Postoperative Vomiting Following Laparoscopic Cholecystectomy Is Associated with Intraoperative Fluid Administration: A Retrospective Cohort Study
Abstract
1. Introduction
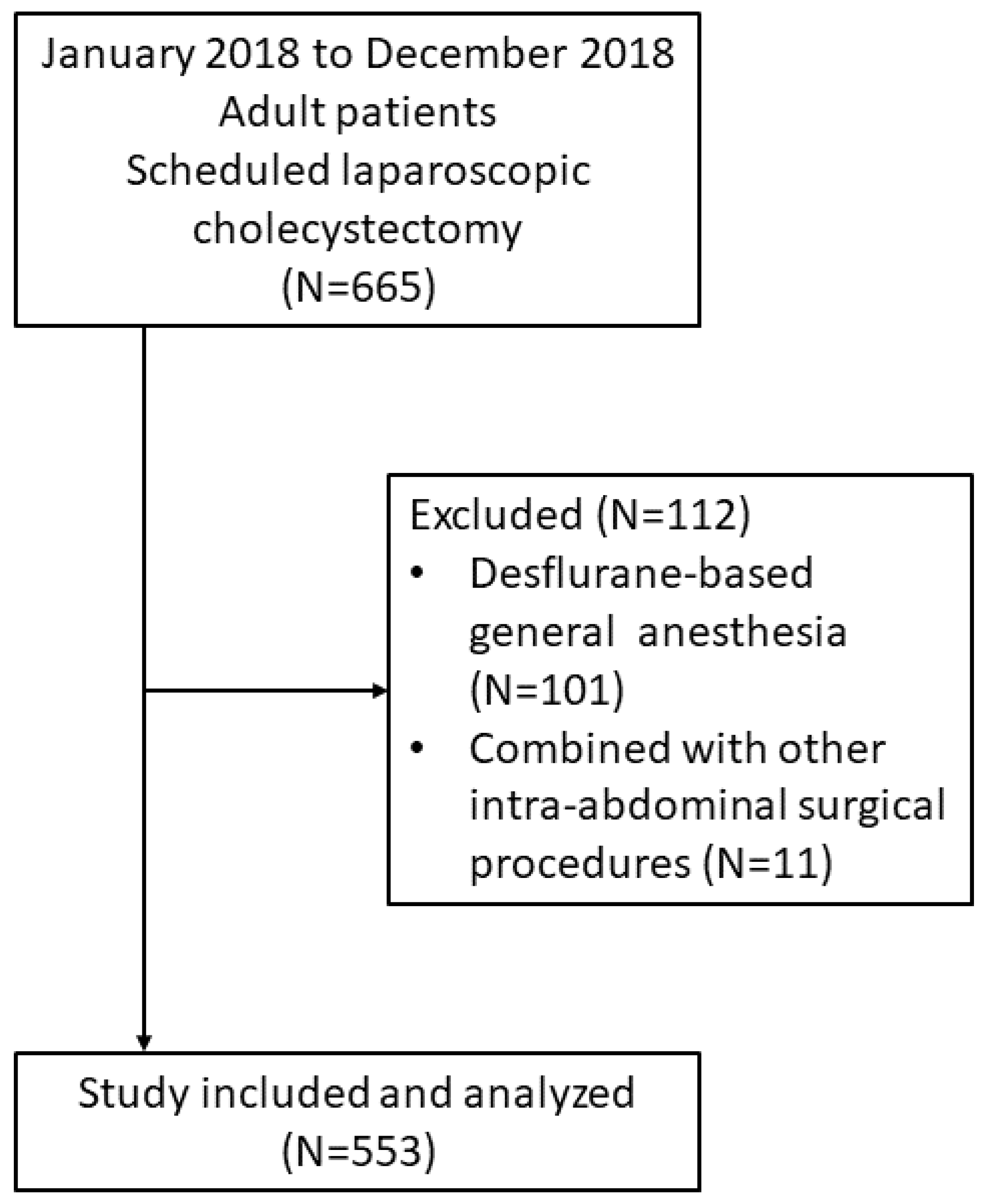
2. Methods
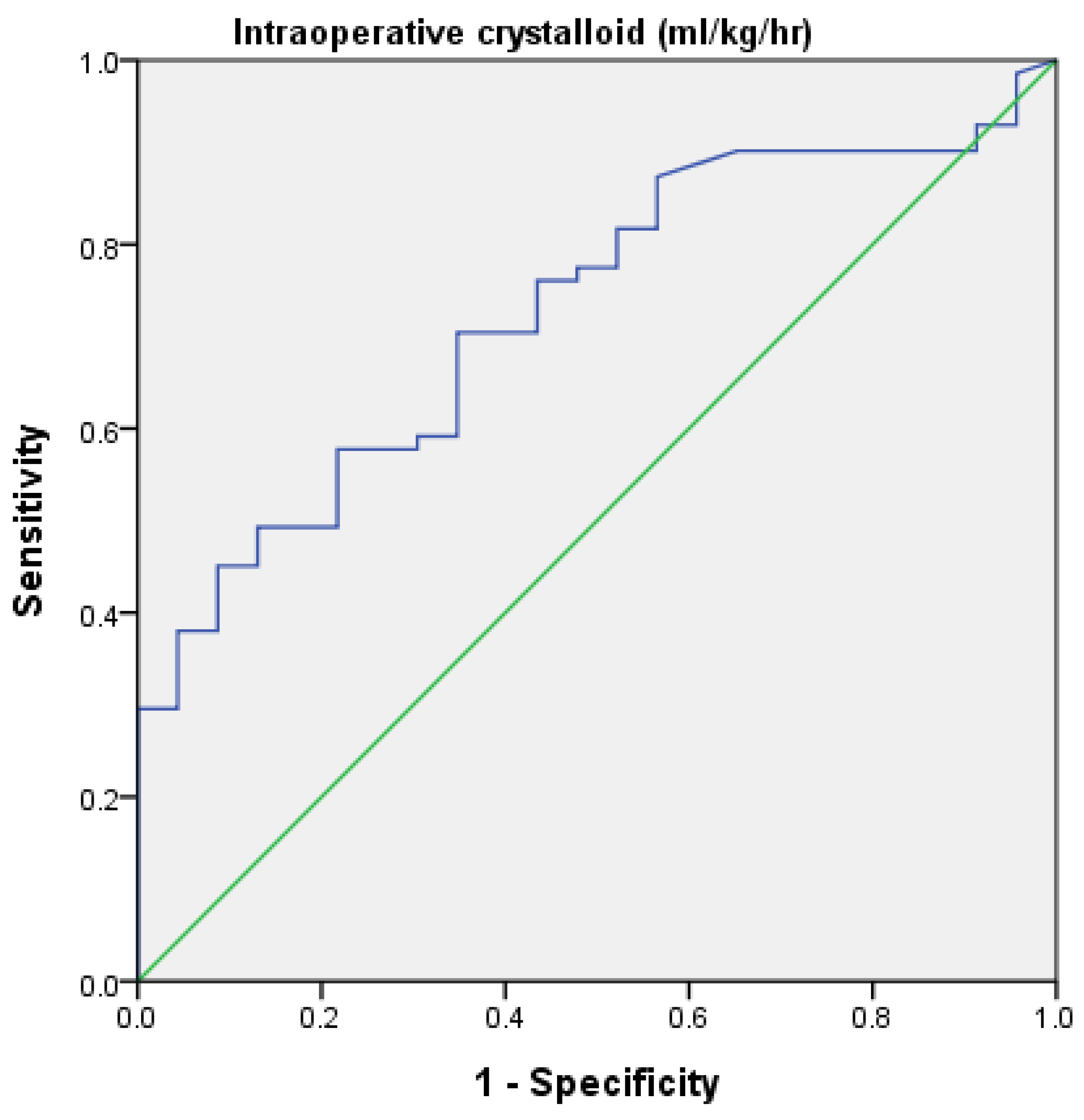
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Apfel, C.; Heidrich, F.; Jukar-Rao, S.; Jalota, L.; Hornuss, C.; Whelan, R.; Zhang, K.; Cakmakkaya, O. Evidence-based analysis of risk factors for postoperative nausea and vomiting. Br. J. Anaesth. 2012, 109, 742–753. [Google Scholar] [CrossRef]
- Cohen, M.M.; Duncan, P.G.; DeBoer, D.P.; Tweed, W.A. The postoperative interview: Assessing risk factors for nausea and vomiting. Anesth. Analg. 1994, 78, 7–16. [Google Scholar] [CrossRef]
- Apfel, C.C.; Laara, E.; Koivuranta, M.; Greim, C.A.; Roewer, N. A simplified risk score for predicting postoperative nausea and vomiting: Conclusions from cross-validations between two centers. Anesthesiology 1999, 91, 693–700. [Google Scholar] [CrossRef]
- Gan, T.J.; Belani, K.G.; Bergese, S.; Chung, F.; Diemunsch, P.; Habib, A.S.; Jin, Z.; Kovac, A.L.; Meyer, T.A.; Urman, R.D. Fourth consensus guidelines for the management of postoperative nausea and vomiting. Anesth. Analg. 2019, 131, 411–448. [Google Scholar] [CrossRef]
- Turgut, H.C.; Arslan, M. An overview of treatment options for postoperative nausea and vomiting after laparoscopic surgical procedures. Anaesth. Pain Intensive Care 2019, 20, 193–200. [Google Scholar]
- Back, I.N. Palliative Medicine Handbook, 3rd ed.; BPM Books: Cardiff, UK, 2001. [Google Scholar]
- Salazar-Parra, M.; Guzman-Ramirez, B.G.; Pintor-Belmontes, K.J.; Barbosa-Camacho, F.J.; Bernal-Hernandez, A.; Cruz-Neri, R.U.; Fuentes-Orozco, C.; Aguirre, L.L.R.; Rodriguez-Navarro, D.; Brancaccio-Perez, I.V.; et al. Gender Differences in Postoperative Pain, Nausea and Vomiting After Elective Laparoscopic Cholecystectomy. World J. Surg. 2020, 44, 4070–4076. [Google Scholar] [CrossRef]
- Bleier, J.I.; Aarons, C.B. Perioperative fluid restriction. Clin. Colon. Rectal. Surg. 2013, 26, 197–202. [Google Scholar] [CrossRef][Green Version]
- Ghosh, S.; Rai, K.K.; Shivakumar, H.R.; Upasi, A.P.; Naik, V.G.; Bharat, A. Incidence and risk factors for postoperative nausea and vomiting in orthognathic surgery: A 10-year retrospective study. J. Korean Assoc. Oral. Maxillofac. Surg. 2020, 46, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Jewer, J.K.; Wong, M.J.; Bird, S.J.; Habib, A.S.; Parker, R.; George, R.B. Supplemental perioperative intravenous crystalloids for postoperative nausea and vomiting. Cochrane Database Syst. Rev. 2019, 3, CD012212. [Google Scholar] [CrossRef]
- Holte, K.; Klarskov, B.; Christensen, D.S.; Lund, C.; Nielsen, K.G.; Bie, P.; Kehlet, H. Liberal versus restrictive fluid administration to improve recovery after laparoscopic cholecystectomy: A randomized, double-blind study. Ann. Surg. 2004, 240, 892–899. [Google Scholar] [CrossRef]
- Magner, J.J.; McCaul, C.; Carton, E.; Gardiner, J.; Buggy, D. Effect of intraoperative intravenous crystalloid infusion on postoperative nausea and vomiting after gynaecological laparoscopy: Comparison of 30 and 10 mL kg(−1). Br. J. Anaesth. 2004, 93, 381–385. [Google Scholar] [CrossRef]
- Apfel, C.C.; Kranke, P.; Katz, M.H.; Goepfert, C.; Papenfuss, T.; Rauch, S.; Heineck, R.; Greim, C.A.; Roewer, N. Volatile anaesthetics may be the main cause of early but not delayed postoperative vomiting: A randomized controlled trial of factorial design. Br. J. Anaesth. 2002, 88, 659–668. [Google Scholar] [CrossRef] [PubMed]
- Mauermann, E.; Clamer, D.; Ruppen, W.; Bandschapp, O. Association between intra-operative fentanyl dosing and postoperative nausea/vomiting and pain: A prospective cohort study. Eur. J. Anaesthesiol. 2019, 36, 871–880. [Google Scholar] [CrossRef] [PubMed]
- Roberts, G.W.; Bekker, T.B.; Carlsen, H.H.; Moffatt, C.H.; Slattery, P.J.; McClure, A.F. Postoperative nausea and vomiting are strongly influenced by postoperative opioid use in a dose-related manner. Anesth. Analg. 2005, 101, 1343–1348. [Google Scholar] [CrossRef]
- Coluzzi, F.; Pappagallo, M.; National Initiative on Pain Control. Opioid therapy for chronic noncancer pain: Practice guidelines for initiation and maintenance of therapy. Minerva Anestesiol. 2005, 71, 425–433. [Google Scholar] [PubMed]
- Ortega, A.E.; Peters, J.H.; Incarbone, R.; Estrada, L.; Ehsan, A.; Kwan, Y.; Spencer, C.J.; Moore-Jeffries, E.; Kuchta, K.; Nicoloff, J.T. A prospective randomized comparison of the metabolic and stress hormonal responses of laparoscopic and open cholecystectomy. J. Am. Coll. Surg. 1996, 183, 249–256. [Google Scholar] [PubMed]
- Vaughan, J.; Nagendran, M.; Cooper, J.; Davidson, B.R.; Gurusamy, K.S. Anaesthetic regimens for day-procedure laparoscopic cholecystectomy. Cochrane Database Syst. Rev. 2014, CD009784. [Google Scholar] [CrossRef] [PubMed]
- Longo, M.A.; Cavalheiro, B.T.; de Oliveira Filho, G.R. Laparoscopic cholecystectomy under neuraxial anesthesia compared with general anesthesia: Systematic review and meta-analyses. J. Clin. Anesth. 2017, 41, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Yu, G.; Wen, Q.; Qiu, L.; Bo, L.; Yu, J. Laparoscopic cholecystectomy under spinal anaesthesia vs. general anaesthesia: A meta-analysis of randomized controlled trials. BMC Anesth. 2015, 15, 176. [Google Scholar] [CrossRef] [PubMed]
- Zdravkovic, M.; Kamenik, M. A prospective randomized controlled study of combined spinal-general anesthesia vs. general anesthesia for laparoscopic gynecological surgery: Opioid sparing properties. J. Clin. Anesth. 2020, 64, 109808. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, S.I.; Nagarekha, D.; Hegade, G.; Marutheesh, M. Postoperative nausea and vomiting: A simple yet complex problem. Anesth Essays Res. 2016, 10, 388–396. [Google Scholar] [CrossRef] [PubMed]
- Weibel, S.; Schaefer, M.S.; Raj, D.; Rucker, G.; Pace, N.L.; Schlesinger, T.; Meybohm, P.; Kienbaum, P.; Eberhart, L.H.J.; Kranke, P. Drugs for preventing postoperative nausea and vomiting in adults after general anaesthesia: An abridged Cochrane network meta-analysis(‡ section sign). Anaesthesia 2020. [Google Scholar] [CrossRef]
- Klenke, S.; de Vries, G.J.; Schiefer, L.; Seyffert, N.; Bachmann, H.S.; Peters, J.; Frey, U.H. CHRM3 rs2165870 polymorphism is independently associated with postoperative nausea and vomiting, but combined prophylaxis is effective. Br. J. Anaesth. 2018, 121, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Darvall, J.N.; Leslie, K. Pounds of Prevention but Only Ounces of Cure: The Need for More Research on the Treatment of Postoperative Nausea and Vomiting. Anesthesiology 2019, 130, 183–185. [Google Scholar] [CrossRef] [PubMed]
| Features | Total | No POV | POV | p-Value |
|---|---|---|---|---|
| Sex | ||||
| Female | 296 (53.5%) | 225 (48.5%) | 71 (79.8%) | <0.001 *** |
| Male | 257 (46.5%) | 239 (51.5%) | 18 (20.2%) | |
| Age (years) | ||||
| 20 to 49 | 193 (34.9%) | 155 (33.4%) | 38 (42.7%) | 0.087 |
| 50 to 69 | 250 (45.2%) | 210 (45.3%) | 40 (44.9%) | |
| 70 and above | 110 (19.9%) | 99 (21.3%) | 11 (12.4%) | |
| Weight (kg) | 66.0 (58.0–75.5) | 67.0 (59.0–77.0) | 63.0 (54.5–70.5) | 0.001 ** |
| Sevoflurane consumption (mL/h) | 11.3 (9.2–13.2) | 11.3 (9.2–13.3) | 11.5 (9.3–13.0) | 0.946 |
| Morphine equivalent: Intraoperative (mg) | 13.0 (12.8–17.5) | 13.0 (12.5–17.9) | 13.0 (13.0–17.5) | 0.539 |
| Morphine equivalent: PACU (mg) | 0.59 (0.48–0.71) a | 0.58 (0.45–0.70) a | 0.67 (0.38–0.97) a | 0.522 |
| Morphine equivalent: Ward (mg) | 1.42 (1.12–1.72) a | 1.49 (1.15–1.83) a | 1.09 (0.39–1.78) a | 0.327 |
| BIS | ||||
| None | 238 (43.0%) | 207 (44.6%) | 31 (34.8%) | 0.088 |
| Yes | 315 (57.0%) | 257 (55.4%) | 58 (65.2%) | |
| ASA | ||||
| I | 25 (4.5%) | 19 (4.1%) | 6 (6.7%) | 0.033 * |
| II | 392 (70.9%) | 322 (69.4%) | 70 (78.7%) | |
| III | 136 (24.6%) | 123 (26.5%) | 13 (14.6%) | |
| Anesthesia time (h) | ||||
| <2 | 76 (13.7%) | 62 (13.4%) | 14 (15.7%) | 0.235 |
| 2 to <4 | 403 (72.9%) | 335 (72.2%) | 68 (76.4%) | |
| 4 and above | 74 (13.4%) | 67 (14.4%) | 7 (7.9%) | |
| Types of antiemetic drugs | 0.319 | |||
| None | 311 (56.2%) | 257 (55.4%) | 54 (60.7%) | |
| One | 204 (36.9%) | 172 (37.1%) | 32 (35.9%) | |
| Two and above | 38 (6.9%) | 35 (7.5%) | 3 (3.4%) | |
| Intraoperative crystalloid (mL/kg/h) | 2.35 (1.80–3.05) | 2.35 (1.82–3.06) | 2.38 (1.79–3.02) | 0.784 |
| Intraoperative urine output (mL/kg/h) | 0.38 (0.32–0.44) | 0.37 (0.33–0.45) | 0.31 (0.16–0.45) | 0.062 |
| Types of intraoperative antihypertensives | ||||
| None | 389 (70.3%) | 329 (70.9%) | 60 (67.4%) | |
| One | 137 (24.8%) | 115 (24.8%) | 22 (24.7%) | 0.402 |
| Two and above | 27 (4.9%) | 20 (4.3%) | 7 (7.9%) | |
| Patient-controlled analgesia | ||||
| None | 511 (92.4%) | 426 (91.8%) | 85 (95.5%) | 0.228 |
| Yes | 42 (7.6%) | 38 (8.2%) | 4 (4.5%) |
| Univariate | Multivariate | |||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Male | 1 | 1 | ||
| Female | 4.18 (2.42–7.25) | <0.001 *** | 9.71 (2.87–33.33) | <0.001 *** |
| Age 20 to 49 | 1 | 0.093 | 1 | 0.096 |
| Age 50 to 69 | 0.78 (0.48–1.27) | 0.313 | 0.41 (0.16–1.04) | 0.060 |
| Age 70 and above | 0.45 (0.22–0.93) | 0.030 * | 0.29 (0.09–0.96) | 0.043 * |
| Body weight | 0.97 (0.95–0.99) | 0.002 ** | 0.98 (0.95–1.01) | 0.104 |
| With BIS | 1 | 1 | ||
| Without BIS | 1.51 (0.94–2.42) | 0.089 | 1.35 (0.72–2.53) | 0.351 |
| Apfel score 0 | 1 | 1 | ||
| Apfel score 1 | 1.60 (0.72–3.55) | 0.251 | 0.28 (0.08–1.03) | 0.055 |
| Apfel score 2 | 2.39 (1.05–5.45) | 0.038* | 0.14 (0.02–0.85) | 0.032 * |
| Apfel score 3 and 4 | 3.30 (1.14–9.60) | 0.028* | 0.14 (0.02–1.06) | 0.056 |
| ASA I | 1 | 1 | ||
| ASA II | 0.69 (0.27–1.79) | 0.433 | 0.57 (0.16–2.07) | 0.389 |
| ASA III | 0.34 (0.11–0.99) | 0.047 * | 0.47 (0.11–2.09) | 0.321 |
| Sevoflurane consumption | 0.98 (0.93–1.04) | 0.551 | 1.04 (0.97–1.11) | 0.261 |
| Anesthesia time (hours) | ||||
| <2 | 1 | 1 | ||
| 2 to <4 | 0.90 (0.48–1.70) | 0.743 | 0.92 (0.40–2.11) | 0.848 |
| 4 and above | 0.46 (0.18–1.22) | 0.120 | 1.10 (0.31–3.91) | 0.885 |
| Intraoperative crystalloid | 0.90 (0.72–1.11) | 0.310 | 0.71 (0.51–0.99) | 0.048 * |
| Intraoperative urine output | 0.80 (0.55–1.18) | 0.261 | 1.09 (0.68–1.76) | 0.711 |
| Morphine equivalent: intraoperative | 0.98 (0.93–1.03) | 0.429 | 1.02 (0.95–1.10) | 0.539 |
| Morphine equivalent: PACU | 1.05 (0.90–1.23) | 0.540 | 0.99 (0.81–1.22) | 0.963 |
| Morphine equivalent: Ward | 0.97 (0.90–1.04) | 0.350 | 0.98 (0.89–1.07) | 0.589 |
| No antihypertensive | 1 | 1 | ||
| One antihypertensive | 1.05 (0.62–1.79) | 0.860 | 1.33 (0.68–2.63) | 0.405 |
| Two or more antihypertensives | 1.92 (0.78–4.74) | 0.157 | 2.75 (0.83–9.13) | 0.098 |
| No antiemetic | 1 | 1 | ||
| One antiemetic | 0.89 (0.55–1.43) | 0.618 | 0.59 (0.32–1.07) | 0.082 |
| Two or more antiemetics | 0.41 (0.12–1.38) | 0.148 | 0.37 (0.08–1.80) | 0.218 |
| Without PCA | 1 | 1 | ||
| With PCA | 0.53 (0.18–1.52) | 0.235 | 0.71 (0.17–2.91) | 0.633 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsieh, C.-Y.; Poon, Y.-Y.; Ke, T.-Y.; Chiang, M.-H.; Li, Y.-Y.; Tsai, P.-N.; Wu, S.-C. Postoperative Vomiting Following Laparoscopic Cholecystectomy Is Associated with Intraoperative Fluid Administration: A Retrospective Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 5305. https://doi.org/10.3390/ijerph18105305
Hsieh C-Y, Poon Y-Y, Ke T-Y, Chiang M-H, Li Y-Y, Tsai P-N, Wu S-C. Postoperative Vomiting Following Laparoscopic Cholecystectomy Is Associated with Intraoperative Fluid Administration: A Retrospective Cohort Study. International Journal of Environmental Research and Public Health. 2021; 18(10):5305. https://doi.org/10.3390/ijerph18105305
Chicago/Turabian StyleHsieh, Chia-Yu, Yan-Yuen Poon, Ting-Yu Ke, Min-Hsien Chiang, Yan-Yi Li, Peng-Neng Tsai, and Shao-Chun Wu. 2021. "Postoperative Vomiting Following Laparoscopic Cholecystectomy Is Associated with Intraoperative Fluid Administration: A Retrospective Cohort Study" International Journal of Environmental Research and Public Health 18, no. 10: 5305. https://doi.org/10.3390/ijerph18105305
APA StyleHsieh, C.-Y., Poon, Y.-Y., Ke, T.-Y., Chiang, M.-H., Li, Y.-Y., Tsai, P.-N., & Wu, S.-C. (2021). Postoperative Vomiting Following Laparoscopic Cholecystectomy Is Associated with Intraoperative Fluid Administration: A Retrospective Cohort Study. International Journal of Environmental Research and Public Health, 18(10), 5305. https://doi.org/10.3390/ijerph18105305







