Burnout in Professional Psychotherapists: Relationships with Self-Compassion, Work–Life Balance, and Telepressure
Abstract
1. Introduction
1.1. High Rates of Burnout in Professional Psychotherapists
1.2. Self-Compassion
1.3. Burnout and Work–Life Balance
1.4. Telepressure
1.5. Aims
- RQ1.
- How is burnout related to self-compassion, work–life balance and telepressure?
- RQ2.
- RQ2. How is burnout predicted by these variables?
- RQ3.
- Does self-compassion moderate the relationship between work–life balance and burnout?
2. Materials and Methods
2.1. Participants
2.2. Instruments
2.3. Procedure
3. Results
3.1. Relationships among Motivation, Engagement, Resilience, and Self-Criticism/-Compassion (RQ1)
3.2. Predictors of Motivation (RQ2)
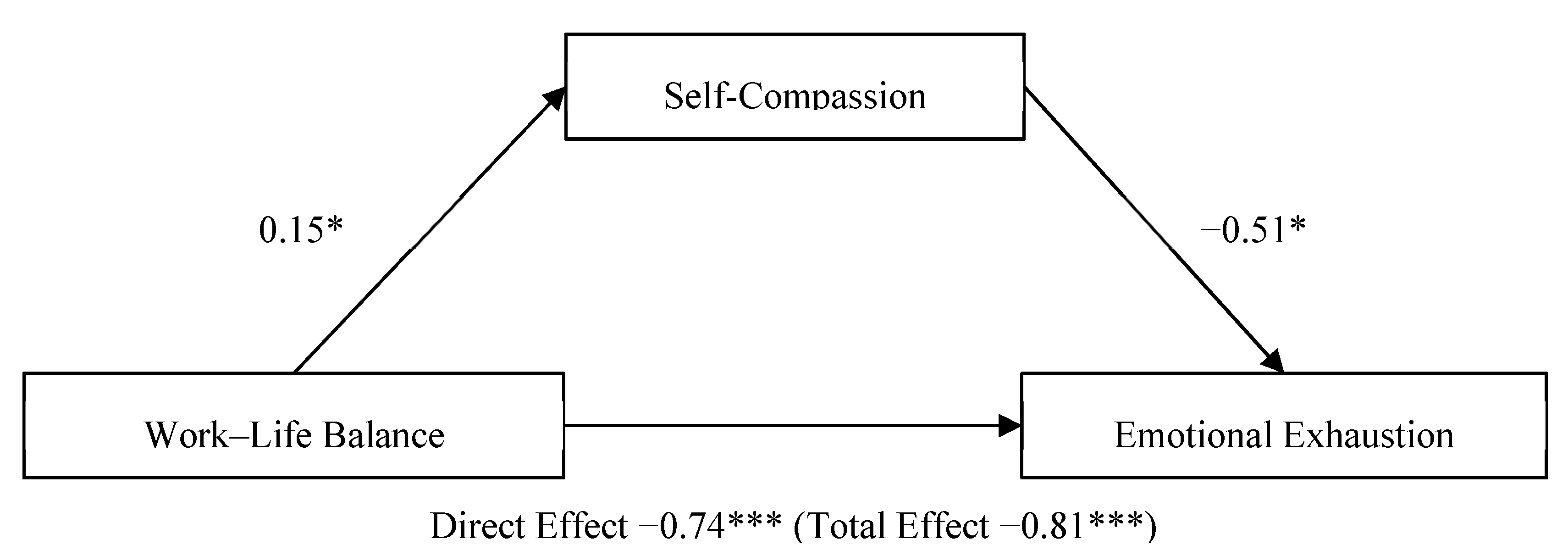
3.3. Mediation of Self-Compassion on Work–Life Balance—Emotional Exhaustion
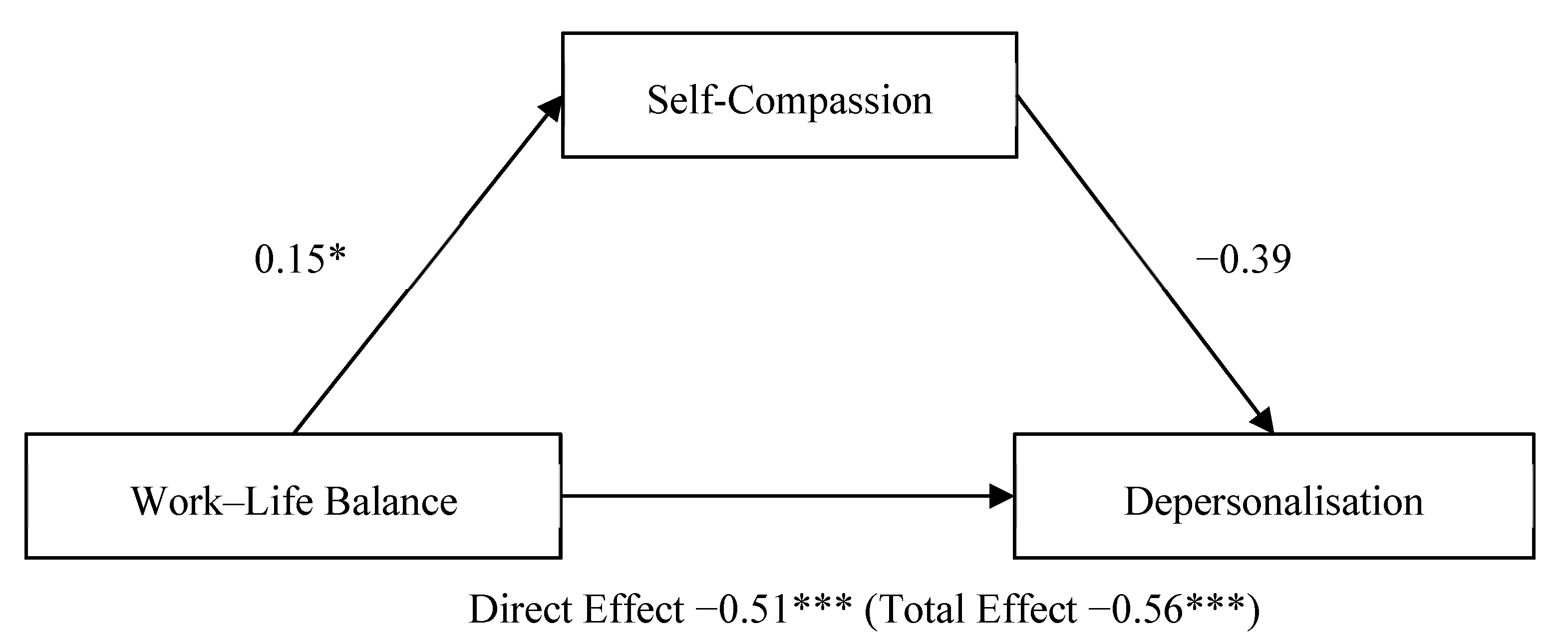
3.4. Mediation of Self-Compassion on Work–Life Balance—Depersonalisation
4. Discussion
4.1. Self-Compassion and Burnout
4.2. Predictors of Burnout
4.3. Mediation of Self-Compassion on Work–Life Balance
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- De Kock, J.H.; Latham, H.A.; Leslie, S.J.; Grindle, M.; Munoz, S.A.; Ellis, L.; Polson, R.; O’Malley, C.M. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: Implications for supporting psychological well-being. BMC Public Health 2021, 21, 104. [Google Scholar] [CrossRef] [PubMed]
- Godlee, F. Protect our healthcare workers. Br. Med. J. 2020, 369, m1324. [Google Scholar] [CrossRef]
- Gold, J.A. Covid-19: Adverse mental health outcomes for healthcare workers. Br. Med. J. 2020, 369. [Google Scholar] [CrossRef] [PubMed]
- Preti, E.; Di Mattei, V.; Perego, G.; Ferrari, F.; Mazzetti, M.; Taranto, P.; Di Pierro, R.; Madeddu, F.; Calati, R. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: Rapid review of the evidence. J. Behav. Health Serv. Res. 2020, 22, 504–518. [Google Scholar] [CrossRef]
- Knaak, S.; Mantler, E.; Szeto, A. Mental illness-related stigma in healthcare: Barriers to access and care and evidence-based solutions. Healthc Manag. Forum. 2017, 30, 111–116. [Google Scholar] [CrossRef]
- Stuijfzand, S.; Deforges, C.; Sandoz, V.; Sajin, C.-T.; Jaques, C.; Elmers, J.; Horsch, A. Psychological impact of an epidemic/pandemic on the mental health of healthcare professionals: A rapid review. BMC Public Health 2020, 20, 1230. [Google Scholar] [CrossRef] [PubMed]
- Simionato, G.; Simpson, S.; Reid, C. Burnout as an ethical issue in psychotherapy. J. Clin. Psychol. 2019, 56, 470–482. [Google Scholar] [CrossRef]
- Deniz, M.E. Self-compassion, intolerance of uncertainty, fear of COVID-19, and well-being: A serial mediation investigation. Pers. Individ. Differ. 2021, 177, 110824. [Google Scholar] [CrossRef]
- Simionato, G.K.; Simpson, S. Personal risk factors associated with burnout among psychotherapists: A systematic review of the literature. J. Clin. Psychol. 2018, 74, 1431–1456. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, P. The Compassionate Mind; Robinson: Edinburgh, UK, 2009. [Google Scholar]
- Nguyen, T.M.; Le, G.N.H. The influence of COVID-19 stress on psychological well-being among Vietnamese adults: The role of self-compassion and gratitude. Traumatology 2021. [Google Scholar] [CrossRef]
- Neff, K. Definition and Three Elements of Self Compassion. Available online: https://self-compassion.org/the-three-elements-of-self-compassion-2/# (accessed on 11 May 2021).
- Allen, A.B.; Goldwasser, E.R.; Leary, M.R. Self-compassion and Well-being among Older Adults. Self Identity 2012, 11, 428–453. [Google Scholar] [CrossRef] [PubMed]
- Satici, S.A.; Kayis, A.R.; Satici, B.; Griffiths, M.D.; Can, G. Resilience, hope, and subjective happiness among the turkish population: Fear of COVID-19 as a mediator. Int. J. Ment. Health Addict. 2020. [Google Scholar] [CrossRef] [PubMed]
- Kotera, Y.; Ozaki, A.; Miyatake, H.; Tsunetoshi, C.; Nishikawa, Y.; Tanimoto, T. Mental health of medical workers in Japan during COVID-19: Relationships with loneliness, hope and self-compassion. Curr. Psychol. 2021. [Google Scholar] [CrossRef]
- Maslach, C.; Leiter, M.P. Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry 2016, 15, 103–111. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E. The job demands-resources model: State of the art. J. Manag. Psychol. 2007, 22, 309–328. [Google Scholar] [CrossRef]
- WHO. Burn-Out an ‘Occupational Phenomenon’: International Classification of Diseases, Burn-out an ‘Occupational Phenomenon’: International Classification of Diseases. Available online: https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases (accessed on 24 April 2021).
- Hobfoll, S.E. Conservation of resources: A new attempt at conceptualizing stress. Am. Psychol. 1989, 44, 513–524. [Google Scholar] [CrossRef]
- Campion, J.; Javed, A.; Sartorius, N.; Marmot, M. Addressing the public mental health challenge of COVID-19. Lancet Psychiatry 2020, 7, 657–659. [Google Scholar] [CrossRef]
- Chaturvedi, S.K. Covid-19, Coronavirus and mental health rehabilitation at times of crisis. J. Psychosoc. Rehabil. Ment. Health 2020, 7, 1–2. [Google Scholar] [CrossRef]
- Mukhtar, S. Mental health and psychosocial aspects of coronavirus outbreak in Pakistan: Psychological intervention for public mental health crisis. Asian J. Psychiatry 2020, 51, 102069. [Google Scholar] [CrossRef] [PubMed]
- Raudenská, J.; Steinerová, V.; Javůrková, A.; Urits, I.; Kaye, A.D.; Viswanath, O.; Varrassi, G. Occupational burnout syndrome and post-traumatic stress among healthcare professionals during the novel coronavirus disease 2019 (COVID-19) pandemic. Best Pr. Res. Clin. Anaesthesiol. 2020, 34, 553–560. [Google Scholar] [CrossRef] [PubMed]
- Steffensen, D.S.; McAllister, C.P.; Perrewé, P.L.; Wang, G.; Brooks, C.D. “You’ve got mail”: A daily investigation of email demands on job tension and work-family conflict. J. Bus. Psychol. 2021, 1–14. [Google Scholar] [CrossRef]
- ONS. Coronavirus and Homeworking in the UK; Office for National Statistics: London, UK, 2020.
- Shklarski, L.; Abrams, A.; Bakst, E. Navigating changes in the physical and psychological spaces of psychotherapists during Covid-19: When home becomes the office. Pract. Innov. 2021, 6, 55–66. [Google Scholar] [CrossRef]
- Barber, L.K.; Santuzzi, A.M. Please respond ASAP: Workplace telepressure and employee recovery. J. Occup. Health Psychol. 2015, 20, 172–189. [Google Scholar] [CrossRef] [PubMed]
- Barnett, J.E. The ethical practice of psychotherapy: Clearly within our reach. Psychotherapy 2019, 56, 431–440. [Google Scholar] [CrossRef]
- Montemurro, N.; Perrini, P. Will COVID-19 change neurosurgical clinical practice? Br. J. Neurosurg. 2020, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Kotera, Y.; Cockerill, V.; Chircop, J.G.E.; Forman, D. Mental health shame, self-compassion and sleep in UK nursing students: Complete mediation of self-compassion in sleep and mental health. Nurs. Open 2021, 8, 1325–1335. [Google Scholar] [CrossRef]
- Coleman, C.; Martensen, C.; Scott, R.; Indelicato, N.A. Unpacking self-care: The connection between mindfulness, self-compassion, and self-care for counselors. Couns. Wellness Prof. Couns. J. 2016, 5, 1–8. [Google Scholar]
- BACP. BACP Ethical Framework for the Counselling Professions. Available online: https://www.bacp.co.uk/events-and-resources/ethics-and-standards/ethical-framework-for-the-counselling-professions/ (accessed on 11 May 2021).
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- West, C.P.; Dyrbye, L.N.; Satele, D.V.; Sloan, J.A.; Shanafelt, T.D. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J. Gen. Intern. Med. 2012, 27, 1445–1452. [Google Scholar] [CrossRef]
- Raes, F.; Pommier, E.; Neff, K.D.; Van Gucht, D. Construction and factorial validation of a short form of the Self-compassion scale. Clin. Psychol. Psychother. 2011, 18, 250255. [Google Scholar] [CrossRef]
- Neff, K.D. The development and validation of a scale to measure self-compassion. Self Identity 2003, 2, 223–250. [Google Scholar] [CrossRef]
- Daniels, L.; Carraher, L. The Work-Life Manual: Gaining a Competitive Edge by Balancing the Demands of Employees’ Work and Home Lives; Industorial Society: London, UK, 2000. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; The Guilford Press: New York, NY, USA, 2013; p. 507. [Google Scholar]
- Hoaglin, D.C.; Iglewicz, B. Fine-tuning some resistant rules for outlier labeling. J. Am. Stat. Assoc. 1987, 82, 1147. [Google Scholar] [CrossRef]
- Tukey, J.W. The Future of data analysis. Ann. Math. Stat. 1962, 33, 1–67. [Google Scholar] [CrossRef]
- Manh Than, H.; Minh Nong, V.; Trung Nguyen, C.; Phu Dong, K.; Ngo, H.T.; Thu Doan, T.; Thu Do, N.; Huyen Thi Nguyen, T.; Van Do, T.; Xuan Dao, C.; et al. Mental health and health-related quality-of-life outcomes among frontline health workers during the peak of COVID-19 outbreak in Vietnam: A cross-sectional study. Risk Manag. Healthc. Policy 2020, 13, 2927–2936. [Google Scholar] [CrossRef]
- Xiao, X.; Zhu, X.; Fu, S.; Hu, Y.; Li, X.; Xiao, J. Psychological impact of healthcare workers in China during COVID-19 pneumonia epidemic: A multi-center cross-sectional survey investigation. J. Affect. Disord. 2020, 274, 405–410. [Google Scholar] [CrossRef] [PubMed]
- Field, A.P. Discovering Statistics Using IBM SPSS Statistics; Sage: London, UK, 2017. [Google Scholar]
- Schaufeli, W.; Salanova, M.; González-romá, V.; Bakker, A. The measurement of engagement and burnout: A two sample confirmatory factor analytic approach. J. Happiness Stud. 2002, 3, 71–92. [Google Scholar] [CrossRef]
- Neff, K.D. Self-compassion, self-esteem, and well-being. Soc. Pers. Psychol. Compass 2011, 5, 1–12. [Google Scholar] [CrossRef]
- Coaston, S.C. Self-care through self-compassion: A balm for burnout. Prof. Couns. 2017, 7, 285–297. [Google Scholar] [CrossRef]
- Neff, K.D.; Knox, M.C.; Long, P.; Gregory, K. Caring for others without losing yourself: An adaptation of the mindful self-compassion program for healthcare communities. J. Clin. Psychol. 2020. [Google Scholar] [CrossRef]
- Santuzzi, A.M.; Barber, L.K. Workplace Telepressure and Worker Well-Being: The Intervening Role of Psychological Detachment. Occup. Health Sci. 2018, 2, 337–363. [Google Scholar] [CrossRef]
- Molino, M.; Cortese, C.G.; Ghislieri, C. Unsustainable working conditions: The association of destructive leadership, use of technology, and workload withworkaholism and exhaustion. Sustainability 2019, 11, 446. [Google Scholar] [CrossRef]
- Antoun, J.; Brown, D.J.; Jones, D.J.W.; Sangala, N.C.; Lewis, R.J.; Shepherd, A.I.; McNarry, M.A.; Mackintosh, K.A.; Mason, L.; Corbett, J.; et al. Understanding the impact of initial COVID-19 restrictions on physical activity, wellbeing and quality of life in shielding adults with end-stage renal disease in the United Kingdom dialysing at home versus in-centre and their experiences with telemedicine. Int. J. Environ. Res. Public Health 2021, 18, 3144. [Google Scholar] [CrossRef] [PubMed]
- Dev, V.; Fernando, A.T.; Lim, A.G.; Consedine, N.S. Does self-compassion mitigate the relationship between burnout and barriers to compassion? A cross-sectional quantitative study of 799 nurses. Int. J. Nurs. Stud. 2018, 81, 81–88. [Google Scholar] [CrossRef]
- Kirby, J.N. Compassion interventions: The programmes, the evidence, and implications for research and practice. Psychol. Psychother. Theory Res. Pract. 2017, 90, 432–455. [Google Scholar] [CrossRef]
- Kotera, Y.; Green, P.; Sheffield, D. Work-life balance of UK construction workers: Relationship with mental health. Constr. Manag. Econ. 2019, 38. [Google Scholar] [CrossRef]
- Krasner, M.S.; Epstein, R.M.; Beckman, H.; Suchman, A.L.; Chapman, B.; Mooney, C.J.; Quill, T.E. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. J. Am. Med. Assoc. 2009, 302, 1284–1293. [Google Scholar] [CrossRef]
- Kotera, Y. De-stigmatising self-care: Impact of self-care webinar during COVID-19. Int. J. Spa Wellness 2021, 1–5. [Google Scholar] [CrossRef]
- Kotera, Y.; Green, P.; Rhodes, C.; Williams, A.; Chircop, J.; Spink, R.; Rawson, R.; Okere, U. Dealing with isolation using online morning huddles for university lecturers during physical distancing by COVID-19: Field notes. Int. Rev. Res. Open Distrib. Learn. 2020, 21, 238–244. [Google Scholar] [CrossRef]
- Ugwu, L.I.; Enwereuzor, I.K.; Fimber, U.S.; Ugwu, D.I. Nurses’ burnout and counterproductive work behavior in a Nigerian sample: The moderating role of emotional intelligence. Int. J. Afr. Nurs. Sci. 2017, 7, 106–113. [Google Scholar] [CrossRef]
- Nishimura, K.; Nakamura, F.; Takegami, M.; Fukuhara, S.; Nakagawara, J.; Ogasawara, K.; Ono, J.; Shiokawa, Y.; Miyachi, S.; Nagata, I.; et al. Cross-sectional survey of workload and burnout among Japanese physicians working in stroke care the nationwide survey of acute stroke care capacity for proper designation of comprehensive stroke center in japan (j-aspect) study. Circ. Cardiovasc. Qual. Outcomes 2014, 7, 414–422. [Google Scholar] [CrossRef]
- Bannai, A.; Ukawa, S.; Tamakoshi, A. Long working hours and psychological distress among school teachers in Japan. J. Occup. Health 2015, 57, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Leiter, M.P.; Maslach, C. Areas of worklife: A structured approach to organizational predictors of job burnout. Res. Occup. Stress Well Being 2003, 3, 91–134. [Google Scholar] [CrossRef]
- McCormack, H.M.; MacIntyre, T.E.; O’Shea, D.; Herring, M.P.; Campbell, M.J. The prevalence and cause(s) of burnout among applied psychologists: A systematic review. Front. Psychol. 2018, 9, 1897. [Google Scholar] [CrossRef]
- Hashem, Z.; Zeinoun, P. Self-compassion explains less burnout among healthcare professionals. Mindfulness 2020, 11, 2542–2551. [Google Scholar] [CrossRef]
- Somer, E.; Amos-Williams, T.; Stein, D.J. Evidence-based treatment for depersonalisation-derealisation disorder (DPRD). BMC Psychol. 2013, 1, 20. [Google Scholar] [CrossRef]
- Farrelly, S.; Peters, E.; Azis, M.; David, A.; Hunter, E.C. A brief CBT intervention for depersonalisation/derealisation in psychosis: Study protocol for a feasibility randomised controlled trial. Pilot Feasibility Stud. 2016, 2, 47. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kotera, Y.; Van Gordon, W. Effects of self-compassion training on work-related well-being: A systematic review. Front. Psychol. 2021, 12. [Google Scholar] [CrossRef]
- Kotera, Y.; Sheffield, D. Revisiting the self-compassion scale-short form: Stronger associations with self-inadequacy and resilience. SN Compr. Clin. Med. 2020, 2, 761–769. [Google Scholar] [CrossRef]
- Kotera, Y.; Van Laethem, M.; Ohshima, R. Cross-cultural comparison of mental health between Japanese and Dutch workers: Relationships with mental health shame, self-compassion, work engagement and motivation. Cross Cult. Strateg. Manag. 2020, 27, 511–530. [Google Scholar] [CrossRef]
- Devaux, M.; Sassi, F. Social disparities in hazardous alcohol use: Self-report bias may lead to incorrect estimates. Eur. J. Public Health 2016, 26, 129–134. [Google Scholar] [CrossRef]
- Montemurro, N. Intracranial hemorrhage and COVID-19, but please do not forget “old diseases” and elective surgery. Brain Behav Immun. 2021, 92, 207–208. [Google Scholar] [CrossRef]
- Picaza Gorrochategi, M.; Eiguren Munitis, A.; Dosil Santamaria, M.; Ozamiz Etxebarria, N. Stress, anxiety, and depression in people aged over 60 in the COVID-19 outbreak in a sample collected in Northern Spain. Am. J. Geriatr. Psychiatry 2020, 28, 993–998. [Google Scholar] [CrossRef] [PubMed]
| Scale | Constructs (Range) | M | SD | α |
|---|---|---|---|---|
| Maslach Burnout Inventory 2-Item Version | Emotional Exhaustion (1–7) | 2.75 | 1.66 | NA |
| Depersonalisation (1–7) | 1.86 | 1.48 | NA | |
| Self-Compassion Scale-Short Form | Self-Compassion (1–5) | 3.67 | 0.73 | 0.90 |
| Work–Life Balance Checklist | Work–Life Balance (1–5) | 3.37 | 0.96 | 0.85 |
| 6-Item Telepressure Scale | Telepressure (1–5) | 2.58 | 0.97 | 0.93 |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Gender (0 = F, M = 1) | - | ||||||||
| 2 | Age | 0.13 | - | |||||||
| 3 | Experience | 0.02 | 0.60 ** | - | ||||||
| 4 | Weekly Working Hours | 0.19 | −0.02 | 0.32 ** | - | |||||
| 5 | Emotion Exhaustion | −0.05 | −0.41 ** | −0.01 | 0.48 ** | - | ||||
| 6 | Depersonalisation | 0.13 | −0.27 ** | −0.08 | 0.31 ** | 0.57 ** | - | |||
| 7 | Self-Compassion | 0.04 | 0.40 ** | 0.34 ** | 0.03 | −0.30 ** | −0.24 * | - | ||
| 8 | Work–Life Balance | −0.07 | 0.04 | 0.04 | −0.30 ** | −0.47 ** | −0.35 ** | 0.21 * | - | |
| 9 | Telepressure | −0.05 | −0.25 ** | −0.19 | −0.15 | 0.29 ** | 0.20 * | −0.29 ** | −0.19 | - |
| Emotional Exhaustion | Depersonalisation | |||||
|---|---|---|---|---|---|---|
| 95% CI | 95% CI | |||||
| B | Lower | Upper | B | Lower | Upper | |
| Step 1 | ||||||
| Gender (0 = F, 1 = M) | 0.004 | −0.20 | 0.21 | 0.17 | −0.02 | 0.37 |
| Age | −0.19 *** | −0.27 | −0.17 | −0.12 ** | −0.20 | −0.04 |
| Step 2 | ||||||
| Gender (0 = F, 1 = M) | −0.12 | −0.27 | 0.04 | 0.11 | −0.08 | 0.29 |
| Age | −0.14 *** | −0.21 | −0.07 | −0.09 * | −0.17 | −0.004 |
| Weekly Working Hours | 0.39 *** | 0.26 | 0.52 | 0.20 * | 0.04 | 0.35 |
| Self-Compassion | −0.19 | −0.56 | 0.18 | −0.20 | −0.63 | 0.24 |
| Work–Life Balance | −0.48 *** | −0.73 | −0.23 | −0.36 * | −0.66 | −0.05 |
| Telepressure | 0.24 ** | 0.06 | 0.41 | 0.13 | −0.07 | 0.34 |
| Adj. R2 Δ | 38% | 14% | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kotera, Y.; Maxwell-Jones, R.; Edwards, A.-M.; Knutton, N. Burnout in Professional Psychotherapists: Relationships with Self-Compassion, Work–Life Balance, and Telepressure. Int. J. Environ. Res. Public Health 2021, 18, 5308. https://doi.org/10.3390/ijerph18105308
Kotera Y, Maxwell-Jones R, Edwards A-M, Knutton N. Burnout in Professional Psychotherapists: Relationships with Self-Compassion, Work–Life Balance, and Telepressure. International Journal of Environmental Research and Public Health. 2021; 18(10):5308. https://doi.org/10.3390/ijerph18105308
Chicago/Turabian StyleKotera, Yasuhiro, Robert Maxwell-Jones, Ann-Marie Edwards, and Natalie Knutton. 2021. "Burnout in Professional Psychotherapists: Relationships with Self-Compassion, Work–Life Balance, and Telepressure" International Journal of Environmental Research and Public Health 18, no. 10: 5308. https://doi.org/10.3390/ijerph18105308
APA StyleKotera, Y., Maxwell-Jones, R., Edwards, A.-M., & Knutton, N. (2021). Burnout in Professional Psychotherapists: Relationships with Self-Compassion, Work–Life Balance, and Telepressure. International Journal of Environmental Research and Public Health, 18(10), 5308. https://doi.org/10.3390/ijerph18105308







