Abstract
Background: As the U.S. Food and Drug Administration considers a low nicotine product standard for cigarettes, it is important to examine how people who smoke, especially individuals from priority populations disproportionately affected by smoking, perceive low nicotine content (LNC) cigarettes and their relative risk perceptions of alternative nicotine delivery system (ANDS) products, including e-cigarettes and snus, and medicinal nicotine. Methods: Data are from Wave 4 (2016–2017) of the adult Population Assessment of Tobacco Use and Health (PATH) Study. We examined respondents’ absolute risk perceptions about nicotine, LNC cigarettes, ANDS products and medicinal nicotine; their relative risk perceptions of LNC cigarettes and ANDS products compared to conventional cigarettes; and their relative risk perceptions of medicinal nicotine compared to ANDS products. Results: The majority of respondents across priority smoking populations indicated snus, e-cigarettes, and LNC cigarettes were ‘about the same’ level of harmfulness or addictiveness as conventional cigarettes. The majority of respondents indicated e-cigarettes to be ‘about the same’ harmfulness as medicinal nicotine. Conclusions: Our study indicates that adults who smoke cigarettes generally have misperceptions about the harms of nicotine and the relative risks of ANDS products and such misperceptions exist regardless of their racial/ethnic identity, sexual orientation, and gender identity.
Keywords:
nicotine; low nicotine cigarettes; e-cigarettes; snus; risk perceptions; race; ethnicity; LGBTQ+ 1. Introduction
In 2017, the Food and Drug Administration (FDA) proposed a new regulatory approach for reducing the public health burden of commercial tobacco use in the United States (US) [1]. The nicotine-focused framework developed by FDA regulators relies on the concept that a continuum of harm exists for nicotine and tobacco products—with products such as nicotine replacement therapy representing the least harmful products on this continuum and combusted cigarettes representing the most harmful—and that moving people away from using the most harmful products is essential for improving public health outcomes [2,3]. This framework is founded in the evidence that nicotine, while responsible for the highly addictive nature of commercial tobacco products, is not directly responsible for most tobacco-related disease—rather, it is the other chemicals present in tobacco or tobacco smoke [4]. Cigarettes are the most commonly used commercial tobacco product in the U.S. and pose the greatest threat to consumer health due to the exposure to harmful toxicants via combusted tobacco smoke [5,6,7]. E-cigarettes and snus, two types of alternative nicotine delivery system (ANDS) products, are likely to be less harmful relative to cigarettes because they are not combusted, although the effects of long-term use for some products (e.g., e-cigarettes) are unknown. Finally, medicinal nicotine products, such as nicotine gum and patches, are longstanding FDA-approved pharmacotherapies for smoking cessation with minimal safety concerns for short- or long-term use [8,9]; however, uptake of these products is relatively low with only about 30% of people using medicinal nicotine during cessation attempts [8].
As part of this new continuum of harm framework, the FDA proposed implementing a low nicotine product standard for all commercially available cigarettes, which would require cigarettes to have nicotine levels that are minimally or non-addictive [1]. Since nicotine is the primary reinforcing constituent in cigarettes that contributes to establishing and maintaining smoking behavior, drastically reducing the allowable nicotine content could prevent adolescents from becoming dependent on cigarettes and help people who currently smoke cigarettes to quit or cut down [10,11]. Indeed, results from clinical trials consistently report reductions in smoking behavior, toxicant exposure, and nicotine dependence among adult smokers who switched to low nicotine content (LNC) cigarettes [12,13,14,15,16,17,18,19]. Such trials also report minimal evidence of the following potential unintended consequences: compensatory smoking behavior due to decreased nicotine levels, exacerbation of psychiatric symptoms, or increases in alcohol or cannabis use among adults smoking LNC cigarettes [12,16,17,20,21,22,23,24,25,26]. In a simulation study, population estimates indicate that as many as 5 million people will quit smoking within the first year of a low nicotine product standard [27]. However, the public health benefits of a nicotine reduction policy depend on a second component of the nicotine-focused framework: making alternative nicotine products available for people who are unwilling or unable to stop using nicotine. This can be achieved both by supporting innovations in and access to medicinal nicotine as well as via thoughtful regulation of the commercial marketplace of non-medicinal ANDS products [1]. Together, this two-pronged public health approach could result in upwards of 55 million life-years gained over the next 50 years [27].
One important consideration for implementing the proposed framework is determining whether the public understands the continuum of harm for commercial nicotine and tobacco products. In general, the relatively minor role of nicotine’s contribution to disease development is not well understood by the public [28]. For example, research on medicinal nicotine highlights the confusion surrounding the harms of nicotine. In prior studies, people frequently reported nicotine gum or patches to be as harmful as smoking cigarettes [29,30]. More recently, a nationally representative survey found that nearly half of respondents incorrectly reported that nicotine causes cancer [31]. Within the context of a low nicotine product standard for cigarettes, this nicotine misperception is problematic because people could misconstrue “reduced nicotine” to mean “reduced harm”. Indeed, Byron et al. reported that nearly half of participants believed LNC cigarettes were less carcinogenic, and this misperception was associated with decreased intentions to quit smoking when asked to predict their behavior if the government mandated that tobacco companies reduce the nicotine in cigarettes [32]. LNC cigarettes are beneficial over conventional cigarettes to the extent that they may promote or facilitate smoking cessation or reductions; however, continued smoking with LNC cigarettes at similar levels as conventional cigarettes would not likely afford users substantial health benefits. Thus, misperceptions about the risks of smoking LNC cigarettes, if they lead to persistence of smoking, could reduce the public health impact of a low nicotine product standard.
As previously stated, e-cigarettes and snus are likely to be less harmful relative to smoking cigarettes, but consumers may not understand the risks of using these products relative to cigarettes or other combusted tobacco products. With regard to e-cigarettes, the risk perceptions literature reports mixed findings. Early research indicated that many groups (e.g., adults, adolescents, people who smoke) perceived e-cigarettes to be less harmful to health relative to cigarettes, which is likely accurate within the context of the tobacco continuum of harm [2,33,34]. However, over time, risk perceptions have shifted towards e-cigarettes being perceived as harmful products [33,34]. For example, Huang et al. found that nearly 65% of respondents in 2017 perceived e-cigarettes to be equally or more harmful than cigarettes, and that this misperception significantly increased over a five-year period [35]. Other studies report substantial misperceptions concerning snus, with people incorrectly believing that using snus is equally or more harmful than smoking cigarettes [36,37,38]. However, the epidemiological data from Sweden indicate the people who use snus have substantially lower risks of developing tobacco-related diseases compared to people who smoke cigarettes [39]. If people who are unable to stop using nicotine believe ANDS products, such as e-cigarettes and snus, are equally or more harmful than cigarettes, then they may not make the switch, thereby reducing the public health impact of the nicotine-focused framework. Importantly, consumer beliefs, such as product risk perceptions, are central tenets of several health behavior theories [40,41], which state that people’s beliefs influence their behaviors. Therefore, targeting risk perceptions to change behavior is a key target in tobacco control research [42,43]. Within the tobacco control literature, there is evidence demonstrating that targeting risk perceptions about tobacco products can change use behaviors, such as reducing initiation and increasing quit attempts [44,45,46]. Therefore, examining risk perceptions of nicotine, LNCs and ANDS products, including e-cigarettes and snus, are critical for understanding how a nicotine-focus framework may affect smoking behavior.
Although the overall smoking prevalence continues to decline in the U.S., cigarette smoking is now more heavily concentrated among underserved and priority populations including racial and ethnic minoritized groups and people identifying as lesbian, gay, bisexual, transgender, queer, and other sexual or gender identities (LGBTQ+) [7]. Factors contributing to the increased smoking prevalence among these groups include systematic racism and/or discrimination, [47,48,49] as well as targeted marketing and advertising campaigns by the tobacco industry [50,51,52,53,54]. Understanding how racial and ethnic minoritized groups and LGBTQ+ people perceive LNC cigarettes and ANDS is important for assessing how the nicotine-focused framework may benefit all populations, including whether the proposed framework may exacerbate existing smoking-related health disparities. Although a few prior LNC and/or ANDS risk perception studies have reported outcomes for people identifying as Black or African American [31,32,55], to our knowledge, this topic has been understudied among people identifying as American Indian or Alaskan Native, Asian, Hispanic, Native Hawaiian or Pacific Islander or more than one race. Further, data concerning risk perceptions among LGBTQ+ populations are also limited: one prior study examining risk perceptions among LGBTQ+ populations was restricted to young adults [55], while another included older people identifying as LGB but did not explicitly examine perceptions among people identifying as transgender [56]. As a result, there are notable gaps in the risk perception literature concerning subgroups within the LGBTQ+ population, with a particular dearth of estimates from nationally representative data sources. Therefore, the primary aims of the current study are (1) to describe the overall trends in risk perceptions of nicotine in general, low nicotine content cigarettes, and two ANDS products (e-cigarettes and snus) using a U.S. representative sample; and (2) to examine the findings among minoritized groups to determine if there are differences in risk perceptions.
2. Materials and Methods
2.1. Data Source
Data are from Wave 4 (2016–2017) of the adult Population Assessment of Tobacco Use and Health (PATH) Study Restricted-Use Files. Briefly, PATH is a U.S. representative cohort study of tobacco and nicotine use that started data collection during 2013–2014 (Wave 1). For Wave 1, PATH used a stratified address-based, area-probability sampling design that oversampled tobacco users and African American adults. Survey weights were created that adjusted for the study design and account for nonresponse and over-and under-coverage of certain population groups. The probability sample and weights allow for estimates that are representative of the non-institutionalized, civilian U.S. population. For data collection, field interviewers visited respondents’ homes to conduct interviews using audio computer-assisted self-interviews. At the time of data analysis for the present study, Wave 4 was the most recent wave with public-use data available for analysis. Unique to Wave 4 is a replenishment sample that was combined with the Wave 4 respondents who were from the Wave 1 Cohort to account for loss to follow-up among prior waves. This combined set of Wave 4 participants forms the Wave 4 data and included 33,822 adult respondents. Further details on the PATH methodology can be found elsewhere [57,58]. This study was submitted for review to the University of Minnesota Institutional Review Board but the board determined the study did not constitute human subjects research because of the de-identified nature of the secondary data analysis.
2.2. Measures
Perceptions of harm of cigarettes, non-combustible tobacco products, and nicotine: The following question was asked separately for each product/product characteristics shown in the brackets: “How harmful do you think [cigarettes/e-cigarettes or other electronic nicotine products/snus/nicotine in nicotine replacement products/nicotine/nicotine in cigarettes/nicotine in e-cigarettes or other electronic nicotine products] is/are to health”. Response options were: “Not at all harmful”, “Slightly harmful”, “Somewhat harmful”, “Very Harmful”, and “Extremely Harmful”.
Perceptions of low nicotine cigarettes and non-combustible tobacco products relative to regular cigarettes: Additionally, we examined the following questions: “In your opinion, do you think cigarettes with lower amounts of nicotine are less harmful, about the same, or more harmful to a person’s health than regular cigarettes?”, “In your opinion, do you think that cigarettes with lower amounts of nicotine are less addictive, about the same, or more addictive than regular cigarettes?”, “Is using [e-cigarettes or other electronic nicotine products/snus] less harmful, about the same, or more harmful than smoking cigarettes?”
Perceptions of e-cigarettes relative to nicotine replacement therapy: Only e-cigarettes were asked about in relation to nicotine replacement therapy with the following question: “Do you think using e-cigarettes or other electronic nicotine products is less harmful, about the same, or more harmful than using nicotine patch, gum, or lozenge?”
Perceptions of nicotine: We examined the following two questions on nicotine perceptions “Do you believe nicotine is the main substance in tobacco that makes people want to use tobacco products?”, “Do you believe nicotine is the chemical that causes most of the cancer caused by smoking cigarettes?”. Response options were: “Definitely yes”, “Probably yes”, “Probably not”, “Definitely not”. For all questions, respondents were able to report “I don’t know”.
Race and Ethnicity: To assess the social constructs of race and ethnicity, respondents were asked the following questions: “What is your race?” and “Are you Hispanic, [Latino| Latina], or of Spanish origin?”. For the current study, we classified respondents into six groups, although we recognize that important heterogeneity exists within the groups: (1) American Indian/Alaskan Native (non-Hispanic/Latino/Latina/Spanish origin (HLLS)); (2) Black/African American (non-HLLS); (3) Asian (non-HLLS) which includes Asian Indian, Chinese, Filipino, Japanese, Korean, Vietnamese and Other Asian; (4) Hispanic/Latino/Latina/Spanish origin; (5) Native Hawaiian/Guamanian/Chamorro/Samoan/Other Pacific Islander and those identifying with ‘more than one race’ (non-HLLS); and (6) white (non-HLLS).
Of note, respondents who identified as Hispanic/ Latino/Latina/Spanish origin were classified into the Hispanic/Latino/Latina/Spanish origin group, regardless of their racial identity. Respondents who identified as American Indian/Alaskan Native in combination with any other race(s) were classified into the American Indian/Alaskan Native group in order to increase the sample size. Prior studies using PATH data have applied a similar classification approach [59,60,61,62]. Finally, due to the small sample sizes for those identifying as Native Hawaiian/Guamanian/Chamorro/Samoan/Other Pacific Islander or ‘more than one race’ (with the exception of American Indian/Alaskan Native), we combined these respondents into one group to increase power.
Sexual Orientation and Gender Identity: To assess sexual orientation, respondents were asked the following question: “Do you consider yourself to be straight, lesbian or gay, bisexual, or something else?” To assess gender identity, respondents were asked: “Do you consider yourself to be transgender?” Response options were “Yes” or “No”. Since the question did not explicitly ask if respondents identified as cisgender, gender non-conforming, non-binary, etc., we opted to define those who answered “No” as “nontransgender” rather than make assumptions about their gender identities.
2.3. Analytical Sample
Given the interest in how people who currently smoke perceive low nicotine content cigarettes, ANDS products, and nicotine, data for the present analyses were restricted to people reporting current and established use of cigarettes, which is defined in PATH by the following criteria: respondents who have smoked at least 100 cigarettes in their lifetime, and currently smoke every day or some days. We further restricted the sample to respondents who did not report established use of non-combustible tobacco products (i.e., e-cigarettes or snus) which was defined in PATH by the following criteria: respondents who have ever used (electronic nicotine products/snus), have ever used them fairly regularly, and currently use every day or some days. Experimental users of non-combustible tobacco products were therefore included, which is defined in PATH by the following criteria: respondents who have never used (electronic nicotine products/snus) fairly regularly, and currently use every day or some days.
2.4. Statistical Analyses
All response options to perception measures, including “I don’t know”, were examined among the overall sample (i.e., not by race/ethnicity, sexual orientation, or transgender identity) to understand the distribution of perceptions. Sensitivity analyses were conducted among the overall sample by people who smoke daily versus somedays. Due to sample size concerns for comparisons across race/ethnicity group, sexual orientation, and transgender identity, perceptions of harm of cigarettes, non-combustible tobacco products, and nicotine to health were modeled as a continuous measure from 0 (“Not at all harmful”) to 4 (“Extremely harmful”). All other measures were collapsed to a bivariate measure, which compared the misperception versus the accurate perception based on available evidence to date.
Analyses were conducted using SAS version 9.4. There were minimal missing data (<1–3%) for any given measure. Respondents’ missing measures were excluded from the corresponding analysis. In accordance with the PATH user guidebook [58], analyses were performed with appropriate survey procedures, sampling weights, and variance estimation [63,64] to produce estimates representative of the non-institutionalized, civilian U.S. population at the time of Wave 4 data collection (2016–2017). Data were summarized descriptively via weighted means or proportions and corresponding 95% confidence intervals (CIs).
For the race/ethnicity comparisons, respondents who identified as white (non-HLS) were used as the reference group for two reasons: (1) to frame the results to highlight implications for minoritized groups that may experience smoking-related disparities resulting from systemic racism and social/economic disadvantage; and (2) white (non-HLS) respondents had the largest sample size and therefore, resulted in the greatest statistical power. Similarly, for the sexual orientation and gender identity comparisons, respondents who identified as straight were used as the reference group for sexual orientation modeling and respondents who identified as non-transgender were used as the reference group for gender identity modeling. Similarly, people identifying as straight and non-transgender were used as the reference groups because members of the LGBTQ+ community experience greater smoking-related disparities attributable to stigma/discrimination and the straight/non-transgender groups had larger sample sizes, which resulted in the greatest statistical power.
3. Results
3.1. Overall Sample
The overall sample comprised 8340 respondents who reported current and established use of cigarettes but no current and established use of non-combustible tobacco products. Average respondent age was 44.45 years and slightly more than one-half were male (51.88%) and reported that their highest level of educational attainment was high school graduation/GED or less (57.93%).
Distributions of perceptions among the overall sample are shown in Figure 1A–D and Supplementary Table S1. Regarding harmfulness of cigarettes, snus, e-cigarettes, and nicotine, the vast majority of participants perceived these products to be in the range of ‘somewhat harmful’ to ‘extremely harmful’ (Figure 1A). Distribution of responses to harmfulness of e-cigarettes differed the most from that of cigarettes whereby responses of ‘not at all harmful’, ‘slightly harmful’ and ‘somewhat harmful’ were higher for e-cigarettes than cigarettes. Results based on a continuous variable from 0 (not at all harmful) to 4 (extremely harmful) reflect these distributions, whereby the mean response varied slightly from 2.49 for e-cigarettes to 2.94 for cigarettes (Supplementary Table S1). Regarding harmfulness relative to cigarettes (Figure 1B), the majority of respondents indicated LNC cigarettes, snus, and e-cigarettes to be ‘about the same’ harmfulness as cigarettes. Relative to NRT, the majority of respondents indicated e-cigarettes to be ‘about the same’ harmfulness as NRT and the distribution of responses nearly mirrored the distribution of responses when harmfulness of e-cigarettes was relative to cigarettes. These relationships are likely explained by Figure 1C, which shows that nearly two-thirds (63.83%) of respondents reported “definitely yes” or “probably yes” to the statement ‘nicotine in cigarettes causes most of the cancer caused by smoking’. Finally, despite the vast majority (81.89%) of respondents reporting “definitely yes” or “probably yes” to the statement ‘nicotine causes people to use tobacco’ (Figure 1C), most respondents reported that LNC cigarettes had “about the same” level of addictiveness as normal nicotine content (NNC) cigarettes (Figure 1D).
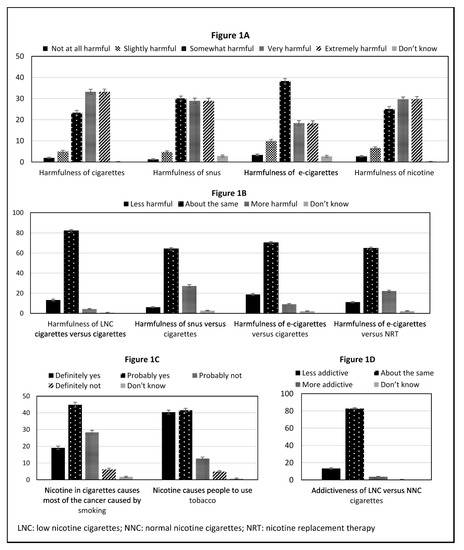
Figure 1.
Proportions and 95% confidence intervals for response categories. Persons who currently smoke daily or some days (n = 8430). (A) displays the perceived harm of products; (B) displays the relative risk of products; (C) displays health risks of nicotine; (D) displays the relative addictiveness of low nicotine cigarettes versus normal nicotine cigarettes.
Distributions of perceptions among respondents who smoke daily (i.e., removing respondents who smoked some days, n = 1785) are shown in Supplementary Figure S1A–D and Supplementary Table S1. Results were similar to those when including respondents who smoke some days. For these reasons, analyses comparing across race/ethnicity, sexual orientation, and gender identity combine respondents who currently smoke cigarettes daily and respondents who currently smoke somedays.
3.2. Race/Ethnicity Group Comparisons
As shown in Figure 2A and Table 1, patterns in mean responses to harmfulness of cigarettes, snus, e-cigarettes, and nicotine were similar across the multiple race and ethnicity groups with a few notable differences. The perceived harmfulness of e-cigarettes was significantly higher among American Indian/Alaskan Native respondents relative to white respondents. The perceived harmfulness of snus and nicotine was significantly higher among Black/African American respondents relative to white respondents. Similar observations were seen for Hispanic/Latino/Latina/Spanish origin respondents, but this is also within the context of this group viewing cigarettes as more harmful than white respondents.
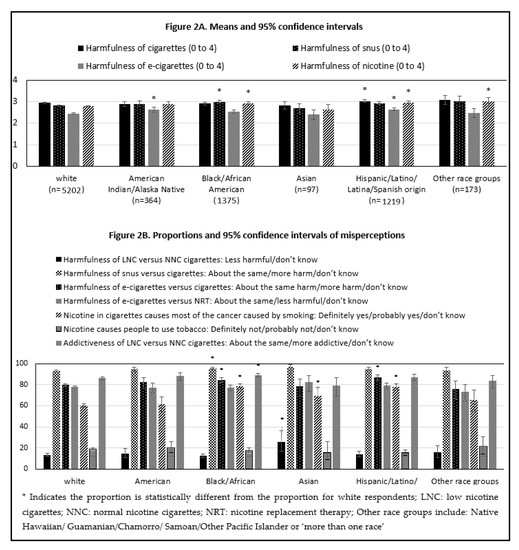
Figure 2.
Means or proportions and 95% confidence intervals for response categories. Persons who currently smoke daily or some days by race/ethnicity. (A) displays the perceived harm of products by racial and ethnic groups; (B) displays the proportion of respondents endorsing a misperception about nicotine or the relative risks of products by racial and ethnic group.

Table 1.
Weighted mean values or weighted proportions and corresponding 95% confidence intervals; PATH Wave 4 adults; Current established daily or someday smokers.
Figure 2B and Table 1 show proportions of misperceptions which include the response ‘don’t know’ by race/ethnicity. Between 12.38 and 25.53% of respondents across race and ethnicity groups reported a misperception to the statement on the harmfulness of LNC versus NNC cigarettes and the proportion was significantly higher for Asian respondents (25.53%) when compared with white respondents (12.38%). Misperceptions regarding harmfulness of snus and e-cigarettes versus cigarettes were represented among the vast majority (>75%) of respondents across race/ethnicity groups. A significantly greater proportion of Black/African American versus white respondents misperceived the harmfulness of snus and e-cigarettes relative to cigarettes. A significantly greater proportion of Hispanic/Latino/Latina/Spanish origin versus white respondents misperceived the harmfulness of e-cigarettes compared to cigarettes. The majority of respondents (>60%) across race/ethnicity groups indicated a misperception to the statement ‘nicotine in cigarettes causes most of the cancer caused by smoking’ and the proportion of respondents with the misperception was significantly higher among Black/African American (78.41%), Asian (69.53%) and Hispanic/Latino/Latina/Spanish origin (77.99%) versus white respondents (60.18%). Finally, the vast majority of respondents had a misperception about the addictiveness of LNC versus NNC cigarettes, with respondents reporting that LNC cigarettes are ‘about the same’ addictiveness as NNC cigarettes.
3.3. Sexual Orientation and Gender Identity Comparisons
As shown in Figure 3A and Table 2 and Table 3, patterns in mean responses to the harmfulness of cigarettes, snus, e-cigarettes, and nicotine were similar across sexual orientation and gender identity groups and reflect the overall population findings. However, there were a few significant differences. Perceived harmfulness of cigarettes and snus was higher for respondents who were bisexual versus straight respondents. Perceived harmfulness of cigarettes and nicotine in general was higher for respondents who were reported their sexual orientation as ‘something else’ versus straight.
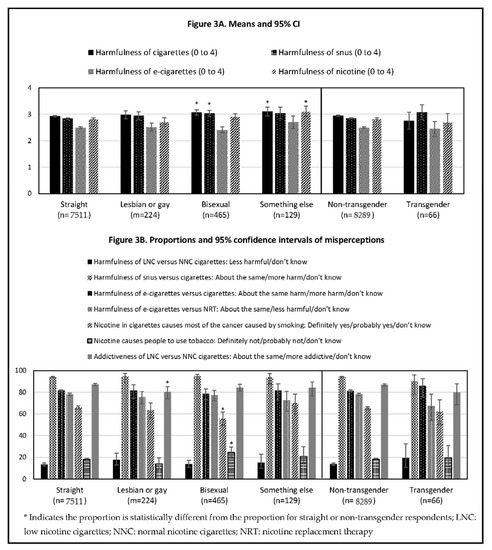
Figure 3.
Means or proportions and 95% confidence intervals for response categories. Persons who currently smoke daily or some days by sexual orientation and gender identity. (A) displays the perceived harm of products by sexual orientation and gender identity; (B) displays the proportion of respondents endorsing a misperception about nicotine or the relative risks of products by sexual orientation and gender identity.

Table 2.
Weighted mean values or weighted proportions and corresponding 95% confidence intervals; PATH Wave 4 adults; Current established daily or someday smokers who are not established users of non-combustible products by sexual orientation.

Table 3.
Weighted mean values or weighted proportions and corresponding 95% confidence intervals; PATH Wave 4 adults; Current established daily or someday smokers who are not established users of non-combustible products by transgender identity.
Overall, as shown in Figure 3B and Table 3, misperceptions were similar across sexual orientation and gender identity groups but with a few significant differences. The proportion who had a misperception on the addictiveness of LNC versus NNC cigarettes was lower in respondents who identified as lesbian or gay versus straight. The proportion who had a misperception to the statement ‘nicotine in cigarettes causes most of the cancer caused by smoking’ was lower in respondents who were bisexual compared to straight, while the proportion of respondents who had a misperception to the statement ‘nicotine causes people to use tobacco’ was higher in respondents who were bisexual compared to straight.
4. Discussion
Our results indicate that adults in the U.S. who smoke cigarettes generally have misperceptions about the harms of nicotine and the relative risks of ANDS products, which is consistent with findings from prior research [29,32,65]. For most of the risk perception questions we examined from the PATH survey, the majority of respondents, regardless of their racial/ethnic identity, sexual orientation, and gender identity, reported misperceptions. This is concerning because the FDA’s nicotine-focused framework relies on people who are unable or unwilling to quit nicotine to differentiate the harms of the different products. The most harmful delivery system of nicotine is the cigarette and other combusted products because the user is exposed to toxicants in the tobacco smoke that cause cancer and other smoking-related illnesses [6]. However, based on our findings from the relative risk questions, most people who smoke cigarettes do not differentiate between the harms of using cigarettes and the harms of using potentially reduced risk ANDS products, indicating that they do not understand the tobacco continuum of harm. For example, when comparing snus to cigarettes, over 90% of respondents indicated the non-combusted product was equally or more harmful than cigarettes. This finding is especially interesting in light of the fact that the FDA’s first approved ‘modified risk tobacco product’ application from Swedish Match was for the following snus relative risk claim: “Using General Snus instead of cigarettes puts you at lower risk of mouth cancer, heart disease, lung cancer, stroke, emphysema, and chronic bronchitis” [66]. A recent study found that when people who smoke were exposed to snus advertisements that included modified risk claims, the majority of respondents accurately reported lower relative risk perceptions for snus compared to cigarettes but also understood that snus is not completely harmless [67]. Thus, health communication campaigns explaining the tobacco continuum of harm, including the potential risks and benefits of using non-combusted products in place of cigarettes, will be critical when implementing a nicotine-focused framework.
Since risk perceptions contribute to behavior [40,41], examining perceptions by race/ethnicity, sexual orientation, and gender identity can help inform how these populations may respond to a low nicotine product standard in cigarettes. Moreover, early identification of misperceptions can provide an opportunity to prepare tailored messages prior to and concurrently with the implementation of a low nicotine product standard for cigarettes. In the current study, we found that the risk perception ratings across the populations studied generally aligned with the overall results and suggest that most people are not well-informed about the harms of nicotine. For example, nearly three-quarters of respondents indicated that the nicotine in medicinal nicotine products is somewhat to extremely harmful, which may partially explain why so few people use NRT during quit attempts [8]. As such, some people who want to quit smoking may benefit from other cessation approaches, such as mHealth applications or other pharmacotherapies (e.g., varenicline), to support their quit attempts, if efforts to correct misperceptions about medicinal nicotine risks are not successful. Overall, our results suggest that the majority of adults who smoke cigarettes across all priority populations could benefit from both nicotine-specific education, i.e., explaining the risks of addiction and correcting misperceptions about the health risks of nicotine, and product-specific education, i.e., explaining the relative risks across products containing nicotine.
That being said, there were a few notable differences in risk perceptions across the groups. First, a significantly greater proportion of respondents identifying as Black/African American, Asian and Hispanic/Latino/Latina/Spanish origin relative to white respondents incorrectly attributed nicotine as the ‘chemical that causes most of the cancer caused by smoking cigarettes’, although the majority of respondents also indicated this misperception. Respondents who identified as American Indian/Alaskan Native and Hispanic/Latino/Latina/Spanish origin had significantly higher e-cigarette risk ratings relative to respondents identifying as white. Respondents identifying as Black/African American, Hispanic/Latino/Latina/Spanish origin, bisexual, or another sexual orientation reported higher risk perceptions ratings for snus relative to respondents identifying as white or straight. Together, these findings could be interpreted to suggest that some people from minoritized groups may be less willing to switch to ANDS products if the FDA implements a low nicotine product standard for cigarettes. If these individuals instead continue to smoke cigarettes (i.e., LNC cigarettes), then the full benefits of a nicotine reduction policy for these minoritized groups may be attenuated and, as a result, widen existing smoking disparities. However, another interpretation is that more people from minoritized groups would quit tobacco altogether—as the robust VLNC literature indicates that use of VLNC cigarettes increases the likelihood of making a quit attempt or achieving abstinence [12,13,18,68,69,70,71,72]—versus switching to ANDS products. These findings merit further exploration. To date, little research is available examining the impact of a low nicotine product standard for cigarettes on smoking and quitting behavior among most of the minoritized groups examined in the current study.
Developing and implementing targeted communication interventions for different racial/ethnic groups as well as sexual orientation and gender identity would allow public health officials to more effectively communicate with these subgroups based on their unique values, perceptions of tobacco products, and causes of tobacco use (e.g., systemic racism). Targeting messages to specific populations enhances its effectiveness, because messages are most effective when they are perceived as relevant to a population [73,74]. One successful example of targeted messaging is The Real Cost national campaign, aimed at preventing youth from initiating smoking [45,46,75]. However, we are unaware of any existing messaging for many of the minoritized groups examined in this study, with a few exceptions [76,77,78]. Thus, future research should explore optimal ways to communicate to these groups about a low nicotine product standard for cigarettes and the tobacco continuum of harm.
Interestingly, the only question for which the majority of respondents answered correctly was that ‘nicotine causes people to use tobacco’. In contrast, across the different populations studied, between 79 and 89% of respondents reported the misperception that LNC cigarettes had ‘about the same’ level of addictiveness as NNC cigarettes. Our findings highlight an important disconnect in understanding of LNC cigarettes with regard to the measures used in the present study. Potential reasons for this disconnect may include that participants interpreted the question on LNC cigarettes as referring to “light” or “ultra-light” cigarettes, which were falsely promoted by the tobacco industry as safer cigarettes [78]. Another possible reason for the observed disconnect is that the nicotine level of LNC cigarettes was never quantified in the survey measure. Recent studies have shown that stating “95% of the nicotine would be removed”, which reflects levels of nicotine in LNC cigarettes versus conventional cigarettes, results in more accurate perceptions of the addictiveness of LNC cigarettes [79]. Another observed misperception is that over 60% of respondents indicated that it is the nicotine in cigarettes causing cancer, which is consistent with prior studies including one among U.S. physicians [31,32,80]. Again, such findings point to the need for educating the public about the harms of nicotine and LNC cigarettes prior to implementing a low nicotine product standard for cigarettes. As shown in prior research by Villanti and colleagues, brief communication interventions can be effective in correcting misperceptions of LNC cigarettes, ANDS products, and medicinal nicotine [28].
Our findings must be considered within the context of a few limitations. First, Wave 4 recruitment occurred in 2016–2017, so perceptions of alternative products may have changed over time. Second, new nicotine products, such as heated tobacco products and oral nicotine pouches, are now available and should be examined within the context of the nicotine-focused framework, especially since IQOS, a heated tobacco product, has received approval by the FDA to be marketed as a modified risk tobacco product [81]. Future research may want to examine perceptions of IQOS’ reduced exposure claims relative to LNC cigarettes and other ANDS products. Third, as previously described, the wording of the question assessing the relative addictiveness of low nicotine cigarettes compared to conventional cigarettes was vague, which may have contributed to misperceptions. Fourth, we opted to focus on snus specifically rather than all smokeless tobacco products because of the robust epidemiological literature supporting reduced health risks compared to smoking [32]. Studies examining absolute and relative risk perceptions of other smokeless tobacco products may also be important for understanding how the public perceives the tobacco continuum of harm. Fifth, this study did not examine adolescent risk perceptions, a population for which e-cigarettes are the most frequently used tobacco product [82]. One challenge for communicating risks of using ANDS relative to smoking cigarettes will be to do so in a manner that encourages product switching among adults who are unwilling or unable to stop smoking but that does not encourage adolescents to experiment with the products because they may misinterpret reduced harm to mean no harm. More communication research is needed that balances adolescent prevention and adult harm reduction messaging. Finally, we want to reiterate that race and ethnicity are social and not biological constructs. Grouping respondents into mutually exclusive categories increased our sample sizes and subsequently our statistical power to identify differences across the groups. However, this approach limited our ability to examine the important within-group differences that exist across minoritized groups, such as American Indian/Alaskan Native and Asian populations and the LGBTQ+ community. This study is a first step in understanding the risk perceptions of LNC cigarettes and ANDS products among understudied, minoritized groups; however, more research is needed to understand the nuances within groups in order to inform future health communication campaigns.
5. Conclusions
The majority of adults who smoke cigarettes reported misperceptions about nicotine and nicotine-containing products with relatively consistent findings across different priority smoking populations. Thus, if the FDA intends to move forward with implementing a nicotine-focused framework to improve public health, then time and resources are needed to educate the public about the tobacco continuum of harm and to correct misperceptions about nicotine, low nicotine content cigarettes, ANDS products, including e-cigarettes and snus, and medicinal nicotine. Additional targeted messages for racial, ethnic and LGBTQ+ groups may also be beneficial for ensuring that all smoking populations benefit from a nicotine-focused framework.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijerph18105311/s1, Figure S1: Proportions and 95% confidence intervals for all response categories, Table S1: Weighted mean values or weighted proportions and corresponding 95% confidence intervals.
Author Contributions
Conceptualization, D.M.C., R.L.D.-A., L.R.P., J.C.R., M.B.-T., E.C.D. and D.K.H.; methodology, D.M.C., R.L.D.-A. and L.R.P.; software, D.M.C.; formal analysis, D.M.C.; investigation, D.M.C. and R.L.D.-A.; resources, E.C.D. and D.K.H.; data curation, D.M.C.; Writing—Original draft preparation, D.M.C. and R.L.D.-A.; Writing—Review and Editing, L.R.P., J.C.R., M.B.-T., E.C.D. and D.K.H.; visualization, D.M.C.; supervision, E.C.D. and D.K.H.; project administration, D.M.C. and R.L.D.-A.; funding acquisition, E.C.D. and D.K.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Institute of Drug Abuse and the Food and Drug Administration’s Center for Tobacco Products, grant number U54DA031659 (to EC Donny and DK Hatsukami); the National Institute on Drug Abuse, grant number K01DA043413 (to LR Pacek); the National Institute on Minority Health and Health Disparities, grant number K01MD014795 (to DM Carroll); and the National Cancer Institute, grant number R03CA252767 (to RL Denlinger-Apte). This content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Food and Drug Administration.
Institutional Review Board Statement
This study was submitted for review by the University of Minnesota institutional review board and deemed to not constitute human subjects research due to the de-identified nature of the secondary data analysis.
Informed Consent Statement
Not applicable.
Data Availability Statement
All analyses were performed in the Inter-university Consortium for Political and Social Research’s Virtual Data Enclave (VDE) using the PATH Restricted Use Files [55]. Details on how to access these data are found here: https://www.icpsr.umich.edu/web/NAHDAP/studies/36231, accessed 15 January–15 March 2021.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Gottlieb, S.; Zeller, M. A Nicotine-Focused Framework for Public Health. N. Engl. J. Med. 2017, 377, 1111–1114. [Google Scholar] [CrossRef] [PubMed]
- Abrams, D.B.; Glasser, A.M.; Pearson, J.L.; Villanti, A.C.; Collins, L.K.; Niaura, R.S. Harm Minimization and Tobacco Control: Reframing Societal Views of Nicotine Use to Rapidly Save Lives. Ann. Rev. Public Health 2018, 39, 193–213. [Google Scholar] [CrossRef] [PubMed]
- Zeller, M.; Hatsukami, D.K. The Strategic Dialogue on Tobacco Harm Reduction Group The Strategic Dialogue on Tobacco Harm Reduction: A vision and blueprint for action in the US. Tob. Control 2009, 18, 324–332. [Google Scholar] [CrossRef]
- US Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General; Department Of Health And Human Services: Washington, DC, USA, 2014.
- Hecht, S.S. Tobacco Smoke Carcinogens and Lung Cancer. J. Natl. Cancer Inst. 1999, 91, 1194–1210. [Google Scholar] [CrossRef] [PubMed]
- A Report of the Surgeon General: How Tobacco Smoke Causes Disease; Surgeon General’s Report; U.S.; Department of Health and Human Services, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health: Washington, DC, USA, 2010.
- Cornelius, M.E.; Wang, T.W.; Jamal, A.; Loretan, C.G.; Neff, L.J. Tobacco Product Use Among Adults—United States, 2019. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1736–1742. [Google Scholar] [CrossRef]
- Smoking Cessation: A Report of the Surgeon General; Department of Health and Human Services, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health: Atlanta, GA, USA, 2020.
- Hartmann-Boyce, J.; Chepkin, S.C.; Ye, W.; Bullen, C.; Lancaster, T. Nicotine replacement therapy versus control for smoking cessation. Cochrane Database Syst. Rev. 2018, 5, CD000146. [Google Scholar] [CrossRef] [PubMed]
- Benowitz, N.L.; Henningfield, J.E. Establishing a Nicotine Threshold for Addiction—The Implications for Tobacco Regulation. N. Engl. J. Med. 1994, 331, 123–125. [Google Scholar] [CrossRef] [PubMed]
- Benowitz, N.L.; E Henningfield, J. Reducing the nicotine content to make cigarettes less addictive. Tob. Control 2013, 22, i14–i17. [Google Scholar] [CrossRef]
- Donny, E.C.; Denlinger, R.L.; Tidey, J.W.; Koopmeiners, J.S.; Benowitz, N.L.; Vandrey, R.G.; Al’Absi, M.; Carmella, S.G.; Cinciripini, P.M.; Dermody, S.S.; et al. Randomized Trial of Reduced-Nicotine Standards for Cigarettes. N. Engl. J. Med. 2015, 373, 1340–1349. [Google Scholar] [CrossRef] [PubMed]
- Hatsukami, D.K.; Luo, X.; Jensen, J.A.; al’Absi, M.; Allen, S.S.; Carmella, S.G.; Chen, M.; Cinciripini, P.M.; Denlinger-Apte, R.; Drobes, D.J.; et al. Effect of Immediate vs Gradual Reduction in Nicotine Content of Cigarettes on Biomarkers of Smoke Exposure: A Randomized Clinical Trial. JAMA 2018, 320, 880–891. [Google Scholar] [CrossRef] [PubMed]
- Shiffman, S.; Kurland, B.F.; Scholl, S.M.; Mao, J.M. Nondaily Smokers’ Changes in Cigarette Consumption With Very Low-Nicotine-Content Cigarettes: A Randomized Double-blind Clinical Trial. JAMA Psychiatry 2018, 75, 995–1002. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.T.; Koopmeiners, J.S.; Tessier, K.M.; Davis, E.M.; Conklin, C.A.; Denlinger-Apte, R.L.; Lane, T.; Murphy, S.E.; Tidey, J.W.; Hatsukami, D.K.; et al. Randomized Trial of Low-Nicotine Cigarettes and Transdermal Nicotine. Am. J. Prev. Med. 2019, 57, 515–524. [Google Scholar] [CrossRef] [PubMed]
- Tidey, J.W.; Colby, S.M.; Denlinger-Apte, R.L.; Goodwin, C.; A Cioe, P.; Cassidy, R.N.; Swift, R.M.; Lindgren, B.R.; Rubin, N.; Murphy, S.E.; et al. Effects of 6-Week Use of Very Low Nicotine Content Cigarettes in Smokers With Serious Mental Illness. Nicotine Tob. Res. 2019, 21, S38–S45. [Google Scholar] [CrossRef] [PubMed]
- Higgins, S.T.; Tidey, J.W.; Sigmon, S.C.; Heil, S.H.; Gaalema, D.E.; Lee, D.; Hughes, J.R.; Villanti, A.C.; Bunn, J.Y.; Davis, D.R.; et al. Changes in Cigarette Consumption With Reduced Nicotine Content Cigarettes Among Smokers With Psychiatric Conditions or Socioeconomic Disadvantage: 3 Randomized Clinical Trials. JAMA Netw. Open 2020, 3, e2019311. [Google Scholar] [CrossRef]
- Krebs, N.M.; Zhu, J.; Wasserman, E.; Kuprewicz, R.; Martinez, D.J.; Veldheer, S.; Livelsberger, C.; Modesto, J.; Reinhart, L.; Trushin, N.; et al. Switching to Progressively Reduced Nicotine Content Cigarettes in Smokers With Low Socioeconomic Status: A Double-Blind Randomized Clinical Trial. Nicotine Tob. Res. 2020. [Google Scholar] [CrossRef] [PubMed]
- Mercincavage, M.; Lochbuehler, K.; Wileyto, E.P.; Benowitz, N.L.; Tyndale, R.F.; Lerman, C.; Strasser, A.A. Association of Reduced Nicotine Content Cigarettes With Smoking Behaviors and Biomarkers of Exposure Among Slow and Fast Nicotine Metabolizers: A Nonrandomized Clinical Trial. JAMA Netw. Open 2018, 1, e181346. [Google Scholar] [CrossRef] [PubMed]
- Pacek, L.R.; Vandrey, R.; Dermody, S.S.; Denlinger-Apte, R.L.; Lemieux, A.; Tidey, J.W.; McClernon, F.J.; Bangdiwala, A.S.; Drobes, D.J.; Al’Absi, M.; et al. Evaluation of a reduced nicotine product standard: Moderating effects of and impact on cannabis use. Drug Alcohol Depend. 2016, 167, 228–232. [Google Scholar] [CrossRef]
- Smith, T.T.; Koopmeiners, J.S.; White, C.M.; Denlinger-Apte, R.L.; Pacek, L.R.; De Jesús, V.R.; Wang, L.; Watson, C.; Blount, B.C.; Hatsukami, D.K.; et al. The Impact of Exclusive Use of Very Low Nicotine Cigarettes on Compensatory Smoking: An Inpatient Crossover Clinical Trial. Cancer Epidemiol. Biomark. Prev. 2020, 29, 880–886. [Google Scholar] [CrossRef]
- Denlinger-Apte, R.L.; Donny, E.C.; Lindgren, B.R.; Rubin, N.; Goodwin, C.; DeAtley, T.; Colby, S.M.; A Cioe, P.; Hatsukami, D.K.; Tidey, J.W. Smoking Topography Characteristics During a 6-Week Trial of Very Low Nicotine Content Cigarettes in Smokers With Serious Mental Illness. Nicotine Tob. Res. 2019, 22, 1414–1418. [Google Scholar] [CrossRef]
- Dermody, S.S.; Tidey, J.W.; Denlinger, R.L.; Pacek, L.R.; Al’Absi, M.; Drobes, D.J.; Hatsukami, R.K.; Vandrey, R.; Donny, E.C. The Impact of Smoking Very Low Nicotine Content Cigarettes on Alcohol Use. Alcohol. Clin. Exp. Res. 2016, 40, 606–615. [Google Scholar] [CrossRef]
- Dermody, S.S.; Tessier, K.M.; Meier, E.; Al’Absi, M.; Denlinger-Apte, R.L.; Drobes, D.J.; Jensen, J.; Koopmeiners, J.S.; Pacek, L.R.; Tidey, J.W.; et al. An Evaluation of Potential Unintended Consequences of a Nicotine Product Standard: A Focus on Drinking History and Outcomes. Nicotine Tob. Res. 2020. [Google Scholar] [CrossRef]
- Higgins, S.T.; Heil, S.H.; Sigmon, S.C.; Tidey, J.W.; Gaalema, D.E.; Hughes, J.R.; Stitzer, M.L.; Durand, H.; Bunn, J.Y.; Priest, J.S.; et al. Addiction Potential of Cigarettes with Reduced Nicotine Content in Populations With Psychiatric Disorders and Other Vulnerabilities to Tobacco Addiction. JAMA Psychiatry 2017, 74, 1056. [Google Scholar] [CrossRef] [PubMed]
- Tidey, J.W.; Pacek, L.R.; Koopmeiners, J.S.; Vandrey, R.; Nardone, N.; Drobes, D.J.; Benowitz, N.L.; Dermody, S.S.; Lemieux, A.; Denlinger, R.L.; et al. Effects of 6-Week Use of Reduced-Nicotine Content Cigarettes in Smokers With and Without Elevated Depressive Symptoms. Nicotine Tob. Res. 2016, 19, 59–67. [Google Scholar] [CrossRef]
- Apelberg, B.J.; Feirman, S.P.; Salazar, E.; Corey, C.G.; Ambrose, B.K.; Paredes, A.; Richman, E.; Verzi, S.J.; Vugrin, E.D.; Brodsky, N.S.; et al. Potential Public Health Effects of Reducing Nicotine Levels in Cigarettes in the United States. N. Engl. J. Med. 2018, 378, 1725–1733. [Google Scholar] [CrossRef] [PubMed]
- Villanti, A.C.; Byron, M.J.; Mercincavage, M.; Pacek, L.R. Misperceptions of Nicotine and Nicotine Reduction: The Importance of Public Education to Maximize the Benefits of a Nicotine Reduction Standard. Nicotine Tob. Res. 2019, 21, S88–S90. [Google Scholar] [CrossRef] [PubMed]
- Bansal, M.A.; Cummings, K.M.; Hyland, A.; Giovino, G.A. Stop-smoking medications: Who uses them, who misuses them, and who is misinformed about them? Nicotine Tob. Res. 2004, 6, 303–310. [Google Scholar] [CrossRef]
- Bansal-Travers, M.; Cummings, K.M.; Hyland, A.; Brown, A.; Celestino, P. Educating smokers about their cigarettes and nicotine medications. Health Educ. Res. 2010, 25, 678–686. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, E.K.; Nguyen, A.B.; Persoskie, A.; Hoffman, A.C. U.S. adults’ addiction and harm beliefs about nicotine and low nicotine cigarettes. Prev. Med. 2017, 96, 94–100. [Google Scholar] [CrossRef]
- Byron, M.J.; Jeong, M.; Abrams, D.B.; Brewer, N.T. Public misperception that very low nicotine cigarettes are less carcinogenic. Tob. Control 2018, 27, 712–714. [Google Scholar] [CrossRef]
- Romijnders, K.A.G.J.; Van Osch, L.; De Vries, H.; Talhout, R. Perceptions and Reasons Regarding E-Cigarette Use among Users and Non-Users: A Narrative Literature Review. Int. J. Environ. Res. Public Health 2018, 15, 1190. [Google Scholar] [CrossRef]
- Glasser, A.M.; Collins, L.; Pearson, J.L.; Abudayyeh, H.; Niaura, R.S.; Abrams, D.B.; Villanti, A.C. Overview of Electronic Nicotine Delivery Systems: A Systematic Review. Am. J. Prev. Med. 2017, 52, e33–e66. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Feng, B.; Weaver, S.R.; Pechacek, T.F.; Slovic, P.; Eriksen, M.P. Changing Perceptions of Harm of e-Cigarette vs Cigarette Use Among Adults in 2 US National Surveys From 2012 to 2017. JAMA Netw. Open 2019, 2, e191047. [Google Scholar] [CrossRef]
- Wackowski, O.A.; Ray, A.E.; Stapleton, J.L. Smokers’ perceptions of risks and harm from snus relative to cigarettes: A latent profile analysis study. Addict. Behav. 2019, 91, 171–174. [Google Scholar] [CrossRef] [PubMed]
- Wackowski, O.A.; Delnevo, C.D. Young Adults’ Risk Perceptions of Various Tobacco Products Relative to Cigarettes: Results From the National Young Adult Health Survey. Health Educ. Behav. 2016, 43, 328–336. [Google Scholar] [CrossRef]
- Popova, L.; Ling, P.M. Perceptions of Relative Risk of Snus and Cigarettes Among US Smokers. Am. J. Public Health 2013, 103, e21–e23. [Google Scholar] [CrossRef]
- Clarke, E.; Thompson, K.; Weaver, S.; Thompson, J.; O’Connell, G. Snus: A compelling harm reduction alternative to cigarettes. Harm Reduct. J. 2019, 16, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, I.M. The health belief model and preventive health behavior. Health Educ. Behav. 1974, 2, 354–386. [Google Scholar] [CrossRef]
- Ajzen, I. From Intentions to Actions: A Theory of Planned Behavior. In Action Control; SSSP Spring Series in Social Psychology; Kuhl, J., Beckmann, J., Eds.; Springer: Berlin/Heidelberg, Germany, 1985. [Google Scholar]
- Schmälzle, R.; Renner, B.; Schupp, H.T. Health Risk Perception and Risk Communication. Policy Insights Behav. Brain Sci. 2017, 4, 163–169. [Google Scholar] [CrossRef]
- Yzer, M. Reasoned action theory: Persuasion as belief-based behavior change. In The SAGE Handbook of Persuasion: Developments in Theory and Practice; SAGE Publications, Inc.: Newcastle upon Tyne, UK, 2012; pp. 120–136. [Google Scholar]
- Brennan, E.; Gibson, L.A.; Kybert-Momjian, A.; Liu, J.; Hornik, R.C. Promising Themes for Antismoking Campaigns Targeting Youth and Young Adults. Tob. Regul. Sci. 2017, 3, 29–46. [Google Scholar] [CrossRef]
- Duke, J.C.; MacMonegle, A.J.; Nonnemaker, J.M.; Farrelly, M.C.; Delahanty, J.C.; Zhao, X.; Smith, A.A.; Rao, P.; Allen, J.A. Impact of The Real Cost Media Campaign on Youth Smoking Initiation. Am. J. Prev. Med. 2019, 57, 645–651. [Google Scholar] [CrossRef]
- Farrelly, M.C.; Duke, J.C.; Nonnemaker, J.; MacMonegle, A.J.; Alexander, T.N.; Zhao, X.; Delahanty, J.C.; Rao, P.; Allen, J.A. Association Between The Real Cost Media Campaign and Smoking Initiation Among Youths—United States, 2014–2016. MMWR. Morb. Mortal. Wkly. Rep. 2017, 66, 47–50. [Google Scholar] [CrossRef] [PubMed]
- Bello, M.S.; Liautaud, M.M.; De La Cerda, J.T.; Pang, R.D.; Ray, L.A.; Ahluwalia, J.A.; Leventhal, A.M. Association of frequency of perceived exposure to discrimination with tobacco withdrawal symptoms and smoking lapse behavior in African Americans. Addiction 2021, 116, 914–925. [Google Scholar] [CrossRef]
- Kcomt, L.; Evans-Polce, R.J.; Engstrom, C.W.; West, B.T.; McCabe, S.E. Discrimination, Sexual Orientation Discrimination, and Severity of Tobacco Use Disorder in the United States: Results From the National Epidemiologic Survey on Alcohol and Related Conditions-III. Nicotine Tob. Res. 2020. [Google Scholar] [CrossRef] [PubMed]
- Kendzor, D.E.; Businelle, M.S.; Reitzel, L.R.; Rios, D.M.; Scheuermann, T.S.; Pulvers, K.; Ahluwalia, J.S. Everyday Discrimination Is Associated With Nicotine Dependence Among African American, Latino, and White Smokers. Nicotine Tob. Res. 2013, 16, 633–640. [Google Scholar] [CrossRef] [PubMed]
- Washington, H.A. Burning Love: Big Tobacco Takes Aim at LGBT Youths. Am. J. Public Health 2002, 92, 1086–1095. [Google Scholar] [CrossRef] [PubMed]
- Anderson, S.J. Marketing of menthol cigarettes and consumer perceptions: A review of tobacco industry documents. Tob. Control 2011, 20, ii20–ii28. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.G.L.; Henriksen, L.; Rose, S.W.; Moreland-Russell, S.; Ribisl, K.M. A Systematic Review of Neighborhood Disparities in Point-of-Sale Tobacco Marketing. Am. J. Public Health 2015, 105, e8–e18. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.G.L.; Pan, W.K.; Henriksen, L.; Goldstein, A.O.; Ribisl, K.M. Is There a Relationship Between the Concentration of Same-Sex Couples and Tobacco Retailer Density? Nicotine Tob. Res. 2016, 18, 147–155. [Google Scholar] [CrossRef]
- Ribisl, K.M.; D’Angelo, H.; Feld, A.L.; Schleicher, N.C.; Golden, S.D.; Luke, D.A.; Henriksen, L. Disparities in tobacco marketing and product availability at the point of sale: Results of a national study. Prev. Med. 2017, 105, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Ganz, O.; Johnson, A.L.; Cohn, A.M.; Rath, J.; Horn, K.; Vallone, D.; Villanti, A.C. Tobacco harm perceptions and use among sexual and gender minorities: Findings from a national sample of young adults in the United States. Addict. Behav. 2018, 81, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Nayak, P.; Salazar, L.F.; Kota, K.K.; Pechacek, T.F. Prevalence of use and perceptions of risk of novel and other alternative tobacco products among sexual minority adults: Results from an online national survey, 2014–2015. Prev. Med. 2017, 104, 71–78. [Google Scholar] [CrossRef]
- Hyland, A.; Ambrose, B.K.; Conway, K.P.; Borek, N.; Lambert, E.; Carusi, C.; Taylor, K.; Crosse, S.; Fong, G.T.; Cummings, K.M.; et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) Study. Tob. Control 2017, 26, 371–378. [Google Scholar] [CrossRef]
- United States Department of Health and Human Services; National Institutes of Health; National Institute on Drug Abuse; Food and Drug Administration; Center for Tobacco Products. Population Assessment of Tobacco and Health (PATH) Study [United States] Restricted-Use Files 2021; Population Assessment of Tobacco and Health (PATH) Study Series; Inter-University Consortium for Political and Social Research: Ann Arbor, MI, USA, 2021.
- NCAI Policy Research Center, Disaggregating American Indian & Alaska Native Data: A Review of Literature; National Congress of American Indians: Washington, DC, USA, 2016.
- Carroll, D.M.; Soto, C.; Baezconde-Garbanati, L.; Huang, L.-L.; Lienemann, B.A.; Meissner, H.I.; Rose, S.W.; Unger, J.B.; Cruz, T.B. Tobacco Industry Marketing Exposure and Commercial Tobacco Product Use Disparities among American Indians and Alaska Natives. Subst. Use Misuse 2019, 55, 261–270. [Google Scholar] [CrossRef]
- Cobb, N.; Espey, D.; King, J. Health Behaviors and Risk Factors Among American Indians and Alaska Natives, 2000–2010. Am. J. Public Health 2014, 104, S481–S489. [Google Scholar] [CrossRef] [PubMed]
- Espey, D.K.; Jim, M.A.; Cobb, N.; Bartholomew, M.; Becker, T.; Haverkamp, D.; Plescia, M. Leading Causes of Death and All-Cause Mortality in American Indians and Alaska Natives. Am. J. Public Health 2014, 104, S303–S311. [Google Scholar] [CrossRef] [PubMed]
- Judkins, D.R. Fay’s method for variance estimation. J. Off. Stat. 1990, 6, 223–239. [Google Scholar]
- McCarthy, P.J. Pseudoreplication: Further Evaluation and Applications of the Balanced Half-Sample Technique; Department of Health and Human Services, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health: Washington, DC, USA, 1969. [Google Scholar]
- Cardamone, L.; Salzberg, M.R.; O’Brien, T.J.; Jones, N.C. Antidepressant therapy in epilepsy: Can treating the comorbidities affect the underlying disorder? Br. J. Pharmacol. 2013, 168, 1531–1554. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration. FDA Grants First-Ever Modified Risk Orders to Eight Smokeless Tobacco Products; Food and Drug Administration: Silver Spring, MD, USA, 2019.
- Pillitteri, J.L.; Shiffman, S.; Sembower, M.A.; Polster, M.R.; Curtin, G.M. Assessing comprehension and perceptions of modified-risk information for snus among adult current cigarette smokers, former tobacco users, and never tobacco users. Addict. Behav. Rep. 2020, 11, 100254. [Google Scholar] [CrossRef]
- Denlinger-Apte, R.L.; Kotlyar, M.; Koopmeiners, J.S.; Tidey, J.W.; Luo, X.; Benowitz, N.L.; A Jensen, J.; Ikuemonisan, J.O.; Pacek, L.R.; Smith, T.T.; et al. Effects of Very Low Nicotine Content Cigarettes on Smoking Behavior and Biomarkers of Exposure in Menthol and Non-menthol Smokers. Nicotine Tob. Res. 2019, 21, S63–S72. [Google Scholar] [CrossRef]
- Hatsukami, D.K.; Hertsgaard, L.A.; Vogel, R.I.; Jensen, J.A.; Murphy, S.E.; Hecht, S.S.; Carmella, S.G.; Al’Absi, M.; Joseph, A.M.; Allen, S.S. Reduced Nicotine Content Cigarettes and Nicotine Patch. Cancer Epidemiol. Biomark. Prev. 2013, 22, 1015–1024. [Google Scholar] [CrossRef]
- Hatsukami, D.K.; Kotlyar, M.; Hertsgaard, L.A.; Zhang, Y.; Carmella, S.G.; Jensen, J.A.; Allen, S.S.; Shields, P.G.; Murphy, S.E.; Stepanov, I.; et al. Reduced nicotine content cigarettes: Effects on toxicant exposure, dependence and cessation. Addiction 2010, 105, 343–355. [Google Scholar] [CrossRef] [PubMed]
- Walker, N.; Howe, C.; Bullen, C.; Grigg, M.; Glover, M.; McRobbie, H.; Laugesen, M.; Parag, V.; Whittaker, R. The combined effect of very low nicotine content cigarettes, used as an adjunct to usual Quitline care (nicotine replacement therapy and behavioural support), on smoking cessation: A randomized controlled trial. Addiction 2012, 107, 1857–1867. [Google Scholar] [CrossRef] [PubMed]
- McRobbie, H.; Przulj, D.; Smith, K.M.; Cornwall, D. Complementing the Standard Multicomponent Treatment for Smokers with Denicotinized Cigarettes: A Randomized Trial. Nicotine Tob. Res. 2015, 18, 1134–1141. [Google Scholar] [CrossRef] [PubMed]
- Baig, S.A.; Pepper, J.K.; Morgan, J.C.; Brewer, N.T. Social identity and support for counteracting tobacco company marketing that targets vulnerable populations. Soc. Sci. Med. 2017, 182, 136–141. [Google Scholar] [CrossRef] [PubMed]
- Kreuter, M.W.; Wray, R.J. Tailored and Targeted Health Communication: Strategies for Enhancing Information Relevance. Am. J. Health Behav. 2003, 27 (Suppl. 3), S227–S232. [Google Scholar] [CrossRef]
- Navarro, M.A.; Hoffman, L.; Crankshaw, E.C.; Guillory, J.; Jacobs, S. LGBT Identity and Its Influence on Perceived Effectiveness of Advertisements from a LGBT Tobacco Public Education Campaign. J. Health Commun. 2019, 24, 469–481. [Google Scholar] [CrossRef] [PubMed]
- Hinds, J.T.; Chow, S.; Loukas, A.; Perry, C.L. Reactions to targeted tobacco control messaging: Transgender and gender diverse young adult perspectives. Drug Alcohol Depend. 2021, 218, 108440. [Google Scholar] [CrossRef]
- Cruz, T.B.; Rose, S.W.; Lienemann, B.A.; Byron, M.J.; Meissner, H.I.; Baezconde-Garbanati, L.; Huang, L.-L.; Carroll, D.M.; Soto, C.; Unger, J.B. Pro-tobacco marketing and anti-tobacco campaigns aimed at vulnerable populations: A review of the literature. Tob. Induc. Dis. 2019, 17, 68. [Google Scholar] [CrossRef]
- Shiffman, S.; Pillitteri, J.L.; Burton, S.L.; Rohay, J.M.; Gitchell, J.G. Smokers’ beliefs about “Light” and “Ultra Light” cigarettes. Tob. Control 2001, 10, i17–i23. [Google Scholar]
- Byron, M.J.; Hall, M.G.; King, J.L.; Ribisl, K.M.; Brewer, N.T. Reducing Nicotine Without Misleading the Public: Descriptions of Cigarette Nicotine Level and Accuracy of Perceptions About Nicotine Content, Addictiveness, and Risk. Nicotine Tob. Res. 2019, 21, S101–S107. [Google Scholar] [CrossRef]
- Steinberg, M.B.; Manderski, M.T.B.; Wackowski, O.A.; Singh, B.; Strasser, A.A.; Delnevo, C.D. Nicotine Risk Misperception Among US Physicians. J. Gen. Intern. Med. 2020, 1–3. [Google Scholar] [CrossRef] [PubMed]
- FDA Authorizes Marketing of IQOS Tobacco Heating System with ‘Reduced Exposure’ Information; FDA: New Hampshire, MD, USA, 2020; Volume 7.
- Gentzke, A.S.; Creamer, M.; Cullen, K.A.; Ambrose, B.K.; Willis, G.; Jamal, A.; King, B.A. Vital Signs: Tobacco Product Use among Middle and High School Students—United States, 2011–2018. MMWR. Morb. Mortal. Wkly. Rep. 2019, 68, 157–164. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).