Food Insecurity and Water Insecurity in Rural Zimbabwe: Development of Multidimensional Household Measures
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting and Population
2.2. Data Collection
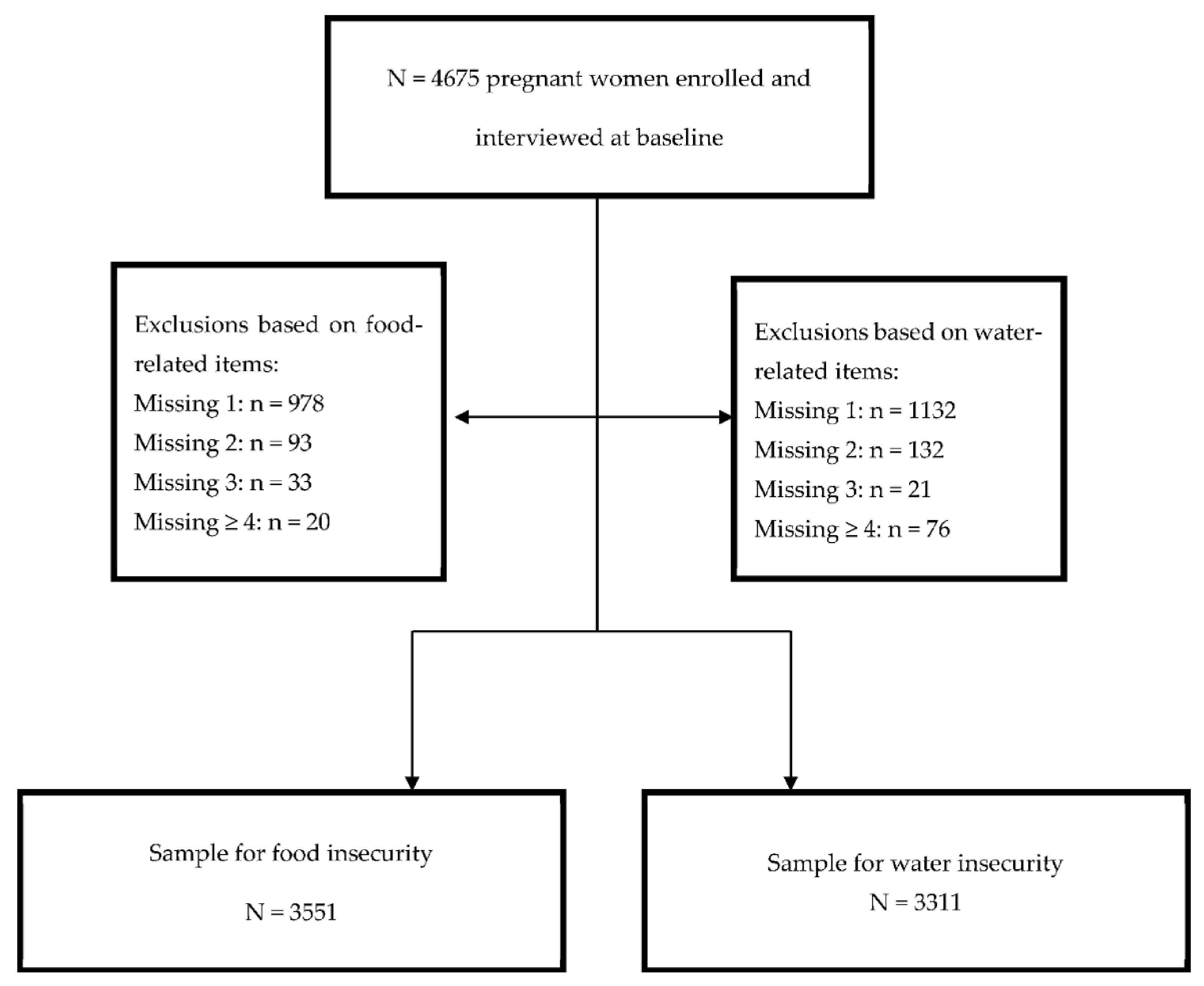
2.3. Sample Selection
2.4. Item Variable Selection
2.5. Statistical Analyses
2.5.1. Descriptives
2.5.2. Item Reduction
2.5.3. Validity Assessments
2.5.4. Sensitivity Analysis
3. Results
3.1. Participant Characteristics
3.2. Multiple Correspondence Analysis (MCA)
3.3. Validity Assessments
4. Discussion
4.1. Food Insecurity (FI)
4.2. Water Insecurity (WI)
4.3. Validity Assessments
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- FAO; IFAD; UNICEF; WFP; WHO. The State of Food Security and Nutrition in the World 2019. Safeguarding against Economic Slowdowns and Downturns; FAO: Rome, Italy, 2019. [Google Scholar]
- WWAP. The United Nations World Water Development Report 2019: Leaving No One Behind; UNESCO World Water Assessment Programme: Paris, France, 2019. [Google Scholar]
- FAO; IFAD; WFP. The State of Food Insecurity in the World 2013. The Multiple Dimensions of Food Security; FAO: Rome, Italy, 2013. [Google Scholar]
- HWISE. Household Water Insecurity Experiences Scale. A Cross-Culturally Validated Scale to Measure Water Insecurity at Household Level. Available online: https://sites.northwestern.edu/hwise/ (accessed on 20 December 2020).
- Young, S.L.; Boateng, G.O.; Jamaluddine, Z.; Miller, J.D.; Frongillo, E.A.; Neilands, T.B.; Collins, S.M.; Wutich, A.; Jepson, W.E.; Stoler, J. The Household Water InSecurity Experiences (HWISE) Scale: Development and validation of a household water insecurity measure for low-income and middle-income countries. BMJ Glob. Health 2019, 4. [Google Scholar] [CrossRef] [PubMed]
- Jepson, W.; Budds, J.; Eichelberger, L.; Harris, L.; Norman, E.; O’Reilly, K.; Pearson, A.; Shah, S.; Shinn, J.; Staddon, C.; et al. Advancing human capabilities for water security: A relational approach. Water Secur. 2017, 1, 46–52. [Google Scholar] [CrossRef]
- WaterAid. Water Security Framework; WaterAid: London, UK, 2012. [Google Scholar]
- Jones, A.D.; Ngure, F.M.; Pelto, G.; Young, S.L. What are we assessing when we measure food security? A compendium and review of current metrics. Adv. Nutr. 2013, 4, 481–505. [Google Scholar] [CrossRef] [PubMed]
- Jepson, W.E.; Wutich, A.; Colllins, S.M.; Boateng, G.O.; Young, S.L. Progress in household water insecurity metrics: A cross-disciplinary approach. Wiley Interdiscip. Rev. Water 2017, 4. [Google Scholar] [CrossRef]
- Maxwell, D.; Vaitla, B.; Coates, J. How do indicators of household food insecurity measure up? An empirical comparison from Ethiopia. Food Policy 2014, 47, 107–116. [Google Scholar] [CrossRef]
- Coates, J.; Swindale, A.; Bilinsky, P. Household Food Insecurity Access Scale (HFIAS) for Measurement of Household Food Access: Indicator Guide (v. 3); Food and Nutrition Technical Assistance Project, Academy for Educational Development: Washington, DC, USA, 2007. [Google Scholar]
- Cafiero, C.; Viviani, S.; Nord, M. Food security measurement in a global context: The food insecurity experience scale. Measurement 2018, 116, 146–152. [Google Scholar] [CrossRef]
- Swindale, A.; Bilinsky, P. Household Dietary Diversity Score (HDDS) for Measurement of Household Food Access: Indicator Guide (v.2); FHI 360/FANTA: Washington, DC, USA, 2006. [Google Scholar]
- Maxwell, D.G.; Caldwell, R. Coping Strategies Index: A Tool for Rapid Measurement of Household Food Security and the Impact of Food Aid Programs in Humanitarian Emergencies. In Field Methods Manual; Cooperative for Assistance and Relief Everywhere, Inc. (CARE): Geneva, Switzerland, 2008. [Google Scholar]
- Coates, J.; Frongillo, E.A.; Rogers, B.L.; Webb, P.; Wilde, P.E.; Houser, R. Commonalities in the Experience of Household Food Insecurity across Cultures: What Are Measures Missing? J. Nutr. 2006, 136, 1438S–1448S. [Google Scholar] [CrossRef]
- Maxwell, D.; Coates, J.; Vaitla, B. How Do Different Indicators of Household Food Security Compare? Empirical Evidence from Tigray; Feinstein International Center, Tufts University: Somerville, MA, USA, 2013. [Google Scholar]
- Broussard, N.H.; Tandon, S. Food Insecurity Measures: Experience-Based versus Nutrition-Based Evidence from India, Bangladesh, and Ethiopia; U.S Department of Agriculture, Economic Research Service: Washington, DC, USA, 2016. Available online: www.ers.usda.gov/publications (accessed on 12 September 2020).
- FAO. Proceedings International Scientific Symposium on Food and Nutrition Security information: From Valid Measurement to Effective Decision Making, Rome, Italy, 17–19 January 2012; FAO: Rome, Italy, 2013. [Google Scholar]
- Howard, G.; Bartram, J. Domestic Water Quantity, Service, Level and Health; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- UNICEF; WHO. Core Questions on Water, Sanitation and Hygiene for Household Surveys: 2018 Update; United Nations Children’s Fund (UNICEF) and World Health Organization (WHO): New York, NY, USA, 2018. [Google Scholar]
- Boateng, G.O.; Collins, S.M.; Mbullo, P.; Wekesa, P.; Onono, M.; Neilands, T.B.; Young, S.L. A novel household water insecurity scale: Procedures and psychometric analysis among postpartum women in western Kenya. PLoS ONE 2018, 13, e0198591. [Google Scholar] [CrossRef]
- Collins, S.M.; Mbullo Owuor, P.; Miller, J.D.; Boateng, G.O.; Wekesa, P.; Onono, M.; Young, S.L. ‘I know how stressful it is to lack water!’ Exploring the lived experiences of household water insecurity among pregnant and postpartum women in western Kenya. Glob. Public Health 2019, 14, 649–662. [Google Scholar] [CrossRef]
- Stevenson, E.G.; Ambelu, A.; Caruso, B.A.; Tesfaye, Y.; Freeman, M.C. Community Water Improvement, Household Water Insecurity, and Women’s Psychological Distress: An Intervention and Control Study in Ethiopia. PLoS ONE 2016, 11, e0153432. [Google Scholar] [CrossRef]
- Stevenson, E.G.; Greene, L.E.; Maes, K.C.; Ambelu, A.; Tesfaye, Y.A.; Rheingans, R.; Hadley, C. Water insecurity in 3 dimensions: An anthropological perspective on water and women’s psychosocial distress in Ethiopia. Soc. Sci. Med. 2012, 75, 392–400. [Google Scholar] [CrossRef]
- Aihara, Y.; Shrestha, S.; Sharma, J. Household water insecurity, depression and quality of life among postnatal women living in urban Nepal. J. Water Health 2016, 14, 317–324. [Google Scholar] [CrossRef]
- Maxfield, A. Testing the theoretical similarities between food and water insecurity: Buffering hypothesis and effects on mental wellbeing. Soc. Sci. Med. 2020, 244, 112412. [Google Scholar] [CrossRef]
- Tsai, A.C.; Kakuhikire, B.; Mushavi, R.; Vorechovska, D.; Perkins, J.M.; McDonough, A.Q.; Bangsberg, D.R. Population-based study of intra-household gender differences in water insecurity: Reliability and validity of a survey instrument for use in rural Uganda. J. Water Health 2016, 14, 280–292. [Google Scholar] [CrossRef]
- Wutich, A.; Ragsdale, K. Water insecurity and emotional distress: Coping with supply, access, and seasonal variability of water in a Bolivian squatter settlement. Soc. Sci. Med. 2008, 67, 2116–2125. [Google Scholar] [CrossRef]
- Tomaz, P.; Jepson, W.; Jader de Oliveira, S. Urban Household Water Insecurity from the Margins: Perspectives from Northeast Brazil. Prof. Geogr. 2020, 72, 481–498. [Google Scholar] [CrossRef]
- Lester, S.; Rhiney, K. Going beyond basic access to improved water sources: Towards deriving a water accessibility index. Habitat Int. 2018, 73, 129–140. [Google Scholar] [CrossRef]
- Jepson, W. Measuring ‘no-win’ waterscapes: Experience-based scales and classification approaches to assess household water security in colonias on the US–Mexico border. Geoforum 2014, 51, 107–120. [Google Scholar] [CrossRef]
- Nagata, J.M.; Gomberg, S.; Hagan, M.J.; Heyman, M.B.; Wojcicki, J.M. Food insecurity is associated with maternal depression and child pervasive developmental symptoms in low-income Latino households. J. Hunger Environ. Nutr. 2019, 14, 526–539. [Google Scholar] [CrossRef]
- Cooper-Vince, C.E.; Arachy, H.; Kakuhikire, B.; Vorechovska, D.; Mushavi, R.C.; Baguma, C.; McDonough, A.Q.; Bangsberg, D.R.; Tsai, A.C. Water insecurity and gendered risk for depression in rural Uganda: A hotspot analysis. BMC Public Health 2018, 18, 1143. [Google Scholar] [CrossRef]
- Abrahams, Z.; Lund, C.; Field, S.; Honikman, S. Factors associated with household food insecurity and depression in pregnant South African women from a low socio-economic setting: A cross-sectional study. Soc. Psychiatry Psychiatr. Epidemiol. 2018, 53, 363–372. [Google Scholar] [CrossRef] [PubMed]
- Brewis, A.; Workman, C.; Wutich, A.; Jepson, W.; Young, S.; Household Water Insecurity Experiences—Research Coordination Network. Household water insecurity is strongly associated with food insecurity: Evidence from 27 sites in low- and middle-income countries. Am. J. Hum. Biol. 2019, 31, e23309. [Google Scholar] [CrossRef] [PubMed]
- Brewis, A.; Choudhary, N.; Wutich, A. Household water insecurity may influence common mental disorders directly and indirectly through multiple pathways: Evidence from Haiti. Soc. Sci. Med. 2019, 238, 112520. [Google Scholar] [CrossRef] [PubMed]
- Behera, B.K.; Rout, P.K.; Behera, S. Water, Energy and Food Security: Pillars for Zero Hunger. In Move Towards Zero Hunger; Behera, B.K., Rout, P.K., Behera, S., Eds.; Springer: Singapore, 2019; pp. 37–60. [Google Scholar] [CrossRef]
- Brewis, A.; Choudhary, N.; Wutich, A. Low water access as a gendered physiological stressor: Blood pressure evidence from Nepal. Am. J. Hum. Biol. 2019, 31, e23234. [Google Scholar] [CrossRef]
- Choudhary, N.; Schuster, R.; Brewis, A.; Wutich, A. Water insecurity potentially undermines dietary diversity of children aged 6-23 months: Evidence from India. Matern. Child Nutr. 2020, 16, e12929. [Google Scholar] [CrossRef]
- Schuster, R.C.; Butler, M.S.; Wutich, A.; Miller, J.D.; Young, S.L.; Household Water Insecurity Experiences-Research Coordination Network. “If there is no water, we cannot feed our children”: The far-reaching consequences of water insecurity on infant feeding practices and infant health across 16 low- and middle-income countries. Am. J. Hum. Biol. 2019, 32, e23357. [Google Scholar] [CrossRef]
- Boateng, G.O.; Workman, C.L.; Miller, J.D.; Onono, M.; Neilands, T.B.; Young, S.L. The syndemic effects of food insecurity, water insecurity, and HIV on depressive symptomatology among Kenyan women. Soc. Sci. Med. 2020, 113043. [Google Scholar] [CrossRef]
- Workman, C.L.; Brewis, A.; Wutich, A.; Young, S.; Stoler, J.; Kearns, J. Understanding Biopsychosocial Health Outcomes of Syndemic Water and Food Insecurity: Applications for Global Health. Am. J. Trop. Med. Hyg. 2020, 104, 8–11. [Google Scholar] [CrossRef]
- Coates, J. Build it back better: Deconstructing food security for improved measurement and action. Glob. Food Secur. 2013, 2, 188–194. [Google Scholar] [CrossRef]
- FAO; IFAD; UNICEF; WFP; WHO. The State of Food Security and Nutrition in the World 2018. Building Climate Resilinece for Food Security and Nutrition; FAO: Rome, Italy, 2018. [Google Scholar]
- WHO; UNICEF. Progress on Drinking Water, Sanitation and Hygiene: 2017 Update and SDG Baselines; World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF): Geneva, Switzerland, 2017. [Google Scholar]
- Mambondiyani, A. Groundwater Crisis in Zimbabwe Brought on by Droughts. Eos, 2 September 2020. Available online: https://eos.org/articles/groundwater-crisis-in-zimbabwe-brought-on-by-droughts (accessed on 12 September 2020).
- FNC. Zimbabwe National Nutrition Survey 2018; Food and Nutrition Council: Harare, Zimbabwe, 2018. [Google Scholar]
- ZimStat. Inter-Censal Demographic Survey 2017; Zimbabwe National Statistics Agency: Harare, Zimbabwe, 2017. [Google Scholar]
- Gandure, S.; Drimie, S.; Faber, M. Food Security Indicators after Humanitarian Interventions Including Food Aid in Zimbabwe. Food Nutr. Bull. 2010, 31, 513–523. [Google Scholar] [CrossRef]
- Humphrey, J.H.; Mbuya, M.N.N.; Ntozini, R.; Moulton, L.H.; Stoltzfus, R.J.; Tavengwa, N.V.; Mutasa, K.; Majo, F.; Mutasa, B.; Mangwadu, G.; et al. Independent and combined effects of improved water, sanitation, and hygiene, and improved complementary feeding, on child stunting and anaemia in rural Zimbabwe: A cluster-randomised trial. Lancet Glob. Health 2019, 7, e132–e147. [Google Scholar] [CrossRef]
- Prendergast, A.J.; Chasekwa, B.; Evans, C.; Mutasa, K.; Mbuya, M.N.N.; Stoltzfus, R.J.; Smith, L.E.; Majo, F.D.; Tavengwa, N.V.; Mutasa, B.; et al. Independent and combined effects of improved water, sanitation, and hygiene, and improved complementary feeding, on stunting and anaemia among HIV-exposed children in rural Zimbabwe: A cluster-randomised controlled trial. Lancet Child. Adolesc. Health 2019, 3, 77–90. [Google Scholar] [CrossRef]
- Humphrey, J.H.; Jones, A.D.; Manges, A.; Mangwadu, G.; Maluccio, J.A.; Mbuya, M.N.; Moulton, L.H.; Ntozini, R.; Prendergast, A.J.; Stoltzfus, R.J.; et al. The Sanitation Hygiene Infant Nutrition Efficacy (SHINE) Trial: Rationale, Design, and Methods. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2015, 61 (Suppl. 7), S685–S702. [Google Scholar] [CrossRef]
- ACF. Food Security and Livelihood Assessments: A Practical Guide for Field Workers; Action Contre la Faim International: New York, NY, USA, 2010. [Google Scholar]
- GWP. Water Security: Putting the Concept into Practice; Global Water Partnership Technical Committee: Stockholm, Sweden, 2014. [Google Scholar]
- Sassi, M. Understanding Food Insecurity: Key Features, Indicators, and Response Design; Springer: Cham, Switzerland, 2017. [Google Scholar]
- WWAP. The United Nations World Water Development Report 2018: Nature-Based Solutions for Water; UNESCO: Paris, France, 2018. [Google Scholar]
- Stoler, J.; Brewis, A.; Harris, L.M.; Wutich, A.; Pearson, A.L.; Rosinger, A.Y.; Schuster, R.C.; Young, S.L. Household water sharing: A missing link in international health. Int. Health 2018, 11, 163–165. [Google Scholar] [CrossRef]
- UN. International Decade for Action “Water for Life” 2005–2015. Available online: http://www.un.org/waterforlifedecade/human_right_to_water.shtml (accessed on 1 January 2020).
- Smets, H. Quantifying the Affordability Standard. In The Human Right to Water: Theory, Practice and Prospects; Russell, A.F.S., Langford, M., Eds.; Cambridge University Press: Cambridge, UK, 2017; pp. 225–275. [Google Scholar] [CrossRef]
- Greenacre, M.J.; Blasius, J. Multiple Correspondence Analysis and Related Methods; Chapman & Hall/CRC: Boca Raton, FL, USA, 2006; 581p. [Google Scholar]
- Lê, S.; Josse, J.; Husson, F. FactoMineR: An R Package for Multivariate Analysis. J. Stat. Softw. 2008, 25, 1–18. [Google Scholar] [CrossRef]
- Chavent, M.; Kuentz-Simonet, V.; Saracco, J. Multivariate analysis of mixed data: The PCAmixdata R package. arXiv 2019, arXiv:1411.4911. [Google Scholar]
- Bannigan, K.; Watson, R. Reliability and validity in a nutshell. J. Clin. Nurs. 2009, 18, 3237–3243. [Google Scholar] [CrossRef]
- Hu, L.t.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Modeling A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Kline, R. Principles and Practice of Structural Equation Modeling, 3rd ed.; The Guilford Press: New York, NY, USA, 2010. [Google Scholar]
- Hays, R.D.; Sherbourne, C.D.; Mazel, R.M. The rand 36-item health survey 1.0. Health Econ. 1993, 2, 217–227. [Google Scholar] [CrossRef]
- Matare, C.R.; Mbuya, M.N.N.; Dickin, K.L.; Constas, M.A.; Pelto, G.; Chasekwa, B.; Humphrey, J.H.; Stoltzfus, R.J.; Sanitation Hygiene Infant Nutrition Efficacy Trial Team Andrew Prendergast. Maternal Capabilities Are Associated with Child Caregiving Behaviors Among Women in Rural Zimbabwe. J. Nutr. 2020, 151, 685–694. [Google Scholar] [CrossRef]
- Chibanda, D.; Mangezi, W.; Tshimanga, M.; Woelk, G.; Rusakaniko, P.; Stranix-Chibanda, L.; Midzi, S.; Maldonado, Y.; Shetty, A.K. Validation of the Edinburgh Postnatal Depression Scale among women in a high HIV prevalence area in urban Zimbabwe. Arch. Women’s Ment. Health 2010, 13, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Chasekwa, B.; Maluccio, J.A.; Ntozini, R.; Moulton, L.H.; Wu, F.; Smith, L.E.; Matare, C.R.; Stoltzfus, R.J.; Mbuya, M.N.N.; Tielsch, J.M.; et al. Measuring wealth in rural communities: Lessons from the Sanitation, Hygiene, Infant Nutrition Efficacy (SHINE) trial. PLoS ONE 2018, 13, e0199393. [Google Scholar] [CrossRef] [PubMed]
- De Goeij, M.C.; van Diepen, M.; Jager, K.J.; Tripepi, G.; Zoccali, C.; Dekker, F.W. Multiple imputation: Dealing with missing data. Nephrol. Dial. Transpl. 2013, 28, 2415–2420. [Google Scholar] [CrossRef]
- Ashby, S.; Kleve, S.; McKechnie, R.; Palermo, C. Measurement of the dimensions of food insecurity in developed countries: A systematic literature review. Public Health Nutr. 2016, 19, 2887–2896. [Google Scholar] [CrossRef] [PubMed]
- Young, S.L.; Miller, J.D.; Frongillo, E.A.; Boateng, G.O.; Jamaluddine, Z.; Neilands, T.B.; The Hwise Research Coordination Network. Validity of a Four-Item Household Water Insecurity Experiences Scale for Assessing Water Issues Related to Health and Well-Being. Am. J. Trop Med. Hyg. 2021, 104, 391–394. [Google Scholar] [CrossRef] [PubMed]
- Hadley, C.; Tegegn, A.; Tessema, F.; Cowan, J.A.; Asefa, M.; Galea, S. Food insecurity, stressful life events and symptoms of anxiety and depression in east Africa: Evidence from the Gilgel Gibe growth and development study. J. Epidemiol. Community Health 2008, 62, 980. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.D. Food Insecurity and Mental Health Status: A Global Analysis of 149 Countries. Am. J. Prev. Med. 2017, 53, 264–273. [Google Scholar] [CrossRef] [PubMed]
- Pheley, A.M.; Holben, D.H.; Graham, A.S.; Simpson, C. Food Security and Perceptions of Health Status: A Preliminary Study in Rural Appalachia. J. Rural Health 2002, 18, 447–453. [Google Scholar] [CrossRef]
- Anema, A.; Fielden, S.J.; Castleman, T.; Grede, N.; Heap, A.; Bloem, M. Food Security in the Context of HIV: Towards Harmonized Definitions and Indicators. AIDS Behav. 2014, 18, 476–489. [Google Scholar] [CrossRef]
- Gebremichael, D.Y.; Hadush, K.T.; Kebede, E.M.; Zegeye, R.T. Food Insecurity, Nutritional Status, and Factors Associated with Malnutrition among People Living with HIV/AIDS Attending Antiretroviral Therapy at Public Health Facilities in West Shewa Zone, Central Ethiopia. Biomed. Res. Int. 2018, 2018, 1913534. [Google Scholar] [CrossRef]
- Knight, L.; Schatz, E.; Lewis, K.R.; Mukumbang, F.C. ‘When you take pills you must eat’: Food (in)security and ART adherence among older people living with HIV. Glob. Public Health 2019, 15, 97–110. [Google Scholar] [CrossRef]
- Bhutta, Z.A.; Das, J.K.; Rizvi, A.; Gaffey, M.F.; Walker, N.; Horton, S.; Webb, P.; Lartey, A.; Black, R.E. Evidence-based interventions for improvement of maternal and child nutrition: What can be done and at what cost? Lancet 2013, 382, 452–477. [Google Scholar] [CrossRef]
- Luby, S.P.; Rahman, M.; Arnold, B.F.; Unicomb, L.; Ashraf, S.; Winch, P.J.; Stewart, C.P.; Begum, F.; Hussain, F.; Benjamin-Chung, J.; et al. Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Bangladesh: A cluster randomised controlled trial. Lancet Glob. Health 2018, 6, e302–e315. [Google Scholar] [CrossRef]
- Null, C.; Stewart, C.P.; Pickering, A.J.; Dentz, H.N.; Arnold, B.F.; Arnold, C.D.; Benjamin-Chung, J.; Clasen, T.; Dewey, K.G.; Fernald, L.C.H.; et al. Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Kenya: A cluster-randomised controlled trial. Lancet Glob. Health 2018, 6, e316–e329. [Google Scholar] [CrossRef]
- Bhutta, Z.A.; Akseer, N.; Keats, E.C.; Vaivada, T.; Baker, S.; Horton, S.E.; Katz, J.; Menon, P.; Piwoz, E.; Shekar, M.; et al. How countries can reduce child stunting at scale: Lessons from exemplar countries. Am. J. Clin. Nutr. 2020, 112, 894S–904S. [Google Scholar] [CrossRef]
- Ruben, R.; Verhagen, J.; Plaisier, C. The Challenge of Food Systems Research: What Difference Does It Make? Sustainability 2018, 11, 171. [Google Scholar] [CrossRef]
- Smiley, S.L.; Stoler, J. Socio-environmental confounders of safe water interventions. WIREs Water 2020, 7, e1438. [Google Scholar] [CrossRef]
- Pickering, A.J.; Null, C.; Winch, P.J.; Mangwadu, G.; Arnold, B.F.; Prendergast, A.J.; Njenga, S.M.; Rahman, M.; Ntozini, R.; Benjamin-Chung, J.; et al. The WASH Benefits and SHINE trials: Interpretation of WASH intervention effects on linear growth and diarrhoea. Lancet Glob. Health 2019, 7, e1139–e1146. [Google Scholar] [CrossRef]
- Cumming, O.; Arnold, B.F.; Ban, R.; Clasen, T.; Esteves Mills, J.; Freeman, M.C.; Gordon, B.; Guiteras, R.; Howard, G.; Hunter, P.R.; et al. The implications of three major new trials for the effect of water, sanitation and hygiene on childhood diarrhea and stunting: A consensus statement. BMC Med. 2019, 17, 173. [Google Scholar] [CrossRef]
- Greenacre, M. Correspondence Analysis in Practice, 2nd ed.; Chapman and Hall/CRC: Boca Raton, FL, USA, 2007. [Google Scholar]
- Wutich, A.; Budds, J.; Jepson, W.; Harris, L.M.; Adams, E.; Brewis, A.; Cronk, L.; DeMyers, C.; Maes, K.; Marley, T.; et al. Household water sharing: A review of water gifts, exchanges, and transfers across cultures. Wiley Interdiscip. Rev. Water 2018, 5, e1309. [Google Scholar] [CrossRef]
- Murrell, A.; Jones, R. Measuring Food Insecurity Using the Food Abundance Index: Implications for Economic, Health and Social Well-Being. Int. J. Environ. Res. Public Health 2020, 17, 2434. [Google Scholar] [CrossRef] [PubMed]
- Yong, A.G.; Pearce, S. A Beginner’s Guide to Factor Analysis: Focusing on Exploratory Factor Analysis. Tutor. Quant. Methods Psychol. 2013, 9, 79–94. [Google Scholar] [CrossRef]
- Worthington, R.L.; Whittaker, T.A. Scale Development Research:A Content Analysis and Recommendations for Best Practices. Couns. Psychol. 2006, 34, 806–838. [Google Scholar] [CrossRef]

| Insecurity | Dimension | Item Variable * | Description of Item Variable | Data Collection | Variable Parameterization ** | Recall Period |
|---|---|---|---|---|---|---|
| Food | Availability | Stock of staple food | Number of days of staple foods available for all household members. | Reported by participating women | 8 ordered categories (days): (1) 0–7, (2) 8–30, (3) 31–60, (4) 61–90, (5) 91–120, (6) 121–180, (7) 181–270, (8) >270 | Present |
| Garden | Household has a garden to grow fruits and/or vegetables | Reported by participating women | Yes vs. No | Present | ||
| Leftover food a | Food left over from last cooking time for the household. | Observed by interviewer | Yes vs. No | Present | ||
| Access | Food not preferred | Household relies on inexpensive and less prefered food. | Reported by participating women | Yes vs. No | Month | |
| Insufficient food | Household members skip entire days without eating, limit portion sizes or reduce number of meals. | Reported by participating women | Yes vs. No | Month | ||
| Food help | Household requires help from family and friends for food, sends members to eat elsewhere or begs for food. | Reported by participating women | Yes vs. No | Month | ||
| Food on credit | Household borrows or purchases food on credit. | Reported by participating women | Yes vs. No | Month | ||
| Assets sold for food | Household sells possessions and assets to afford food. | Reported by participating women | Yes vs. No | Past 3–4 months | ||
| Time to food market | Time taken to go from the homestead to the closest food market (one-way). | Estimated by participating women | 4 ordered categories (minutes): (1) 0–20, (2) 21–40, (3) 41–60, (4) >60 | Usual | ||
| Transportation a | Method of transportation to get to the food market. | Reported by participating women | Categorical: On foot vs. Other (Motor vehicle or bicycle) | Usual | ||
| Utilization | Household diet diversity | Household dietary diversity score calculated from FFQ with reported consumption of 12 food groups. | Reported by participating women | <6 food groups vs. ≥6 food groups | Past 24 h | |
| Handwashing | Responded volunteered answer “Washed hands prior to food handling” when asked reasons for handwashing. | Reported by participating women | Yes vs. No | Usual | ||
| Food storage location | Location of leftover food: on the floor or in an elevated position. | Observed by interviewer | Elevated vs. floor | Present | ||
| Food container a | Leftover foods stored in open or closed containers. | Observed by interviewer | Covered vs. Not covered | Present | ||
| Reliability | Social shocks | Household experienced conflict, legal issues or divorce. | Reported by participating women | Yes vs. No | Past year | |
| Economic shocks | Household experienced job loss, business failure or loss of assets. | Reported by participating women | Yes vs. No | Past year | ||
| Agriculture shocks | Household experienced loss of crops and/or livestock. | Reported by participating women | Yes vs. No | Past year | ||
| Health shocks | Household members experienced death, disease and/or injury. | Reported by participating women | Yes vs. No | Past year | ||
| Water | Availability | Water volume | Total quantity of water immediately available to household. | Calculated from observed data | 4 categories: (1) 0–20 L, (2) >20–40 L, (3) >40–60 L, (4) >60 L | Present |
| Irrigation water a | Household has access to water for irrigation. | Reported by participating women | Yes vs. No | Present | ||
| Access | Time to drinking source | Time taken to get to main source of drinking water from homestead (one-way). | Estimated by participating women | <15 min vs. ≥15 min | Usual | |
| Distance to drinking source | Distance to main drinking water source from homestead (one-way). | Estimated by participating women | <1000 m vs. ≥1000 m | Usual | ||
| Time to non-drinking source | Time taken to get to main source of non-drinking water (one-way). | Estimated by participating women | <15 min vs. ≥15 min | Usual | ||
| Distance to non-drinking source | Distance to main source of water for non-drinking purposes(one-way). | Estimated by participating women | <1000 m vs. ≥1000 m | Usual | ||
| Water purchase a | Does the household purchase water usually? | Reported by participating women | Yes vs. No | Usual | ||
| Utilization | Drinking source type | Water source: (1) piped into dwelling, (2) piped into yard or plot, (3) piped into public tap or standpipe, (4) borehole, (5) protected deep well, (6) unprotected deep well, (7) protected shallow well, (8) unprotected shallow well, (9) improvised shallow well, (10) protected spring, (11) unprotected spring, (12) surface water from river/dam/stream/lake, (13) river bank, (14) rainwater harvester, (15) water truck/Bowser, (16) bottled | Reported by participating women | 3 categories: (1) piped, protected sources, bottled, water truck and rainwater harvester, (2) unprotected ground water and improvised water sources, (3) surface water and river banks. | Usual | |
| Non-drinking source type | Same as drinking source type above | Same as above | Same as above | Usual | ||
| Water satisfaction | Satisfaction with smell, color and taste of water from main water sources. | Reported by participating women | 3 categories: Satisfied/Neutral/Unsatisfied | Usual | ||
| Water treatment | Household treats water to make it safe for consumption e.g., boiling, bleaching, use chlorine, etc. | Reported by participating women | Yes vs. No | Usual | ||
| Water container | Water meant for drinking was kept in covered containers. | Observed by interviewer | Covered vs. Not covered | Present | ||
| Reliability | Drinking water frequency | Frequency at which main source for drinking water runs dry. | Reported by participating women | Ever vs. Never | Anytime over past year | |
| Non-drinking water frequency | Frequency at which main source for non-drinking water runs dry. | Reported by participating women | Ever vs. Never | Anytime over past year |
| Type of Validity | Purpose | Assessment Methods |
|---|---|---|
| Internal | To determine the extent to which the dimensions obtained are consistent within the sample and across time. | 1. CFA with a sub-sample of the population at baseline to cross-validate the number of dimensions and loading patterns. |
| 2. CFA with the same households reporting information at 18 months to cross-validate the results across time. | ||
| Predictive | To determine the extent to which the dimension scores predict known related outcomes. | Linear regression to estimate the associations between dimensions of: |
| 2. Water insecurity and perceived health status and depression symptomatology. | ||
| 1. Food insecurity and perceived health status and depression symptomatology. | ||
| Discriminant | To determine the extent to which the dimension scores are differentiated as expected according to known groups. | Tests of differentiation between dimension scores across known groups using linear regression: |
| 1. Food insecurity: season (hungry vs plenty), SES-status, HIV-status. | ||
| 2. Water insecurity: season (rainy vs dry), wealth index, HIV-status. | ||
| Convergent | To determine the extent to which the dimension scores are associated with other constructs that are closely related. | Linear regression to estimate association between dimensions of: |
| 1. Food insecurity and receiving food aid. | ||
| 2. Water insecurity and frequency of water collection. |
| Characteristics | Food Sample | Water Sample |
|---|---|---|
| Socio-demographic *, N | 3551 | 3311 |
| Trial arm, n (%) | ||
| SOC | 803 (22.61) | 772 (22.61) |
| IYCF | 872 (24.56) | 780 (24.56) |
| WASH | 914 (25.74) | 856 (25.74) |
| WASH + IYCF | 962 (27.09) | 903 (27.09) |
| Living with HIV, n/N (%) | 556/3537 (15.66) | 524/3297 (15.66) |
| Rainy season at interview, n/N (%) | - | 1473/3310 (45.17) |
| Hungry season at interview, n/N(%) | 1030/3545 (29.01) | 942 (29.01) |
| Woman’s education, n (%) | ||
| Primary | 640 (18.02) | 596 (18.02) |
| Some secondary | 1263 (35.57) | 1199 (35.57) |
| Completed secondary | 1510 (42.52) | 1382 (42.52) |
| Women employed, n/N(%) | 298/3241 (8.39) | 284/3302 (8.39) |
| SES tercile, n (%) | ||
| lower | 1141 (32.13) | 1079 (32.13) |
| middle | 1192 (33.57) | 1117 (33.57) |
| upper | 1214 (34.19) | 1111 (34.19) |
| Women partnered, n/N(%) | 3233/3384 (91.04) | 3015/3156 (91.04) |
| Parous 1, n/N(%) | 1885/2254 (53.08) | 1964/2330 (59.32) |
| Religion: Apostolic, n/N(%) | 1596/3411 (44.95) | 1513/3176 (44.95) |
| Depression, n/N(%) | 201/3485 (5.66) | 155/3170 (5.66) |
| Woman’s age, n/mean (SD) | 3401/26.42 (6.72) | 3171/26.32 (6.68) |
| Household size, n/median (IQR) | 3432/5 (3) | 3199/5 (3) |
| Perceived health status 1, n/mean (SD) | 3065/3.42 (0.99) | 2874/3.42 (0.99) |
| Food item variables **, N | 3551 | |
| Staple food stocks | ||
| >270 days | 402 (11.32) | - |
| 181–270 days | 370 (10.42) | - |
| 121–180 days | 584 (16.45) | - |
| 91–120 days | 296 (8.34) | - |
| 61–90 days | 447 (12.59) | - |
| 31–60 days | 459 (12.93) | - |
| 8–30 days | 562 (15.83) | - |
| 0–7 days | 431 (12.14) | - |
| Garden, N (%) | 2904 (81.78) | - |
| Leftover food, N (%) | 1705 (48.01) | - |
| Food not preferred | 2478 (69.78) | - |
| Insufficient food | 866 (24.39) | - |
| Food help | 477 (13.43) | - |
| Food on credit | 898 (25.29) | - |
| Assets sold for food | 404 (11.38) | - |
| Time to food market, n (%) | ||
| 0–20 min | 985 (27.74) | - |
| 21–40 min | 842 (23.71) | - |
| 41–60 min | 1005 (28.3) | - |
| >1 h | 719 (20.25) | - |
| Transportation, n (%) | ||
| Bicycle/Motor | 150 (4.22) | - |
| Walking | 3384 (95.3) | - |
| Household meets diet diversity | 2581 (72.68) | - |
| Handwashing prior to food handling | 3198 (90.06) | - |
| Food storage location | ||
| Elevated position | 2091 (58.88) | - |
| On floor | 1460 (41.12) | - |
| Food container covered | 3513 (98.93) | - |
| Social shocks | 261 (7.35) | - |
| Economic shocks | 472 (13.29) | - |
| Agriculture shocks | 893 (25.15) | - |
| Health shocks | 1670 (47.03) | - |
| Water item variables **, N | 3311 | |
| Volume | ||
| >60 L | - | 370 (11.17) |
| 41 to 60 L | - | 458 (13.83) |
| 21 to 40 L | - | 1093 (33.01) |
| 0–20 L | - | 1390 (41.98) |
| Water for irrigation | - | 699 (21.11) |
| One-way ≤ 15 min to drinking water source | - | 2411 (72.82) |
| Distance ≤ 1000 m to drinking source | - | 2902 (87.65) |
| One-way ≤ 15 min to non-drinking source | - | 2470 (74.6) |
| Distance ≤ 1000 m to non-drinking source | - | 2918 (88.13) |
| Purchase of water | - | 5 (0.15) |
| Type of drinking source | ||
| Improved (piped, protected) | - | 2097 (63.33) |
| Unprotected ground | - | 954 (28.81) |
| Surface water | - | 260 (7.85) |
| Type of non-drinking source | ||
| Improved (piped, protected) | - | 1105 (33.37) |
| Unprotected ground | - | 970 (29.3) |
| Surface water | - | 1236 (37.33) |
| Satisfaction with main water source | ||
| Satisfied | - | 2677 (80.85) |
| Neither satisfied not unsatisfied | - | 343 (10.36) |
| Unsatisfied | - | 291 (8.79) |
| Drinking water treated | - | 412 (12.44) |
| Drinking water containers covered | - | 2143 (64.72) |
| Drinking water always available | - | 2892 (87.35) |
| Water for non-drinking purposes always available | - | 2951 (89.13) |
| Food Insecurity (N = 3551) | Water Insecurity (N = 3311) | ||||||
|---|---|---|---|---|---|---|---|
| MCA Food Dimensions | 1 | 2 | 3 | MCA Water Dimensions | 1 | 2 | 3 |
| Dimension Names | Poor Food Access | Household Shocks | Low Food Availability and Quality | Dimension Names | Poor Water Access | Poor Water Quality | Low Water Reliability |
| Stock of staple food | 0.11 | 0.05 | 0.31 | Water volume | 0.01 | 0 | 0.01 |
| Garden | 0 | 0 | 0.32 | Time to drinking source | 0.56 | 0 | 0 |
| Food not preferred | 0.48 | 0.01 | 0.0 | Distance to drinking source | 0.48 | 0 | 0 |
| Insufficient food | 0.52 | 0 | 0.01 | Time to non-drinking source | 0.58 | 0 | 0 |
| Food help | 0.47 | 0 | 0 | Distance to non-drinking source | 0.49 | 0 | 0 |
| Food on credit | 0.47 | 0.01 | 0 | Drinking source | 0.09 | 0.76 | 0.06 |
| Assets sold for food | 0.02 | 0.04 | 0.05 | Non-drinking source | 0.10 | 0.66 | 0.01 |
| Time to food market | 0.03 | 0.05 | 0.11 | Water satisfaction | 0.04 | 0.30 | 0 |
| Handwashing | 0 | 0.01 | 0.02 | Water treatment | 0 | 0.04 | 0 |
| Food storage location | 0.01 | 0 | 0.11 | Water container | 0 | 0 | 0.01 |
| Household diet diversity | 0.03 | 0.06 | 0.25 | Frequency of availability of drinking water at the source | 0 | 0 | 0.70 |
| Social shocks | 0.01 | 0.07 | 0.03 | ||||
| Economic shocks | 0.02 | 0.32 | 0.01 | Frequency of availability of non-drinking water at the source | 0 | 0 | 0.70 |
| Agriculture shocks | 0.01 | 0.36 | 0 | ||||
| Health shocks | 0 | 0.34 | 0 | ||||
| Eigenvalue | 2.17 | 1.32 | 1.22 | Eigenvalue | 2.36 | 1.78 | 1.50 |
| % variance | 9.06 | 5.93 | 5.13 | % variance | 13.29 | 9.93 | 8.14 |
| Median score (IQR)* | −0.32 (1.35) | −0.14 (1.36) | −0.07 (1.34) | Median (IQR) | −0.48 (1.40) | −0.28 (2.01) | −0.32 (0.26) |
| Min, max score * | −1.33, 3.39 | −2.25, 3.41 | −2.81, 3.93 | Min, max | −1.04, 3.63 | −1.41, 2.43 | −1.46, 3.46 |
| Measure | Food Insecurity | Water Insecurity | ||
|---|---|---|---|---|
| Groups | Baseline Test Sample 1 | 18 months 2 | Baseline Test Sample 1 | 18 months |
| N | 2132 | 3612 | 1998 | 3879 |
| RMSEA ≤ 0.05 (range: 0, 0.10) | 0.04 (0.03, 0.04) | 0.04 (0.03, 0.04) | 0.04 (0.04, 0.05) | 0.06 (0.06, 0.07) |
| CFI ≥ 0.95 | 0.88 | 0.90 | 0.96 | 0.97 |
| TLI ≥ 0.90 | 0.87 | 0.88 | 0.95 | 0.97 |
| SRMR ≤ 0.08 | 0.07 | 0.08 | 0.07 | 0.09 |
| Food Insecurity (N = 3551) β [95% CI] | Water Insecurity (N = 3311) β [95% CI] | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Validity | Variable | Expected direction | n/N Median (IQR) | Poor food access | Household shocks | Low food quality and availability | n/N Median (IQR) | Poor water access | Poor water quality | Low water reliability |
| −0.38 (1.34) | −0.18 (1.35) | −0.08 (1.40) | −0.47 (1.40) | −0.27 (1.99) | −0.33 (0.28) | |||||
| Predictive | a Perceived health status | Negative | 3065 | −0.16 | −0.13 | −0.05 | 2874 | −0.04 | −0.04 | −0.07 |
| [−0.19, −0.12] | [−0.17, −0.09] | [−0.08, −0.01] | [−0.08, −0.01] | [−0.08, −0.01] | [−0.11, −0.03] | |||||
| a Depression | Positive | 3485 | 0.52 | 0.37 | 0.26 | 3236 | 0.22 | 0.22 | 0.23 | |
| [0.38, 0.66] | [0.23, 0.51] | [0.12, 0.41] | [0.07, 0.36] | [0.07, 0.36] | [0.08, 0.37] | |||||
| Discriminant | b Season: Hungry vs. Plenty | Positive | 1030/3545 | 0.12 | 0.04 | 0.25 | - | - | - | - |
| [0.05, 0.20] | [−0.03, 0.12] | [0.18, 0.32] | ||||||||
| b Season: Dry vs. Rainy | Positive | - | - | - | - | 1837/3310 | 0.16 | 0.03 | −0.11 | |
| [0.09, 0.22] | [−0.04, 0.10] | [−0.18, −0.04] | ||||||||
| c Middle SES vs. High SES | Positive | 1192/3547 | 0.29 | −0.14 | 0.27 | 1111/3307 | 0.05 | 0.18 | 0.05 | |
| [0.21, 0.37] | [−0.22, −0.06] | [0.19, 0.35] | [−0.03, 0.13] | [0.09, 0.26] | [−0.03, 0.14] | |||||
| c Low SES vs. High SES | Positive | 1141/3548 | 0.56 | −0.27 | 0.61 | 1117/3308 | 0.15 | 0.32 | 0.01 | |
| [0.48, 0.64] | [−0.35, −0.19] | [0.53, 0.69] | [0.07, 0.24] | [0.24, 0.40] | [−0.07, 0.10] | |||||
| d HIV-positive vs. HIV negative | Positive | 556/3547 | 0.21 | −0.01 | 0.16 | 524/3297 | 0.06 | 0.05 | −0.02 | |
| [0.12, 0.30] | [−0.05, 0.02] | [0.07, 0.24] | [−0.03, 0.15] | [−0.04, 0.15] | [−0.11, 0.07] | |||||
| Convergent | c Receive food aid vs. no food aid | Positive | 316/3551 | 0.12 | 0.19 | 0.06 | - | - | - | - |
| [0.00, 0.23] | [0.07, 0.30] | [−0.05, 0.18] | ||||||||
| a Water collection- Weekly vs. Daily | Positive | - | - | - | - | 488/3306 | 0.17 | 0 | 0.05 | |
| [0.07, 0.27] | [−0.09, 0.10] | [−0.05, 0.15] | ||||||||
| a Water collection- Monthly vs. Daily | Positive | - | - | - | - | 140/3307 | 0.24 | −0.09 | −0.08 | |
| [0.07, 0.41] | [−0.26, 0.08] | [−0.25, 0.09] | ||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koyratty, N.; Jones, A.D.; Schuster, R.; Kordas, K.; Li, C.-S.; Mbuya, M.N.N.; Boateng, G.O.; Ntozini, R.; Chasekwa, B.; Humphrey, J.H.; et al. Food Insecurity and Water Insecurity in Rural Zimbabwe: Development of Multidimensional Household Measures. Int. J. Environ. Res. Public Health 2021, 18, 6020. https://doi.org/10.3390/ijerph18116020
Koyratty N, Jones AD, Schuster R, Kordas K, Li C-S, Mbuya MNN, Boateng GO, Ntozini R, Chasekwa B, Humphrey JH, et al. Food Insecurity and Water Insecurity in Rural Zimbabwe: Development of Multidimensional Household Measures. International Journal of Environmental Research and Public Health. 2021; 18(11):6020. https://doi.org/10.3390/ijerph18116020
Chicago/Turabian StyleKoyratty, Nadia, Andrew D. Jones, Roseanne Schuster, Katarzyna Kordas, Chin-Shang Li, Mduduzi N. N. Mbuya, Godfred O. Boateng, Robert Ntozini, Bernard Chasekwa, Jean H. Humphrey, and et al. 2021. "Food Insecurity and Water Insecurity in Rural Zimbabwe: Development of Multidimensional Household Measures" International Journal of Environmental Research and Public Health 18, no. 11: 6020. https://doi.org/10.3390/ijerph18116020
APA StyleKoyratty, N., Jones, A. D., Schuster, R., Kordas, K., Li, C.-S., Mbuya, M. N. N., Boateng, G. O., Ntozini, R., Chasekwa, B., Humphrey, J. H., Smith, L. E., & on behalf of the SHINE Trial Team. (2021). Food Insecurity and Water Insecurity in Rural Zimbabwe: Development of Multidimensional Household Measures. International Journal of Environmental Research and Public Health, 18(11), 6020. https://doi.org/10.3390/ijerph18116020









