The Effect of a Physical Activity Coaching Intervention on Accelerometer-Measured Sedentary Behaviours in Insufficiently Physically Active Ambulatory Hospital Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Intervention
2.3. Outcomes
2.4. Analysis
3. Results
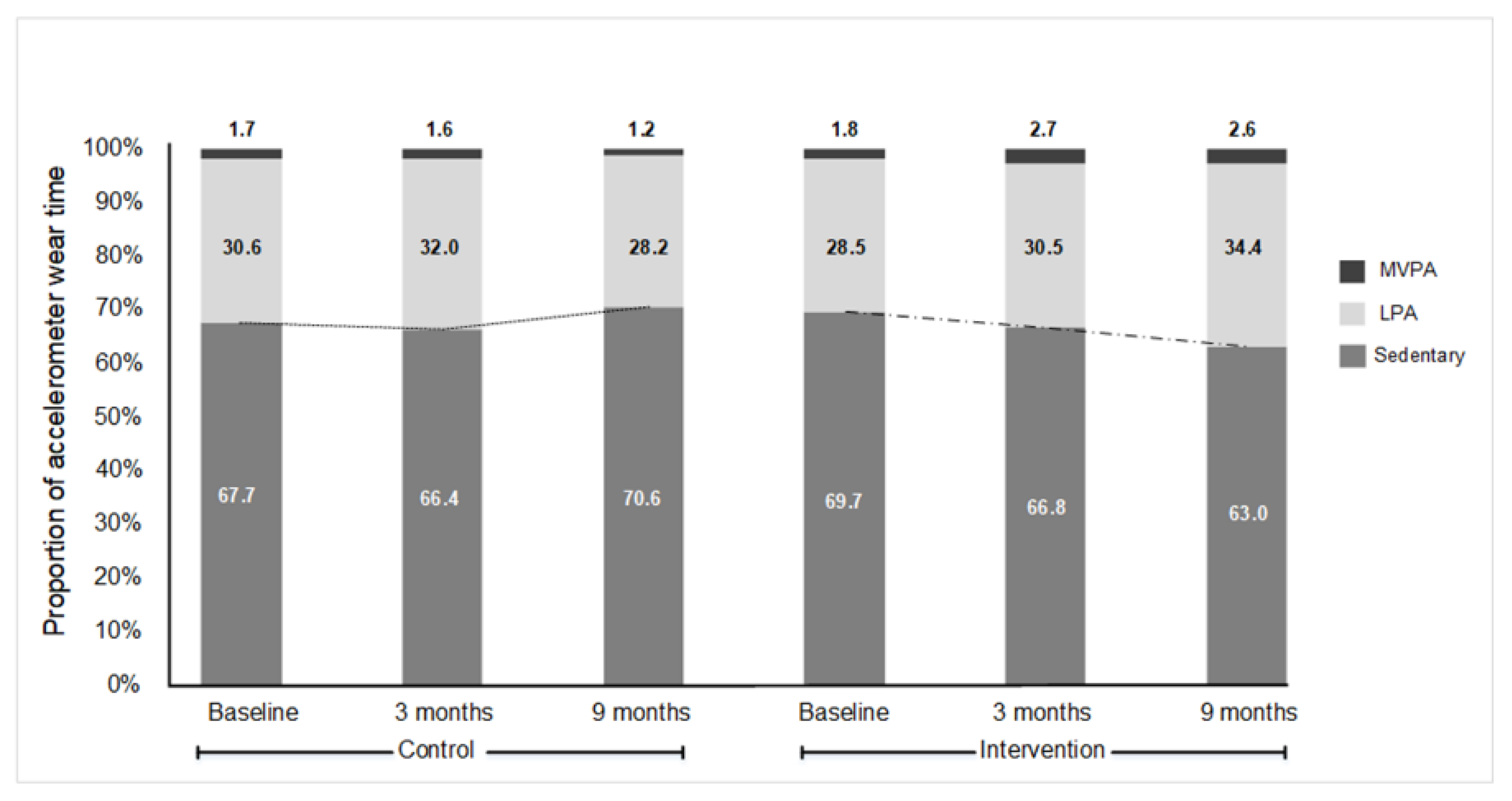
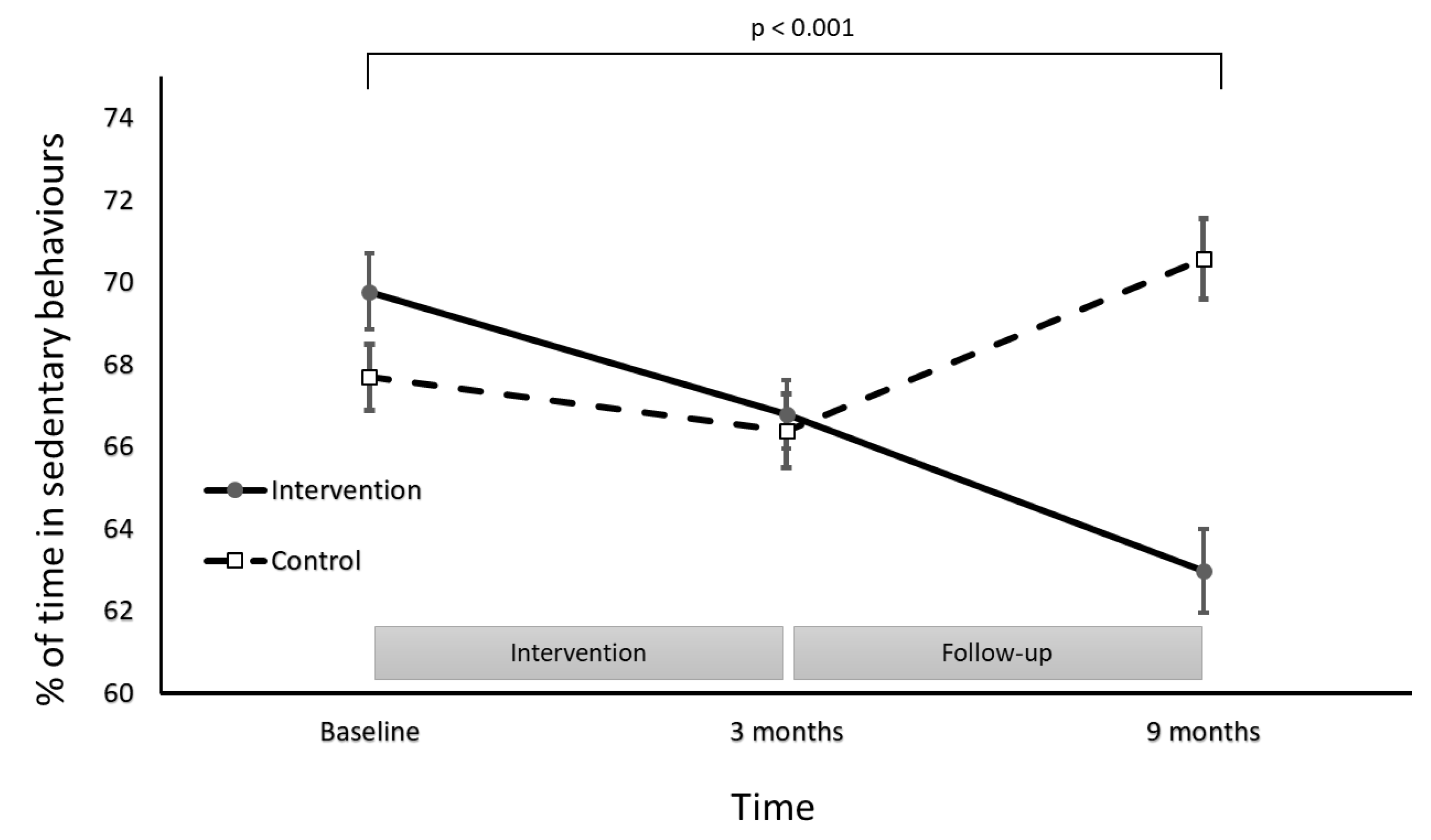
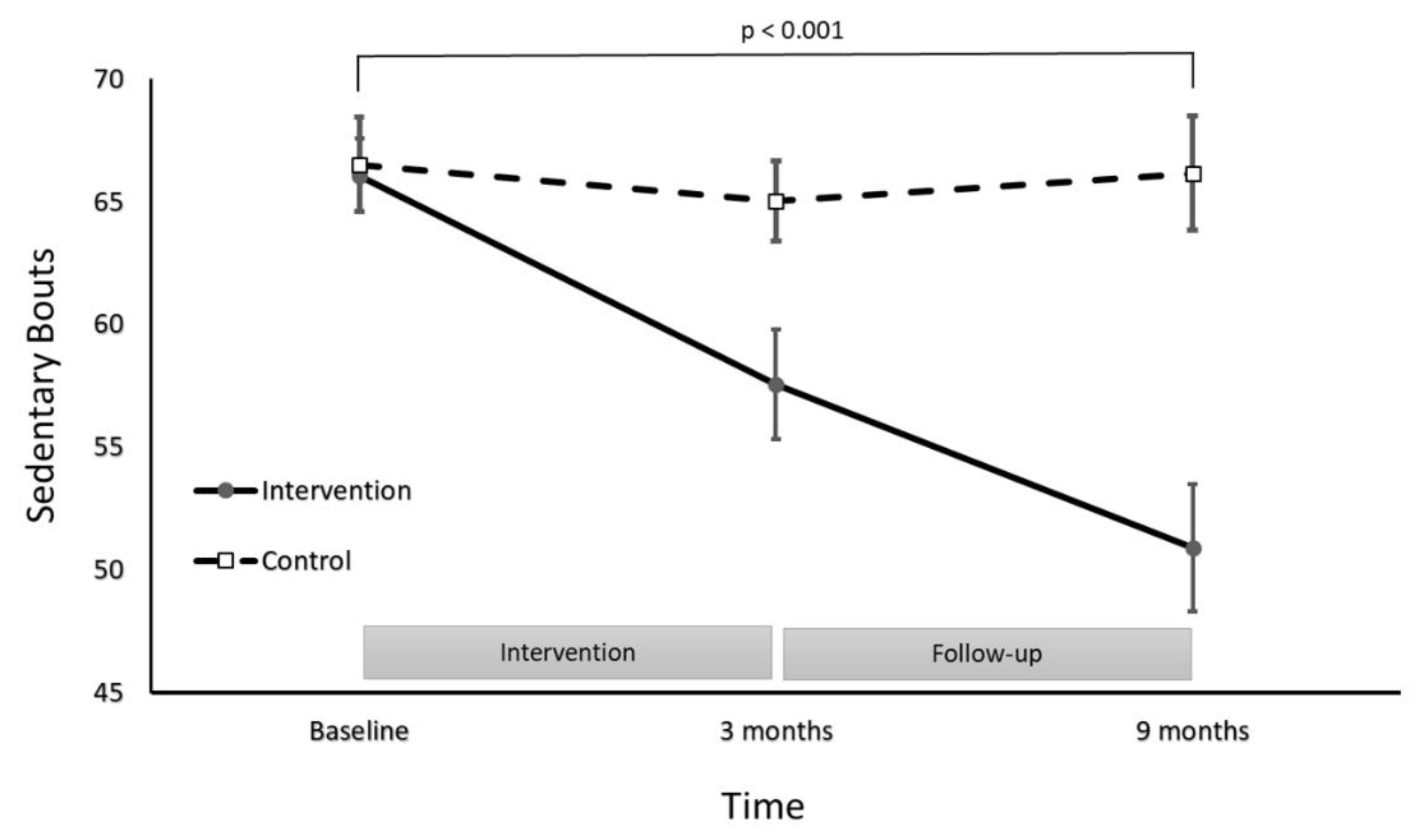
Sedentary Behaviour Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kohl, H.W., 3rd; Craig, C.L.; Lambert, E.V.; Inoue, S.; Alkandari, J.R.; Leetongin, G.; Kahlmeier, S. The pandemic of physical inactivity: Global action for public health. Lancet 2012, 380, 294–305. [Google Scholar] [CrossRef]
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.F.M.; Altenburg, T.M.; Chinapaw, M.J.M. Sedentary Behavior Research Network (SBRN)—Terminology Consensus Project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 75. [Google Scholar] [CrossRef] [PubMed]
- Dempsey, P.C.; Biddle, S.J.H.; Buman, M.P.; Chastin, S.; Ekelund, U.; Friedenreich, C.M.; Katzmarzyk, P.T.; Leitzmann, M.F.; Stamatakis, E.; van der Ploeg, H.P.; et al. New global guidelines on sedentary behaviour and health for adults: Broadening the behavioural targets. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 151. [Google Scholar] [CrossRef] [PubMed]
- Biswas, A.; Oh, P.I.; Faulkner, G.E.; Bajaj, R.R.; Silver, M.A.; Mitchell, M.S.; Alter, D.A. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: A systematic review and meta-analysis. Ann. Int. Med. 2015, 162, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Chomistek, A.K.; Manson, J.E.; Stefanick, M.L.; Lu, B.; Sands-Lincoln, M.; Going, S.B.; Garcia, L.; Allison, M.A.; Sims, S.T.; LaMonte, M.J.; et al. Relationship of sedentary behavior and physical activity to incident cardiovascular disease: Results from the Women’s Health Initiative. J. Am. Coll. Cardiol. 2013, 61, 2346–2354. [Google Scholar] [CrossRef]
- Bauman, A.E.; Petersen, C.B.; Blond, K.; Rangul, V.; Hardy, L.L. The descriptive epidemiology of sedentary behaviour. In Sedentary Behaviour Epidemiology; Springer: Cham, Switzerland, 2018; pp. 73–106. [Google Scholar]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Samdal, G.B.; Eide, G.E.; Barth, T.; Williams, G.; Meland, E. Effective behaviour change techniques for physical activity and healthy eating in overweight and obese adults; systematic review and meta-regression analyses. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 42. [Google Scholar] [CrossRef]
- Martin, A.; Fitzsimons, C.; Jepson, R.; Saunders, D.H.; van der Ploeg, H.P.; Teixeira, P.J.; Gray, C.M.; Mutrie, N. Interventions with potential to reduce sedentary time in adults: Systematic review and meta-analysis. Br. J. Sports Med. 2015, 49, 1056–1063. [Google Scholar] [CrossRef]
- Weiner, L.S.; Takemoto, M.; Godbole, S.; Nelson, S.H.; Natarajan, L.; Sears, D.D.; Hartman, S.J. Breast cancer survivors reduce accelerometer-measured sedentary time in an exercise intervention. J. Cancer Surviv. 2019, 13, 468–476. [Google Scholar] [CrossRef]
- Fine, L.J.; Philogene, G.S.; Gramling, R.; Coups, E.J.; Sinha, S. Prevalence of multiple chronic disease risk factors. 2001 National Health Interview Survey. Am. J. Prev. Med. 2004, 27 (Suppl. 2), 18–24. [Google Scholar] [CrossRef]
- Spring, B.; King, A.C.; Pagoto, S.L.; Van Horn, L.; Fisher, J.D. Fostering multiple healthy lifestyle behaviors for primary prevention of cancer. Am. Psychol. 2015, 70, 75–90. [Google Scholar] [CrossRef] [PubMed]
- Prince, S.A.; Saunders, T.J.; Gresty, K.; Reid, R.D. A comparison of the effectiveness of physical activity and sedentary behaviour interventions in reducing sedentary time in adults: A systematic review and meta-analysis of controlled trials. Obes. Rev. 2014, 15, 905–919. [Google Scholar] [CrossRef] [PubMed]
- Barrett, S.; Begg, S.; O’Halloran, P.; Kingsley, M. A physical activity coaching intervention can improve and maintain physical activity and health-related outcomes in adult ambulatory hospital patients: The Healthy4U-2 randomised controlled trial. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 156. [Google Scholar] [CrossRef]
- Vansteenkiste, M.; Sheldon, K.M. There’s nothing more practical than a good theory: Integrating motivational interviewing and self-determination theory. Br. J. Clin. Psychol. 2006, 45 Pt 1, 63–82. [Google Scholar] [CrossRef]
- Barrett, S.; Begg, S.; O’Halloran, P.; Kingsley, M. Integrated motivational interviewing and cognitive behaviour therapy can increase physical activity and improve health of adult ambulatory care patients in a regional hospital: The Healthy4U randomised controlled trial. BMC Public Health 2018, 18, 1166. [Google Scholar] [CrossRef] [PubMed]
- Tudor-Locke, C.; Camhi, S.M.; Troiano, R.P. A catalog of rules, variables, and definitions applied to accelerometer data in the National Health and Nutrition Examination Survey, 2003–2006. Prev. Chronic Dis. 2012, 9, E113. [Google Scholar] [CrossRef] [PubMed]
- Choi, L.; Liu, Z.; Matthews, C.E.; Buchowski, M.S. Validation of accelerometer wear and nonwear time classification algorithm. Med. Sci. Sports Exerc. 2011, 43, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Freedson, P.S.; Melanson, E.; Sirard, J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med. Sci. Sports Exerc. 1998, 30, 777–781. [Google Scholar] [CrossRef]
- Shao, J.; Zhong, B. Last observation carry-forward and last observation analysis. Stat. Med. 2003, 22, 2429–2441. [Google Scholar] [CrossRef]
- Healy, G.N.; Matthews, C.E.; Dunstan, D.W.; Winkler, E.A.; Owen, N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003-06. Eur. Heart J. 2011, 32, 590–597. [Google Scholar] [CrossRef]
- Buman, M.P.; Winkler, E.A.; Kurka, J.M.; Hekler, E.B.; Baldwin, C.M.; Owen, N.; Ainsworth, B.E.; Healy, G.N.; Gardiner, P.A. Reallocating time to sleep, sedentary behaviors, or active behaviors: Associations with cardiovascular disease risk biomarkers, NHANES 2005-2006. Am. J. Epidemiol. 2014, 179, 323–334. [Google Scholar] [CrossRef] [PubMed]
- Carr, L.J.; Karvinen, K.; Peavler, M.; Smith, R.; Cangelosi, K. Multicomponent intervention to reduce daily sedentary time: A randomised controlled trial. BMJ Open 2013, 3, e003261. [Google Scholar] [CrossRef] [PubMed]
- Peachey, M.M.; Richardson, J.; Tang, A.V.; Dal-Bello Haas, V.; Gravesande, J. Environmental, behavioural and multicomponent interventions to reduce adults’ sitting time: A systematic review and meta-analysis. Br. J. Sports Med. 2020, 54, 315. [Google Scholar] [CrossRef] [PubMed]
- Saunders, T.J.; Larouche, R.; Colley, R.C.; Tremblay, M.S. Acute sedentary behaviour and markers of cardiometabolic risk: A systematic review of intervention studies. Nutr. Metab. 2012, 2012, 712435. [Google Scholar] [CrossRef]
- Prince, S.A.; Cardilli, L.; Reed, J.L.; Saunders, T.J.; Kite, C.; Douillette, K.; Fournier, K.; Buckley, J.P. A comparison of self-reported and device measured sedentary behaviour in adults: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 31. [Google Scholar] [CrossRef]
- Hartman, S.J.; Pekmezi, D.; Dunsiger, S.I.; Marcus, B.H. Physical Activity Intervention Effects on Sedentary Time in Spanish-Speaking Latinas. J. Phys. Act. Health 2020, 17, 343–348. [Google Scholar] [CrossRef]
- Pinto, B.; Dunsiger, S.; Stein, K. Does a peer-led exercise intervention affect sedentary behavior among breast cancer survivors? Psychooncology 2017, 26, 1907–1913. [Google Scholar] [CrossRef]
- Siddique, J.; de Chavez, P.J.; Craft, L.L.; Freedson, P.; Spring, B. The Effect of Changes in Physical Activity on Sedentary Behavior: Results From a Randomized Lifestyle Intervention Trial. Am. J. Health Promot. 2017, 31, 287–295. [Google Scholar] [CrossRef]
- Naar-King, S.; Earnshaw, P.; Breckon, J. Toward a Universal Maintenance Intervention: Integrating Cognitive-Behavioral Treatment With Motivational Interviewing for Maintenance of Behavior Change. J. Cognit. Psychother. 2013, 27, 126–137. [Google Scholar] [CrossRef]
- Kerr, J.; Marinac, C.R.; Ellis, K.; Godbole, S.; Hipp, A.; Glanz, K.; Mitchell, J.; Laden, F.; James, P.; Berrigan, D. Comparison of Accelerometry Methods for Estimating Physical Activity. Med. Sci. Sports Exerc. 2017, 49, 617–624. [Google Scholar] [CrossRef]
- Atkin, A.J.; Gorely, T.; Clemes, S.A.; Yates, T.; Edwardson, C.; Brage, S.; Salmon, J.; Marshall, S.J.; Biddle, S.J. Methods of Measurement in epidemiology: Sedentary Behaviour. Int. J. Epidemiol. 2012, 41, 1460–1471. [Google Scholar] [CrossRef] [PubMed]
- Lyden, K.; Kozey Keadle, S.L.; Staudenmayer, J.W.; Freedson, P.S. Validity of two wearable monitors to estimate breaks from sedentary time. Med. Sci. Sports Exerc. 2012, 44, 2243–2252. [Google Scholar] [CrossRef] [PubMed]
| Variable | Intervention | Control | p-Value |
|---|---|---|---|
| n | 60 | 60 | |
| Age (years) | 54 ± 8 | 53 ± 7 | 0.46 a |
| Sex: female, n (%) | 40 (67%) | 41 (68%) | 0.84 b |
| Stature (cm) | 165 ± 9 | 167 ± 7 | 0.17 a |
| Weight (kg) | 84.5 ± 9.9 | 84.3 ± 9.1 | 0.92 a |
| BMI (kg/m2) | 31.0 ± 4.4 | 30.0 ± 4.2 | 0.19 a |
| MVPA (min/day) | 14.7 ± 5.2 | 14.3 ± 4.7 | 0.67 a |
| Number of sedentary bouts | 66 ± 12 | 67 ± 15 | 0.40 a |
| Daily average of time spent in sedentary bouts (mins) | 551 ± 77 | 555 ± 96 | 0.25 a |
| Average length of sedentary bouts (mins) | 60 ± 14 | 61 ± 16 | 0.71 a |
| Proportion of day in sedentary | 70 ± 7 | 68 ± 6 | 0.09 a |
| Smoker, n (%) | 7 (10%) | 5 (10%) | 0.71 b |
| Obesity, n (%) | 30 (50%) | 32 (53%) | 0.64 b |
| Hypertension, n (%) | 20 (33%) | 18 (30%) | 0.66 b |
| OA/RA, n (%) | 22 (37%) | 20 (33%) | 0.71 b |
| Depression/anxiety, n (%) | 12 (20%) | 13 (22%) | 0.74 b |
| Outcome | Control | Intervention | Analyses | |||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 3 Months | 9 Months | Baseline | 3 Months | 9 Months | Time x Group (F) a | Effect Size b | |
| Total sedentary bouts | 67 ± 15 | 65 ± 13 | 66 ± 18 | 66 ± 12 | 58 ± 17 | 50 ± 20 | 7.13 * | 0.57 |
| Daily average of sedentary bouts (min) | 551 ± 77 | 533 ± 77 | 538 ± 137 | 555 ± 98 | 506 ± 91 | 472 ± 137 | 2.93 | 0.024 |
| Average length of sedentary bouts (min) | 61 ± 16 | 59 ± 15 | 62 ± 32 | 60 ± 14 | 69 ± 31 | 76 ± 40 | 2.31 | 0.019 |
| Proportion of day spent sedentary (%) | 68 ± 6 | 66 ± 7 | 71 ± 8 | 70 ± 7 | 68 ± 6 | 63 ± 8 | 16.98 * | 0.126 |
| MVPA (min/day) [14] | 14 ± 5 | 13 ± 6 | 10 ± 6 | 15 ± 5 | 23 ± 10 | 22 ± 10 | 28.7 * | 0.20 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barrett, S.; Begg, S.; O′Halloran, P.; Kingsley, M. The Effect of a Physical Activity Coaching Intervention on Accelerometer-Measured Sedentary Behaviours in Insufficiently Physically Active Ambulatory Hospital Patients. Int. J. Environ. Res. Public Health 2021, 18, 5543. https://doi.org/10.3390/ijerph18115543
Barrett S, Begg S, O′Halloran P, Kingsley M. The Effect of a Physical Activity Coaching Intervention on Accelerometer-Measured Sedentary Behaviours in Insufficiently Physically Active Ambulatory Hospital Patients. International Journal of Environmental Research and Public Health. 2021; 18(11):5543. https://doi.org/10.3390/ijerph18115543
Chicago/Turabian StyleBarrett, Stephen, Stephen Begg, Paul O′Halloran, and Michael Kingsley. 2021. "The Effect of a Physical Activity Coaching Intervention on Accelerometer-Measured Sedentary Behaviours in Insufficiently Physically Active Ambulatory Hospital Patients" International Journal of Environmental Research and Public Health 18, no. 11: 5543. https://doi.org/10.3390/ijerph18115543
APA StyleBarrett, S., Begg, S., O′Halloran, P., & Kingsley, M. (2021). The Effect of a Physical Activity Coaching Intervention on Accelerometer-Measured Sedentary Behaviours in Insufficiently Physically Active Ambulatory Hospital Patients. International Journal of Environmental Research and Public Health, 18(11), 5543. https://doi.org/10.3390/ijerph18115543







