Knowledge and Preference Towards Mode of Delivery among Pregnant Women in the United Arab Emirates: The Mutaba’ah Study
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Profile of the Study Population
3.2. Knowledge Towards Mode of Delivery
3.3. Factors Associated with a Lack of Adequate Knowledge on Mode of Delivery
3.4. Preferred Mode of Delivery for Current Pregnancy
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Betrán, A.P.; Torloni, M.R.; Zhang, J.; Ye, J.; Mikolajczyk, R.T.; Deneux-Tharaux, C.; Oladapo, O.T.; Souza, J.P.; Tunçalp, Ö.; Vogel, J.P.; et al. What is the optimal rate of caesarean section at population level? A systematic review of ecologic studies. Reprod. Health 2015, 12, 1–10. [Google Scholar] [CrossRef] [PubMed]
- WHO. World Health Organization Statement on Caesarean Section Rates. Available online: http://apps.who.int/iris/bitstream/10665/161442/1/WHO_RHR_15.02_eng.pdf (accessed on 9 October 2020).
- Steer, P.J.; Modi, N. Elective caesarean sections—Risks to the infant. Lancet 2009, 374, 675–676. [Google Scholar] [CrossRef]
- Victora, C.G.; Barros, F.C. Beware: Unnecessary caesarean sections may be hazardous. Lancet 2006, 367, 1796–1797. [Google Scholar] [CrossRef]
- Mascarello, K.C.; Matijasevich, A.; Santos, I.; Silveira, M.F. Early and late puerperal complications associated with the mode of delivery in a cohort in Brazil. Rev. Bras. Epidemiol. 2018, 21, e180010. [Google Scholar] [CrossRef]
- Sharma, S.; Dhakal, I. Cesarean vs Vaginal Delivery: An Institutional Experience. JNMA J. Nepal. Med. Assoc. 2018, 56, 535–539. [Google Scholar] [CrossRef]
- Fahmy, W.M.; Crispim, C.A.; Cliffe, S. Association between maternal death and cesarean section in Latin America: A systematic literature review. Midwifery 2018, 59, 88–93. [Google Scholar] [CrossRef]
- Zaręba, K.; Banasiewicz, J.; Rozenek, H.; Wójtowicz, S.; Jakiel, G. Peripartum Predictors of the Risk of Postpartum Depressive Disorder: Results of a Case-Control Study. Int. J. Environ. Res. Public Health 2020, 17, 8726. [Google Scholar] [CrossRef]
- Shay, L.A.; Lafata, J.E. Where Is the Evidence? A Systematic Review of Shared Decision Making and Patient Outcomes. Med. Decis. Mak. 2015, 35, 114–131. [Google Scholar] [CrossRef]
- Stiggelbout, A.M.; Pieterse, A.H.; De Haes, J.C.J.M. Shared decision making: Concepts, evidence, and practice. Patient Educ. Couns. 2015, 98, 1172–1179. [Google Scholar] [CrossRef]
- Veroff, D.; Marr, A.; Wennberg, D.E. Enhanced Support For Shared Decision Making Reduced Costs Of Care For Patients With Preference-Sensitive Conditions. Health Aff. 2013, 32, 285–293. [Google Scholar] [CrossRef]
- Weckesser, A.; Farmer, N.; Dam, R.; Wilson, A.; Morton, V.H.; Morris, R.K. Women’s perspectives on caesarean section recovery, infection and the PREPS trial: A qualitative pilot study. BMC Pregnancy Childbirth 2019, 19, 1–10. [Google Scholar] [CrossRef]
- Majlesi, M.; Montazeri, A.; Rakhshani, F.; Nouri-Khashe-Heiran, E.; Akbari, N. ‘No to unnecessary caesarean sections’: Evaluation of a mass-media campaign on women’s knowledge, attitude and intention for mode of delivery. PLoS ONE 2020, 15, e0235688. [Google Scholar] [CrossRef] [PubMed]
- UN. The Millennium Development Goals Report. Available online: https://www.un.org/millenniumgoals/2015_MDG_Report/pdf/MDG%202015%20rev%20(July%201).pdf (accessed on 1 October 2020).
- WHO. Countdown to 2015: Maternal, Newborn, & Child Survival. Available online: http://www.countdown2015mnch.org/ (accessed on 15 October 2020).
- Taha, Z.; Hassan, A.A.; Wikkeling-Scott, L.; Papandreou, D. Prevalence and Associated Factors of Caesarean Section and its Impact on Early Initiation of Breastfeeding in Abu Dhabi, United Arab Emirates. Nutrition 2019, 11, 2723. [Google Scholar] [CrossRef] [PubMed]
- Al-Rifai, R.H.; Ali, N.; Barigye, E.T.; Al Haddad, A.H.I.; Al Maskari, F.; Loney, T.; Ahmed, L.A. Maternal and birth cohort studies in the Gulf Cooperation Council countries: A systematic review and meta-analysis. Syst. Rev. 2020, 9, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Al Haddad, A.; Ali, N.; Elbarazi, I.; Elabadlah, H.; Al-Maskari, F.; Narchi, H.; Brabon, C.; Ghazal-Aswad, S.; Alshalabi, F.M.; Zampelas, A.; et al. Mutaba’ah—Mother and Child Health Study: Protocol for a prospective cohort study investigating the maternal and early life determinants of infant, child, adolescent and maternal health in the United Arab Emirates. BMJ Open 2019, 9, e030937. [Google Scholar] [CrossRef] [PubMed]
- Ghotbi, F.; Sene, A.A.; Azargashb, E.; Shiva, F.; Mohtadi, M.; Zadehmodares, S.; Farzaneh, F.; Yasai, F.-A.-M. Women’s knowledge and attitude towards mode of delivery and frequency of cesarean section on mother’s request in six public and private hospitals in Tehran, Iran, 2012. J. Obstet. Gynaecol. Res. 2014, 40, 1257–1266. [Google Scholar] [CrossRef]
- STROBE Group. STROBE Statement: Home. 2007. Available online: https://www.strobe-statement.org/index.php?id=strobe-home (accessed on 15 February 2020).
- Jadoon, B.; Mahaini, R.; Gholbzouri, K. Determinants of over and underuse of caesarean births in the Eastern Mediterranean Region: An updated review. East. Mediterr. Health J. 2019, 25, 837–846. [Google Scholar] [CrossRef]
- Bergeron, V. The ethics of cesarean section on maternal request: A feminist critique of the american college of obstetricians and gynecologists’ position on patient-choice surgery. Bioethics 2007, 21, 478–487. [Google Scholar] [CrossRef]
- Minkoff, H. The Ethics of Cesarean Section by Choice. Semin. Perinatol. 2006, 30, 309–312. [Google Scholar] [CrossRef]
- WHO. World Health Organization Recommendations: Non-Clinical Interventions to Reduce Unnecessary Caesarean Sections. Available online: https://www.who.int/reproductivehealth/publications/non-clinical-interventions-to-reduce-cs/en/ (accessed on 15 September 2020).
- Eide, K.T.; Bærøe, K. How to reach trustworthy decisions for caesarean sections on maternal request: A call for beneficial power. J. Med. Ethic 2020, 10, 6071. [Google Scholar] [CrossRef]
- Saoji, A.; Nayse, J.; Kasturwar, N.; Nisha, R. Women’s knowledge, perceptions, and potential demand towards caesarean section. Natl. J. Community Med. 2011, 2, 244–248. [Google Scholar]
- Rice, P.L.; Naksook, C. Caesarean or vaginal birth: Perceptions and experience of Thai women in Australian hospitals. Aust. N. Z. J. Public Health 1998, 22, 604–608. [Google Scholar] [CrossRef] [PubMed]
- Ali, N.; Elbarazi, I.; Alabboud, S.; Al-Maskari, F.; Loney, T.; Ahmed, L.A. Antenatal Care Initiation among Pregnant Women in the United Arab Emirates: The Mutaba’ah Study. Front. Public Health 2020, 8, 211. [Google Scholar] [CrossRef] [PubMed]
- Ali, N.; Elbarazi, I.; Ghazal-Aswad, S.; Al-Maskari, F.; Al-Rifai, R.H.; Oulhaj, A.; Loney, T.; Ahmed, L.A. Impact of Recurrent Miscarriage on Maternal Outcomes in Subsequent Pregnancy: The Mutaba’ah Study. Int. J. Women’s Health 2020, 12, 1171–1179. [Google Scholar] [CrossRef]
- Fransisco, K.; Sanchez, M. Vaginal Birth After Cesarean Section (VBAC): Informed Choice and a Source of Empowerment among Black Women in the United States. In Global Perspectives on Women’s Sexual and Reproductive Health across the Lifecourse; Springer Science and Business Media LLC.: Berlin/Heidelberg, Germany, 2017; pp. 75–89. [Google Scholar]
- Abu Dhabi Department of Health (AKA Health Authority), Health Authority-Abu Dhabi. HAAD Standard for Premarital Screening and Counseling Program. 2013; pp. 2–5. Available online: Doh.gov.ae (accessed on 8 December 2020).
| N (Valid %) | |
|---|---|
| Age (mean = 30.6 years ± 5.8 SD) | |
| 18–24 | 209 (16.0) |
| 25–29 | 350 (26.9) |
| ≥30 | 744 (57.1) |
| Educational attainment | |
| Two-year diploma and above | 639 (53.1) |
| Secondary schooling and below | 565 (46.9) |
| Missing | 99 |
| Husband’s educational attainment | |
| Two-year diploma and above | 628 (50.2) |
| Secondary schooling and below | 623 (49.8) |
| Missing/Do not know | 52 |
| Employed | |
| No | 830 (68.9) |
| Yes | 374 (31.1) |
| Missing | 99 |
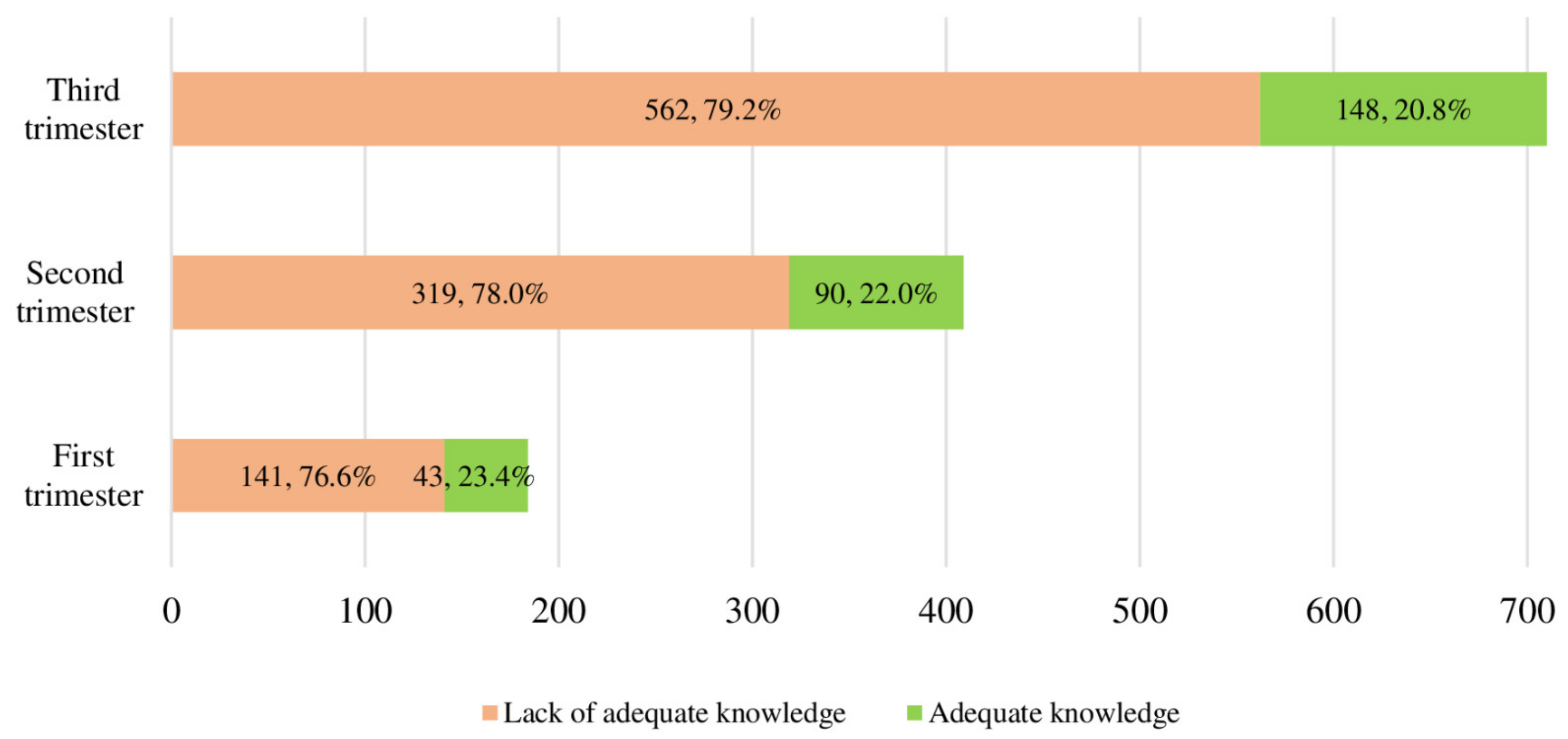
| Gestational trimester (mean gestational age = 6.4 months ± 2.2 SD) | |
| First | 184 (14.1) |
| Second | 409 (31.4) |
| Third | 710 (54.5) |
| Parity (mean = 3.0 ± 1.8 SD) | |
| Nulliparous (1st pregnancy) | 279 (23.4) |
| At least one child | 913 (76.6) |
| Missing | 111 |
| Gravidity (mean = 3.6 ± 2.2 SD) | |
| Never been pregnant before | 394 (30.2) |
| At least one pregnancy | 909 (69.8) |
| Mode of last delivery | |
| Vaginal | 772 (79.2) |
| CS | 203 (20.8) |
| Missing/Nulliparous | 328 |
| Previous eventful pregnancy | |
| Never | 199 (23.1) |
| 1–2 events | 494 (57.4) |
| ≥3 events | 168 (12.9) |
| Missing/nulliparous | 442 |
| Preferred mode of upcoming delivery | |
| CS | 122 (9.4) |
| Vaginal | 1128 (86.9) |
| Have not decided | 48 (3.6) |
| Missing | 5 |
| Knowledge Item | Expected Answer | Reported Answer | |
|---|---|---|---|
| Correct | Incorrect or Not Sure | ||
| n (%) | n (%) | ||
| Cesarean delivery is less painful | Strongly agree/agree | 311 (23.9) | 992 (76.1) |
| Maternal complications of cesarean delivery are greater | Strongly agree/agree | 813 (62.4) | 490 (37.6) |
| Infection risk of cesarean delivery is higher than vaginal delivery | Strongly agree/agree | 599 (46.0) | 704 (54.0) |
| Emotional relationship between mother and baby after vaginal delivery is better | Strongly agree/agree | 824 (63.2) | 479 (36.8) |
| Infants born by cesarean section are smarter compared with those born by vaginal delivery | Strongly disagree/disagree | 493 (37.8) | 810 (62.2) |
| Infant bone fractures are impossible in cesarean section delivery | Strongly disagree/disagree | 219 (16.8) | 1084 (83.2) |
| It is reasonable to request cesarean section again for next delivery after the first cesarean section | Strongly agree/agree | 432 (33.2) | 871 (66.8) |
| Respiratory disorders in infants born by cesarean section are less likely than those born by vaginal delivery | Strongly disagree/disagree | 245 (18.8) | 1058 (81.2) |
| Hemorrhage after cesarean delivery is less than after vaginal delivery | Strongly disagree/disagree | 210 (16.1) | 1093 (83.9) |
| Cesarean section is reasonable when the baby is in breech presentation | Strongly agree/agree | 771 (59.2) | 532 (40.8) |
| Adequacy of knowledge (mean score = 3.7 ± 2.2 SD) | |||
| Lack of adequate knowledge (score 0–5) | 1022 (78.4) | ||
| Adequate knowledge (score 6–10) | 281 (21.6) | ||
| OR (95% CI) | aOR (95% CI) | |
|---|---|---|
| Age, years | ||
| ≥30 | 1.00 | 1.00 |
| 25–29 | 0.97 (0.72–1.31) | 0.90 (0.61–1.33) |
| 18–24 | 1.61 (1.07–2.44) 1 | 3.07 (1.07–8.86) 1 |
| Educational attainment | ||
| Two-years diploma or above | 1.00 | 1.00 |
| Secondary schooling or below | 1.31 (0.99–1.73) | 1.34 (0.95–1.89) |
| Husband’s educational attainment | ||
| Two-years diploma or above | 1.00 | 1.00 |
| Secondary schooling or below | 1.06 (0.81–1.38) | 1.08 (0.79–1.31) |
| Current working status | ||
| Working | 1.00 | 1.00 |
| Not working | 1.18 (0.88–1.58) | 1.12 (0.85–1.59) |
| Gestational trimester | ||
| Third | 1.00 | 1.00 |
| Second | 0.93 (0.69–1.26) | 0.71 (0.48–1.04) |
| First | 0.86 (0.58–1.27) | 0.75 (0.46–1.24) |
| Parity | ||
| At least one child | 1.00 | 1.00 |
| Nulliparous | 1.19 (0.85–1.68) | – |
| Gravidity | ||
| Never been pregnant before | 1.00 | 1.00 |
| At least one pregnancy | 0.99 (0.75–1.33) | – |
| Previous eventful pregnancy | ||
| ≥3 events | 1.00 | 1.00 |
| 1–2 events | 1.33 (0.88–2.01) | 1.36 (0.88–2.12) |
| Never | 1.28 (0.79–2.1 | 1.39 (0.88–2.37) |
| Mode of last delivery | ||
| Vaginal | 1.00 | 1.00 |
| CS | 1.81 (1.18–2.75) 2 | 1.90 (1.06–3.40) 1 |
| CS, (after excluding nulliparous women) | 1.89 (1.13–3.16) 1 | 2.15 (1.22–3.79) 2 |
| Preferred mode of delivery for current pregnancy | ||
| Vaginal | 1.00 | 1.00 |
| CS | 1.97 (1.14–3.38) 1 | 1.41 (0.66–3.00) |
| Have not decided yet | 2.08 (0.87–4.94) | 1.02 (1.04–3.33) |
| CS 122 (%) | Vaginal 1128 (%) | p-Value | OR (95% CI) | aOR (95% CI) | |
|---|---|---|---|---|---|
| Age | <0.001 | ||||
| 18–24 | 95 (77.9) | 625 (55.4) | 1.00 | 1.08 (1.02–1.14) 2 | |
| 25–29 | 25 (20.5) | 308 (27.3) | 7.91 (1.85–33.79) 3 | ||
| ≥30 | 2 (1.6) | 195 (17.3) | 14.82 (3.62–60.67) 4 | ||
| Educational attainment | 0.811 | ||||
| Two-years diploma and above | 59 (51.8) | 551 (52.9) | 1.00 | – | |
| Secondary schooling and below | 55 (48.2) | 490 (47.1) | 1.05 (0.71–1.54) | ||
| Husband’s educational attainment | 0.265 | ||||
| Two-years diploma and above | 53 (44.9) | 545 (50.3) | 1.00 | – | |
| Secondary schooling and below | 65 (55.1) | 538 (49.7) | 1.24 (0.85–1.82) | ||
| Employed | 0.004 | ||||
| No | 65 (57.0) | 738 (70.9) | 1.00 | 1.00 | |
| Yes | 49 (43.0) | 303 (29.1) | 1.84 (1.24–2.72) 3 | 1.96 (1.13–3.40) 2 | |
| Gestational trimester | 0.462 | ||||
| First | 16 (13.1) | 159 (14.1) | 1.00 | – | |
| Second | 44 (36.1) | 345 (30.6) | 1.26 (0.70–2.14) | ||
| Third | 62 (50.8) | 624 (55.3) | 0.99 (0.56–1.76) | ||
| Parity1 | <0.001 | ||||
| Nulliparous | 10 (8.8) | 248 (24.1) | 1.00 | ||
| At least one child | 103 (91.2) | 782 (75.9) | 3.27 (1.68–6.35) 4 | 1.60 (0.30–8.37) | |
| Gravidity1 | 0.001 | ||||
| Never been pregnant before | 20 (16.4) | 349 (30.9) | 1.00 | 1.00 | |
| At least one pregnancy | 102 (83.6) | 779 (69.1) | 2.28 (1.39–3.75) 2 | 1.38 (0.50–3.84) | |
| Mode of last delivery | <0.001 | ||||
| Vaginal | 20 (18.7) | 737 (87.5) | 1.00 | 1.00 | |
| CS | 87 (81.3) | 105 (12.5) | 30.53 (18.02–51.73) 4 | 31.10 (17.71–55.71) 4 | |
| Knowledge level | 0.013 | ||||
| Adequate knowledge | 16 (13.1) | 258 (22.9) | 1.00 | 1.00 | |
| Lack of adequate knowledge | 106 (86.9) | 870 (77.1) | 1.97 (1.14–3.38) 2 | 1.70 (0.81–3.57) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Rifai, R.H.; Elbarazi, I.; Ali, N.; Loney, T.; Oulhaj, A.; Ahmed, L.A. Knowledge and Preference Towards Mode of Delivery among Pregnant Women in the United Arab Emirates: The Mutaba’ah Study. Int. J. Environ. Res. Public Health 2021, 18, 36. https://doi.org/10.3390/ijerph18010036
Al-Rifai RH, Elbarazi I, Ali N, Loney T, Oulhaj A, Ahmed LA. Knowledge and Preference Towards Mode of Delivery among Pregnant Women in the United Arab Emirates: The Mutaba’ah Study. International Journal of Environmental Research and Public Health. 2021; 18(1):36. https://doi.org/10.3390/ijerph18010036
Chicago/Turabian StyleAl-Rifai, Rami H., Iffat Elbarazi, Nasloon Ali, Tom Loney, Abderrahim Oulhaj, and Luai A. Ahmed. 2021. "Knowledge and Preference Towards Mode of Delivery among Pregnant Women in the United Arab Emirates: The Mutaba’ah Study" International Journal of Environmental Research and Public Health 18, no. 1: 36. https://doi.org/10.3390/ijerph18010036
APA StyleAl-Rifai, R. H., Elbarazi, I., Ali, N., Loney, T., Oulhaj, A., & Ahmed, L. A. (2021). Knowledge and Preference Towards Mode of Delivery among Pregnant Women in the United Arab Emirates: The Mutaba’ah Study. International Journal of Environmental Research and Public Health, 18(1), 36. https://doi.org/10.3390/ijerph18010036





