Resilience in the Storm: Impacts of Changed Daily Lifestyles on Mental Health in Persons with Chronic Illnesses under the COVID-19 Pandemic
Abstract
1. Introduction
1.1. Pandemic Adjustment for Persons with a Chronic Illness
1.2. Daily Lifestyle Disruption, Psychological Resilience and Mental Health
1.3. The Current Study
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Measurements
2.4. Statistical Analysis
3. Results
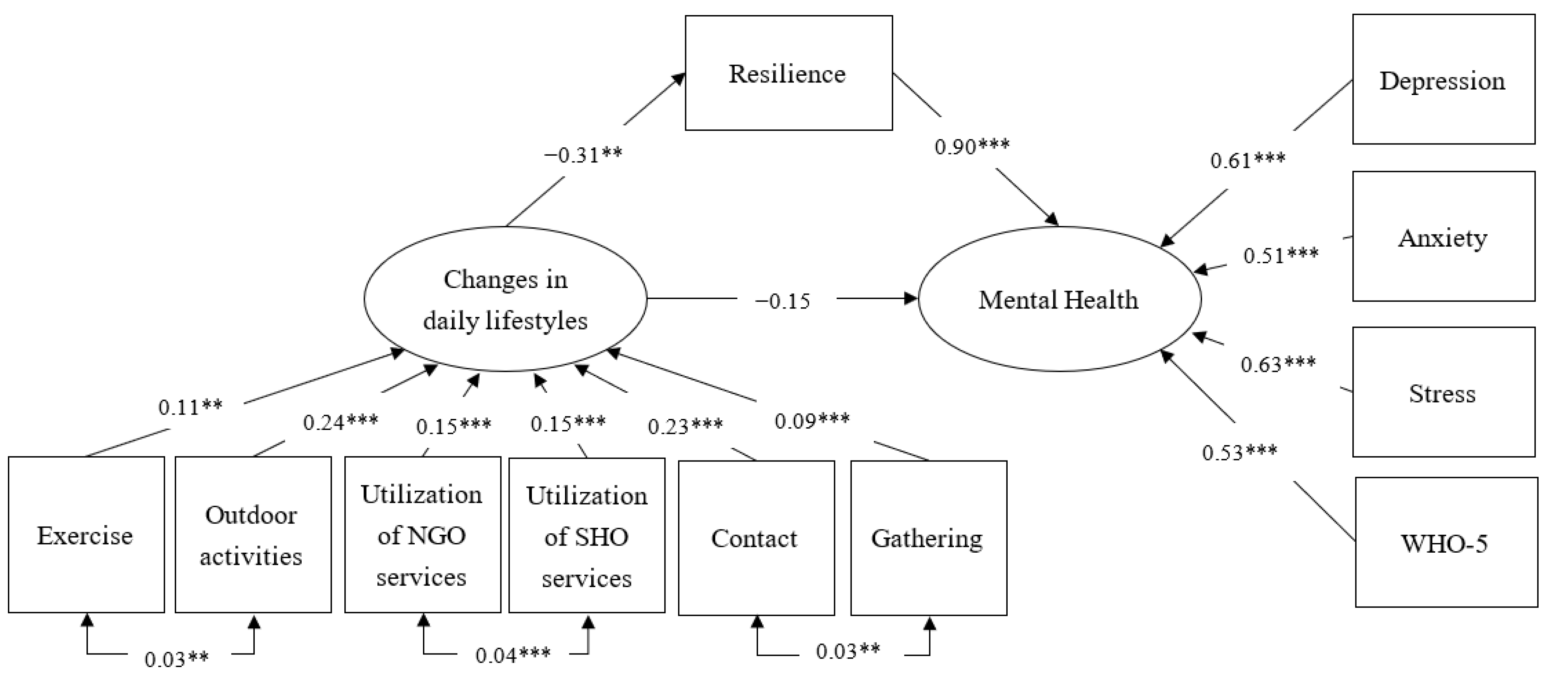
3.1. Relationships between Changes in Daily Lifestyles and Psychological Resilience and Mental Health
3.2. Mediation Effect of Psychological Resilience
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Horesh, D.; Brown, A.D. Traumatic stress in the age of COVID-19: A call to close critical gaps and adapt to new realities. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, 331. [Google Scholar] [CrossRef]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Li, D.C.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef]
- McKinsey & Company. Understanding the Hidden Costs of COVID-19’s Potential Impact on US Healthcare. 2020. Available online: https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/understanding-the-hidden-costs-of-covid-19s-potential-impact-on-us-healthcare (accessed on 25 May 2021).
- Department Census and Statistics, HKSAR Government. Thematic Household Survey Reports No. 68. November 2019. Available online: https://www.censtatd.gov.hk/en/data/stat_report/product/C0000022/att/B11302682019XXXXB0100.pdf (accessed on 25 May 2021).
- Stein, D.J.; Benjet, C.; Gureje, O.; Lund, C.; Scott, K.M.; Poznyak, V.; van Ommeren, M. Integrating mental health with other non-communicable diseases. BMJ 2019, 364, 295. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Salgado, J.; Andrés-Villas, M.; Domínguez-Salas, S.; Díaz-Milanés, D.; Ruiz-Frutos, C. Related health factors of psychological distress during the COVID-19 pandemic in Spain. Int. J. Environ. Res. Public Health 2020, 17, 3947. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.K.; et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020, 87, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Mazza, C.; Ricci, E.; Biondi, S.; Colasanti, M.; Ferracuti, S.; Napoli, C.; Roma, P. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: Immediate psychological responses and associated factors. Int. J. Environ. Res. Public Health 2020, 17, 3165. [Google Scholar] [CrossRef]
- Bitan, D.T.; Grossman-Giron, A.; Bloch, Y.; Mayer, Y.; Shiffman, N.; Mendlovic, S. Fear of COVID-19 scale: Psychometric characteristics, reliability and validity in the Israeli population. Psychiatry Res. 2020, 289, 113100. [Google Scholar] [CrossRef]
- Horesh, D.; Kapel Lev-Ari, R.; Hasson-Ohayon, I. Risk factors for psychological distress during the COVID-19 pandemic in Israel: Loneliness, age, gender, and health status play an important role. Br. J. Health Psychol. 2020, 25, 925–933. [Google Scholar] [CrossRef]
- Palmer, K.; Monaco, A.; Kivipelto, M.; Onder, J.; Maggi, S.; Michel, J.-P.; Prieto, R.; Sykara, G.; Donde, S. The potential long-term impact of the COVID-19 outbreak on patients with non-communicable diseases in Europe: Consequences for healthy ageing. Aging Clin. Exp. Res. 2020, 32, 1189–1194. [Google Scholar] [CrossRef]
- Smith, M.L.; Steinman, L.E.; Casey, E. Combatting social isolation among older adults in a time of physical distancing: The COVID-19 social connectivity paradox. Front. Public Health 2020, 8, 403. [Google Scholar] [CrossRef] [PubMed]
- Giuntella, O.; Hyde, K.; Saccardo, S.; Sadoff, S. Lifestyle and mental health disruptions during Covid-19. Proc. Natl. Acad. Sci. USA 2021, 118. [Google Scholar] [CrossRef]
- Di Santo, S.G.; Franchini, F.; Filiputti, B.; Martone, A.; Sannino, S. The effects of COVID-19 and quarantine measures on the lifestyles and mental health of people over 60 at increased risk of dementia. Front. Psychiatry 2020, 11, 578628. [Google Scholar] [CrossRef] [PubMed]
- Connor, K.M.; Davidson, J.R. Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC). Depress. Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef]
- Aburn, G.; Gott, M.; Hoare, K. What is resilience? An integrative review of the empirical literature. J. Adv. Nurs. 2016, 72, 980–1000. [Google Scholar] [CrossRef]
- Hu, T.; Zhang, D.; Wang, J. A meta-analysis of the trait resilience and mental health. Personal. Individ. Differ. 2015, 76, 18–27. [Google Scholar] [CrossRef]
- Kobasa, S.C. Stressful life events, personality, and health: An inquiry into hardiness. J. Personal. Soc. Psychol. 1979, 37, 1. [Google Scholar] [CrossRef]
- Rutter, M. Resilience in the face of adversity: Protective factors and resistance to psychiatric disorder. Br. J. Psychiatry 1985, 147, 598–611. [Google Scholar] [CrossRef] [PubMed]
- Doll, B.; Lyon, M.A. Risk and resilience: Implications for the delivery of educational and mental health services in schools. Sch. Psychol. Rev. 1998, 27, 348–363. [Google Scholar] [CrossRef]
- Kimhi, S.; Marciano, H.; Eshel, Y.; Adini, B. Resilience and demographic characteristics predicting distress during the COVID-19 crisis. Soc. Sci. Med. 2020, 265, 113389. [Google Scholar] [CrossRef]
- Song, S.; Yang, X.; Yang, H.; Zhou, P.; Ma, H.; Teng, C.; Chen, H.; Ou, H.; Li, J.; Mathews, C.A.; et al. Psychological resilience as a protective factor for depression and anxiety among the public during the outbreak of COVID-19. Runing Title: Protective factor of the public during COVID-19. Front. Psychol. 2020, 11, 4104. [Google Scholar]
- Ran, L.; Wang, W.; Ai, M.; Kong, Y.; Chen, J.; Kuang, L. Psychological resilience, depression, anxiety, and somatization symptoms in response to COVID-19: A study of the general population in China at the peak of its epidemic. Soc. Sci. Med. 2020, 262, 113261. [Google Scholar] [CrossRef] [PubMed]
- Ye, Z.; Yang, X.; Zeng, C.; Wang, Y.; Shen, Z.; Li, X.; Lin, D. Resilience, social support, and coping as mediators between COVID-19-related stressful experiences and acute stress disorder among college students in China. Appl. Psychol. Health Well-Being 2020, 12, 1074–1094. [Google Scholar] [CrossRef]
- Hou, W.K.; Hall, B.J.; Hobfoll, S.E. Drive to thrive: A theory of resilience following loss. In Mental Health of Refugee and Conflict-Affected Populations; Springer: Berlin/Heidelberg, Germany, 2018; pp. 111–133. [Google Scholar]
- Killgore, W.D.; Taylor, E.C.; Cloonan, S.A.; Dailey, N.S. Psychological resilience during the COVID-19 lockdown. Psychiatry Res. 2020, 291, 113216. [Google Scholar] [CrossRef]
- Kwok, K.O.; Li, K.K.; Chan, H.H.; Yi, Y.Y.; Tang, A.; Wei, W.I.; Wong, S.Y.S. Community responses during the early phase of the COVID-19 epidemic in Hong Kong: Risk perception, information exposure and preventive measures. MedRxiv 2020. [Google Scholar] [CrossRef]
- Lau, B.H.; Chan, C.L.; Ng, S.-M. Resilience of Hong Kong people in the COVID-19 pandemic: Lessons learned from a survey at the peak of the pandemic in Spring 2020. Asia Pac. J. Soc. Work. Dev. 2020, 1–10. [Google Scholar] [CrossRef]
- Wang, K.; Shi, H.-S.; Geng, F.-L.; Zou, L.-Q.; Tan, S.-P.; Wang, Y.; Neumann, D.L.; Shum, D.H.K.; Chan, R.C.K. Cross-cultural validation of the Depression Anxiety Stress Scale–21 in China. Psychol. Assess. 2016, 28, 88. [Google Scholar] [CrossRef]
- Lin, C.; Lee, S.; Wu, B.; Huang, L.; Sun, H.; Tsen, H. Psychometric properties of the Taiwanese version of the World Health Organization-Five Well-Being index. Acta Psychiatr. Scand. 2013, 127, 331. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.M.Y.; Hui, C.L.M.; Wong, C.S.M.; Suen, Y.N.; Chan, S.K.W.; Lee, E.H.M.; Chang, W.C.; Chen, E.Y.H. Prospective prediction of PTSD and depressive symptoms during social unrest and COVID-19 using a brief online tool. Psychiatry Res. 2021, 298, 113773. [Google Scholar] [CrossRef]
- Mind, H.K. Mind Hong Kong Urges Hongkongers to Ask Themselves How They Feel #BehindTheMask This World Mental Health Day 2020. Available online: https://www.mind.org.hk/press-releases/behindthemask-wmhd-press-release-oct-2020/ (accessed on 15 May 2021).
- Topp, C.W.; Østergaard, S.D.; Søndergaard, S.; Bech, P. The WHO-5 Well-Being Index: A systematic review of the literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef]
- Wang, L.; Shi, Z.; Zhang, Y.; Zhang, Z. Psychometric properties of the 10-item Connor–Davidson Resilience Scale in Chinese earthquake victims. Psychiatry Clin. Neurosci. 2010, 64, 499–504. [Google Scholar] [CrossRef]
- Cournane, S.; Byrne, D.; O’Riordan, D.; Fitzgerald, B.; Silke, B. Chronic disabling disease—Impact on outcomes and costs in emergency medical admissions. QJM Int. J. Med. 2015, 108, 387–396. [Google Scholar] [CrossRef][Green Version]
- Hooper, D.; Coughlan, J.; Mullen, M. Structural Equation Modelling: Guidelines for Determining Model Fit. Electron. J. Bus. Res. Methods 2008, 6, 7. [Google Scholar]
- Choi, E.P.H.; Hui, B.P.H.; Wan, E.Y.F. Depression and anxiety in Hong Kong during COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 3740. [Google Scholar] [CrossRef]
- Hou, W.K.; Lee, T.M.-C.; Liang, L.; Li, T.W.; Liu, H.; Ettman, C.K.; Galea, S. Civil unrest, COVID-19 stressors, anxiety, and depression in the acute phase of the pandemic: A population-based study in Hong Kong. Soc. Psychiatry Psychiatr. Epidemiol. 2021. [Google Scholar] [CrossRef]
- Le, K.; Nguyen, M. The psychological burden of the COVID-19 pandemic severity. Econ. Hum. Biol. 2021, 41, 100979. [Google Scholar] [CrossRef]
- Campbell-Sills, L.; Forde, D.R.; Stein, M.B. Demographic and childhood environmental predictors of resilience in a community sample. J. Psychiatr. Res. 2009, 43, 1007–1012. [Google Scholar] [CrossRef]
- Irigoyen-Camacho, M.E.; Velazquez-Alva, M.C.; Zepeda-Zepeda, M.A.; Cabrer-Rosales, M.F.; Lazarevich, I.; Castaño-Seiquer, A. Effect of Income Level and Perception of Susceptibility and Severity of COVID-19 on Stay-at-Home Preventive Behavior in a Group of Older Adults in Mexico City. Int. J. Environ. Res. Public Health 2020, 17, 7418. [Google Scholar] [CrossRef]
- Joyce, S.; Shand, F.; Tighe, J.; Laurent, S.J.; Bryant, R.A. Harvey SB. Road to resilience: A systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open 2018, 8. [Google Scholar] [CrossRef]
- Kim, G.M.; Lim, J.Y.; Kim, E.J.; Park, S.M. Resilience of patients with chronic diseases: A systematic review. Health Soc. Care Community 2019, 27, 797–807. [Google Scholar] [CrossRef] [PubMed]
- Litvin, S.; Saunders, R.; Maier, M.A.; Lüttke, S. Gamification as an approach to improve resilience and reduce attrition in mobile mental health interventions: A randomized controlled trial. PLoS ONE 2020, 15, e0237220. [Google Scholar] [CrossRef]
- Linardon, J.; Fuller-Tyszkiewicz, M. Attrition and adherence in smartphone-delivered interventions for mental health problems: A systematic and meta-analytic review. J. Consult. Clin. Psychol. 2020, 88, 1. [Google Scholar] [CrossRef]
- Wong, B.Y.-M.; Lam, T.-H.; Lai, A.Y.-K.; Wang, M.P.; Ho, S.-Y. Perceived Benefits and Harms of the COVID-19 Pandemic on Family Well-Being and Their Sociodemographic Disparities in Hong Kong: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 1217. [Google Scholar] [CrossRef]
- Gerussi, V.; Peghin, M.; Palese, A.; Bressan, V.; Visintini, E.; Bontempo, G.; Graziano, E.; De Martino, M.; Isola, M.; Tascini, C. Vaccine Hesitancy among Italian Patients Recovered from COVID-19 Infection towards Influenza and Sars-Cov-2 Vaccination. Vaccines 2021, 9, 172. [Google Scholar] [CrossRef]
- Sherman, S.M.; Smith, L.E.; Sim, J.; Amlôt, R.; Cutts, M.; Dasch, H.; Rubin, G.J.; Sevdalis, N. COVID-19 vaccination intention in the UK: Results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum. Vaccines Immunother. 2020. [Google Scholar] [CrossRef]
- Williams, L.; Gallant, A.J.; Rasmussen, S.; Brown Nicholls, L.A.; Cogan, N.; Deakin, K.; Young, D.; Flowers, P. Towards intervention development to increase the uptake of COVID-19 vaccination among those at high risk: Outlining evidence-based and theoretically informed future intervention content. Br. J. Health Psychol. 2020, 25, 1039–1054. [Google Scholar] [CrossRef]
- Nguyen, K.H.; Srivastav, A.; Razzaghi, H.; Williams, W.; Lindley, M.C.; Jorgensen, C.; Abad, N.; Singleton, J.A. COVID-19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination—United States, September and December 2020. Am. J. Transplant. 2021. [Google Scholar] [CrossRef] [PubMed]
- When You’ve Been Fully Vaccinated. Available online: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/fully-vaccinated.html (accessed on 25 May 2021).
| Variables | N | % |
|---|---|---|
| Age | ||
| <55 | 106 | 26.0% |
| 55–64 | 145 | 35.5% |
| 65 or above | 157 | 38.5% |
| Sex | ||
| Female | 250 | 61.3% |
| Male | 158 | 38.7% |
| Type of chronic disease | ||
| Hypertension | 167 | 40.9% |
| Diabetes | 123 | 30.1% |
| Heart disease | 61 | 15.0% |
| Rheumatoid arthritis | 47 | 11.5% |
| Stroke | 37 | 9.1% |
| Systemic Lupus Erythematosus | 20 | 4.9% |
| Ankylosing Spondylitis | 28 | 6.9% |
| Cancer | 17 | 4.2% |
| Asthma | 11 | 2.7% |
| Brain injury | 6 | 1.5% |
| Epilepsy | 6 | 1.5% |
| Disabling effect of chronic conditions | ||
| 1 type | 243 | 59.6% |
| 2 types | 107 | 26.2% |
| 3 types | 44 | 10.8% |
| 4 types | 14 | 3.4% |
| Working status | ||
| Yes (full-time/part-time/self-employment) | 126 | 30.9% |
| No | 282 | 69.1% |
| Perceived risk of infection of COVID-19 (Mean, SD) | 3.79 | 2.12 |
| Variables | Mean | SD | Bivariate Correlations | |||
|---|---|---|---|---|---|---|
| DASS-21 | 2 | 3 | 4 | 5 | ||
| 1. Depression | 7.64 | 8.47 | 0.62 | 0.73 | −0.59 | −0.54 |
| Mild | 42 | 10.3% | ||||
| Moderate | 60 | 14.5% | ||||
| Severe or above | 47 | 11.5% | ||||
| 2. Anxiety | 8.02 | 7.35 | 0.62 | −0.45 | −0.41 | |
| Mild | 42 | 10.3% | ||||
| Moderate | 60 | 14.7% | ||||
| Severe or above | 47 | 11.5% | ||||
| 3. Stress | 10.93 | 9.08 | −0.61 | −0.57 | ||
| Mild | 40 | 9.8% | ||||
| Moderate | 55 | 13.5% | ||||
| Severe or above | 27 | 6.6% | ||||
| 4. WHO-5 | 47.66 | 22.44 | 0.64 | |||
| With depressive symptoms | 215 | 52.7% | ||||
| 5. CDRS-10 | 26.99 | 7.86 | ||||
| Daily Lifestyles | Increase | Decrease | Same | None | Change or None |
|---|---|---|---|---|---|
| N (%) | |||||
| Physical exercises | 55 (13.5%) | 189 (46.3%) | 143 (35.0%) | 21 (5.1%) | 265 (65.0%) |
| Outdoor activities | 16 (3.9%) | 278 (68.1%) | 106 (26.0%) | 8 (2.0%) | 302 (74.0%) |
| Utilization of NGO services | 22 (5.4%) | 256 (62.7%) | 53 (13.0%) | 77 (18.9%) | 355 (87.0%) |
| Utilization of SHO services | 17 (4.2%) | 200 (49.0%) | 42 (10.3%) | 149 (36.5%) | 366 (89.7%) |
| Contact with others | 41 (10.0%) | 202 (49.5%) | 154 (37.7%) | 11 (2.7%) | 254 (62.3%) |
| Gathering with others | 3 (0.7%) | 363 (89.0%) | 33 (8.1%) | 9 (2.2%) | 375 (91.9%) |
| Change or None of Life Behavior | No | Yes | p-Value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Exercise | |||||
| DASS-21 Depression | 6.02 | 7.97 | 8.52 | 8.61 | 0.004 |
| DASS-21 Anxiety | 6.76 | 7.14 | 8.70 | 7.38 | 0.010 |
| DASS-21 Stress | 8.74 | 8.92 | 12.11 | 8.97 | 0.000 |
| WHO-5 | 51.05 | 22.86 | 45.83 | 22.04 | 0.027 |
| CDRS-10 | 28.36 | 7.48 | 26.25 | 7.98 | 0.008 |
| Outdoor Activities | |||||
| DASS-21 Depression | 6.31 | 8.63 | 8.11 | 8.38 | 0.063 |
| DASS-21 Anxiety | 6.87 | 7.42 | 8.43 | 7.29 | 0.063 |
| DASS-21 Stress | 8.92 | 9.03 | 11.64 | 9.01 | 0.008 |
| WHO-5 | 53.25 | 22.60 | 45.70 | 22.09 | 0.003 |
| CDRS-10 | 29.11 | 7.90 | 26.24 | 7.72 | 0.001 |
| Utilization of NGO services | |||||
| DASS-21 Depression | 6.27 | 7.84 | 7.85 | 8.55 | 0.182 |
| DASS-21 Anxiety | 6.34 | 7.27 | 8.27 | 7.34 | 0.076 |
| DASS-21 Stress | 9.58 | 9.03 | 11.13 | 9.09 | 0.247 |
| WHO-5 | 53.89 | 22.87 | 46.73 | 22.26 | 0.037 |
| CDRS-10 | 28.02 | 8.12 | 26.83 | 7.82 | 0.322 |
| Utilization of SHO services | |||||
| DASS-21 Depression | 6.08 | 8.04 | 7.82 | 8.51 | 0.193 |
| DASS-21 Anxiety | 5.75 | 6.78 | 8.28 | 7.38 | 0.027 |
| DASS-21 Stress | 7.67 | 8.08 | 11.30 | 9.13 | 0.009 |
| WHO-5 | 57.14 | 22.41 | 46.57 | 22.22 | 0.006 |
| CDRS-10 | 29.74 | 6.95 | 26.67 | 7.91 | 0.010 |
| Contact with others | |||||
| DASS-21 Depression | 6.00 | 8.18 | 8.64 | 8.50 | 0.002 |
| DASS-21 Anxiety | 6.75 | 6.94 | 8.79 | 7.49 | 0.006 |
| DASS-21 Stress | 8.48 | 8.64 | 12.42 | 9.04 | 0.000 |
| WHO-5 | 54.05 | 21.16 | 43.78 | 22.35 | 0.000 |
| CDRS-10 | 29.29 | 7.73 | 25.59 | 7.62 | 0.000 |
| Gathering with others | |||||
| DASS-21 Depression | 6.68 | 8.94 | 7.73 | 8.43 | 0.521 |
| DASS-21 Anxiety | 7.32 | 7.29 | 8.08 | 7.36 | 0.567 |
| DASS-21 Stress | 9.55 | 9.15 | 11.05 | 9.08 | 0.370 |
| WHO-5 | 56.12 | 20.14 | 46.91 | 22.50 | 0.017 |
| CDRS-10 | 29.33 | 8.78 | 26.78 | 7.75 | 0.115 |
| Effect | Estimate | 95% LCI | 95% UCI | p-Value | % |
|---|---|---|---|---|---|
| Direct effect (changes in daily lifestyles → mental health) | −0.15 | −0.36 | 0.05 | 0.147 | 35.2% |
| Indirect effect (changes in daily lifestyles → resilience → mental health) | −0.28 | −0.44 | −0.10 | 0.001 | 64.8% |
| Total effect | −0.43 | −0.72 | −0.12 | 0.004 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lau, B.H.P.; Cheung, M.K.T.; Chan, L.T.H.; Chan, C.L.W.; Leung, P.P.Y. Resilience in the Storm: Impacts of Changed Daily Lifestyles on Mental Health in Persons with Chronic Illnesses under the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 5875. https://doi.org/10.3390/ijerph18115875
Lau BHP, Cheung MKT, Chan LTH, Chan CLW, Leung PPY. Resilience in the Storm: Impacts of Changed Daily Lifestyles on Mental Health in Persons with Chronic Illnesses under the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2021; 18(11):5875. https://doi.org/10.3390/ijerph18115875
Chicago/Turabian StyleLau, Bobo H. P., Mike K. T. Cheung, Lucian T. H. Chan, Cecilia L. W. Chan, and Pamela P. Y. Leung. 2021. "Resilience in the Storm: Impacts of Changed Daily Lifestyles on Mental Health in Persons with Chronic Illnesses under the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 18, no. 11: 5875. https://doi.org/10.3390/ijerph18115875
APA StyleLau, B. H. P., Cheung, M. K. T., Chan, L. T. H., Chan, C. L. W., & Leung, P. P. Y. (2021). Resilience in the Storm: Impacts of Changed Daily Lifestyles on Mental Health in Persons with Chronic Illnesses under the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 18(11), 5875. https://doi.org/10.3390/ijerph18115875






