Assessing Factors Associated with TB Awareness in Nepal: A National and Subnational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Data-In-Use
2.2. Outcome Variables and Covariates
2.3. Statistical Analysis
3. Results
3.1. Summary of Socio-Demographic Characteristics of Respondents
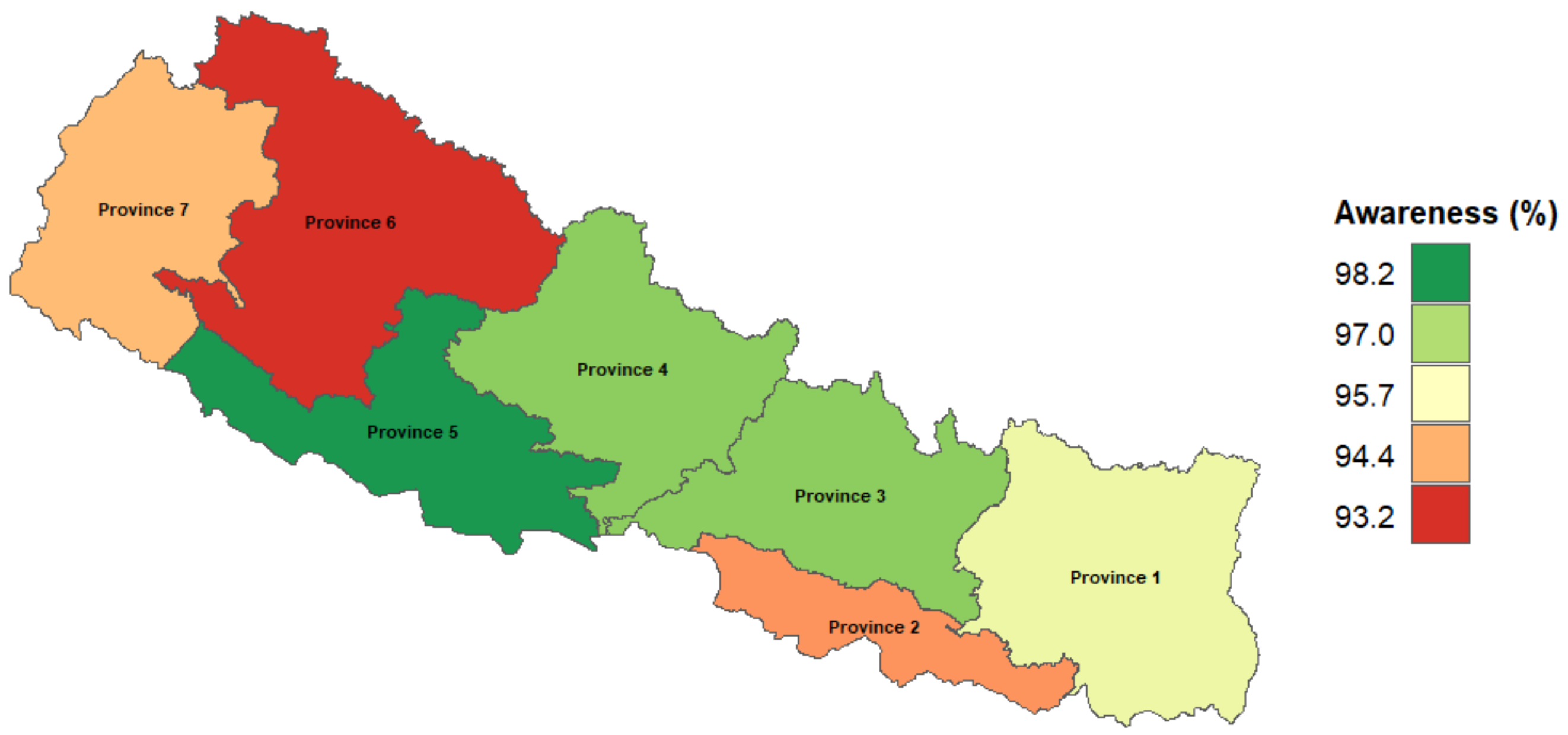
3.2. Proportion of People with TB Awareness at a Subnational Level in Nepal
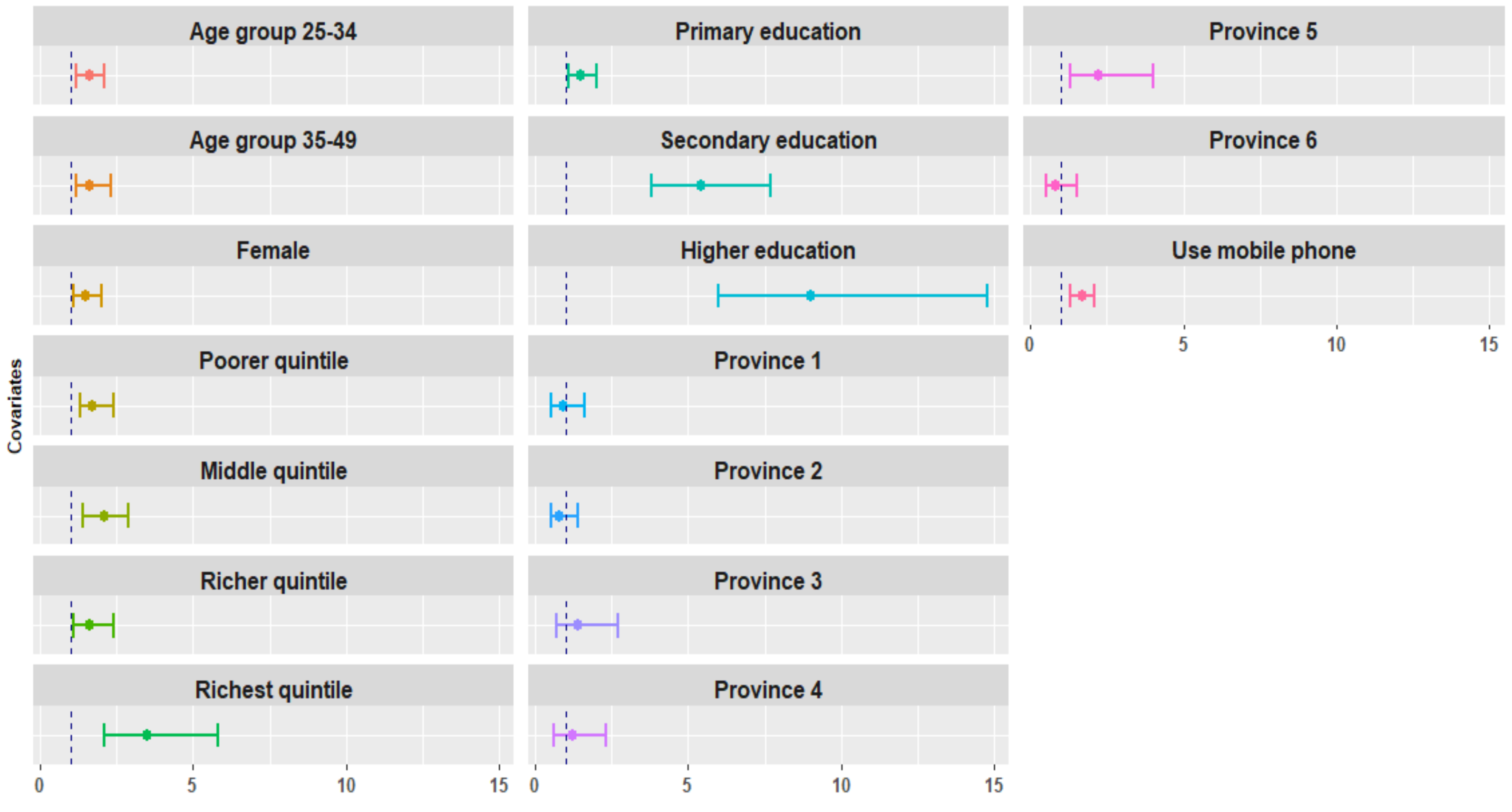
3.3. Variables Associated with TB Awareness
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Proportion (95% Confidence Interval) | |
|---|---|
| TB Awareness | |
| Province 1 (Not determined) | 96.1 (95.3–96.7) |
| Province 2 (Not determined) | 94.1 (93.3–94.9) |
| Province 3 (Bagmati) | 97.4 (96.9–97.9) |
| Province 4 (Gandagi) | 97.4 (96.5–98.1) |
| Province 5 (Lumbini) | 98.1 (97.6–98.6) |
| Province 6 (Karmali) | 93.2 (91.3–94.6) |
| Province 7 (Sudurpashchim) | 94.5 (93.2–95.6) |
Appendix B
References
- World Health Organization (WHO). Global Tuberculosis Programme 1994. TB: A Global Emergency, WHO Report on the TB Epidemic. Available online: https://apps.who.int/iris/handle/10665/58749 (accessed on 28 January 2021).
- WHO. Global Tuberculosis Report 2020. Available online: https://apps.who.int/iris/bitstream/handle/10665/336069/9789240013131-eng.pdf (accessed on 14 October 2020).
- Yadav, S. A new concept in tuberculosis awareness in the low-income countries. Edorium J. Tuberc. 2015, 1, 1–4. [Google Scholar]
- Narayan, B. Tuberculosis in India: A need of Public Awareness & Education. Univ. Maurit. Res. J. 2015, 21, 1–27. [Google Scholar]
- Desalu, O.O.; Adeoti, A.O.; Fadeyi, A.; Salami, A.K.; Fawibe, A.E.; Oyedepo, O.O. Awareness of the Warning Signs, Risk Factors, and Treatment for Tuberculosis among Urban Nigerians. Tuberc. Res. Treat. 2013, 2013, 369717. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gurp, M.G.; Rood, E.; Fatima, R.; Joshi, P.; Verma, S.H.; Khan, A.H.; Blok, L.; Mergenthaler, C.; Bakker, I. Finding gaps in TB notifications: Spatial analysis of geographical patterns of TB notifications, associations with TB program efforts and social determinants of TB risk in Bangladesh, Nepal and Pakistan. BMC Infect. Dis. 2020, 20, 490. [Google Scholar]
- Samal, J. Health Seeking Behaviour among Tuberculosis Patients in India: A Systematic Review. J. Clin. Diagn. Res. 2016, 10, 1–6. [Google Scholar] [CrossRef]
- National Tuberculosis Center, Department of Health Services, Ministry of Nepal. National Strategic Plan for Tuberculosis Prevention, Care and Control 2016–2021. January 2018. Available online: https://nepalntp.gov.np/wp-content/uploads/2018/01/NSP-report-english-revised.pdf (accessed on 3 February 2021).
- National TB Control Center, Ministry of Health and Population, Government of Nepal. TB Burden in Nepal. 24 March 2020. Available online: https://www.who.int/docs/default-source/nepal-documents/policy-brief.pdf?sfvrsn=37b5881c_2 (accessed on 3 February 2021).
- National Tuberculosis Center, Department of Health Services, Ministry of Nepal. National Tuberculosis Management Guidelines 2019. Available online: https://nepalntp.gov.np/wp-content/uploads/2019/10/National-Tuberculosis-Management-Guidelines-2019_Nepal.pdf (accessed on 3 February 2021).
- Huddart, H.; Bossury, T.; Pons, V.; Baral, S.; Pai, M.; Delavallade, C. Knowledge about tuberculosis and infection prevention behavior: A nine city longtuginal study in India. PLoS ONE 2018, 13, e0206245. [Google Scholar] [CrossRef]
- Naidoo, P.; Simbayi, L.; Labadarios, D.; Ntsepe, Y.; Bikitsha, N.; Khan, G.; Sewpaul, R.; Rehle, T. Predictors of knowledge about tuberculosis: Results from SANHANES I, a national, cross-sectional household survey in South Africa. BMC Public Health 2016, 276, 276. [Google Scholar] [CrossRef]
- Khan, A.; Shaikh, B.T.; Bain, M.A. Knowledge, Awareness, and health seeking behavior regarding TB in Rural district of Khyber Pakhtunkhwa, Pakistan. BioMed Res. Int. 2020. [Google Scholar] [CrossRef]
- Paul, S.; Akter, R.; Aftab, A.; Khan, A.M.; Barua, M.; Islam, S.; Islam, A.; Husain, A.; Sarker, M. Knowledge and attitude of key community members towards tuberculosis: Mixed method study from BRAC TB control areas in Bangladesh. BMC Public Health 2015, 15, 52. [Google Scholar] [CrossRef]
- Mishra, P.; Hansen, E.H.; Kafle, K.K. Socio-economic status and adherence to tuberculosis treatment: A case-control study in a district of Nepal. Int. J. Tuberc. Lung Dis. 2005, 9, 1134–1139. [Google Scholar]
- Ten Asbroek, A.H.; Bijlsma, M.W.; Malla, P.; Shrestha, B.; Delnoij, D.M.J. The road to tuberculosis treatment in rural Nepal: A qualitative assessment of 26 journeys. BMC Health Serv. Res. 2008, 8, 7. [Google Scholar] [CrossRef]
- Christian, C.; Burger, C.; Claassens, M.; Bond, V.; Burger, R. Patient predictors of health-seeking behaviour for persons coughing for more than two weeks in high-burden tuberculosis communities: The case of the Western Cape, South Africa. BMC Health Serv. Res. 2019, 160, 160. [Google Scholar] [CrossRef]
- Ministry of Health Ramshah Path, Kathmandu Nepal. Nepal Demografic and Health Survey (NHDS) 2016. Available online: https://www.dhsprogram.com/pubs/pdf/fr336/fr336.pdf (accessed on 1 February 2021).
- WHO. End TB Strategy. Available online: https://www.who.int/tb/strategy/End_TB_Strategy.pdf (accessed on 16 February 2021).
- Li, J.; Chung, P.H.; Leung, C.L.K.; Nishikiori, N.; Chan, E.Y.Y.; Yeoh, E.K. The strategic framework of tuberculosis control and prevention in the elderly: A scoping review towards End TB targets. Infect. Dis. Poverty 2017, 6, 70. [Google Scholar] [CrossRef]
- Rauniyar, S.K.; Rahman, M.M.; Rahman, M.S.; Abe, S.K.; Nomura, S.; Shibuya, K. Inequalities and risk factors analysis in prevarence and management of hypertension in India and Nepal: A national and subnational study. BMC Public Health 2020, 20, 1341. [Google Scholar] [CrossRef]
- Government of Nepal, Ministry of Health and Population Department of Health Services, National Tuberculosis Control Centre. National TB Prevalence Survey 2018/2019. Available online: http://impacttbproject.org/wp-content/uploads/2020/03/TBPS%20Summary%20Report_English_Final_21%20March%202020.pdf (accessed on 3 February 2021).
- Government of Nepal, Ministry of Health and Population Department of Health Services. National Tuberculosis Program Nepal Annual Report 2075/76 (2018/19). Available online: https://nepalntp.gov.np/wp-content/uploads/2020/04/NTP-Annual-Report-2075-76-2018-19.pdf (accessed on 1 February 2021).
- Marahhata, S.B.; Yadav, R.Y.; Giri, D.; Lama, S.; Rijal, K.R.; Mishra, S.R.; Shrestha, A.; Bhattrai, P.R.; Mahato, R.K.; Adhikari, B. Barriers in the access, diagnosis and treatment completion for tuberculosis patients in central and western Nepal: A qualitative study among patients, community members and health care workers. PLoS ONE 2020, 15, e0227293. [Google Scholar]
- Oxlade, O.; Murray, M. Why Are the Poor at Greater Risk in India? PLoS ONE 2012, 7, e0047533. [Google Scholar] [CrossRef]
- Adhikari, N.; Joshi, L.R.; Subedi, B.; Acharya, D.; Adhikari, M.; Thapa, P.; Sultana, R.; Karki, K.B. Tuberculosis in Nepal: Situation, Challenges and Ways Forward. SAARC J. Tuberc. Lung Dis. HIV/AIDS 2019, 17, 34–40. [Google Scholar] [CrossRef]
- Asian Development Bank. Country Poverty Analysis Nepal 2011. Available online: https://www.adb.org/countries/nepal/poverty (accessed on 1 February 2021).
- International Telecommunication Union (ITU). Global ICT Development Index 2017. Measuring the Information Society Report 2017. Available online: https://www.itu.int/en/ITU-D/Statistics/Pages/publications/mis2017.aspx (accessed on 1 February 2021).
- Laster, R.; Park, J.J.H.; Molten, L.M.; Enjetti, A.; Johnston, J.M.; Schwartzman, K.; Tilahun, B.; Delft, A.V. Mobile phone short message service for adherence support and care of patients with tuberculosis infection: Evidence and opportunity. J. Clin. Tuberc. Other Mycobact. Dis. 2019, 16, 100108. [Google Scholar] [CrossRef]
- Choun, K.; Achanta, S.; Naik, B.; Tripathy, J.P.; Thai, S.; Lorent, N.; Khun, K.E.; Griensven, J.V.; Kumar, A.M.V.; Zachariah, R. Using mobile phones to ensure that referred tuberculosis patients reach their treatment facilities: A call that makes a difference. BMC Public Health 2017, 17, 575. [Google Scholar] [CrossRef][Green Version]
- GSMA Intelligence. Accelerating Affordable Smartphone Ownership in Emerging Markets 2017. Available online: https://www.gsma.com/mobilefordevelopment/wp-content/uploads/2018/08/Accelerating-affordable-smartphone-ownership-in-emerging-markets-2017_we.pdf (accessed on 28 February 2021).
- Lee, V.L.; Ho, M.; Kai, C.W.; Aguilera, X.; Wilder-Smith, A. Epidemic preparedness in urban settings: New challenges and opportunities. Lancet 2020, 20, 527–529. [Google Scholar] [CrossRef]
- Nomura, S.; Siesjo, V.; Tomson, G.; Mohr, W.; Fukuchi, E.; Shibuya, K.; Tangcharoensathien, V.; Miyata, H. Contributions of information and communications technology to future health systems and Universal Health Coverage: Application of Japan’s experiences. Health Res. Policy Syst. 2020, 18, 73. [Google Scholar] [CrossRef] [PubMed]
- Japan International Cooperation Agency (JICA). Project report of Tuberculosis and Pulmonary Health Project in Nepal 2005. Available online: https://openjicareport.jica.go.jp/986/986/986_116_11831963.html (accessed on 1 February 2021).
- JICA. Outline of Cooperation in Nepal 2019. Available online: https://www.jica.go.jp/nepal/english/office/others/c8h0vm00009vyd39-att/brochure_12.pdf (accessed on 1 February 2021).
| Characteristics | Number | Proportion (%) |
|---|---|---|
| Total | 16,672 | 100 |
| Gender | ||
| Male | 3978 | 23.9 |
| Female | 12,694 | 76.1 |
| Age group | ||
| 15–24 | 6424 | 38.5 |
| 25–34 | 4991 | 29.9 |
| 35–49 | 5257 | 31.6 |
| Educational attainment | ||
| No formal education | 4534 | 27.2 |
| Primary education | 2889 | 17.3 |
| Secondary education | 6459 | 38.8 |
| Higher education | 2790 | 16.7 |
| Province | ||
| Province 1 (Not determined) | 2826 | 17.0 |
| Province 2 (Not determined) | 3323 | 19.9 |
| Province 3 (Bagmati) | 3670 | 22.0 |
| Province 4 (Gandagi) | 1604 | 9.6 |
| Province 5 (Lumbini) | 2886 | 17.3 |
| Province 6 (Karmali) | 915 | 5.5 |
| Province 7 (Sudurpashchim) | 1448 | 8.7 |
| Owns a mobile phone | ||
| No | 3861 | 23.2 |
| Yes | 12,811 | 76.8 |
| Residence | ||
| Urban | 10,543 | 63.2 |
| Rural | 6129 | 36.8 |
| Variables | TB Awareness Odds Ratio (95% CI) |
|---|---|
| Age group | |
| 15–24 | 1.00 (ref) |
| 25–35 | 1.57 (1.19–2.08) ** |
| 35–49 | 1.61 (1.15–2.26) ** |
| Gender | |
| Male | 1.00 (ref) |
| Female | 1.46 (1.05–2.04) * |
| Wealth quintile | |
| Poorest | 1.00 (ref) |
| Poorer | 1.74 (1.25–2.42) ** |
| Middle | 2.06 (1.44–2.94) *** |
| Richer | 1.64 (1.14–2.36) ** |
| Richest | 3.46 (2.05–5.84) *** |
| Education | |
| No formal education | 1.00 (ref) |
| Primary education | 1.48 (1.10–1.99) * |
| Secondary education | 5.36 (3.76–7.65) *** |
| Higher education | 16.19 (8.04–32.58) *** |
| Owns a mobile phone | |
| No | 1.00 (ref) |
| Yes | 1.66 (1.30–2.10) *** |
| Province | |
| Province 6 (Karmali) | 1.00 (ref) |
| Province 1 (Not determined) | 0.87 (0.49–1.57) |
| Province 2 (Not determined) | 0.79 (0.45–1.41) |
| Province 3 (Bagmati) | 1.42 (0.74–2.71) |
| Province 4 (Gandagi) | 1.21 (0.63–2.31) |
| Province 5 (Lumbini) | 2.24 (1.26–3.97) * |
| Province 7 (Sudurpashchim) | 0.84 (0.48–1.50) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iwaki, Y.; Rauniyar, S.K.; Nomura, S.; Huang, M.C. Assessing Factors Associated with TB Awareness in Nepal: A National and Subnational Study. Int. J. Environ. Res. Public Health 2021, 18, 5124. https://doi.org/10.3390/ijerph18105124
Iwaki Y, Rauniyar SK, Nomura S, Huang MC. Assessing Factors Associated with TB Awareness in Nepal: A National and Subnational Study. International Journal of Environmental Research and Public Health. 2021; 18(10):5124. https://doi.org/10.3390/ijerph18105124
Chicago/Turabian StyleIwaki, Yoko, Santosh Kumar Rauniyar, Shuhei Nomura, and Michael C. Huang. 2021. "Assessing Factors Associated with TB Awareness in Nepal: A National and Subnational Study" International Journal of Environmental Research and Public Health 18, no. 10: 5124. https://doi.org/10.3390/ijerph18105124
APA StyleIwaki, Y., Rauniyar, S. K., Nomura, S., & Huang, M. C. (2021). Assessing Factors Associated with TB Awareness in Nepal: A National and Subnational Study. International Journal of Environmental Research and Public Health, 18(10), 5124. https://doi.org/10.3390/ijerph18105124






