Timing of Home Health Care Initiation and 30-Day Rehospitalizations among Medicare Beneficiaries with Diabetes by Race and Ethnicity
Abstract
1. Introduction
2. Materials and Methods
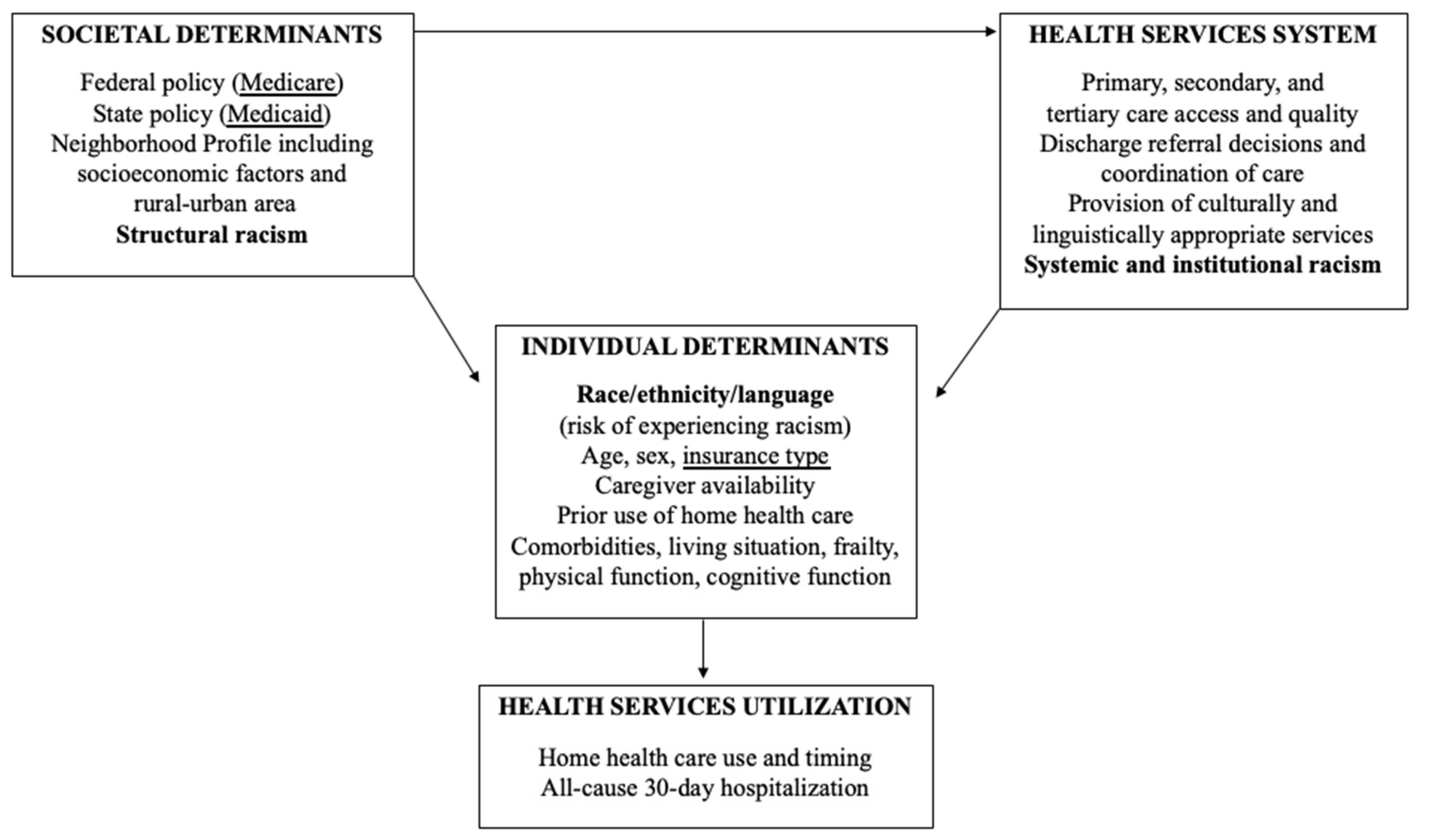
2.1. Study Design and Conceptual Framework
2.2. Study Population
2.3. Data Sources and Variables
2.4. Analytic Approach
3. Results
3.1. Patient Characteristics by Timing of the First Home Health Care Visit
3.2. Balance of Predictors after Propensity Score Weighting
3.3. Home Health Care Timing and Rehospitalization
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Enomoto, L.M.; Shrestha, D.P.; Rosenthal, M.B.; Hollenbeak, C.S.; Gabbay, R.A. Risk factors associated with 30-day readmission and length of stay in patients with type 2 diabetes. J. Diabetes Complicat. 2017, 31, 122–127. [Google Scholar] [CrossRef]
- Sonmez, H.; Kambo, V.; Avtanski, D.; Lutsky, L.; Poretsky, L. The readmission rates in patients with versus those without diabetes mellitus at an urban teaching hospital. J. Diabetes Complicat. 2017, 31, 1681–1685. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, K.N.; McHugh, S.M.; Tracey, M.L.; Fitzgerald, A.P.; Kearney, P.M. Health service utilization and related costs attributable to diabetes. Diabet. Med. 2018, 35, 1727–1734. [Google Scholar] [CrossRef]
- American Diabetes Association. Economic costs of diabetes in the U.S. in 2017. Diabetes Care 2018, 41, 917–928. [Google Scholar] [CrossRef] [PubMed]
- Whitehouse, C.R.; Sharts-Hopko, N.C.; Smeltzer, S.C.; Horowitz, D.A. Supporting transitions in care for older adults with type 2 diabetes mellitus and obesity. Res. Geront. Nurs. 2018, 11, 71–81. [Google Scholar] [CrossRef] [PubMed]
- LaManna, J.B.; Bushy, A.; Norris, A.E.; Chase, S.K. Early and intermediate hospital-to-home transition outcomes of older adults diagnosed with diabetes. Diabetes Educator. 2016, 42, 72–86. [Google Scholar] [CrossRef] [PubMed]
- Chase, J.D.; Russell, D.; Huang, L.; Hanlon, A.; O’Connor, M.; Bowles, K.H. Relationships between race/ethnicity and health care utilization among older post-acute home health care patients. J. Appl. Gerontol. 2020, 39, 201–213. [Google Scholar] [CrossRef] [PubMed]
- Xiao, R.; Miller, J.A.; Zafirau, W.J.; Gorodeski, E.Z.; Young, J.B. Impact of home health care on health care resource utilization following hospital discharge: A cohort study. Am. J. Med. 2018, 131, 395–407.e35. [Google Scholar] [CrossRef]
- Hildebrand, J.A.; Billimek, J.; Lee, J.A.; Sorkin, D.H.; Olshansky, E.F.; Clancy, S.L.; Evangelista, L.S. Effect of diabetes self-management education on glycemic control in Latino adults with type 2 diabetes: A systematic review and meta-analysis. Patient Educ. Couns. 2020, 103, 266–275. [Google Scholar] [CrossRef]
- Cunningham, A.T.; Crittendon, D.R.; White, N.; Mills, G.D.; Diaz, V.; LaNoue, M.D. The effect of diabetes self-management education on HbA1c and quality of life in African-Americans: A systematic review and meta-analysis. BMC Health Serv. Res. 2018, 18, 367. [Google Scholar] [CrossRef] [PubMed]
- Beck, J.; Greenwood, D.A.; Blanton, L.; Bollinger, S.T.; Butcher, M.K.; Condon, J.E.; Cypress, M.; Faulkner, P.; Fischl, A.H.; Francis, T.; et al. 2017 national standards for diabetes self-management education and support. Diabetes Spectr. 2017, 30, 301–314. [Google Scholar] [CrossRef]
- Topaz, M.; Trifilio, M.; Maloney, D.; Bar-Bachar, O.; Bowles, K.H. Improving patient prioritization during hospital-homecare transition: A pilot study of a clinical decision support tool. Res. Nurs. Health 2018, 41, 440–447. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, M.; Bowles, K.H.; Feldman, P.H.; St Pierre, S.; Jarrín, O.; Shah, S.; Murtaugh, C.M. Frontloading and intensity of skilled home health visits: A state of the science. Home Health Care Serv. Q. 2014, 33, 159–175. [Google Scholar] [CrossRef]
- Wang, J.; Liebel, D.V.; Yu, F.; Caprio, T.V.; Shang, J. Inverse dose-response relationship between home health care services and rehospitalization in older adults. J. Am. Med. Dir. Assoc. 2019, 20, 736–742. [Google Scholar] [CrossRef] [PubMed]
- Murtaugh, C.M.; Deb, P.; Zhu, C.; Peng, T.R.; Barron, Y.; Shah, S.; Moore, S.M.; Bowles, K.H.; Kalman, J.; Feldman, P.H.; et al. Reducing readmissions among heart failure patients discharged to home health care: Effectiveness of early and intensive nursing services and early physician follow-up. Health Serv. Res. 2017, 52, 1445–1472. [Google Scholar] [CrossRef] [PubMed]
- Irani, E.; Hirschman, K.B.; Cacchione, P.Z.; Bowles, K.H. Home health nurse decision-making regarding visit intensity planning for newly admitted patients: A qualitative descriptive study. Home Health Care Serv. Q. 2018, 37, 211–231. [Google Scholar] [CrossRef]
- Li, J.; Qi, M.; Werner, R.M. Assessment of receipt of the first home health care visit after hospital discharge among older adults. JAMA Netw. Open 2020, 3, e2015470. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.M.; Jarrín, O.F.; Lin, H.; Tsui, J.; Dharamdasani, T.; Thomas-Hawkins, C. Post-acute home health care referral and utilization in older adults with diabetes. Int. J. Environ. Res. Public Health 2021, 18, 3196. [Google Scholar] [CrossRef]
- Bowles, K.H.; Ratcliffe, S.J.; Holmes, J.H.; Keim, S.; Potashnik, S.; Flores, E.; Humbrecht, D.; Whitehouse, C.R.; Naylor, M.D. Using a decision support algorithm for referrals to post-acute care. J. Am. Med. Dir. Assoc. 2019, 20, 408–413. [Google Scholar] [CrossRef]
- Centers for Medicare and Medicaid Services QualityNet. Hospital Readmissions Reduction Program: Payment Reduction Methodology. Available online: https://qualitynet.cms.gov/inpatient/hrrp/methodology (accessed on 29 April 2021).
- Rodríguez, H.P.; Fulton, B.D.; Phillips, A.Z. The early impact of the Centers for Medicare & Medicaid Services State Innovation Models Initiative on 30-day hospital readmissions among adults with diabetes. Med. Care 2020, 58 (Suppl. 6), S22–S30. [Google Scholar] [CrossRef]
- Andersen, R.M.; Newman, J.F. Societal and individual determinants of medical care utilization in the United States. Milbank Q. 2005, 83, 1–28. [Google Scholar] [CrossRef]
- Ogunwole, S.M.; Golden, S.H. Social determinants of health and structural inequities- Root causes of diabetes disparities. Diabetes Care 2021, 44, 11–13. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.J.; Andrews, R.; Stryer, D.; Friedman, B. Racial/ethnic disparities in potentially preventable readmissions: The case of diabetes. Am. J. Public Health 2005, 95, 1561–1567. [Google Scholar] [CrossRef] [PubMed]
- Jarrín, O.F.; Nyandege, A.N.; Grafova, I.B.; Dong, X.; Lin, H. Validity of race and ethnicity codes in Medicare administrative data compared with gold-standard self-reported Race collected during routine home health care visits. Med. Care 2020, 58, e1–e8. [Google Scholar] [CrossRef] [PubMed]
- Grafova, I.B.; Jarrín, O.F. Beyond black and white: Mapping misclassification Medicare beneficiaries’ race and ethnicity. Med. Care Res. Rev. 2020. online first. [Google Scholar] [CrossRef]
- Moore, B.J.; White, S.; Washington, R.; Coenen, N.; Elixhauser, A. Identifying increased risk of readmission and in-hospital mortality using hospital administrative data: The AHRQ Elixhauser Comorbidity Index. Med. Care 2017, 55, 698–705. [Google Scholar] [CrossRef]
- Kind, A.J.; Jencks, S.; Brock, J.; Yu, M.; Bartels, C.; Ehlenbach, W.; Greenberg, C.; Smith, M. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: A retrospective cohort study. Ann. Intern. Med. 2014, 161, 765–774. [Google Scholar] [CrossRef]
- U.S. Department of Agriculture. Rural-urban Continuum Codes Documentation. Available online: https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/documentation/ (accessed on 28 February 2021).
- Rosenbaum, P.R.; Rubin, D.B. The central role of the propensity score in observational studies for causal effects. Biometrika 1983, 70, 41–55. [Google Scholar] [CrossRef]
- Austin, P.C.; Stuart, E.A. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Statist. Med. 2015, 34, 3661–3679. [Google Scholar] [CrossRef]
- Hernán, M.A.; Robins, J.M. Estimating causal effects from epidemiological data. J. Epi. Comm. Health 2006, 60, 578–586. [Google Scholar] [CrossRef]
- Centers for Medicare and Medicaid Services. Center for Clinical Standards and Quality/Quality, Safety & Oversight Group. Home Health Agency (HHA) Interpretive Guidelines. August 2018. Available online: https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/QSO18-25-HHA.pdf (accessed on 1 May 2021).
- Centers for Medicare & Medicaid Services. Home Health Care–National Data. The National Averages for Critical Quality Measures of Home Health Agencies. Available online: https://data.cms.gov/provider-data/dataset/97z8-de96 (accessed on 1 May 2021).
- Deb, P.; Murtaugh, C.M.; Bowles, K.H.; Mikkelson, M.E.; Nouri Khajavi, H.; Moore, S.; Barron, Y.; Feldman, P.H. Does early follow-up improve the outcomes of sepsis survivors discharged to home health care? Med. Care 2019, 57, 633–640. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.F.; Popoola, T.; Radhakrishnan, K.; Suzuki, S.; Homan, S. Improving diabetic patient transition to home healthcare: Leading risk factors for 30-day readmission. Am. J. Manag. Care 2015, 21, 440–450. [Google Scholar] [PubMed]
- Eby, E.; Hardwick, C.; Yu, M.; Gelwicks, S.; Deschamps, K.; Xie, J.; George, T. Predictors of 30 day hospital readmission in patients with type 2 diabetes: A retrospective, case-control, database study. Curr. Med. Res. Opin. 2015, 31, 107–114. [Google Scholar] [CrossRef]
- Menke, A.; Casagrande, S.; Geiss, L.; Cowie, C.C. Prevalence of and trends in diabetes among adults in the United States, 1988–2012. JAMA 2015, 314, 1021–1029. [Google Scholar] [CrossRef] [PubMed]
- Walker, R.J.; Strom Williams, J.; Egede, L.E. Influence of race, ethnicity and social determinants of health on diabetes outcomes. Am. J. Med. Sci. 2016, 351, 366–373. [Google Scholar] [CrossRef] [PubMed]
- Raval, A.D.; Zhou, S.; Wei, W.; Bhattacharjee, S.; Miao, R.; Sambamoorthi, U. 30-day readmission among elderly Medicare beneficiaries with type 2 diabetes. Popul. Health Manag. 2015, 18, 256–264. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.; Lloyd, J.T.; Giuriceo, K.; Day, T.; Shrank, W.; Rajkumar, R. Systematic review and meta-analysis of patient race/ethnicity, socioeconomics, and quality for adult type 2 diabetes. Health Serv. Res. 2020, 55, 741–772. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.D.; Wald, H.L.; Boxer, R.S.; Masoudi, F.A.; Burke, R.E.; Capp, R.; Coleman, E.A.; Ginde, A.A. Characteristics associated with home health care referrals at hospital discharge: Results from the 2012 National Inpatient Sample. Health Serv. Res. 2017, 52, 879–894. [Google Scholar] [CrossRef]
- Gandhi, K.; Lim, E.; Davis, J.; Chen, J.J. Racial disparities in health service utilization among Medicare fee-for-service beneficiaries adjusting for multiple chronic conditions. J. Aging Health 2018, 30, 1224–1243. [Google Scholar] [CrossRef]
- Fang, M. Trends in the prevalence of diabetes among U.S. adults: 1999–2016. Am. J. Prev. Med. 2018, 55, 497–505. [Google Scholar] [CrossRef]
- Chen, H.F.; Homan, S.; Carlson, E.; Popoola, T.; Radhakrishnan, K. The impact of race and neighborhood racial composition on preventable readmissions for diabetic Medicare home health beneficiaries. J. Rac. Ethn. Health Disparities 2017, 4, 648–658. [Google Scholar] [CrossRef] [PubMed]
- Phillips, A.Z.; Rodriguez, H.P. Adults with diabetes residing in “food swamps” have higher hospitalization rates. Health Serv. Res. 2019, 54, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R.; Lawrence, J.A.; Davis, B.A. Racism and health: Evidence and needed research. Annu. Rev. Public Health 2019, 40, 105–125. [Google Scholar] [CrossRef] [PubMed]
- Krieger, N. Discrimination and health inequities. Int. J. Health Serv. 2014, 44, 643–710. [Google Scholar] [CrossRef]
- Bailey, Z.D.; Krieger, N.; Agénor, M.; Graves, J.; Linos, N.; Bassett, M.T. Structural racism and health inequities in the USA: Evidence and interventions. Lancet 2017, 389, 1453–1463. [Google Scholar] [CrossRef]
- Centers for Medicare & Medicaid Services (CMS) Center for Medicare & Medicaid Innovation. Evaluation of the Home Health Value-Based Purchasing (HHVBP) Model, Third Annual Report. 2020. Available online: https://innovation.cms.gov/data-and-reports/2020/hhvbp-thirdann-rpt (accessed on 28 February 2021).
- American Hospital Association. ICD-10-CM Coding for Social Determinants of Health. Available online: https://www.aha.org/system/files/2018-04/value-initiative-icd-10-code-social-determinants-of-health.pdf (accessed on 30 April 2021).
- Davitt, J.K.; Bourjolly, J.; Frasso, R. Understanding inequities in home health care outcomes: Staff views on agency and system factors. Res. Gerontol. Nurs. 2015, 8, 119–129. [Google Scholar] [CrossRef]
- Crist, J.D.; Koerner, K.M.; Hepworth, J.T.; Pasvogel, A.; Marshall, C.A.; Cruz, T.P.; Effken, J.A. Differences in transitional care provided to Mexican American and non-Hispanic white older adults. J. Transcult. Nurs. 2017, 28, 159–167. [Google Scholar] [CrossRef]
- Bleich, S.N.; Findling, M.G.; Casey, L.S.; Blendon, R.J.; Benson, J.M.; Steelfisher, G.K.; Sayde, J.M.; Miller, C. Discrimination in the United States: Experiences of Black Americans. Health Serv. Res. 2019, 54, 1399–1408. [Google Scholar] [CrossRef]
- Sefcik, J.S.; Ritter, A.Z.; Flores, E.J.; Nock, R.H.; Chase, J.D.; Bradway, C.; Potashnik, S.; Bowles, K.H. Why older adults may decline offers of post-acute care services: A qualitative descriptive study. Geriatr. Nurs. 2017, 38, 238–243. [Google Scholar] [CrossRef]
- Nardi, D.; Waite, R.; Nowak, M.; Hatcher, B.; Hines-Marin, V.; Stacciarini, J.R. Achieving health equity through eradicating structural racism in the United States: A call to action for nursing leadership. J. Nurs. Scholarsh. 2020, 52, 696–704. [Google Scholar] [CrossRef]
- Golden, S.H.; Joseph, J.J.; Hill-Briggs, F. Casting a health equity lens on endocrinology and diabetes. J. Clin. Endocrinol. Metab. 2021, 106, e1909–e1916. [Google Scholar] [CrossRef] [PubMed]
- Ford, C.L.; Jeffers, K.S. Critical race theory’s antiracism approaches: Moving from the ivory tower to the front lines of public health. In Racism: Science & Tools for the Public Health Professional; Ford, C.L., Griffith, D.M., Bruce, M.A., Gilbert, K.L., Eds.; American Public Health Association: Washington, DC, USA, 2019; pp. 327–342. ISBN 978-0-87553-303-2. [Google Scholar]
- Karunakaran, A.; Zhao, H.; Rubin, D.J. Predischarge and postdischarge risk factors for hospital readmission among patients with diabetes. Med. Care 2018, 56, 634–642. [Google Scholar] [CrossRef] [PubMed]
- Skopec, L.; Zuckerman, S.; Aarons, J.; Wissoker, D.; Huckfeldt, P.J.; Feder, J.; Berenson, R.A.; Dey, J.; Oliveira, I. Home health use in Medicare Advantage compared to use in traditional Medicare. Health Aff. 2020, 39, 1072–1079. [Google Scholar] [CrossRef] [PubMed]
| Timing of the First Home Health Care Visit | |||||
|---|---|---|---|---|---|
| Total n = 786,734 | Day 0–2 153,132 (19.5) | Day 3–7 46,659 (5.9) | Day 8–14 13,975 (1.8) | Not Received 572,968 (72.8) | |
| Race/Ethnicity | |||||
| White | 534,725 | 108,661 (20.3) | 29,450 (5.5) | 8806 (1.6) | 387,808 (72.5) |
| Black | 134,246 | 26,321 (19.6) | 10,443 (7.8) | 3045 (2.3) | 94,437 (70.3) |
| Hispanic | 86,824 | 13,897 (16.0) | 5233 (6.0) | 1665 (1.9) | 66,029 (76.0) |
| Asian American/Pacific Islander | 19,888 | 3409 (17.1) | 1234 (6.2) | 365 (1.8) | 14,880 (74.8) |
| American Indian/Alaska Native | 5859 | 834 (14.2) | 299 (5.1) | 94 (1.6) | 4632 (79.1) |
| Unknown | 5192 | - | - | - | 5192 (100) |
| Sex, male | 402,779 | 70,416 (17.5) | 20,060 (5.0) | 6283 (1.6) | 306,020 (76.0) |
| Sex, female | 383,955 | 82,716 (21.5) | 26,599 (6.9) | 7692 (2.0) | 266,948 (69.5) |
| Age (x, SD) | 73.1 (9.7) | 75.50 (10.1) | 75.14 (10.1) | 74.54 (10.2) | 72.30 (9.4) |
| Insurance | |||||
| Fee-for-service (FFS) | 363,675 | 70,665 (19.4) | 19,692 (5.4) | 5882 (1.6) | 267,436 (73.6) |
| FFS + Medicaid | 143,162 | 36,078 (25.2) | 10,664 (7.4) | 3312 (2.3) | 93,108 (65.0) |
| Medicare Advantage (MA) | 189,393 | 29,665 (15.7) | 10,289 (5.4) | 2923 (1.5) | 146,516 (77.4) |
| MA + Medicaid | 90,504 | 16,724 (18.5) | 6014 (6.6) | 1858 (2.1) | 65,908 (72.8) |
| Neighborhood profile | |||||
| Urban, advantaged | 549,157 | 107,109 (19.5) | 32,822 (6.0) | 9558 (1.7) | 399,668 (72.8) |
| Urban, disadvantaged | 98,567 | 19,162 (19.4) | 6777 (6.9) | 2057 (2.1) | 70,571 (71.6) |
| Rural, advantaged | 106,827 | 20,191 (18.9) | 5144 (4.8) | 1682 (1.6) | 79,810 (74.7) |
| Rural, disadvantaged | 32,183 | 6670 (20.7) | 1916 (6.0) | 678 (2.1) | 22,919 (71.2) |
| Elixhauser CI (x, SD) | 30.0 (16.5) | 31.61 (16.5) | 32.22 (16.6) | 31.93 (16.6) | 26.53 (16.3) |
| Common comorbidities | |||||
| Chronic pulmonary disease | 206,479 | 45,509 (22.0) | 13,890 (6.7) | 4117 (2.0) | 142,963 (69.2) |
| Congestive heart failure | 294,105 | 68,420 (23.2) | 20,965 (7.1) | 6011 (2.0) | 198,709 (67.6) |
| Dementia | 128,668 | 39,060 (30.4) | 12,055 (9.4) | 3507 (2.7) | 74,046 (57.5) |
| Depression | 89,824 | 19,688 (21.9) | 6188 (6.9) | 1726 (1.9) | 62,222 (69.3) |
| Diabetes, complicated | 231,299 | 52,197 (22.6) | 15,738 (6.8) | 4626 (2.0) | 158,738 (68.6) |
| End-stage renal disease | 62,900 | 10,960 (17.4) | 4609 (7.3) | 1468 (2.3) | 45,863 (72.9) |
| Fluid/electrolyte | 273,619 | 60,449 (22.1) | 18,910 (6.9) | 5518 (2.0) | 188,742 (69.0) |
| Hypertension | 706,560 | 136,437 (19.3) | 41,964 (5.9) | 12,549 (1.8) | 515,610 (73.0) |
| Peripheral vascular disease | 135,577 | 29,913 (22.1) | 8559 (6.3) | 2652 (2.0) | 94,453 (69.7) |
| Prior home health care (120 days) | 120,823 | 58,908 (48.8) | 16,149 (13.4) | 3866 (3.2) | 41,900 (34.7) |
| Length of stay in days (x, SD) | 3.9 (3.4) | 5.2 (4.1) | 4.6 (4.2) | 4.3 (3.6) | 3.4 (3.0) |
| Discharged to home health care | 209,150 | 120,193 (57.5) | 27,979 (13.4) | 4029 (1.9) | 56,949 (27.2) |
| Discharged to home with self-care | 577,584 | 32,939 (5.7) | 18,680 (3.2) | 9946 (1.7) | 516,019 (89.3) |
| Rehospitalization within 30 days (outcome) | 122,740 | 30,126 (24.5) | 9314 (7.6) | 5626 (4.6) | 77,674 (63.3) |
| Home Health Care Timing | Overall | Discharged to Self-Care | Discharged to Home Health Care |
|---|---|---|---|
| Full Cohort Reference = day 0–2 | OR, 95% CI | OR, 95% CI | OR, 95% CI |
| With propensity score weighting | |||
| Delayed (day 3–7) | 1.28, 1.25–1.32 *** | 1.39, 1.34–1.43 *** | 1.00, 0.95–1.06 |
| Late (day 8–14) | 4.12, 3.97–4.28 *** | 4.72, 4.52–4.94 *** | 2.53, 2.36–2.72 *** |
| No home health care received | 0.98, 0.97–1.00 *** | 0.85, 0.84–0.87 *** | 1.18, 1.15–1.21 *** |
| Without propensity score weighting | |||
| Delayed (day 3–7) | 1.08, 1.05–1.11 *** | 1.18, 1.12–1.23 *** | 0.99, 0.96–1.02 |
| Late (day 8–14) | 3.28, 3.16–3.41 *** | 3.42, 3.26–3.60 *** | 2.43, 2.27–2.60 *** |
| No home health care received | 0.96, 0.95–0.98 *** | 0.85, 0.82–0.88 *** | 1.15, 1.12–1.18 *** |
| Home Health Care Timing | Overall | Discharged to Self-Care | Discharged to Home Health Care |
|---|---|---|---|
| Reference = day 0–2 | OR, 95% CI | OR, 95% CI | OR, 95% CI |
| White | n = 534,725 | n = 390,464 | n = 144,261 |
| Delayed (day 3–7) | 1.33, 1.29–1.38 *** | 1.44, 1.38–1.50 *** | 1.04, 0.98–1.11 |
| Late (day 8–14) | 4.54, 4.34–4.75 *** | 5.16, 4.89–5.44 *** | 2.76, 2.53–3.01 *** |
| No home health care received | 0.98, 0.96–1.00 | 0.83, 0.81–0.85 *** | 1.20, 1.16–1.24 *** |
| Black | n = 134,246 | n = 96,164 | n = 38,082 |
| Delayed (day 3–7) | 1.16, 1.08–1.24 *** | 1.27, 1.17–1.38 *** | 0.94, 0.83–1.06 |
| Late (day 8–14) | 3.32, 3.03–3.64 *** | 3.93, 3.52–4.39 *** | 2.11, 1.78–2.52 *** |
| No home health care received | 1.00, 0.96–1.04 | 0.89, 0.84–0.93 *** | 1.21, 1.13–1.29 *** |
| Hispanic | n = 86,824 | n = 66,989 | n = 19,835 |
| Delayed (day 3-7) | 1.11, 1.02–1.21 * | 1.18, 1.07–1.31 *** | 0.89, 0.75–1.06 |
| Late (day 8–14) | 3.04, 2.70–3.41 *** | 3.30, 2.89–3.77 *** | 2.20, 1.73–2.80 *** |
| No home health care received | 0.94, 0.90–0.99 * | 0.88, 0.83–0.93 *** | 1.07, 0.97–1.17 |
| Asian American/Pacific Islander | n = 19,888 | n = 14,590 | n = 5298 |
| Delayed (day 3–7) | 1.52, 1.27–1.83 *** | 1.94, 1.56–2.42 *** | 0.93, 0.66–1.31 |
| Late (day 8–14) | 4.72, 3.69–6.03 *** | 6.88, 5.14–9.21 *** | 1.91, 1.16–3.14 * |
| No home health care received | 1.09, 0.98–1.22 | 1.19, 1.03–1.37 | 0.93, 0.78–1.12 |
| American Indian/Alaska Native | n = 5859 | n = 4682 | n = 1177 |
| Delayed (day 3–7) | 1.50, 1.08–2.09, p < 0.05 | 1.83, 1.24–2.70 ** | 0.49, 0.21–1.16 |
| Late (day 8–14) | 4.69, 2.95–7.44 *** | 5.97, 3.48–10.25 *** | 1.35, 0.40–4.54 |
| No home health care received | 0.94, 0.77–1.16 | 0.74, 0.57–0.96 | 1.52, 0.99–2.33 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Smith, J.M.; Lin, H.; Thomas-Hawkins, C.; Tsui, J.; Jarrín, O.F. Timing of Home Health Care Initiation and 30-Day Rehospitalizations among Medicare Beneficiaries with Diabetes by Race and Ethnicity. Int. J. Environ. Res. Public Health 2021, 18, 5623. https://doi.org/10.3390/ijerph18115623
Smith JM, Lin H, Thomas-Hawkins C, Tsui J, Jarrín OF. Timing of Home Health Care Initiation and 30-Day Rehospitalizations among Medicare Beneficiaries with Diabetes by Race and Ethnicity. International Journal of Environmental Research and Public Health. 2021; 18(11):5623. https://doi.org/10.3390/ijerph18115623
Chicago/Turabian StyleSmith, Jamie M., Haiqun Lin, Charlotte Thomas-Hawkins, Jennifer Tsui, and Olga F. Jarrín. 2021. "Timing of Home Health Care Initiation and 30-Day Rehospitalizations among Medicare Beneficiaries with Diabetes by Race and Ethnicity" International Journal of Environmental Research and Public Health 18, no. 11: 5623. https://doi.org/10.3390/ijerph18115623
APA StyleSmith, J. M., Lin, H., Thomas-Hawkins, C., Tsui, J., & Jarrín, O. F. (2021). Timing of Home Health Care Initiation and 30-Day Rehospitalizations among Medicare Beneficiaries with Diabetes by Race and Ethnicity. International Journal of Environmental Research and Public Health, 18(11), 5623. https://doi.org/10.3390/ijerph18115623







