 2008; Volume 542. [Google Scholar]
- Valente, T.W. Network models and methods for studying the diffusion of innovations. Models Methods Soc. Netw. Anal. 2005, 28, 98. [Google Scholar]
- Strang, D.; Tuma, N.B. Spatial and temporal heterogeneity in diffusion. Am. J. Sociol. 1993, 99, 614–639. [Google Scholar] [CrossRef]
- Reisner, S.L.; Mimiaga, M.J.; Skeer, M.; VanDerwarker, R.; Gaucher, M.J.; O’Connor, C.A.; Medeiros, M.S.; Safren, S.A. What makes a respondent-driven sampling “seed” productive? Example of finding at-risk Massachusetts men who have sex with men. J. Urban Health 2010, 87, 467–479. [Google Scholar] [CrossRef]
- Forrest, J.I.; Lachowsky, N.J.; Lal, A.; Cui, Z.; Sereda, P.; Raymond, H.F.; Ogilvie, G.; Roth, E.A.; Moore, D.; Hogg, R.S. Factors Associated with Productive Recruiting in a Respondent-Driven Sample of Men who Have Sex with Men in Vancouver, Canada. J. Urban Health 2016, 93, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-efficacy: Toward a Unifying Theory of Behavioral Change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef] [PubMed]
- Putnam, R.D. Bowling Alone: The Collapse and Revival of American Community; Simon and Schuster: New York, NY, USA, 2000. [Google Scholar]
- Reed, S.J.; Miller, R.L. Connect to Protect® and the Creation of Aids-Competent Communities. AIDS Educ. Prev. 2013, 25, 255–267. [Google Scholar] [CrossRef][Green Version]
- Reich, S.M.; Subrahmanyam, K.; Espinoza, G. Friending, IMing, and hanging out face-to-face: Overlap in adolescents’ online and offline social networks. Dev. Psychol. 2012, 48, 356. [Google Scholar] [CrossRef] [PubMed]
- Young, L.E.; Ramachandran, A.; Schumm, L.P.; Khanna, A.S.; Schneider, J.A. The potential of online social networking data for augmenting the study of high-risk personal networks among young men who have sex with men at-risk for HIV. Soc. Netw. 2020, 63, 201–212. [Google Scholar] [CrossRef]
- Lospinoso, J.; Snijders, T.A.B. Goodness of fit for stochastic actor-oriented models. Methodol. Innov. 2019, 12, 2059799119884282. [Google Scholar] [CrossRef]
| Effect (Parameter Name) | Description |
|---|---|
| Facebook Network Dynamics | |
| Behavior Effects (PrEP adoption) | |
| Behavior of actor (egoPlusAltX) | Effect of the behavior (PrEP adoption) on friendship formation |
| Same behavior Facebook friend (sameX) | Preference to form friendships based on same behavior (both actors are PrEP adopters) |
| Study Effects | |
| Same training group assignment Facebook friend (sameX) | Preference to form friendships with participants assigned to the same training group |
| Additional Covariate Effects (age, HIV status, PrEP intentions) | |
| Actor covariate (egoPlusAltX) | Effect of the attribute on friendship formation |
| Same or similar covariate Facebook friend (sameX or simX) | Preference to form friendships with peers who share the same categorical or continuous trait |
| Dyadic identity (W) | Effect of having a referral relationship on friendship formation |
| Structural Effects | |
| Degree (density) | Tendency to form friendships |
| Network Closure (gwesp) | Preference to form friendships with the friends of current Facebook friends |
| Preferential Attachment (degPlus) | Preference to form friendships with highly connected network members |
| Degree Assortativity (outInAss) | Preference of high degree actors to form friendships with other high degree network members |
| Isolate (outIso) | Tendency for network isolates to remain isolated |
| PrEP Adoption Process | |
| Contagion Effects | |
| Total exposure (totExposure) | Total number of friends that are PrEP adopters |
| Infection by degree (infectDeg) | The infectiousness of highly connected PrEP adopters (influence determined by degree) |
| Intrinsic Effects (treatment assignment, age, HIV status, PrEP intentions) | |
| Actor covariate (RateX) | Effect of an actor attribute on the rate of PrEP adoption |
| Intervention Arm (n = 174) | Control Arm (n = 166) | |||
|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 1 | Wave 2 | |
| Binary Characteristics | N (%) | N (%) | N (%) | N (%) |
| PrEP Adoption | 10 (5.8) | 25 (14.4) | 11 (6.6) | 20 (12.0) |
| HIV positive | 74 (42.5) | -- | 71 (42.8) | -- |
| PrEP intentions (in next 6 months) | ||||
| Probably/definitely would not take PrEP | 24 (14.7) | -- | 16 (10.4) | -- |
| Might take PrEP | 77 (47.2) | -- | 74 (48.1) | -- |
| Probably/definitely would take PrEP | 62 (38.1) | -- | 64 (41.6) | -- |
| Continuous Characteristics | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) |
| Age | 26.1 (4.3) | -- | 25.3 (4.0) | -- |
| Number of referrals | 0.8 (0.8) | -- | 0.7 (0.8) | -- |
| Number of training group co-members | 4.7 (2.1) | -- | 3.8 (1.8) | -- |
| Intervention Arm | Control Arm | |||
|---|---|---|---|---|
| Characteristic | Baseline | 12-Months | Baseline | 12-Months |
| Mean (SD) of Facebook friendships | 13.1 (10.8) | 17.2 (13.6) | 9.8 (9.2) | 13.8 (12.3) |
| Network density | 0.08 | 0.10 | 0.06 | 0.08 |
| Edge count | 1140 | 1497 | 813 | 1146 |
| Transitivity | 0.27 | 0.30 | 0.25 | 0.31 |
| Centralization | 0.16 | 0.23 | 0.18 | 0.23 |
| Period 1 | Period 1 | |||
| Number of new Facebook friendship ties | 555 | 533 | ||
| Number of stable Facebook friendship ties | 942 | 613 | ||
| Number of dissolved Facebook friendship ties | 198 | 200 | ||
| Jaccard Index a | 0.56 | 0.46 | ||
| Intervention Arm | Control Arm | |||
|---|---|---|---|---|
| Effect | b | (SE) | b | (SE) |
| Facebook Network Dynamics Sub-model | ||||
| Structural effects | ||||
| Basic rate parameter | 6.31 | (0.31) | 7.68 | (0.37) |
| Degree (density) | −3.10 *** | (0.31) | −2.97 *** | (0.33) |
| Network closure (gwesp) | 0.26 * | (0.12) | 0.58 *** | (0.13) |
| Preferential Attachment (degPlus) | 0.005 | (0.01) | −0.003 | (0.01) |
| Degree Assortativity (outInAss) | 0.06 ** | (0.02) | 0.06 ** | (0.02) |
| Isolates (outIso) | 1.96 | (1.26) | 2.69 *** | (0.68) |
| Behavior effects | ||||
| PrEP adoption actor | 0.14 | (0.30) | 0.11 | (0.32) |
| Same PrEP adoption Facebook friend | 0.14 | (0.36) | 0.26 | (0.39) |
| Study effects | ||||
| Same training group assignment Facebook friend | 0.92 *** | (0.17) | 0.34 | (0.22) |
| Other actor covariate effects | ||||
| Age of actor | 0.01 | (0.01) | 0.02 ** | (0.007) |
| Similar age Facebook friend | 1.30 *** | (0.21) | 0.78 *** | (0.22) |
| HIV status actor | 0.19 ** | (0.06) | −0.10 | (0.07) |
| Same HIV status Facebook friend | 0.18 * | (0.08) | −0.005 | (0.08) |
| PrEP intentions actor | 0.13 ** | (0.05) | 0.07 | (0.05) |
| Same PrEP intentions Facebook friend | −0.01 | (0.14) | 0.22 | (0.14) |
| Dyadic covariate effects | ||||
| Study referral tie | 0.67 † | (0.37) | 1.49 *** | (0.43) |
| PrEP Adoption Process Sub-model | ||||
| Contagion effects | ||||
| Rate of period 1 | 0.31 | (0.35) | 0.12 | (0.13) |
| Total exposure | 0.13 | (1.89) | 0.41 | (2.71) |
| Infection by degree | −0.01 | (0.06) | −0.02 | (0.10) |
| Instrinsic effects | ||||
| HIV status actor | −1.34 * | (0.65) | −1.99 * | (0.98) |
| PrEP intentions actor | 0.51 | (0.42) | 1.12 † | (0.67) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Young, L.E.; Schneider, J.A. The Co-Evolution of Network Structure and PrEP Adoption among a Large Cohort of PrEP Peer Leaders: Implications for Intervention Evaluation and Community Capacity-Building. Int. J. Environ. Res. Public Health 2021, 18, 6051. https://doi.org/10.3390/ijerph18116051
Young LE, Schneider JA. The Co-Evolution of Network Structure and PrEP Adoption among a Large Cohort of PrEP Peer Leaders: Implications for Intervention Evaluation and Community Capacity-Building. International Journal of Environmental Research and Public Health. 2021; 18(11):6051. https://doi.org/10.3390/ijerph18116051
Chicago/Turabian StyleYoung, Lindsay E., and John A. Schneider. 2021. "The Co-Evolution of Network Structure and PrEP Adoption among a Large Cohort of PrEP Peer Leaders: Implications for Intervention Evaluation and Community Capacity-Building" International Journal of Environmental Research and Public Health 18, no. 11: 6051. https://doi.org/10.3390/ijerph18116051
APA StyleYoung, L. E., & Schneider, J. A. (2021). The Co-Evolution of Network Structure and PrEP Adoption among a Large Cohort of PrEP Peer Leaders: Implications for Intervention Evaluation and Community Capacity-Building. International Journal of Environmental Research and Public Health, 18(11), 6051. https://doi.org/10.3390/ijerph18116051






