Analysis of Effectiveness of a Supplement Combining Harpagophytum procumbens, Zingiber officinale and Bixa orellana in Healthy Recreational Runners with Self-Reported Knee Pain: A Pilot, Randomized, Triple-Blind, Placebo-Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
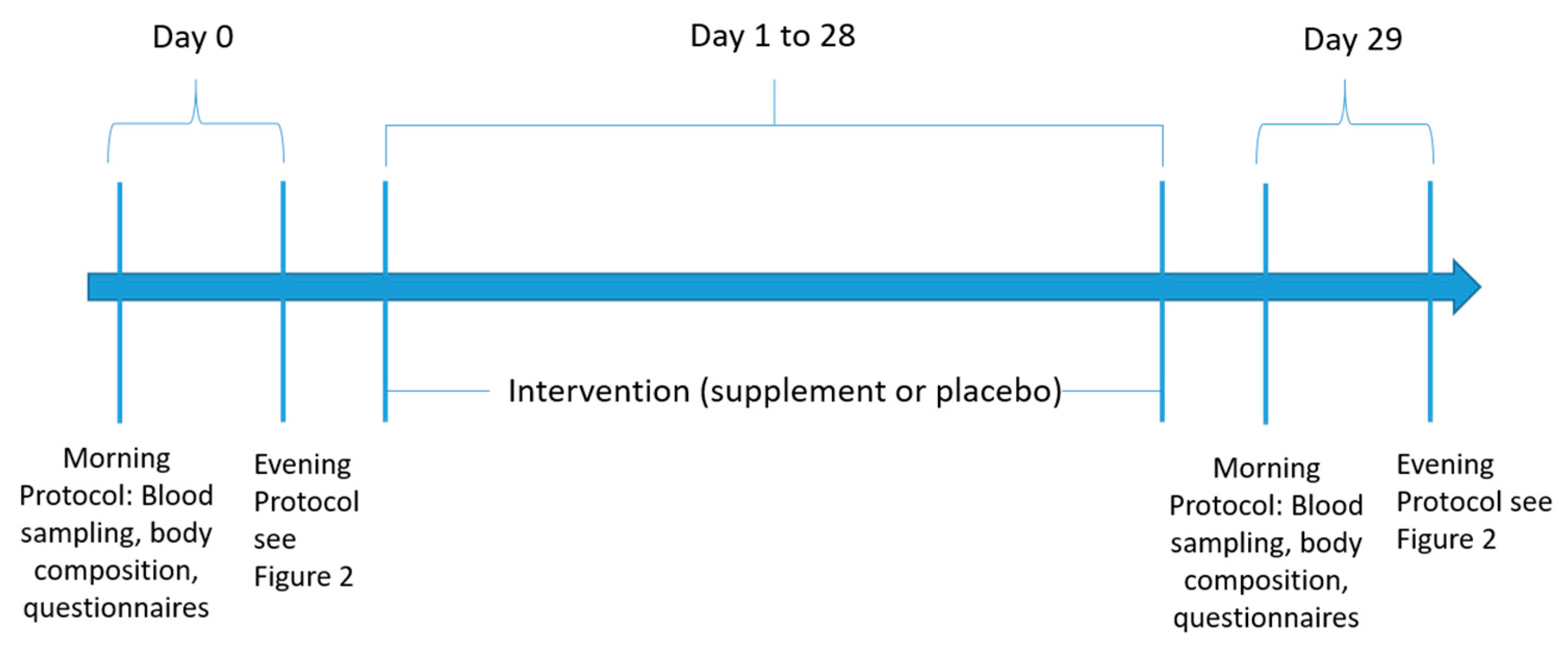
2.2. Study Protocol
2.2.1. Mornings
2.2.2. Evenings
2.3. Socioeconomic Data and Lifestyle Behavior
2.4. Physical Activity
2.5. Dietary Intake
2.6. Anthropometry
2.7. Clinical Chemistry
2.8. Thermography
2.9. Biomechanics
2.10. Ergospirometry
2.11. Composition of the Supplement
2.12. Statistical Analysis
3. Results
3.1. Body Composition
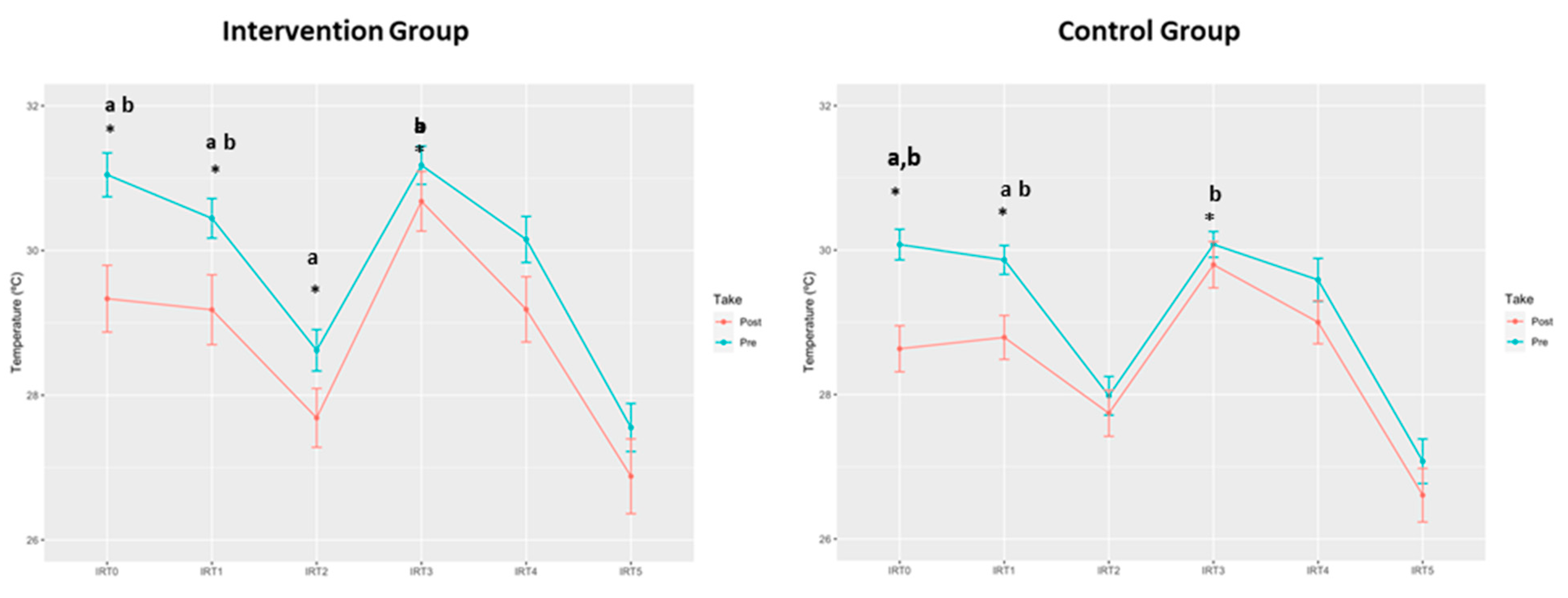
3.2. Thermography
3.3. Biomechanics
3.4. Machine Learning Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chumlea, W.C.; Roche, A.F.; Steinbaugh, M.L. Estimating stature from knee height for persons 60 to 90 years of age. J. Am. Geriatr. Soc. 1985, 33, 116–120. [Google Scholar] [CrossRef]
- Ng, S.W.; Popkin, B.M. Time use and physical activity: A shift away from movement across the globe. Obes. Rev. 2012, 13, 659–680. [Google Scholar] [CrossRef] [PubMed]
- Booth, F.W.; Roberts, C.K.; Thyfault, J.P.; Ruegsegger, G.N.; Toedebusch, R.G. Role of Inactivity in chronic diseases: Evolutionary insight and pathophysiological mechanisms. Physiol. Rev. 2017, 97, 1351–1402. [Google Scholar] [CrossRef] [PubMed]
- Vandelanotte, C.; Short, C.; Rockloff, M.; Di Millia, L.; Ronan, K.; Happell, B.; Duncan, M.J. How do different occupational factors influence total, occupational, and leisure-time physical activity? J. Phys. Act. Health 2015, 12, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451. [Google Scholar] [CrossRef] [PubMed]
- Scheerder, J.; Breedveld, K.; Borgers, J. Running across Europe: The Rise and Size of One of the Largest Sport Markets; Palgrave Macmillan: London, UK, 2015. [Google Scholar]
- Spiers, A.; Harris, S.; Charlton, A.; Smale, P. England. In Running across Europe: The Rise and Size of One of the Largest Sport Markets; Scheerder, J., Breedveld, K., Borgers, J., Eds.; Palgrave Macmillan: London, UK, 2015; pp. 81–104. [Google Scholar]
- Forsberg, P. Denmark. In Running across Europe: The Rise and Size of One of the Largest Sport Markets; Scheerder, J., Breedveld, K., Borgers, J., Eds.; Palgrave Macmillan: London, UK, 2015; pp. 59–80. [Google Scholar]
- Borgers, J.; Vos, S.; Scheerder, J. Belgium (Flanders). In Running across Europe: The Rise and Size of One of the Largest Sport Markets; Scheerder, J., Breedveld, K., Borgers, J., Eds.; Palgrave Macmillan: London, UK, 2015; pp. 28–58. [Google Scholar]
- Ramírez-Vélez, R.; Lobelo, F.; Izquierdo, M. Exercise for disease prevention and management: A precision medicine approach. J. Am. Med. Dir. Assoc. 2017, 18, 633–634. [Google Scholar] [CrossRef]
- Francis, P.; Whatman, C.; Sheerin, K.; Hume, P.; Johnson, M.I. The proportion of lower limb running injuries by gender, anatomical location and specific pathology: A systematic review. J. Sports Sci. Med. 2019, 18, 21–31. [Google Scholar]
- Videbaek, S.; Bueno, A.M.; Nielsen, R.O.; Rasmussen, S. Incidence of running-related injuries per 1000 h of running in different types of runners: A systematic review and meta-analysis. Sports Med. 2015, 45, 1017–1026. [Google Scholar] [CrossRef]
- Taunton, J.E.; Ryan, M.B.; Clement, D.B.; McKenzie, D.C.; Lloyd-Smith, D.R.; Zumbo, B.D. A retrospective case-control analysis of 2002 running injuries. Br. J. Sports Med. 2002, 36, 95–101. [Google Scholar] [CrossRef]
- Calin, M.A.; Mologhianu, G.; Savastru, R.; Calin, M.R.; Brailescu, C.M. A review of the effectiveness of thermal infrared imaging in the diagnosis and monitoring of knee diseases. Infrared Phys. Technol. 2015, 69, 19–25. [Google Scholar] [CrossRef]
- Brenner, J.S. Overuse injuries, overtraining, and burnout in child and adolescent athletes. Pediatrics 2007, 119, 1242–1245. [Google Scholar] [CrossRef] [PubMed]
- Marti, B.; Vader, J.P.; Minder, C.E.; Abelin, T. On the epidemiology of running injuries. The 1984 Bern Grand-Prix study. Am. J. Sports Med. 1988, 16, 285–294. [Google Scholar] [CrossRef]
- Linton, L.; Valentin, S. Running with injury: A study of UK novice and recreational runners and factors associated with running related injury. J. Sci. Med. Sport 2018, 21, 1221–1225. [Google Scholar] [CrossRef]
- Mellinger, S.; Neurohr, G.A. Evidence based treatment options for common knee injuries in runners. Ann. Transl. Med. 2019, 7, S249. [Google Scholar] [CrossRef]
- Kozinc, Z.; Sarabon, N. Effectiveness of Movement Therapy Interventions and Training Modifications for Preventing Running Injuries: A Meta-Analysis of Randomized Controlled Trials. J. Sports Sci. Med. 2017, 16, 421–428. [Google Scholar]
- Sellami, M.; Slimeni, O.; Pokrywka, A.; Kuvacic, G.; Hayes, L.D.; Milic, M.; Padulo, J. Herbal medicine for sports: A review. J. Int. Soc. Sports Nutr. 2018, 15, 14. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; McLachlan, A.; Hunter, D. Vitamin and mineral supplements: The role of supplements and complementary medicines in osteoarthritis: An evidence-based guide to practice. AJP Aust. J. Pharm. 2019, 100, 62. [Google Scholar]
- Mncwangi, N.; Chen, W.; Vermaak, I.; Viljoen, A.M.; Gericke, N. Devil’s Claw—A review of the ethnobotany, phytochemistry and biological activity of Harpagophytum procumbens. J. Ethnopharmacol. 2012, 143, 755–771. [Google Scholar] [CrossRef] [PubMed]
- Chrubasik, J.E.; Roufogalis, B.D.; Chrubasik, S. Evidence of effectiveness of herbal antiinflammatory drugs in the treatment of painful osteoarthritis and chronic low back pain. Phytother. Res. 2007, 21, 675–683. [Google Scholar] [CrossRef]
- Warnock, M.; McBean, D.; Suter, A.; Tan, J.; Whittaker, P. Effectiveness and safety of Devil’s Claw tablets in patients with general rheumatic disorders. Phytother. Res. 2007, 21, 1228–1233. [Google Scholar] [CrossRef]
- Menghini, L.; Recinella, L.; Leone, S.; Chiavaroli, A.; Cicala, C.; Brunetti, L.; Vladimir-Knežević, S.; Orlando, G.; Ferrante, C. Devil′s claw (Harpagophytum procumbens) and chronic inflammatory diseases: A concise overview on preclinical and clinical data. Phytother. Res. 2019, 33, 2152–2162. [Google Scholar] [CrossRef]
- Moré, M.; Gruenwald, J.; Pohl, U.; Uebelhack, R. A Rosa canina-Urtica dioica–Harpagophytum procumbens/zeyheri Combination Significantly Reduces Gonarthritis Symptoms in a Randomized, Placebo-Controlled Double-Blind Study. Planta Med. 2017, 83, 1384–1391. [Google Scholar] [CrossRef]
- Wilson, P.B. Ginger (Zingiber officinale) as an analgesic and ergogenic aid in sport: A systemic review. J. Strength Cond. Res. 2015, 29, 2980–2995. [Google Scholar] [CrossRef]
- Mao, Q.Q.; Xu, X.Y.; Cao, S.Y.; Gan, R.Y.; Corke, H.; Beta, T.; Li, H.B. Bioactive compounds and bioactivities of ginger (Zingiber officinale Roscoe). Foods 2019, 8, 185. [Google Scholar] [CrossRef]
- Zehsaz, F.; Farhangi, N.; Mirheidari, L. The effect of Zingiber officinale R. rhizomes (ginger) on plasma pro-inflammatory cytokine levels in well-trained male endurance runners. Cent. Eur. J. Immunol. 2014, 39, 174–180. [Google Scholar] [CrossRef]
- Ezzat, S.M.; Ezzat, M.I.; Okba, M.M.; Menze, E.T.; Abdel-Naim, A.B. The hidden mechanism beyond ginger (Zingiber officinale Rosc.) potent in vivo and in vitro anti-inflammatory activity. J. Ethnopharmacol. 2018, 214, 113–123. [Google Scholar] [CrossRef] [PubMed]
- Wilson, P.B. A randomized double-blind trial of ginger root for reducing muscle soreness and improving physical performance recovery among experienced recreational distance runners. J. Diet. Suppl. 2020, 17, 121–132. [Google Scholar] [CrossRef] [PubMed]
- Black, C.D.; Herring, M.P.; Hurley, D.J.; O’Connor, P.J. Ginger (Zingiber officinale) reduces muscle pain caused by eccentric exercise. J. Pain 2010, 11, 894–903. [Google Scholar] [CrossRef]
- Bartels, E.M.; Folmer, V.N.; Bliddal, H.; Altman, R.D.; Juhl, C.; Tarp, S.; Zhang, W.; Christensen, R. Efficacy and safety of ginger in osteoarthritis patients: A meta-analysis of randomized placebo-controlled trials. Osteoarthr. Cartil. 2015, 23, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Dominguez-Balmaseda, D.; Diez-Vega, I.; Larrosa, M.; San Juan, A.F.; Issaly, N.; Moreno-Pérez, D.; Burgos, S.; Sillero-Quintana, M.; Gonzalez, C.; Bas, A.; et al. Effect of a blend of zingiber officinale roscoe and bixa orellana l. herbal supplement on the recovery of delayed-onset muscle soreness induced by unaccustomed eccentric resistance training: A randomized, triple-blind, placebo-controlled trial. Front. Physiol. 2020, 11, 826. [Google Scholar] [CrossRef]
- Roehrs, M.; Conte, L.; da Silva, D.T.; Duarte, T.; Maurer, L.H.; de Carvalho, J.A.M.; Moresco, R.N.; Somacal, S.; Emanuelli, T. Annatto carotenoids attenuate oxidative stress and inflammatory response after high-calorie meal in healthy subjects. Food Res. Int. 2017, 100, 771–779. [Google Scholar] [CrossRef] [PubMed]
- Bergmark Brian, A.; Bhatt Deepak, L.; McGuire Darren, K.; Cahn, A.; Mosenzon, O.; Steg Ph, G.; Im, K.; Kanevsky, E.; Gurmu, Y.; Raz, I.; et al. Metformin use and clinical outcomes among patients with diabetes mellitus with or without heart failure or kidney dysfunction. Circulation 2019, 140, 1004–1014. [Google Scholar] [CrossRef]
- López-Rodríguez, C.; Laguna, M.; Gómez-Cabello, A.; Gusi, N.; Espino, L.; Villa, G.; Pedrero-Chamizo, R.; Casajus, J.A.; Ara, I.; Aznar, S. Validation of the self-report EXERNET questionnaire for measuring physical activity and sedentary behavior in elderly. Arch. Gerontol. Geriatr. 2017, 69, 156–161. [Google Scholar] [CrossRef]
- Hagstromer, M.; Oja, P.; Sjostrom, M. The International Physical Activity Questionnaire (IPAQ): A study of concurrent and construct validity. Public Health Nutr. 2006, 9, 755–762. [Google Scholar] [CrossRef]
- Gomez-Candela, L.K.V.C.; Lorenco Nogueira, T. Guía Visual de Alimentos y Raciones; Editores Médicos S.A. (EDIMSA): Madrid, Spain, 2008. [Google Scholar]
- Fernández-Cuecas, I.; Sillero-Quintana, M.; García-Concepción, M.A.; Ribot-Serrano, J.; Gómez-Carmona, P.; Marins, J.B. Monitoring skin thermal response to training with infrared thermography. New Stud. Athl. 2014, 29, 57–71. [Google Scholar]
- Moreira, D.G.; Costello, J.T.; Brito, C.J.; Adamczyk, J.G.; Ammer, K.; Bach, A.J.; Costa, C.M.; Eglin, C.; Fernandes, A.A.; Fernández-Cuevas, I. Thermographic imaging in sports and exercise medicine: A Delphi study and consensus statement on the measurement of human skin temperature. J. Therm. Biol. 2017, 69, 155–162. [Google Scholar] [CrossRef]
- Pochaczevsky, R. Thermography in posttraumatic pain. Am. J. Sports Med. 1987, 15, 243–250. [Google Scholar] [CrossRef]
- Fernández-Cuevas, I.; Bouzas Marins, J.C.; Arnáiz Lastras, J.; Gómez Carmona, P.M.; Piñonosa Cano, S.; García-Concepción, M.Á.; Sillero-Quintana, M. Classification of factors influencing the use of infrared thermography in humans: A review. Infrared Phys. Technol. 2015, 71, 28–55. [Google Scholar] [CrossRef]
- Requena-Bueno, L.; Priego-Quesada, J.I.; Jimenez-Perez, I.; Gil-Calvo, M.; Pérez-Soriano, P. Validation of ThermoHuman automatic thermographic software for assessing foot temperature before and after running. J. Therm. Biol. 2020, 92, 102639. [Google Scholar] [CrossRef] [PubMed]
- Tibshirani, G.J.W.H. An Introduction to Statistical Learning with Applications in R; Springer: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- The Lancet Respiratory, Medicine Opening the black box of machine learning. Lancet Respir. Med. 2018, 6, 801. [CrossRef]
- Kuhn, M. Building Predictive Models in R Using the caret Package. J. Stat. Softw. 2008, 28, 26. [Google Scholar] [CrossRef]
- Bolón-Canedo, V.; Alonso-Betanzos, A. Ensembles for feature selection: A review and future trends. Inf. Fusion 2019, 52, 1–12. [Google Scholar] [CrossRef]
- Bauer, E.; Kohavi, R. An empirical comparison of voting classification algorithms: Bagging, boosting, and variants. Mach. Learn. 1999, 36, 105–139. [Google Scholar] [CrossRef]
- Quinlan, J.R. Induction of decision trees. Mach. Learn. 1986, 1, 81–106. [Google Scholar] [CrossRef]
- Cortes, C.; Kuznetsov, V.; Mohri, M. Ensemble Methods for Structured Prediction. In Proceedings of the 31st International Conference on International Conference on Machine Learning, Beijing, China, 21–26 June 2014; Volume 32, pp. 1134–1142. [Google Scholar]
- Cheng, T.; Wang, Y.; Bryant, S.H.F. Selector: A Ruby gem for feature selection. Bioinformatics 2012, 28, 2851–2852. [Google Scholar] [CrossRef][Green Version]
- Zamora Saiz, A.; Quesada González, C.; Hurtado Gil, L.; Mondéjar Ruiz, D. An Introduction to Data Analysis in R; Springer International Publishing: Cham, Switzerland, 2020; p. 276. [Google Scholar]
- Denoble, A.E.; Hall, N.; Pieper, C.F.; Kraus, V.B. Patellar skin surface temperature by thermography reflects knee osteoarthritis severity. Clin. Med. Insights Arthritis Musculoskelet. Disord. 2010, 3, 69–75. [Google Scholar] [CrossRef]
- Tripathi, S.; Maier, K.G.; Bruch, D.; Kittur, D.S. Effect of 6-gingerol on pro-inflammatory cytokine production and costimulatory molecule expression in murine peritoneal macrophages. J. Surg. Res. 2007, 138, 209–213. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.X.; Zhao, W.H.; Lu, Y.F.; Wang, C.X. Antioxidant and cytotoxic activities of distillates purified by means of molecular distillation from ginger extract obtained with supercritical CO2 fluid. Chem. Biodivers. 2019, 16, e1900357. [Google Scholar] [CrossRef]
- Haseeb, A.; Ansari, M.Y.; Haqqi, T.M. Harpagoside suppresses IL-6 expression in primary human osteoarthritis chondrocytes. J. Orthop. Res. 2017, 35, 311–320. [Google Scholar] [CrossRef]
- Andersen, M.L.; Santos, E.H.; Seabra Mde, L.; da Silva, A.A.; Tufik, S. Evaluation of acute and chronic treatments with Harpagophytum procumbens on Freund’s adjuvant-induced arthritis in rats. J. Ethnopharmacol. 2004, 91, 325–330. [Google Scholar] [CrossRef]
- Inaba, K.; Murata, K.; Naruto, S.; Matsuda, H. Inhibitory effects of devil’s claw (secondary root of Harpagophytum procumbens) extract and harpagoside on cytokine production in mouse macrophages. J. Nat. Med. 2010, 64, 219–222. [Google Scholar] [CrossRef]
- Gold, J.E.; Cherniack, M.; Buchholz, B. Infrared thermography for examination of skin temperature in the dorsal hand of office workers. Eur. J. Appl. Physiol. 2004, 93, 245–251. [Google Scholar] [CrossRef]
- Sharma, S.D.; Smith, E.M.; Hazleman, B.L.; Jenner, J.R. Thermographic changes in keyboard operators with chronic forearm pain. BMJ 1997, 314, 118. [Google Scholar] [CrossRef] [PubMed]
- Law, J.; Chalmers, J.; Morris, D.E.; Robinson, L.; Budge, H.; Symonds, M.E. The use of infrared thermography in the measurement and characterization of brown adipose tissue activation. Temperature 2018, 5, 147–161. [Google Scholar] [CrossRef]
- Vatansever, F.; Hamblin, M.R. Far infrared radiation (FIR): Its biological effects and medical applications. Photonics Lasers Med. 2012, 4, 255–266. [Google Scholar] [CrossRef] [PubMed]
- Ceyssens, L.; Vanelderen, R.; Barton, C.; Malliaras, P.; Dingenen, B. Biomechanical risk factors associated with running-related injuries: A systematic review. Sports Med. 2019, 49, 1095–1115. [Google Scholar] [CrossRef]
- Cuspidi, C.; Sala, C.; Tadic, M.; Grassi, G.; Mancia, G. Systemic hypertension induced by harpagophytum procumbens (devil’s claw): A case report. J. Clin. Hypertens. 2015, 17, 908–910. [Google Scholar] [CrossRef] [PubMed]
- Musco, N.; Vassalotti, G.; Mastellone, V.; Cortese, L.; Della Rocca, G.; Molinari, M.L.; Calabrò, S.; Tudisco, R.; Cutrignelli, M.I.; Lombardi, P. Effects of a nutritional supplement in dogs affected by osteoarthritis. Vet. Med. Sci. 2019, 5, 325–335. [Google Scholar] [CrossRef] [PubMed]
- Stohs, S.J. Safety and efficacy of Bixa orellana (achiote, annatto) leaf extracts. Phytother. Res. 2014, 28, 956–960. [Google Scholar]


| Variables | Exten(d) (n = 13) | p | Control (n = 15) | p | p | p | ||
|---|---|---|---|---|---|---|---|---|
| Day 0 | Day 30 | Intra | Day 0 | Day 30 | Intra | Inter T0 | Inter T1 | |
| Body composition | ||||||||
| Height (cm) | 174.24 ± 1.57 | 174.24 ± 1.57 | ---- | 173.90 ± 1.83 | 173.90 ± 1.83 | ---- | 0.890 | 0.890 |
| Weight (kg) | 76.83 ± 1.73 | 76.83 ± 1.73 | ---- | 76.35 ± 2.46 | 76.35 ± 2.46 | ---- | 0.880 | 0.880 |
| BMI (kg/m2) | 25.35 ± 0.64 | 25.35 ± 0.64 | ---- | 25.15 ± 0.40 | 25.15 ± 0.40 | ---- | 0.800 | 0.800 |
| Fat Mass (%) | 15.57 ± 1.58 | 15.26 ± 1.52 | 0.321 | 15.02 ± 1.56 | 14.99 ± 1.56 | 0.914 | 0.798 | 0.915 |
| Legs Fat Mass (%) | 4.84 ± 0.39 | 4.62 ± 0.33 | 0.036 | 4.15 ± 0.44 | 4.19 ± 0.49 | 0.630 | 0.249 | 0.476 |
| Trunk Fat Mass (%) | 8.80 ± 1.05 | 8.74 ± 1.04 | 0.768 | 8.87 ± 0.99 | 8.86 ± 0.99 | 0.961 | 0.965 | 0.938 |
| Physical performance | ||||||||
| VO2 max (mL/min) | 4330 ± 89.56 | 4323 ± 90.58 | 0.700 | 4067 ± 124.7 | 4075 ± 93.46 | 0.89 | 0.09 | 0.068 |
| Biochemical variables | ||||||||
| Cholesterol (mg/dL) | 203.1 ± 5.88 | 219.6 ± 5.69 | 0.070 | 213.3 ± 12.2 | 219.6 ± 15.09 | 0.182 | 0.475 | 0.999 |
| HDL (mg/dL) | 63.06 ± 2.57 | 60.77 ± 2.67 | 0.110 | 60.90 ± 2.39 | 61.67 ± 2.15 | 0.250 | 0.560 | 0.803 |
| LDL (mg/dL) | 147.64 ± 4.30 | 154.23 ± 4.76 | 0.070 | 161.55 ± 6.74 | 171.71 ± 9.44 | 0.025 | 0.107 | 0.125 |
| VLDL (mg/dL) | 16.24 ± 1.70 | 15.37 ± 1.27 | 0.539 | 19.83 ± 4.64 | 15.33 ± 1.87 | 0.178 | 0.477 | 0.986 |
| Triglycerides (mg/dL) | 81.2 ± 8.52 | 76.85 ± 6.37 | 0.539 | 99.16 ± 23.20 | 76.64 ± 9.32 | 0.178 | 0.477 | 0.986 |
| GPT (IU/L) | 22.31 ± 1.87 | 22.23 ± 1.42 | 0.940 | 19.73 ± 1.49 | 24.53 ± 2.43 | 0.170 | 0.292 | 0.420 |
| GOT (IU/L) | 27.46 ± 2.01 | 26.69 ± 1.49 | 0.427 | 25.87 ± 1.14 | 29.33 ± 1.53 | 0.047 | 0.497 | 0.2278 |
| GGT (IU/L) | 42.62 ± 10.75 | 32.62 ± 6.76 | 0.107 | 22.73 ± 2.30 | 22.67 ± 1.91 | 0.940 | 0.093 | 0.478 |
| Urea (mg/dL) | 41.77 ± 2.45 | 41.61 ± 3.50 | 0.953 | 42.41 ± 1.75 | 40.27 ± 2.46 | 0.475 | 0.832 | 0.758 |
| Uric acid (mg/L) | 5.45 ± 0.26 | 5.33 ± 0.27 | 0.540 | 5.76 ± 0.23 | 5.79 ± 0.21 | 0.868 | 0.386 | 0.201 |
| Albumin (g/dL) | 4.40 ± 0.06 | 4.41 ± 0.08 | 0.908 | 4.41 ± 0.04 | 4.42 ± 0.04 | 0.774 | 0.933 | 0.902 |
| Creatinine (mg/dL) | 1.03 ± 0.02 | 1.01 ± 0.01 | 0.366 | 1.07 ± 0.02 | 1.06 ± 0.02 | 0.136 | 0.287 | 0.167 |
| CK (mU/mL) | 232.2 ± 28.8 | 198.3 ± 27.3 | 0.257 | 194.7 ± 26.4 | 277.1 ± 52.24 | 0.158 | 0.348 | 0.196 |
| Hemoglobin (g/dL) | 14.98 ± 0.24 | 15.20 ± 0.23 | 0.130 | 15.19 ± 0.20 | 15.20 ± 0.17 | 0.920 | 0.530 | 1.000 |
| Hematocrit (%) | 44.92 ± 0.68 | 45.65 ± 0.55 | 0.130 | 44.99 ± 0.46 | 45.17 ± 0.47 | 0.667 | 0.933 | 0.519 |
| Platelet (109/L) | 230.5 ± 15.55 | 232.9 ± 11.83 | 0.650 | 220.9 ± 11.01 | 215.0 ± 9.28 | 0.413 | 0.617 | 0.245 |
| Neutrophils (109/L) | 3.32 ± 0.19 | 3.39 ± 0.24 | 0.746 | 2.98 ± 0.21 | 3.22 ± 0.22 | 0.333 | 0.232 | 0.619 |
| Lymphocytes (109/L) | 1.96 ± 0.07 | 1.96 ± 0.08 | 0.991 | 1.90 ± 0.10 | 1.79 ± 0.10 | 0.253 | 0.651 | 0.234 |
| Monocytes (109/L) | 0.37 ± 0.02 | 0.38 ± 0.02 | 0.593 | 0.35 ± 0.02 | 0.36 ± 0.02 | 0.689 | 0.517 | 0.501 |
| Eosinophils (109/L) | 0.22 ± 0.03 | 0.22 ± 0.03 | 0.820 | 0.24 ± 0.03 | 0.22 ± 0.03 | 0.236 | 0.650 | 0.981 |
| Basophils (109/L) | 0.03 ± 0.002 | 0.04 ± 0.003 | 0.137 | 0.03 ± 0.003 | 0.03 ± 0.002 | 0.363 | 0.230 | 0.159 |
| Variables | Exten(d) (n = 13) | p | Control (n = 15) | p | p | p | ||
|---|---|---|---|---|---|---|---|---|
| Day 0 | Day 30 | Intra | Day 0 | Day 30 | Intra | Inter T0 | Inter T1 | |
| IRT0 | 31.05 ± 0.30 | 29.33 ± 0.46 | 0.008 | 30.08 ± 0.21 | 28.63 ± 0.32 | 0.001 | 0.013 | 0.387 |
| IRT1 | 30.44 ± 0.27 | 29.18 ± 0.48 | 0.042 | 29.86 ± 0.20 | 28.82 ± 0.30 | 0.014 | 0.034 | 0.345 |
| IRT2 | 28.62 ± 0.29 | 27.69 ± 0.40 | 0.043 | 27.98 ± 0.27 | 27.74 ± 0.31 | 0.434 | 0.116 | 0.915 |
| IRT3 | 31.18 ± 0.26 | 30.68 ± 0.41 | 0.247 | 30.08 ± 0.18 | 29.80 ± 0.31 | 0.435 | 0.002 | 0.098 |
| IRT4 | 30.15 ± 0.32 | 29.19 ± 0.45 | 0.144 | 29.59 ± 0.30 | 29.00 ± 0.30 | 0.101 | 0.231 | 0.394 |
| IRT5 | 27.55 ± 0.33 | 26.88± 0.52 | 0.555 | 27.08 ± 0.31 | 26.61 ± 0.37 | 0.468 | 0.240 | 0.394 |
| Biomechanical Variables | Exten(d) (n = 13) | p | Control (n = 15) | p | p | |||
|---|---|---|---|---|---|---|---|---|
| Day 0 | Day 30 | intra | Day 0 | Day 30 | Intra | Inter T0 | Inter T1 | |
| Foot Contact Time (s) | 0.248 ± 0.004 | 0.246 ± 0.003 | 0.584 | 0.239 ± 0.004 | 0.235 ± 0.005 | 0.247 | 0.189 | 0.098 |
| Gait Length (m) | 2.296 ± 0.035 | 2.284 ± 0.042 | 0.555 | 2.244 ± 0.049 | 2.261 ± 0.045 | 0.787 | 0.504 | 0.836 |
| Gait Frequency (Hz) | 1.345 ± 0.017 | 1.376 ± 0.017 | 0.058 | 1.396 ± 0.014 | 1.402 ± 0.019 | 0.683 | 0.028 | 0.328 |
| Hip Flexion at Foot Contact | 40.940 ± 1.153 | 40.251 ± 1.617 | 0.497 | 39.276 ± 1.856 | 38.670 ± 1.403 | 0.660 | 0.470 | 0.465 |
| Max. Hip Extension During Foot Contact (˚) | −0.586 ± 1.123 | −1.643 ± 1.444 | 0.086 | −0.743 ± 1.373 | −1.414 ± 1.204 | 0.248 | 0.932 | 0.903 |
| Max. Hip Adduction During Foot Contact (˚) | 9.393 ± 1.241 | 10.497 ± 1.238 | 0.036 | 8.903 ± 0.703 | 9.232 ± 0.933 | 0.603 | 0.725 | 0.415 |
| Max. Hip Rotation During Foot Contact (˚) | −2.992 ± 2.646 | −1.560 ± 4.251 | 0.670 | −3.237 ± 2.427 | −4.445 ± 1.979 | 0.474 | 0.946 | 0.526 |
| Knee Flexion at Foot Contact | 15.708 ± 1.425 | 15.726 ± 1.802 | 0.991 | 18.989 ± 1.680 | 20.956 ± 2.023 | 0.194 | 0.155 | 0.068 |
| Max. Knee Flexion During Foot Contact (˚) | 46.272 ± 1.131 | 45.461 ± 1.061 | 0.428 | 47.068 ± 1.331 | 48.563 ± 1.687 | 0.263 | 0.658 | 0.145 |
| Max. Knee Flexion During Swing Phase (˚) | 100.964 ± 2.047 | 98.662 ± 3.243 | 0.322 | 101.995 ± 2.092 | 101.812 ± 2.261 | 0.937 | 0.729 | 0.423 |
| Max. Knee Valgus During Foot Contact (˚) | −4.331 ± 0.948 | −5.453 ± 1.152 | 0.164 | −3.835 ± 0.913 | −4.204 ± 1.105 | 0.484 | 0.710 | 0.442 |
| Max. Knee Varus During Foot Contact (˚) | 5.383 ± 1.448 | 5.897 ± 1.741 | 0.898 | 4.543 ± 0.804 | 4.581 ± 0.837 | 0.917 | 0.534 | 0.504 |
| Max. Knee Rotation During Foot Contact (˚) | 3.600 ± 1.965 | 6.639 ± 2.472 | 0.147 | 4.593 ± 2.479 | 5.156 ± 2.501 | 0.572 | 0.761 | 0.679 |
| Foot Flexion at Foot Contact (˚) | 8.418 ± 1.022 | 7.405 ±1.647 | 0.300 | 7.488 ± 1.004 | 8.140 ± 1.352 | 0.593 | 0.523 | 0.730 |
| Max. Foot Extension During Foot Contact (˚) | 5.489 ± 0.838 | 4.759 ± 1.273 | 0.739 | 5.840 ± 0.702 | 6.628 ± 1.277 | 0.885 | 0.765 | 0.504 |
| Foot Supination at Foot Contact (˚) | 10.738 ± 1.477 | 8.473 ± 1.496 | 0.214 | 10.749 ± 1.489 | 10.191 ± 1.795 | 0.775 | 0.996 | 0.477 |
| Max. Foot Pronation During Foot Contact (˚) | −9.089 ± 1.534 | −11.431 ± 2.100 | 0.489 | −6.737 ± 1.544 | −7.371 ± 2.124 | 0.950 | 0.174 | 0.147 |
| Peak Vertical Reaction Force (N/BW) | 2.564 ± 0.049 | 2.514 ± 0.037 | 0.397 | 2.558 ± 0.059 | 2.541 ± 0.054 | 0.885 | 0.800 | 0.945 |
| Min. Antero-Posterior Reaction Force (N/BW) (Braking) | −0.367 ± 0.011 | −0.370 ± 0.017 | 0.858 | −0.360 ± 0.014 | −0.364 ± 0.016 | 0.787 | 0.596 | 0.596 |
| Max. Antero-Posterior Reaction Force (N/BW) (Impulse) | 0.272± 0.005 | 0.266 ± 0.006 | 0.212 | 0.265 ± 0.009 | 0.271 ± 0.011 | 0.464 | 0.499 | 0.688 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González-Gross, M.; Quesada-González, C.; Rueda, J.; Sillero-Quintana, M.; Issaly, N.; Díaz, A.E.; Gesteiro, E.; Escobar-Toledo, D.; Torres-Peralta, R.; Roller, M.; et al. Analysis of Effectiveness of a Supplement Combining Harpagophytum procumbens, Zingiber officinale and Bixa orellana in Healthy Recreational Runners with Self-Reported Knee Pain: A Pilot, Randomized, Triple-Blind, Placebo-Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 5538. https://doi.org/10.3390/ijerph18115538
González-Gross M, Quesada-González C, Rueda J, Sillero-Quintana M, Issaly N, Díaz AE, Gesteiro E, Escobar-Toledo D, Torres-Peralta R, Roller M, et al. Analysis of Effectiveness of a Supplement Combining Harpagophytum procumbens, Zingiber officinale and Bixa orellana in Healthy Recreational Runners with Self-Reported Knee Pain: A Pilot, Randomized, Triple-Blind, Placebo-Controlled Trial. International Journal of Environmental Research and Public Health. 2021; 18(11):5538. https://doi.org/10.3390/ijerph18115538
Chicago/Turabian StyleGonzález-Gross, Marcela, Carlos Quesada-González, Javier Rueda, Manuel Sillero-Quintana, Nicolas Issaly, Angel Enrique Díaz, Eva Gesteiro, David Escobar-Toledo, Rafael Torres-Peralta, Marc Roller, and et al. 2021. "Analysis of Effectiveness of a Supplement Combining Harpagophytum procumbens, Zingiber officinale and Bixa orellana in Healthy Recreational Runners with Self-Reported Knee Pain: A Pilot, Randomized, Triple-Blind, Placebo-Controlled Trial" International Journal of Environmental Research and Public Health 18, no. 11: 5538. https://doi.org/10.3390/ijerph18115538
APA StyleGonzález-Gross, M., Quesada-González, C., Rueda, J., Sillero-Quintana, M., Issaly, N., Díaz, A. E., Gesteiro, E., Escobar-Toledo, D., Torres-Peralta, R., Roller, M., & Guadalupe-Grau, A. (2021). Analysis of Effectiveness of a Supplement Combining Harpagophytum procumbens, Zingiber officinale and Bixa orellana in Healthy Recreational Runners with Self-Reported Knee Pain: A Pilot, Randomized, Triple-Blind, Placebo-Controlled Trial. International Journal of Environmental Research and Public Health, 18(11), 5538. https://doi.org/10.3390/ijerph18115538








