Barriers and Benefits of the Scheduled Telephone Referral Model (DETELPROG): A Qualitative Approach
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
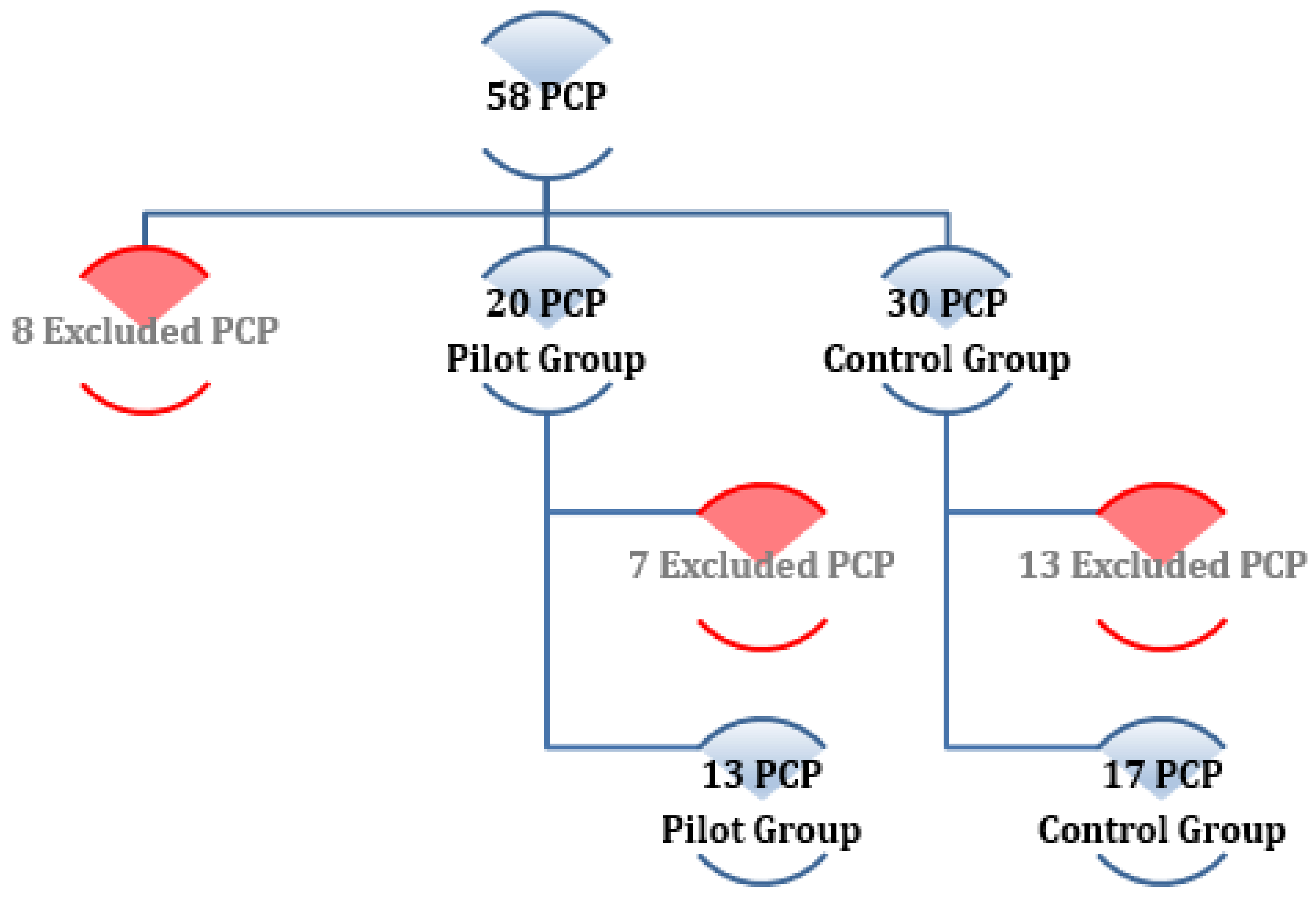
2.2. Study Population
2.3. Selection of Participants
- Inclusion criteria: Being a finite and accessible population, the study was carried out with all the members of the study population who wished to participate in it.
- Exclusion criteria: those PCP and HAP who did not participate in the DETELPROG study or any referral process.
- Key informants: They are participants who, due to the following characteristics, are interesting enough to have their opinions analysed through a semi-structured interview in a deeper way.
- o
- Key informant PCP 1: the PCP that most rejected DETELPROG (21 rejections of 36 referrals).
- o
- Key informant PCP 2: the PCP that least rejected DETELPRG (0 rejections of 14 referrals).
- o
- Key informant HAP 1 and 2: two HAP who had worked in primary care as PCP years earlier were selected for their dual perspective.
2.4. Data Collection
2.5. Barriers in Data Collection
2.6. Data Analysis
- o
- Decision making of the most appropriate type of referral.
- o
- Informed verbal and written consent.
- o
- Technical and programme characteristics for the request of the first appointment.
- o
- Communication with the HAP.
- o
- Technical details (phone, computer, …).
- o
- Interpersonal characteristics (decision making, attitudes, …).
- o
- Patient follow-up.
- o
- PCP-Patient relationship.
- o
- PCP-HAP relationship.
- Recording: interviews and focus groups were recorded in digital format with prior informed consent of the participants.
- Transcript: all recorded data were literally transcribed into a writting computerised processor.
- Comprehensive reading of texts: once the recordings were transcribed, a preliminary reading of these texts was made to correct transcription errors.
- Analysis of the contents: a semantic analysis was carried out in two phases:
- (1)
- Identification of relevant segments of the text (Encoding of transcriptions): Transcripts were encoded by 3 members of the research team, who subsequently agreed on the different categories and their final definitions (Table 2).
- (2)
- Profile analysis: Once the final categories were agreed and all recordings were transcribed, all transcripts were encoded and the transcription content analysis was performed by categories and divided by HAP and PCP profiles, with the help of the Nvivo 12 software (Table 3).
2.7. Ethical Considerations
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Azogil-López, L.M.; Pérez-Lázaro, J.J.; Ávila-Pecci, P.; Medrano-Sánchez, E.M.; Coronado-Vázquez, M.V. Effectiveness of a new model of telephone derivation shared between primary care and hospital care. Aten Primaria 2018, 51, 278–284. [Google Scholar] [CrossRef] [PubMed]
- Azogil-López, L.M.; Pérez-Lázaro, J.J.; Medrano-Sánchez, E.M.; Gómez-Salgado, J.; Coronado-Vázquez, V. DETELPROG Study. Effectiveness of a New Model of Scheduled Telephone Referral from Primary Care to Internal Medicine. A Randomised Controlled Study. J. Clin. Med. 2019, 8, 688. [Google Scholar]
- Cook, D.A.; Sorensen, K.J.; Wilkinson, J.M.; Berger, R.A. Barriers and Decisions When Answering Clinical Questions at the Point of Care. JAMA Intern. Med. 2013, 173, 1962–1969. [Google Scholar] [CrossRef] [PubMed]
- Hone, T.; Macinko, J.; Millett, C. Revisiting Alma-Ata: What is the role of primary health care in achieving the Sustainable Development Goals? Lancet 2018, 392, 1461–1472. [Google Scholar] [CrossRef]
- Junta de Andalucía. Plan de Renovación de la Atención Primaria en Andalucía. Available online: https://www.juntadeandalucia.es/organismos/sobre-junta/planes/detalle/94610.html (accessed on 18 October 2020).
- Ministerio de Sanidad y Bienestar Social. Marco Estratégico para la Atención Primaria y Comunitaria. 2019. Available online: https://www.mscbs.gob.es/profesionales/proyectosActividades/docs/Marco_Estrategico_APS_25Abril_2019.pdf (accessed on 18 October 2020).
- Blank, L.; Baxter, S.; Woods, H.B.; Goyder, E.; Lee, A.; Payne, N.; Rimmer, M. Referral interventions from primary to specialist care: A systematic review of international evidence. Br. J. Gen. Pract. 2014, 64, e765–e774. [Google Scholar] [CrossRef] [PubMed]
- Liddy, C.; Drosinis, P.; Keely, E. Electronic consultation systems: Worldwide prevalence and their impact on patient care—A systematic review. Fam. Pract. 2016, 33, 274–285. [Google Scholar] [PubMed]
- Liddy, C.; Moroz, I.; Afkham, A.; Keely, E. Sustainability of a Primary Care–Driven eConsult Service. Ann. Fam. Med. 2018, 16, 120–126. [Google Scholar] [CrossRef]
- Wrenn, K.; Catschegn, S.; Cruz, M.; Gleason, N.; Gonzales, R. Analysis of an electronic consultation program at an academic medical centre: Primary care provider questions, specialist responses, and primary care provider actions. J. Telemed. Telecare 2016, 23, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Naseriasl, M.; Adham, D.; Janati, A. E-referral Solutions: Successful Experiences, Key Features and Challenges—A Systematic Review. Mater. Soc. Med. 2015, 27, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Sanidad. Sistema de Información de Listas de Espera del Sistema Nacional de Salud. Indicadores resumen [Internet]. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/inforRecopilaciones/listaEspera.htm (accessed on 18 October 2020).
- Ministerio de Sanidad. Opinión de los Ciudadanos. Barómetro Sanitario. 2018. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/BarometroSanitario/home_BS.htm (accessed on 18 October 2020).
- Tuot, D.S.; Liddy, C.; Vimalananda, V.G.; Pecina, J.; Murphy, E.J.; Keely, E.; Simon, S.R.; North, F.; Orlander, J.D.; Chen, A.H. Evaluating diverse electronic consultation programs with a common framework. BMC Health Serv. Res. 2018, 18, 1–11. [Google Scholar]
- Liddy, C.; Drosinis, P.; Fogel, A.; Keely, E. Prevention of delayed referrals through the Champlain BASE eConsult service. Can. Fam. Phys. Med. Fam. Can. 2017, 63, e381–e386. [Google Scholar]
- Shehata, F.; Posner, G.; Afkham, A.; Liddy, C.; Keely, E. Evaluation of an Electronic Consultation Service in Obstetrics and Gynecology in Ontario. Obstet. Gynecol. 2016, 127, 1033–1038. [Google Scholar] [CrossRef] [PubMed]
- Liddy, C.; Drosinis, P.; Deri Armstrong, C.; McKellips, F.; Afkham, A.; Keely, E. What are the cost savings associated with providing access to specialist care through the Champlain BASE eConsult service? A costing evaluation. BMJ Open 2016, 6, e010920. [Google Scholar] [CrossRef] [PubMed]
- Keely, E.; Drosinis, P.; Afkham, A.; Liddy, C. Perspectives of Champlain BASE Specialist Physicians: Their Motivation, Experiences and Recommendations for Providing eConsultations to Primary Care Providers. Stud. Health Technol. Inf. 2015, 209, 38–45. [Google Scholar]
- Liddy, C.; Afkham, A.; Drosinis, P.; Joschko, J.; Keely, E. Impact of and Satisfaction with a New eConsult Service: A Mixed Methods Study of Primary Care Providers. J. Am. Board Fam. Med. 2015, 28, 394–403. [Google Scholar] [CrossRef]
- Vimalananda, V.G.; Gupte, G.; Seraj, S.M.; Orlander, J.; Berlowitz, D.; Fincke, B.G.; Simon, S.R. Electronic consultations (e-consults) to improve access to specialty care: A systematic review and narrative synthesis. J. Telemed. Telecare 2015, 21, 323–330. [Google Scholar] [CrossRef]
- Tuot, D.S.; Leeds, K.; Murphy, E.J.; Sarkar, U.; Lyles, C.R.; Mekonnen, T.; Chen, A.H.M. Facilitators and barriers to implementing electronic referral and/or consultation systems: A qualitative study of 16 health organizations. BMC Health Serv. Res. 2015, 15, 1–10. [Google Scholar] [CrossRef] [PubMed]
- A Osman, M.; Schick-Makaroff, K.; Thompson, S.; Featherstone, R.; Bialy, L.; Kurzawa, J.; Okpechi, I.G.; Habib, S.; Shojai, S.; Jindal, K.; et al. Barriers and facilitators for implementation of electronic consultations (eConsult) to enhance specialist access to care: A scoping review protocol. BMJ Open 2018, 8, e022733. [Google Scholar] [CrossRef]
- Van Der Velden, T.; Schalk, B.W.M.; Harmsen, M.; Adriaansens, G.; Schermer, T.R.; Ten Dam, M.A. Implementation of web-based hospital specialist consultations to improve quality and expediency of general practitioners’ care: A feasibility study. BMC Fam. Pract. 2019, 20, 73. [Google Scholar] [CrossRef]
- Olayiwola, J.N.; Potapov, A.; Gordon, A.; Jurado, J.; Magana, C.; Knox, M.; Tuot, D. Electronic consultation impact from the primary care clinician perspective: Outcomes from a national sample. J. Telemed. Telecare 2019, 25, 493–498. [Google Scholar] [CrossRef]
- Keely, E.; Williams, R.; Epstein, G.; Afkham, A.; Liddy, C. Specialist Perspectives on Ontario Provincial Electronic Consultation Services. Telemed. e-Health 2019, 25, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Joschko, J.; Keely, E.; Grant, R.; Moroz, I.; Graveline, M.; Drimer, N.; Liddy, C. Electronic Consultation Services Worldwide: Environmental Scan. J. Med. Internet Res. 2018, 20, e11112. [Google Scholar] [CrossRef] [PubMed]
- Liddy, C.; Moroz, I.; Mihan, A.; Nawar, N.; Keely, E. A Systematic Review of Asynchronous, Provider-to-Provider, Electronic Consultation Services to Improve Access to Specialty Care Available Worldwide. Telemed. e-Health 2019, 25, 184–198. [Google Scholar] [CrossRef] [PubMed]
- Burden, M.; Sarcone, E.; Keniston, A.; Statland, B.; Taub, J.A.; Allyn, R.L.; Reid, M.B.; Cervantes, L.; Frank, M.G.; Scaletta, N.; et al. Prospective comparison of curbside versus formal consultations. J. Hosp. Med. 2013, 8, 31–35. [Google Scholar] [CrossRef]
- Cook, D.A.; Sorensen, K.J.; Wilkinson, J.M. Value and Process of Curbside Consultations in Clinical Practice: A Grounded Theory Study. Mayo Clin. Proc. 2014, 89, 602–614. [Google Scholar] [CrossRef] [PubMed]
- Denes, E.; Pinet, P.; Cypierre, A.; Durox, H.; Ducroix-Roubertou, S.; Genet, C.; Weinbreck, P. Spectrum of advice and curbside consultations of infectious diseases specialists. Méd. Maladies Infect. 2014, 44, 374–379. [Google Scholar] [CrossRef]
- Sarcone, E.; Stella, S.A.; Allyn, R. Curbside consultations: A call for more investigation into a common practice. Mayo Clin. Proc. 2014, 89, 1589–1590. [Google Scholar] [CrossRef]
- Cook, D.A.; Sorensen, K.J.; Wilkinson, J.M. In reply—Curbside consultations: A call for more investigation into a common practice. Mayo Clin. Proc. 2014, 89, 1590. [Google Scholar] [CrossRef]
- Wadhwa, A.; Lingard, L. A qualitative study examining tensions in interdoctor telephone consultations. Med. Educ. 2006, 40, 759–767. [Google Scholar] [CrossRef]
- Wilson, M.; Mazowita, G.; Ignaszewski, A.; Levin, A.; Barber, C.; Thompson, D.; Barr, S.; Lear, S.; Levy, R.D. Family physician access to specialist advice by telephone: Reduction in unnecessary specialist consultations and emergency department visits. Can. Fam. Phys. Med. Fam. Can. 2016, 62, e668–e676. [Google Scholar]
- Fortney, J.C.; Pyne, J.M.; Turner, E.E.; Farris, K.M.; Normoyle, T.M.; Avery, M.D.; Hilty, D.M.; Unützer, J. Telepsychiatry integration of mental health services into rural primary care settings. Int. Rev. Psychiatry 2015, 27, 525–539. [Google Scholar] [CrossRef] [PubMed]
- Johansson, A.M.; Lindberg, I.; Söderberg, S. Healthcare personnel’s experiences using video consultation in primary healthcare in rural areas. Prim. Health Care Res. Dev. 2016, 18, 73–83. [Google Scholar] [CrossRef]
- Ministerio de la Presidencia del gobierno de España. BOE.es—BOE-A-1999-23750 Ley Orgánica 15/1999, de 13 de diciembre, de Protección de Datos de Carácter Personal. [Internet]. Boletin oficial del estado. 1999. Available online: https://www.boe.es/buscar/act.php?id=BOE-A-1999-23750 (accessed on 6 April 2021).
- Ministerio de la Presidencia del gobierno de España. BOE.es—BOE-A-1999-13967 Real Decreto 994/1999, de 11 de junio, por el que se aprueba el Reglamento de medidas de seguridad de los ficheros automatizados que contengan datos de carácter personal. [Internet]. Boletin oficial del estado. 1999. Available online: https://www.boe.es/buscar/doc.php?id=BOE-A-1999-13967 (accessed on 6 April 2021).
- Myers, J.P. Curbside Consultation in Infectious Diseases: A Prospective Study. J. Infect. Dis. 1984, 150, 797–802. [Google Scholar] [CrossRef] [PubMed]
- Kuo, D.; Gifford, D.R.; Stein, M.D. Curbside Consultation Practices and Attitudes Among Primary Care Physicians and Medical Subspecialists. JAMA 1998, 280, 905–909. [Google Scholar] [CrossRef] [PubMed]
- Rappolt, S. Family physicians’ selection of informal peer consultants: Implications for continuing education. J. Contin. Educ. Health Prof. 2002, 22, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Lattimer, V.; George, S.; Thompson, F.; Thomas, E.; Mullee, M.; Turnbull, J.; Smith, H.; Moore, M.; Bond, H.; Glasper, A. Safety and effectiveness of nurse telephone consultation in out of hours primary care: Randomised controlled trial. BMJ 1998, 317, 1054–1059. [Google Scholar] [CrossRef] [PubMed]
- Campbell, J.L.; Fletcher, E.; Britten, N.; Green, C.; A Holt, T.; Lattimer, V.; Richards, D.; Richards, S.H.; Salisbury, C.; Calitri, R.; et al. Telephone triage for management of same-day consultation requests in general practice (the ESTEEM trial): A cluster-randomised controlled trial and cost-consequence analysis. Lancet 2014, 384, 1859–1868. [Google Scholar] [CrossRef]
- Bodenheimer, T.; Sinsky, C. From Triple to Quadruple Aim: Care of the Patient Requires Care of the Provider. Ann. Fam. Med. 2014, 12, 573–576. [Google Scholar] [CrossRef]
| Sociodemographic Characteristics | PCP (n = 11) | HAP (n = 5) |
|---|---|---|
| Sex n (%) Male Female | 5 (45.45%) 6 (54.55%) | 3 (60%) 2 (40%) |
| Age in years Minimum-Maximum Mean (CI 95%) | 37–66 54.55 (47.31-61.78) | 45–67 57.4 (46–68.8) |
| Work experience in years Minimum-Maximum Mean (CI 95%) | 8–36 22.27 (15.97–28.58) | 19–4132 (20.22–43.78) |
| Years in the same office at the beginning of the DETELPROG Minimum-Maximum Mean (CI 95%) | 0–36 8.64 (1.34–15.93) | 1–30 15.20 (1.73–28.67) |
| Distance to hospital in kilometres Minimum-Maximum Mean (CI 95%) | 36 (±11) | - |
| Number of healthcare cards adjusted by age Minimum-Maximum Mean (CI 95%) | 845–2679 1.756 (1330–2181) | - |
| Number of referrals in 2014 Minimum-Maximum Mean (CI 95%) | 7–59 32.45 (20.62–44.29) | - |
| Rurality index Minimum-Maximum Mean (CI 95%) | −1.09/−0.1 −0.60 (−0.86/−0.32) | - |
| Categories | Definitions |
|---|---|
| Primary Care Physicians as key axis | Feeling of giving the PCP a more key role in decision-making regarding the health of their patients, even in the hospital environment |
| Lack of available tests in primary care | As a cause of the DETELPROG’s success is the scarce tests catalogue available for PC, that allows expanding when agreed with the Hospital Attending Physicians. |
| Comparison with other types of referral | Comments and comparisons with other types of already experienced PC-hospital referral/contact (face-to-face referral, mail, non-scheduled telephone consultation…) |
| General qualitative assessment | General assessment and satisfaction of participants |
| Proposals for improvement | Proposals for improvements made by participants. |
| Ethical-legal implications | Doubts raised about ethical-legal issues |
| Causes for refusing-accepting DETELPROG | Patients and consultations characteristics, or any other type of characteristic that makes the PCP refuse DETELPROG or use it instead of face-to-face referral. |
| Positive or negative characteristics regarding: | |
| PCP-HAP relationship | Characteristics that modify the professional relationship between Primary Care Physicians and Hospital Attending Physicians |
| Physician-patient relationship | Characteristics affecting the PCP-patient relationship |
| Planning DETELPROG | Facilities or problems that have been raised since PCP considered referring the patient until the beginning of the telephone consultation (Planning suitability of the said referral method, informed consent of the patient, planning the day when the telephone consultation will take place, planning the telephone consultation with their workmate). |
| Quantitative improvements | Improvement of quantitative variables: waiting times, commuting, waiting lists, capacity to assist more/less patients. |
| Communication PCP-HAP-patient | Benefits and problems in telephone communication between PCP-HAP-patient (attitudes, agreement and disagreement on complementary tests, treatment, follow-up, revision, advice, quality of information, reliability of information, information record). |
| Organisational characteristics | Any characteristic that depends on DETELPROG organisation (initial training phase/prior preparation of participants, schedule organisation -time and duration-, work overburden, consultation protocolisation…). |
| Technical characteristics | Telephone performance, computer and software performance (access to patients’ medical history, complementary tests, consultation mode…) |
| Category | Verbatim |
|---|---|
| 1. Primary Care Physicians as key axis | “…the family physician increases his or her importance, his or her relevant role, increases decision-making; and, in the end, increases everything by, somehow, assuming more responsibility, though this was advised, agreed, etc., but the family physician becomes an even more relevant key axis in health care…” (key informant HAP 1) |
| 2. Lack of available tests in primary care | “…Before HAP, I was a general physician here in Huelva and my training had dealt with hospital care right after finishing my degree, and I properly knew what to do. The thing is, I didn’t have the appropriate means. So, I suppose… that would be the issue, knowing what to do but having no means available… (key informant HAP 2) “…and then, something basic has been achieved, that is avoiding one step if we, primary care physicians, had the chance to request those complementary tests, more than 90% would be avoided...” (PCP focal group) |
| 3. Comparison with other types of referral | |
| 3.1 Immediate telephone call | “it was a somehow simpler consultation; I would say ‘I’ll request the CAT scan’, and then I would write: ‘The family physician is requesting a CAT scan, I find no contraindications so, I accept’, and everything was somewhat less informed because the family physician requested I prescribed a CAT scan, and the information I received was more or less sensible so I agreed but, well…” (HAP key informant 1) |
| 3.2 E-consultation | “…it has been a long wait because one doesn’t know whether the person is available, maybe on holidays, or off-work or on leave… This happened to me, and then, I received the answer a month later. Also, you don’t feel so much at ease; the questions you may be asked by the specialist regarding the patient, maybe through an online question I write a series of data but there are still some missing that, in face-to-face communication, I would be able to better clarify…” (PCP) |
| 4. General qualitative assessment | “My subjective feeling and that of my patients, which I can communicate to this group, is that it has been a highly positive experience, that is, the patient, as the introduction says, has had improvements in terms of time; he/she has been assisted earlier, has gained in comfortability, not only thanks to avoiding commuting to hospital, but also because the first consultation has been done in front of their family physician, who usually holds a much more intimate relationship with the patient than other specialists they don’t know”. (PCP focal group) “Very useful. I think this is already assumed; it is much more convenient and I would like this type of systems to be implemented. I feel more confident and at ease when contacting that person, having direct contact”. (PCP) “I serve as support, a good one that must be regarded as positive because this supportive element may save lives, but in certain circumstances, on the contrary, you may have overseen some issue and the patient would have benefited more from a face-to-face consultation despite this being a month and a half later in time; we must also be aware of this…” (HAP key informant 1) |
| 5. Ethical-legal implications | “when you refer somebody to hospital, it is like you are getting rid of them, and then the hospital “internist” or specialist is in charge of their health or of that specific problem the patient has. However, this way, well, you can share the patient and the internist is not the sole responsible, but you are instead”. (PCP key informant 2) “…the responsibility is shared, and I’ll let you know why: from the very moment you start telling a hospital specialist about the patient, their history, medication and physical exploration, if that physician does not want to take care of the patient, he/she says, look, this patient…” (PCP focal group) “I must confess that, when this happened, I would say: ‘virtual consultation’, so that later on the fact that I didn’t physically see the patient would be known, that it was a telephone consultation and I had followed what my colleague from PC said, so it is true that I tended to say ‘better safe than sorry’, look, I did what I could by telephone…”. (HAP focal group) “so, obviously, there is a responsibility on the part of PCP, as I was saying, to accept these tests for their patient, but also, there is written responsibility that I requested the test so, if something goes wrong, if there is any negative effect, and the patient demands some explanation, this will go to the physician who requested the test, who hasn’t spoke to the patient, doesn’t know the patient…” (HAP key informant 1) |
| 6. PCP- HAP relationship | “E3: It is not significant. The volume of consultations was not significant for that… E2: It was irregular”. (HAP focal group). “I think so, I think this strengthens the relationship, for example, physician Morales I didn’t know her, and she is so kind and collaborative in every way, and I believe this strengthens the relationship, sure”. (PCP) |
| 7. Physician-patient relationship | “…when answering a telephone consultation, obviously, you cannot see the patient, that is completely out of sight to favour diagnostic speed, which is the actual interest, helping the patient as swiftly as possible…” (HAP key informant 1) “…it was like patients regarded you as something important, that is, as if in hospital you were more valuable and they agreed on opinions that had already been expressed to the patient and on which internists also agreed… What I experienced was an important improvement of the physician-patient relationship”. (PCP key informant 2) |
| 8. Planning DETELPROG | “That is the only thing to change, some appointments, because they were finishing their on-call or they coincided with the specialist’s, which had been on-call as well. That is the only occasion in which we have had to change any appointment… In general, everything was properly done”. (PCP) “No, no. I believe I have a certain amount of experience at the clinical level and, overall, I am able to identify pathologies and solve the issue but, no, for instance, when you receive results and you have to analyse them and revise everything, yes…” (HAP key informant 2) |
| 9. Quantitative improvements | “…one thing has mainly been gained, that is avoiding a step if we, primary care physicians, had the chance to request those complementary tests, this would avoid more than 90%...” (PCP focal group) “…everything was quite swiftly done…”. (PCP key informant 2) |
| 10. PCP-HAP-patient communication | |
| 10.1 Quality and quantity | “I believe that the family physician is quite enriching as when a patient is referred, you are lacking some data and the family physician does know the patient and, even sometimes, their family interrelationship, so there is a bunch of data that are not usually reported through written means but which, at the communication level, are even much more enriching, I would even say that this previous contact is quite enriching”. (HAP key informant 1). “…always, when talking to another person, be it even via phone call, communication is more fluent than what can be said in a written document, which is usually more objective information and, mainly because of time issues, also more limited”. (PCP key informant 1) |
| 10.2 Reliability | “You are not told about the patient the same way depending on who gives you the report. In the end, you opt for requesting an abdominal ultrasound and requesting a consultation”. (HAP focal group). “…there is still a somehow uneasy feeling that I haven’t auscultated the patient, explored them, and I must only assume the data given by the PCP”. (HAP key informant 1) |
| 10.3 Agreements | “E3: This is positive as the first days I request, and then, ‘how do we do it?’, ‘wait till I get informed’, ‘I think I kept the colleague’s phone number and Mari Ángeles, the assistant… (agreement on that). E2: But well, we did it like that, the first ones we referred them to the family physician with the signature and then, the last ones, we signed them here. If anybody wanted a test request or whatever, you would do so, if it was a special coding, and the test would be sent from here and the ultrasound examinations requests were done through the X-rays department and the appointment was programmed as if it had been done face-to-face”. E3: A record is sent, as if the patient were face-to-face, their record… E1: this is why you didn’t encounter any problem, right? E3: No… E2: Each one gave their best, right. (HAP focal group) |
| 10.4 Attitudes | “…at the beginning there were some physicians or internists who were not willing to collaborate much, and we all know who we are referring to. So, this is an issue, lack of collaboration… for me myself and my circumstances…”. “Somehow sardonically they would say “virtual consultation” … At the beginning, internists were skeptical, that a secretary, a virtual model… It was not much heard at the moment but, little by little, they started taking it more seriously…”. (PCP focal group) |
| 11. Organisational characteristics | |
| 11.1 Preparation phase | “E3:…with the problem that you don’t know the interlocutor you are talking to, one gives it for granted that we, physicians, all have the same training… E1: that is questionable. E3: Well, that is why it also depends on who is talking to you in the interconsultation…” (HAP focal group) |
| 11.2 Telephone consultation schedule | “Sometimes it occurred … that nobody answered the phone and the patient needed to go out of the office and wait for some minutes and, then, a quarter of an hour later while I was receiving other patients, we tried again and they answered… no appointment had to be canceled, it just took a bit longer… I received some more patients and, at the second try, it was solved”. (PCP key informant 1) |
| 11.3 Time set for consultation | “As for the consultation times, it was 15 min; do you find it appropriate? “Yes, yes, absolutely”. (PCP key informant 1) |
| 11.4 PCP work overburden | “maybe a bit of overburden for us who, instead of passing the patient over, we need to be more present and aware of what is happening in the medical history but, well, this is our job and what I like doing so, this overburden is not such…” (PCP key informant 2) |
| 11.5 Prior protocols | “…it would be to, somehow, establish the assessment of, somehow, how to put everything together, all the available means and everything we can do to reach a consensus, that is, an appropriate method. Establishing protocols”. (HAP key informant 2) |
| 12. Technical characteristics | “E1: Did you find any problem with telephone communication at the technological level, other from the one we already identified? E3: What I said before about changing room to answer the phone, but it was eventually solved… E2: no, no…”. (HAP focal group) |
| 13.Causes for refusing-accepting DETELPROG | |
| 13.1 Accepting | “This is for standard and easy issues, telephone consultation. For very specific minor issues.” (HAP focal group) “PCP-HAP communication, I believe there would be no a priori limitations. I think that updated and live communication where the family physician explains to the specialist the patient’s circumstance, a priori, the patient’s characteristics may not imply any limitation to reject the telephone consultation”. (HAP key informant 1) “I don’t think so, as telephone communication is simple and direct, and the patient may even be prevented from having to commute to hospital and, if the patient trusts the assisting physician, they will absolutely delegate to him/her”. (PCP key informant 1) |
| 13.2 Refusing | |
| 13.2.1 HAP | “You are not told about the patient in the same way, depending on the physician, and this is highly influential. You eventually end up requesting an abdominal ultrasound and setting an appointment”. “Older more complex patients or not so old but complex imply many nuances that are difficult to solve in a consultation, difficult to leave it solved, or I find it difficult unless both the PC physician and the specialist know the patient, that both know what the issue is about… that way, it could be possible”. “if I don’t know the patient’s issue, I don’t know how to explain if this is a bruise, or Velcro, or crackles. So, this must be seen by the internist… or if it is a skin condition whose origin I don’t identify and may be related to a more general disease…”. (PCP) |
| 13.2.2 PCP | “If I don’t know the patient’s issue, I don’t know how to explain if this is a bruise, or Velcro, or crackles. So, this must be seen by the internist… or if it is a skin condition whose origin I don’t identify and may be related to any more general disease…”. (PCP) “In some odd case with a patient, being critical of myself, maybe due to my own feeling of responsibility, I think, I will make a mistake, not meet expectations…”. (PCP focal group) “Due to the shortage of time we’ve got, we don’t get rid of the patient because, the good point of referral is that you say ‘I’ll refer you to internal medicine, and they’ll take care of you, one less issue to care about, because I don’t have more time but, well… The downside would be that one, it is extra work added to what already is a quite complex schedule and agenda regarding times”. (PCP key informant 1) |
| Benefits | PCP | HAP |
|---|---|---|
| Promotes PCP prominence as coordinator of their patients’ health problems | Repeated opinion | Repeated opinion |
| Improves availability of complementary tests for PCP | Repeated opinion | Repeated opinion |
| Avoids barriers for immediate telephone consultation | Repeated opinion | Repeated opinion |
| Works better than email consultations | Repeated opinion | Not expressed |
| General satisfaction | Very good | Good |
| Improves PCP-patient relationship | Repeated opinion | Not assessable |
| Improves PCP-HAP relationship | Repeated opinion | Repeated opinion |
| Improves information given to HAP | Repeated opinion | Repeated opinion |
| Perception of improvement regarding waiting days | Repeated opinion | Not expressed |
| Appropriate organisation for better DETELPROG | Repeated opinion | Repeated opinion |
| Adequate technical characteristics | Repeated opinion | Repeated opinion |
| Utility for a great majority of present-day referrals | Repeated opinion | Repeated opinion |
| BARRIERS | ||
| No utility for certain patients | Distrustful patients, patients who don’t know how to focus, referrals when assistance is in high pressure moments | Patients wrongly directed by PCP, distrust in PCP, considering PCP not skilled to control the patient’s problem |
| Ethic-legal doubts | No doubts | Doubts |
| Worsens HAP-patient relationship | Not assessable | Repeated opinion |
| Certain insecurity of HAP for not meeting patients | Not assessable | Repeated opinion |
| Barriers | Proposal for Improvement |
|---|---|
| When Primary Care Physicians called at the appointed time, Hospital Attending Physicians were busy with a face-to-face consultation | “I think the ideal would be to establish a fixed time to finish consultations and during which the physician would only be available in a relaxed atmosphere, concentrated and prepared in front of the computer, without carrying out any other activity, just being attentive to telephone consultations…”. |
| Issues regarding verbal explanation of the complementary tests consents | “the only way is for the family physician to have the requests in their office and, thus, be able to note down what has been consulted and agreed with the specialist, in some way”. (HAP key informant 1) |
| Responsibilities regarding patients’ follow-up | “I think the family physician needs to take up a preponderant role as they are in close contact with the patient… The specialist needs to review the tests... there would be clear issues, such as the patient having a neoplasm of the colon because, as in the case I was reporting before, a neoplasm of the colon… referring the patient to surgery or the corresponding specialist”. “…the close relationship between the family physician and the patient, well, maybe the simplest answer from the family physician would be ‘When you undergo the colonoscopy, come over here and let me know, and this way this close relationship would even favour a quick diagnosis”. (HAP key informant 1) |
| Lack of reliability in the information provided by Primary Care Physicians to Hospital Attending Physicians | “I think we should better know the physicians we count on in primary care before implementing something like this, so that we know who we are actually working with”. (HAP focal group) |
| “maybe differentiating by sectors… perhaps the Valverde health centre, has such person as reference, or in Aracena health centre, so-and-so is the referred internist, that is what is sought today… Then, communication would improve as the 7 or 8 physicians of the area would know their reference internists…”. (HAP key informant 1) | |
| Quality of information in telephone communication | “…it would be, somehow, establishing the assessment about how to put everything together in some way, all the available means and everything we can do to reach a consensus, that is, an appropriate method. Establishing protocols”. (HAP key informant 2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Azogil-López, L.M.; Coronado-Vázquez, V.; Pérez-Lázaro, J.J.; Gómez-Salgado, J.; Medrano-Sánchez, E.M. Barriers and Benefits of the Scheduled Telephone Referral Model (DETELPROG): A Qualitative Approach. Int. J. Environ. Res. Public Health 2021, 18, 5280. https://doi.org/10.3390/ijerph18105280
Azogil-López LM, Coronado-Vázquez V, Pérez-Lázaro JJ, Gómez-Salgado J, Medrano-Sánchez EM. Barriers and Benefits of the Scheduled Telephone Referral Model (DETELPROG): A Qualitative Approach. International Journal of Environmental Research and Public Health. 2021; 18(10):5280. https://doi.org/10.3390/ijerph18105280
Chicago/Turabian StyleAzogil-López, Luis Miguel, Valle Coronado-Vázquez, Juan José Pérez-Lázaro, Juan Gómez-Salgado, and Esther María Medrano-Sánchez. 2021. "Barriers and Benefits of the Scheduled Telephone Referral Model (DETELPROG): A Qualitative Approach" International Journal of Environmental Research and Public Health 18, no. 10: 5280. https://doi.org/10.3390/ijerph18105280
APA StyleAzogil-López, L. M., Coronado-Vázquez, V., Pérez-Lázaro, J. J., Gómez-Salgado, J., & Medrano-Sánchez, E. M. (2021). Barriers and Benefits of the Scheduled Telephone Referral Model (DETELPROG): A Qualitative Approach. International Journal of Environmental Research and Public Health, 18(10), 5280. https://doi.org/10.3390/ijerph18105280







