Sleep Health Promotion Interventions and Their Effectiveness: An Umbrella Review
Abstract
1. Introduction
2. Materials and Methods
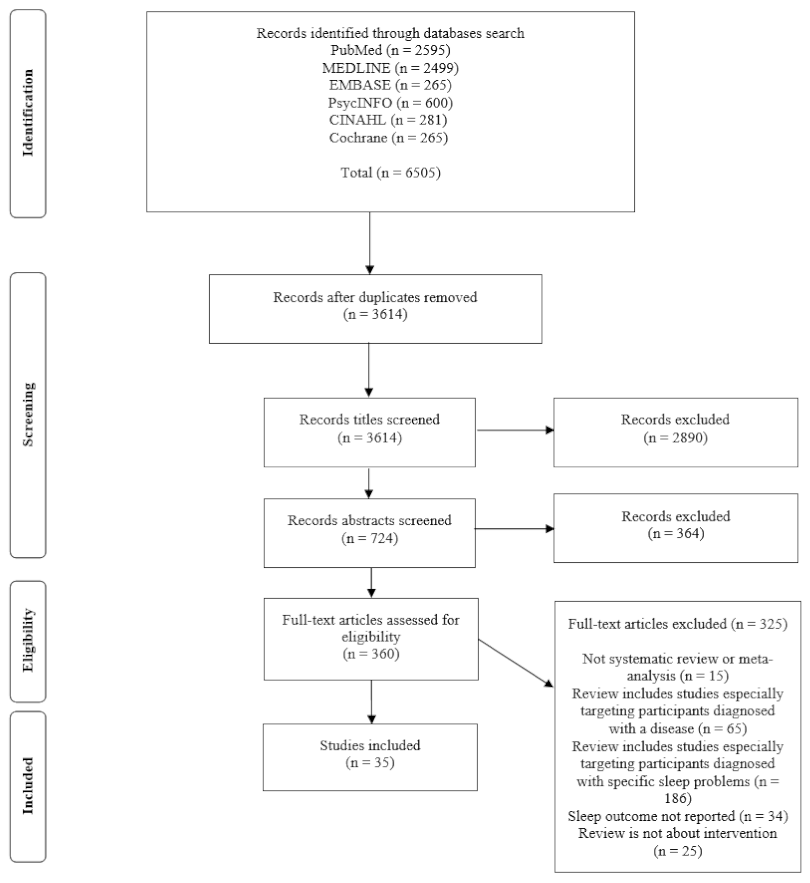
2.1. Search Strategy and Selection Criteria
2.2. Screening and Data Extraction
2.3. Methodological Quality Assessment
3. Results
3.1. Description of Reviews
3.1.1. Included Reviews, Studies, and Quality Assessment
3.1.2. Intervention Types
3.1.3. Target Populations
3.1.4. Intervention Settings
3.1.5. Sleep Measures
3.2. Types of Interventions and Their Effectiveness
3.2.1. Sleep Education
3.2.2. Behavior Change Methods (BCM)
3.2.3. Relaxation Techniques
3.2.4. Physical Exercise Interventions
3.2.5. Mind–Body Exercise (MBE)
3.2.6. Aromatherapy and/or Massage Interventions
3.2.7. Environmental Interventions
3.2.8. Psychotherapy
3.2.9. Later School Start Interventions
3.2.10. Multicomponent Interventions
3.2.11. Other Types of Interventions
4. Discussion
4.1. Strengths and Limitations
4.2. Implications for Practice and Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Buysse, D.J. Sleep health: Can we define it? Does it matter? Sleep 2014, 37, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Cappuccio, F.P.; Taggart, F.M.; Kandala, N.B.; Currie, A.; Peile, E.; Stranges, S.; Miller, M.A. Meta-analysis of short sleep duration and obesity in children and adults. Sleep 2008, 31, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Cappuccio, F.P.; Cooper, D.; D’ Elia, L.; Strazzullo, P.; Miller, M.A. Sleep duration predicts cardiovascular outcomes: A systematic review and meta-analysis of prospective studies. Eur. Heart J. 2011, 32, 1484–1492. [Google Scholar] [CrossRef] [PubMed]
- Cappuccio, F.P.; D’Elia, L.; Strazzullo, P.; Miller, M.A. Quantity and quality of sleep and incidence of type 2 diabetes: A systematic review and meta-analysis. Diabetes Care 2010, 33, 414–420. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Wu, C.; Gan, Y.; Qu, X.; Lu, Z. Insomnia and the risk of depression: A meta-analysis of prospective cohort studies. BMC Psychiatry 2016, 16, 375. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, A.N.; Walker, M.P. The role of sleep in emotional brain function. Annu. Rev. Clin. Psychol. 2014, 10, 679–708. [Google Scholar] [CrossRef]
- Lo, J.; Groeger, J.A.; Cheng, G.H.; Dijk, D.J.; Chee, M. Self-reported sleep duration and cognitive performance in older adults: A systematic review and meta-analysis. Sleep Med. 2016, 17, 87–98. [Google Scholar] [CrossRef]
- Nazari, H.; Moradi, A.; Rahmani, K. A systematic review of the effect of various interventions on reducing fatigue and sleepiness while driving. Chin. J. Traumatol. Zhonghua Chuang Shang Za Zhi 2017, 20, 249–258. [Google Scholar] [CrossRef]
- Ramadan, M.; Al-saleh, K. The association of sleep deprivation on the occurrence of errors by nurses who work the night shift. Curr. Health Sci. J. 2014, 40, 97–103. [Google Scholar] [CrossRef]
- Stranges, S.; Tigbe, W.; Gómez, F.; Thorogood, M.; Kandala, N. Sleep problems: An emerging global epidemic? Findings from the INDEPTH WHO-SAGE study among more than 40,000 older adults from 8 countries across Africa and Asia. Sleep 2012, 35, 1173–1181. [Google Scholar] [CrossRef]
- Grunstein, R.R. Global perspectives on sleep and health issues. J. Natl. Inst. Public Health 2012, 61, 35–42. [Google Scholar]
- Ohayon, M.M. Epidemiological overview of sleep disorders in the general population. Sleep Med. Res. 2011, 2, 1–9. [Google Scholar] [CrossRef]
- Chattu, V.K.; Manzar, M.D.; Kumary, S.; Burman, D.; Spence, D.W.; Pandi-Perumal, S.R. The global problem of insufficient sleep and its serious public health implications. Healthcare 2018, 7, 1. [Google Scholar] [CrossRef]
- Hafner, M.; Stepanek, M.; Taylor, J.; Troxel, W.M.; van Stolk, C. Why sleep matters—The economic costs of insufficient sleep: A cross-country comparative analysis. Rand Health Q. 2017, 6, 11. [Google Scholar]
- Altevogt, B.M.; Colten, H. (Eds.) Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem; National Academies Press: Washington, DC, USA, 2006; pp. 178–180. [Google Scholar] [CrossRef]
- Hale, L.; Troxel, W.; Buysse, D.J. Sleep health: An opportunity for public health to address health equity. Annu. Rev. Public Health 2020, 41, 81–99. [Google Scholar] [CrossRef]
- Luyster, F.S.; Strollo, P.J.; Zee, P.C.; Walsh, J.K. Sleep: A health imperative. Sleep 2012, 35, 727–734. [Google Scholar] [CrossRef]
- 2020 Topics and Objectives—Objectives A–Z|Healthy People 2020. Available online: https://www.healthypeople.gov/2020/topics-objectives/topic/sleep-health/objectives (accessed on 20 November 2020).
- Royal Society for Public Health. Waking up to the Health Benefits of Sleep. Available online: https://www.rsph.org.uk/resourceLibrary/waking-up-to-the-health-benefits-of-sleep.html (accessed on 20 November 2020).
- Sorscher, A.J. How is your sleep: A neglected topic for health care screening. J. Am. Board Fam. Med. JABFM 2008, 21, 141–148. [Google Scholar] [CrossRef]
- Siengsukon, C.F.; Al-dughmi, M.; Stevens, S. Sleep health promotion: Practical information for physical therapists. Phys. Ther. 2017, 97, 826–836. [Google Scholar] [CrossRef]
- Kline, C. Sleep Duration. In Encyclopedia of Behavioral Medicine; Gellman, M.D., Turner, J.R., Eds.; Springer: New York, NY, USA, 2013; pp. 1808–1810. Available online: https://link.springer.com/referenceworkentry/10.1007%2F978-1-4419-1005-9_846 (accessed on 20 November 2020).
- Kline, C. Sleep Quality. In Encyclopedia of Behavioral Medicine; Gellman, M.D., Turner, J.R., Eds.; Springer: New York, NY, USA, 2013; pp. 1811–1813. Available online: https://link.springer.com/referenceworkentry/10.1007%2F978-1-4419-1005-9_849 (accessed on 20 November 2020).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Chiang, I.; Jhangiani, R.; Price, P. Quasi-Experimental Research. In Research Methods in Psychology, 2nd ed.; BCcampus; University of Minnesota Libraries Publishing Edition: Minneapolis, MN, USA, 2015; Volume 135, Available online: https://opentextbc.ca/researchmethods/chapter/quasi-experimental-research (accessed on 20 November 2020).
- Aromataris, E.; Fernandez, R.; Godfrey, C.M.; Holly, C.; Khalil, H.; Tungpunkom, P. Summarizing systematic reviews: Methodological development, conduct and reporting of an umbrella review approach. Int. J. Evid. Based Healthc. 2015, 13, 132–140. [Google Scholar] [CrossRef]
- Cooper, H.; Koenka, A.C. The overview of reviews: Unique challenges and opportunities when research syntheses are the principal elements of new integrative scholarship. Am. Psychol. 2012, 67, 446. [Google Scholar] [CrossRef]
- Pieper, D.; Antoine, S.; Mathes, T.; Neugebauer, E.; Eikermann, M. Systematic review finds overlapping reviews were not mentioned in every other overview. J. Clin. Epidemiol. 2014, 67, 368–375. [Google Scholar] [CrossRef]
- Bryanton, J.; Beck, C.; Montelpare, W. Postnatal parental education for optimizing infant general health and parent-infant relationships. Cochrane Database Syst. Rev. 2013, 28, Cd004068. [Google Scholar] [CrossRef]
- Dietrich, K.; Francis, M.; Knibbs, D.; Umali, L.; Truglio, M. Effectiveness of sleep education programs to improve sleep hygiene and/or sleep quality in college students: A systematic review. JBI Database Syst. Rev. Implement. Rep. 2016, 14, 108–134. [Google Scholar] [CrossRef] [PubMed]
- Neuendorf, R.; Wahbeh, H.; Chamine, I.; Yu, J.; Hutchison, K.; Oken, S. The effects of mind-body interventions on sleep quality: A systematic review. Evid.-Based Complement. Altern. Med. ECAM 2015, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Crichton, G.; Symon, B. Behavioral management of sleep problems in infants under 6 months—What works? J. Dev. Behav. Pediatr. 2016, 37, 164–171. [Google Scholar] [CrossRef]
- Kempler, L.; Sharpe, L.; Miller, C.; Bartlett, D. Do psychosocial sleep interventions improve infant sleep or maternal mood in the postnatal period? A systematic review and meta-analysis of randomised controlled trials. Sleep Med. Rev. 2016, 29, 15–22. [Google Scholar] [CrossRef]
- Mindell, A.; Kuhn, B.; Lewin, S.; Meltzer, L.; Sadeh, A. Behavioral treatment of bedtime problems and night wakings in infants and young children. Sleep 2006, 29, 1263–1276. [Google Scholar] [CrossRef]
- Arora, T.; Taheri, S. Is sleep education an effective tool for sleep improvement and minimizing metabolic disturbance and obesity in adolescents? Sleep Med. Rev. 2017, 36, 3–12. [Google Scholar] [CrossRef]
- Aslund, L.; Arnberg, F.; Kanstrup, M.; Lekander, M. Cognitive and behavioral interventions to improve sleep in school-age children and adolescents: A systematic review and meta-analysis. J. Clin. Sleep Med. 2018, 14, 1937–1947. [Google Scholar] [CrossRef]
- Blunden, S.; Chapman, J.; Rigney, G. Are sleep education programs successful? The case for improved and consistent research efforts. Sleep Med. Rev. 2012, 16, 355–370. [Google Scholar] [CrossRef]
- Busch, V.; Altenburg, M.; Harmsen, A.; Chinapaw, J. Interventions that stimulate healthy sleep in school-aged children: A systematic literature review. Eur. J. Public Health 2017, 27, 53–65. [Google Scholar] [CrossRef]
- Chung, F.; Chan, S.; Lam, Y.; Lai, S.; Yeung, F. School-based sleep education programs for short sleep duration in adolescents: A systematic review and meta-analysis. J. Sch. Health 2017, 87, 401–408. [Google Scholar] [CrossRef]
- Meltzer, J.; Mindell, A. Systematic review and meta-analysis of behavioral interventions for pediatric insomnia. J. Pediatr. Psychol. 2014, 39, 932–948. [Google Scholar] [CrossRef]
- Barger, L.K.; Runyon, M.S.; Renn, M.L.; Moore, C.G.; Weiss, P.M.; Condle, J.P.; Flickinger, K.L.; Divecha, A.A.; Coppler, P.J.; Sequeira, D.J.; et al. Effect of fatigue training on safety, fatigue, and sleep in emergency medical services personnel and other shift workers: A systematic review and meta-analysis. Prehosp. Emerg. Care 2018, 22, 58–68. [Google Scholar] [CrossRef]
- Bonnar, D.; Bartel, K.; Kakoschke, N.; Lang, C. Sleep interventions designed to improve athletic performance and recovery: A systematic review of current approaches. Sports Med. 2018, 48, 683–703. [Google Scholar] [CrossRef]
- Chung, F.; Lee, T.; Yeung, F.; Chan, S.; Chung, Y.; Lin, L. Sleep hygiene education as a treatment of insomnia: A systematic review and meta-analysis. Fam. Pract. 2018, 35, 365–375. [Google Scholar] [CrossRef]
- Friedrich, A.; Schlarb, A. Let’s talk about sleep: A systematic review of psychological interventions to improve sleep in college students. J. Sleep Res. 2018, 27, 4–22. [Google Scholar] [CrossRef]
- Murawski, B.; Wade, L.; Plotnikoff, C.; Lubans, R.; Duncan, J. A systematic review and meta-analysis of cognitive and behavioral interventions to improve sleep health in adults without sleep disorders. Sleep Med. Rev. 2018, 40, 160–169. [Google Scholar] [CrossRef]
- Owais, S.; Chow, T.; Furtado, M.; Frey, N.; Van, J. Non-pharmacological interventions for improving postpartum maternal sleep: A systematic review and meta-analysis. Sleep Med. Rev. 2018, 41, 87–100. [Google Scholar] [CrossRef]
- Halal, E.; Nunes, L. Education in children’s sleep hygiene: Which approaches are effective? A systematic review. J. Pediatr. 2014, 90, 449–456. [Google Scholar] [CrossRef] [PubMed]
- Tamrat, R.; Goyal, M.; Huynh, M. Non-pharmacologic interventions to improve the sleep of hospitalized patients: A systematic review. J. Gen. Intern. Med. 2014, 29, 788–795. [Google Scholar] [CrossRef] [PubMed]
- Slanger, T.E.; Gross, J.V.; Pinger, A.; Morfeld, P.; Bellinger, M.; Duhme, A.L.; Reichardt Ortega, R.A.; Costa, G.; Driscoll, T.R.; Foster, R.G.; et al. Person-directed, non-pharmacological interventions for sleepiness at work and sleep disturbances caused by shift work. Cochrane Database Syst. Rev. 2016, CD010641. [Google Scholar] [CrossRef]
- Hellström, A.; Willman, A. Promoting sleep by nursing interventions in health care settings: A systematic review. Worldviews Evid. Based Nurs. 2011, 8, 128–142. [Google Scholar] [CrossRef] [PubMed]
- Hollenbach, D.; Broker, R.; Herlehy, S.; Stuber, K. Non-pharmacological interventions for sleep quality and insomnia during pregnancy: A systematic review. J. Can. Chiropr. Assoc. 2013, 57, 260–270. [Google Scholar] [PubMed]
- de Niet, G.; Tiemens, B.; Lendemeijer, B.; Hutschemaekers, G. Music-assisted relaxation to improve sleep quality: Meta-analysis. J. Adv. Nurs. 2009, 65, 1356–1364. [Google Scholar] [CrossRef] [PubMed]
- Rubio, Á.; Marín, E.; Ramos, J.; Hernandez, V.; Pérez, R. Effect of exercise on sleep quality and insomnia in middle-aged women: A systematic review and meta-analysis of randomized controlled trials. Maturitas 2017, 100, 49–56. [Google Scholar] [CrossRef]
- Du, S.; Dong, J.; Zhang, H.; Jin, S.; Xu, G.; Liu, Z.; Chen, L.; Yin, H.; Sun, Z. Taichi exercise for self-rated sleep quality in older people: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2015, 52, 368–379. [Google Scholar] [CrossRef]
- Yang, Y.; Ho, H.; Chien, Y.; Chen, C. Exercise training improves sleep quality in middle-aged and older adults with sleep problems: A systematic review. J. Physiother. 2012, 58, 157–163. [Google Scholar] [CrossRef]
- Koch, S.; Haesler, E.; Tiziani, A.; Wilson, J. Effectiveness of sleep management strategies for residents of aged care facilities: Findings of a systematic review. J. Clin. Nurs. 2006, 15, 1267–1275. [Google Scholar] [CrossRef]
- Wu, W.; Kwong, E.; Lan, Y.; Jiang, Y. The effect of a meditative movement intervention on quality of sleep in the elderly: A systematic review and meta-analysis. J. Altern. Complement. Med. 2015, 21, 509–519. [Google Scholar] [CrossRef]
- Hwang, E.; Shin, S. The effects of aromatherapy on sleep improvement: A systematic literature review and meta-analysis. J. Altern. Complement. Med. 2015, 21, 61–68. [Google Scholar] [CrossRef]
- Morgenthaler, I.; Hashmi, S.; Croft, B.; Dort, L.; Heald, L.; Mullington, J. High school start times and the impact on high school students: What we know, and what we hope to learn. J. Clin. Sleep Med. 2016, 12, 1681–1689. [Google Scholar] [CrossRef]
- Minges, E.; Redeker, S. Delayed school start times and adolescent sleep: A systematic review of the experimental evidence. Sleep Med. Rev. 2016, 28, 86–95. [Google Scholar] [CrossRef]
- Marx, R.; Tanner, E.; Davison, C.; Ufholz, L.A.; Freeman, J.; Shankar, R.; Newton, L.; Brown, R.; Parpia, A.; Cozma, I.; et al. Later school start times for supporting the education, health, and well-being of high school students. Cochrane Database Syst. Rev. 2017, 7, CD009467. [Google Scholar] [CrossRef]
- Mihelic, M.; Morawska, A.; Filus, A. Effects of early parenting interventions on parents and infants: A meta-analytic review. J. Child Fam. Stud. 2017, 26, 1507–1526. [Google Scholar] [CrossRef]
- Knowlden, P.; Hackman, L.; Sharma, M. Systematic review of dietary interventions targeting sleep behavior. J. Altern. Complement. Med. 2016, 22, 349–362. [Google Scholar] [CrossRef]
- Louzada, F.M.; Silva, A.G.; Peixoto, C.A.; Menna-Barreto, L. The adolescence sleep phase delay: Causes, consequences and possible interventions. Sleep Sci. 2008, 1, 49–53. [Google Scholar]
- American Academy of Pediatrics. School start times for adolescents. Pediatrics 2014, 134, 642–649. [Google Scholar] [CrossRef]
- Hofmann, S.G.; Asnaani, A.; Vonk, I.J.; Sawyer, A.T.; Fang, A. The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognit. Ther. Res. 2012, 36, 427–440. [Google Scholar] [CrossRef]
- Mitchell, M.D.; Gehrman, P.; Perlis, M.; Umscheid, C.A. Comparative effectiveness of cognitive behavioral therapy for insomnia: A systematic review. BMC Fam. Pract. 2012, 13, 40. [Google Scholar] [CrossRef] [PubMed]
- Barnes, C.M.; Drake, C.L. Prioritizing sleep health: Public health policy recommendations. Perspect. Psychol. Sci. 2015, 10, 733–737. [Google Scholar] [CrossRef] [PubMed]
- Lubas, M.; Szklo, M. A critical review of education-based sleep interventions for undergraduate students: Informing future directions in intervention development. Adolesc. Res. Rev. 2019, 4, 249–266. [Google Scholar] [CrossRef]
- Gruber, R. School-based sleep education programs: A knowledge-to-action perspective regarding barriers, proposed solutions, and future directions. Sleep Med. Rev. 2017, 36, 13–28. [Google Scholar] [CrossRef]
- Belmon, L.S.; Stralen, M.M.; Busch, V.; Harmsen, I.A.; Chinapaw, M.J. What are the determinants of children’s sleep behavior? A systematic review of longitudinal studies. Sleep Med. Rev. 2019, 43, 60–70. [Google Scholar] [CrossRef]
- Johnson, D.A.; Billings, M.E.; Hale, L. Environmental determinants of insufficient sleep and sleep disorders: Implications for population health. Curr. Epidemiol. Rep. 2018, 5, 61–69. [Google Scholar] [CrossRef]
| Intervention Type | Definition and Description | No. of Reviews [References] | Populations Targeted |
|---|---|---|---|
| Sleep Education | Delivering information about sleep in general and/or sleep hygiene tips in an instructional manner (for example in presentations, workshops, online modules, print media). | 17 Reviews [29,30,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46] | Infants, children, adolescents, college students, shift workers, athletes, adults |
| Behavior Change Methods (BCM) | Behavior change methods are based on learning theory, such as stimulus control, sleep schedules and structured routines; often managed by outside helpers such as parents, nurses, etc. | 11 Reviews [29,32,33,34,38,40,42,45,47,48,49] | Elderly (in care facilities), infants, children, adolescents, hospitalized adults, adults, athletes, shift workers |
| Relaxation Techniques | Relaxation techniques such as mindfulness, breathing methods, meditation, guided imagery, progressive muscle relaxation, music, etc. | 9 Reviews [31,35,41,44,45,48,50,51,52] | Adolescents, shift workers, college students, pregnant women, adults, hospitalized adults |
| Physical Exercise | Exercise, including Pilates, and other conditioning, or aerobic exercise; usually facilitated in group settings | 7 Reviews [45,46,51,53,54,55,56] | Older adults (+60), postmenopausal women, pregnant women, postpartum women, middle-aged women, elderly (in care facilities) |
| Mind–Body Exercise (MBE) | Physical exercises with meditative components, including tai chi, yoga, Qigong, and the Rességuier Method | 6 Reviews [31,51,53,54,55,57] | Older adults (+60), pregnant women, middle-aged women, adults, elderly |
| Aromatherapy and/or Massage | Aromatherapy is the therapeutic use of essential oils through inhalation or application on skin through massage; massage is the therapeutic manipulation of soft body tissues through kneading or rubbing; often massage and aromatherapy are implemented in combination | 6 Reviews [46,48,50,51,56,58] | Hospitalized adults, pregnant women, adults, postpartum women, elderly (in care facilities) |
| Environmental | Changes to the physical environment including light therapy, noise reduction, or addressing any other sleep interruptions | 5 Reviews [46,48,49,50,56] | Elderly (in care facilities), hospitalized adults, postpartum women, shift workers |
| Psychotherapy | Psychotherapy interventions administered online, in groups or individually, such as cognitive behavior therapy (CBT) and other psychotherapy including implosive therapy, cognitive refocusing treatment for insomnia, constructive worry, etc. | 4 Reviews [40,41,44,46] | College students, shift workers, children, adolescents, postpartum women |
| Later School Start Times | Schools delaying start time by 20–85 min | 4 Reviews [38,59,60,61] | Adolescents, children |
| Multicomponent | Combinations of two or more intervention types described above | 18 Reviews [29,31,32,33,34,36,37,38,40,41,44,45,48,49,50,51,56,62] | Infants, children, adolescents, adults, college students, elderly (in care facilities), hospitalized patients, shift workers |
| Other | Other kinds of interventions, like dietary, hypnosis, biofeedback therapy, magnet therapy, drinking herbal tea, acupuncture, cryostimulation, and infrared light treatment | 7 Reviews [31,42,44,46,50,51,63] | Elderly (in care facilities), postpartum women, adults, pregnant women, college students, hospitalized patients, athletes |
| Infants and Young Children | ||||||
|---|---|---|---|---|---|---|
| Reference | Types and Descriptions of Interventions | Type of Review (No. of Eligible Studies Included in the Umbrella Review a/Total No. of Studies in the Review) | Study Design | Population (Age Range) | Intervention Settings | Conclusions on Effectiveness |
| Bryanton et al. (2013) [29] |
| Systematic review and meta-analysis (4/27) | RCTs | Infants and their parent | Varied: home, hospital, clinic setting |
|
| Crichton and Symon (2016) [32] |
| Systematic review (11/11) | RCTs, Quasi- experimental | Parents of infants (<6 months) | Varied: home, clinic, or hospital |
|
| Kempler et al. (2015) [33] |
| Systematic review and meta-analysis (9/9) | RCTs | Infants (<12 months) | Varied; clinic, home |
|
| Mihelic et al. (2017) [62] |
| Systematic Review and Meta-analysis (13/36) | RCTs | Parents with infants (<12 months) or pregnant parents | Varied: home and hospital |
|
| Mindell et al. (2006) [34] |
| Systematic review (52/52) | RCTs, Quasi- experimental | Infants and children (<5 years) | Varied: home, clinic. |
|
| School-Aged Children and Adolescents | ||||||
| Arora and Taheri (2017) [35] |
| Systematic review (12/12) | NR | Adolescents (10–18 years) | Varied: school, research clinics |
|
| Aslund et al. (2018) [36] |
| Systematic review and meta-analysis (6/6) | RCTs | Children and adolescents (6–20 years) | Varied: school, group therapy setting, internet, individual sessions |
|
| Blunden et al. (2012) [37] |
| Systematic review (12/12) | RCTs, Quasi- experimental | Children and adolescents (<20 years) | School |
|
| Busch et al. (2017) [38] |
| Systematic review (11/11) | RCT, Quasi- experimental | Children (4–12 years) | Varied: School, home, parent workplace, community settings |
|
| Chung et al. (2017) [39] |
| Systematic review and meta-analysis (7/7) | RCTs | Adolescents (10–19 years) | School |
|
| Halal and Nunes (2014) [47] |
| Systematic review (10/10) | NR | Children (<10 years) | Home/community |
|
| Marx et al. (2017) [61] |
| Systematic review and meta-analysis (8/11) | RCTs, crossover, Quasi- experimental | Secondary, middle, or high school- aged children (13–19 years) | School |
|
| Meltzer et al. (2014) [40] |
| Systematic review and meta-analysis (28/28) | RCTs, Quasi- experimental | Children (<18 years) | Varied: clinic, hospital, home |
|
| Minges and Redeker (2016) [60] |
| Systematic review (6/6) | RCTs, Quasi experimental | Primary or secondary school-aged children (9–18 years) | School |
|
| Morgenthaler et al. (2016) [59] |
| Systematic review and meta-analysis (18/18) | Quasi- experimental | High school-aged children (12–19 years) | School |
|
| Adults | ||||||
| Barger et al. (2018) [41] |
| Systematic review and meta-analysis (16/18) | RCTs, Quasi- experimental | Shift workers (>18 years) | Varied: home, work-based |
|
| Bonnar et al. (2018) [42] |
| Systematic review (10/10) | Quasi- experimental, crossover | Athletes (>18 years) | Unclear |
|
| Chung et al. (2017) [43] |
| Systematic review and meta-analysis (15/15) | RCTs | Adults (NR) | Varied: Clinic or other healthcare setting |
|
| Dietrich et al. (2016) [30] |
| Systematic review (4/4) | RCTs, Quasi- experimental | College students (>18 years) | University |
|
| Friedrich and Schlarb (2017) [44] |
| Systematic review (27/27) | RCTs, quasi- experimental | College students (>18 years) | University |
|
| Hellström et al. (2011) [50] |
| Systematic review (9/9) | RCTs | Adults (>19 years) | Healthcare setting (inpatient) |
|
| Hollenbach et al. (2013) [51] |
| Systematic review (7/7) | RCTs, quasi- experimental | Pregnant women (15–45 years) | Varied; inpatient, and community |
|
| Hwang and Shin (2015) [58] |
| Systematic review and meta-analysis (13/13) | RCTs, quasi- experimental | Adults (NR) | Varied; inpatient, home |
|
| Knowlden et al. (2016) [63] |
| Systematic review (4/21) | RCTs, Crossover | Adults (18–50 years) | Home |
|
| Murawski et al. (2018) [45] |
| Systematic review and meta-analysis (11/11) | RCTs, Quasi- experimental | Adults (18–64 years) | Varied: home, in-group, online |
|
| Neuendorf et al. (2015) [31] |
| Systematic review (112/112) | RCTs | Adults (>18 years) | Varied: home, hospital |
|
| Owais et al. (2018) [46] |
| Systematic review and meta-analysis (15/15) | RCTs, Quasi- experimental | Mothers between delivery and 12 months postpartum | Varied: home, clinic, and hospital |
|
| Rubio et al. (2017) [53] |
| Systematic review and meta-analysis (5/5) | RCTs | Middle-aged women (48–56 years) | Community |
|
| Slanger et al. (2016) [49] |
| Systematic review (12/17) | RCTs, Crossover | Shift workers | Workplace |
|
| Tamrat et al. (2013) [48] |
| Systematic review (13/13) | RCTs, Quasi- experimental | Inpatient adults (NR) | Inpatient setting (hospital) |
|
| Elderly | ||||||
| Du et al. (2015) [54] |
| Systematic review and meta-analysis (5/5) | RCTs | Older participants (>60 years) | Community settings |
|
| Koch et al. (2006) [56] |
| Systematic review (41/41) | RCTs, quasi- experimental | Elderly (>65) years | Aged care facilities |
|
| Wu et al. (2015) [57] |
| Systematic review and meta-analysis (14/14) | RCTs | Elderly (>60 years) with complaints of poor sleep | Varied: senior centers/elderly homes, community center |
|
| Yang et al. (2012) [55] |
| Systematic review (6/6) | RCTs | Older adults (>40 years) | Community |
|
| Adults, Including the Elderly | ||||||
| De Niet et al. (2009) [52] |
| Meta-analysis (5/5) | RCTs | Adults (>18 years) and elderly (>60 years) | Home or hospital setting, college |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Albakri, U.; Drotos, E.; Meertens, R. Sleep Health Promotion Interventions and Their Effectiveness: An Umbrella Review. Int. J. Environ. Res. Public Health 2021, 18, 5533. https://doi.org/10.3390/ijerph18115533
Albakri U, Drotos E, Meertens R. Sleep Health Promotion Interventions and Their Effectiveness: An Umbrella Review. International Journal of Environmental Research and Public Health. 2021; 18(11):5533. https://doi.org/10.3390/ijerph18115533
Chicago/Turabian StyleAlbakri, Uthman, Elizabeth Drotos, and Ree Meertens. 2021. "Sleep Health Promotion Interventions and Their Effectiveness: An Umbrella Review" International Journal of Environmental Research and Public Health 18, no. 11: 5533. https://doi.org/10.3390/ijerph18115533
APA StyleAlbakri, U., Drotos, E., & Meertens, R. (2021). Sleep Health Promotion Interventions and Their Effectiveness: An Umbrella Review. International Journal of Environmental Research and Public Health, 18(11), 5533. https://doi.org/10.3390/ijerph18115533







