Use of a Health Advocacy Model for Survivors of Interpersonal Violence
Abstract
1. Introduction
1.1. Interpersonal Violence
1.2. Health Advocacy
2. Materials and Methods
2.1. Setting
2.2. Ethical Considerations
2.3. Training Health Advocates
2.4. Health Advocacy Delivery
2.5. Measures
2.6. Data Analysis
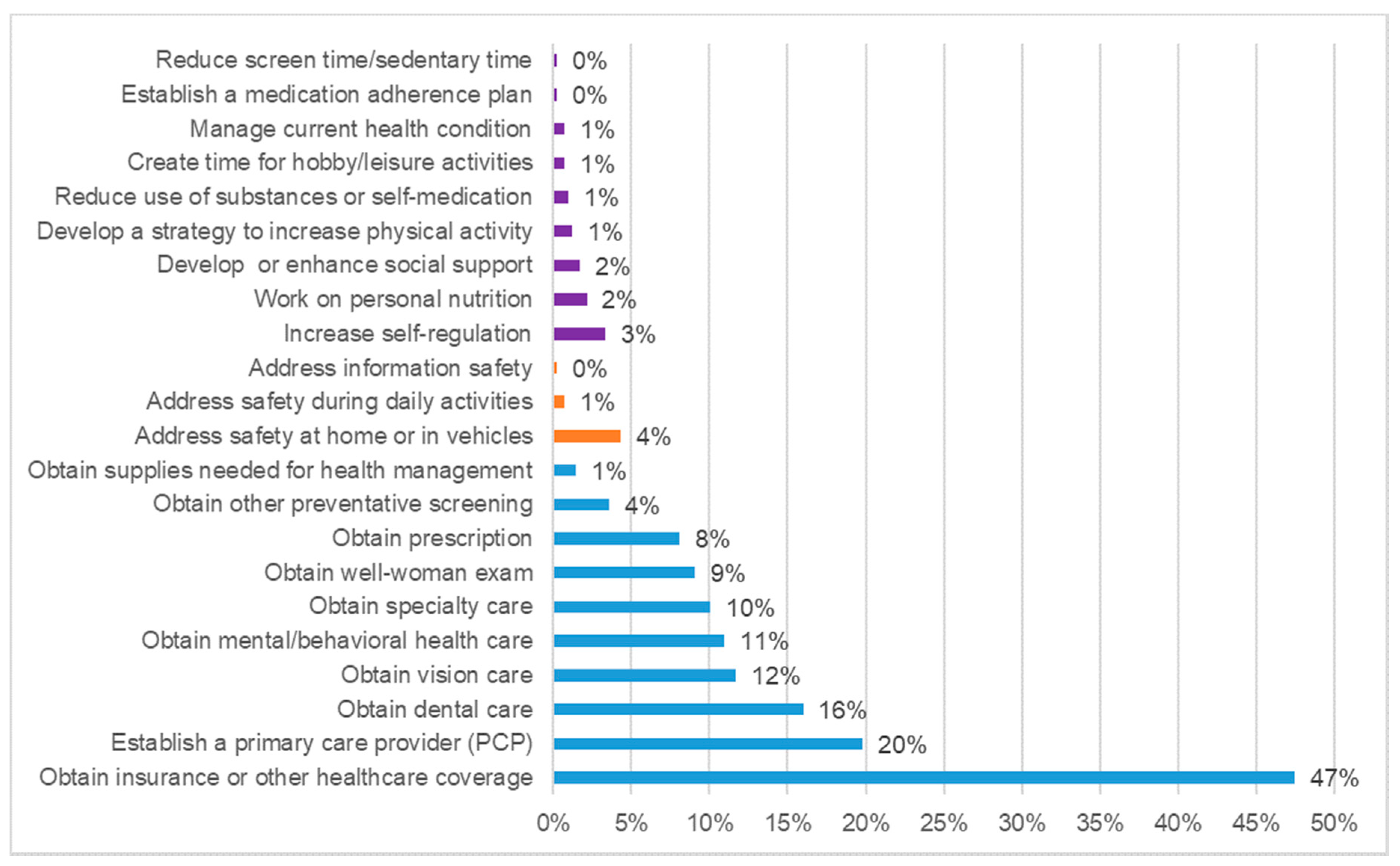
3. Results
4. Discussion and Conclusions
5. Limitations
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Elliott, L. Interpersonal violence. J. Gen. Intern. Med. 2003, 18, 871–872. [Google Scholar] [CrossRef] [PubMed]
- Rutherford, A.; Zwi, A.B.; Grove, N.J.; Butchart, A. Violence: A glossary. J. Epidemiol. Community Health 2007, 61, 676–680. [Google Scholar] [CrossRef]
- Smith, S.G.; Zhang, X.; Basile, K.C.; Merrick, M.T.; Wang, J.; Kresnow, M.; Chen, J. The National Intimate Partner and Sexual Violence Survey (NISVS): 2015 Data Brief—Updated Release; National Center for Injury Prevention and Control & Centers for Disease Control and Prevention: Atlanta, GA, USA, 2018; pp. 154–196. Available online: https://www.cdc.gov/violenceprevention/pdf/2015data-brief508.pdf (accessed on 1 September 2020).
- Campbell, J.C.; Jones, A.S.; Dienemann, J.; Kub, J.; Schollenberger, J.; O’Campo, P.; Gielen, A.C.; Wynne, C. Intimate Partner Violence and Physical Health Consequences. Arch. Intern. Med. 2002, 162, 1157–1163. [Google Scholar] [CrossRef]
- Breiding, M.J.; Black, M.C.; Ryan, G.W. Chronic Disease and Health Risk Behaviors Associated with Intimate Partner Violence—18 U.S. States/Territories, 2005. Ann. Epidemiol. 2008, 18, 538–544. [Google Scholar] [CrossRef]
- Vijayaraghavan, M.; Tochterman, A.; Hsu, E.; Johnson, K.; Marcus, S.; Caton, C.L.M. Health, Access to Health Care, and Health Care use Among Homeless Women with a History of Intimate Partner Violence. J. Community Health 2012, 37, 1032–1039. [Google Scholar] [CrossRef]
- Arias, I.; Corso, P. Average cost per person victimized by an intimate partner of the opposite gender: A comparison of men and women. Violence Vict. 2005, 20, 379–391. [Google Scholar] [CrossRef]
- Bonomi, A.E.; Anderson, M.L.; Rivara, F.P.; Thompson, R.S. Health Care Utilization and Costs Associated with Physical and Nonphysical-Only Intimate Partner Violence. Health Serv. Res. 2009, 44, 1052–1067. [Google Scholar] [CrossRef]
- Jones, A.S.; Dienemann, J.; Schollenberger, J.; Kub, J.; O’Campo, P.; Gielen, A.C.; Campbell, J.C. Long-term costs of intimate partner violence in a sample of female HMO enrollees. Women′s Health Issues 2006, 16, 252–261. [Google Scholar] [CrossRef]
- Peterson, C.; Kearns, M.C.; McIntosh, W.L.; Estefan, L.F.; Nicolaidis, C.; McCollister, K.E.; Gordon, A.; Florence, C. Lifetime Economic Burden of Intimate Partner Violence Among U.S. Adults. Am. J. Prev. Med. 2018, 55, 433–444. [Google Scholar] [CrossRef]
- Christoffel, K.K. Public health advocacy: Process and product. Am. J. Public Health 2000, 90, 722. [Google Scholar]
- Hubinette, M.; Dobson, S.; Scott, I.; Sherbino, J. Health advocacy. Med Teach. 2016, 39, 128–135. [Google Scholar] [CrossRef]
- Miller, W.R.; Rollnick, S. Motivational Interviewing: Helping People Change, 3rd ed.; Guilford Press: New York, NY, USA, 2012. [Google Scholar]
- Söderlund, L.L.; Madson, M.B.; Rubak, S.; Nilsen, P. A systematic review of motivational interviewing training for general health care practitioners. Patient Educ. Couns. 2011, 84, 16–26. [Google Scholar] [CrossRef]
- Walter, J.L.; Peller, J.E. Becoming Solution-Focused in Brief Therapy; Brunner/Mazel Publishers: New York, NY, USA, 1992. [Google Scholar]
- Bannink, F.P. Posttraumatic success: Solution-focused brief therapy. Brief Treat. Crisis Interv. 2008, 8, 215–225. [Google Scholar] [CrossRef]
- Stermensky, G.; Brown, K.S. The perfect marriage: Solution-focused therapy and motivational interviewing in medical family therapy. J. Fam. Med. Prim. Care 2014, 3, 383–387. [Google Scholar] [CrossRef]
- Koetting, C. Trauma-informed care: Helping patients with a painful past. J. Christ. Nurs. 2016, 33, 206–213. [Google Scholar] [CrossRef]
- Raja, S.; Hasnain, M.; Hoersch, M.; Gove-Yin, S.; Rajagopalan, C. Trauma Informed Care in Medicine. Fam. Community Health 2015, 38, 216–226. [Google Scholar] [CrossRef]
- Kiresuk, T.J.; Sherman, E.R. Goal attainment scaling: A general method for evaluating comprehensive community mental health programs. Community Ment. Health J. 1968, 4, 443–453. [Google Scholar] [CrossRef]
- Bovend’Eerdt, T.J.H.; Botell, E.R.; Wade, D.T. Writing SMART rehabilitation goals and achieving goal attainment scaling: A practical guide. Clin. Rehabil. 2009, 23, 352–361. [Google Scholar] [CrossRef]
- Plichta, S.B. Interactions Between Victims of Intimate Partner Violence Against Women and the Health Care System. Trauma Violence Abus. 2007, 8, 226–239. [Google Scholar] [CrossRef]
- Hegarty, K.; McKibbin, G.; Hameed, M.A.; Koziol-McLain, J.; Feder, G.; Tarzia, L.; Hooker, L. Health practitioners’ readiness to address domestic violence and abuse: A qualitative meta-synthesis. PLoS ONE 2020, 15, e0234067. [Google Scholar] [CrossRef]
- De Shazer, S.; Dolan, Y.; Korman, H.; Trepper, T.S.; McCollom, E.; Berg, I.K. More than Miracles: The State of the Art of Solution-Focused Brief Therapy; Routledge: New York, NY, USA, 2007. [Google Scholar]
- Lewis, T.F.; Osborn, C.J. Solution-Focused Counseling and Motivational Interviewing: A Consideration of Confluence. J. Couns. Dev. 2004, 82, 38–48. [Google Scholar] [CrossRef]
- Wand, T. Mental health nursing from a solution focused perspective. Int. J. Ment. Health Nurs. 2010, 19, 210–219. [Google Scholar] [CrossRef]
| Theoretical Influence | Description |
|---|---|
| Motivational Interviewing | Collaborative conversation style to draw out a client’s motivation and commitment to change. |
| Solution-Focused Brief Therapy | Goal-directed approach to draw out a client’s ideas and plans for change. |
| Trauma-Informed Care | Patient-centered communication approach to recognize the influence of past trauma on health behavior. |
| Characteristic | n | % |
|---|---|---|
| Gender | ||
| Female | 334 | 79.7% |
| Not-Female * | 6 | 1.4% |
| Missing | 79 | 18.9% |
| Age ** | 36.93 years | 10.38 (SD) |
| Hispanic | ||
| Yes | 129 | 30.8% |
| No | 134 | 32.0% |
| Missing | 156 | 37.2% |
| Race | ||
| White | 148 | 35.3% |
| Black | 87 | 20.8% |
| Bi/Multi Racial | 22 | 5.3% |
| Other Race | 35 | 8.4% |
| Missing | 127 | 30.3% |
| Referral Organization | ||
| IPV Organization | 353 | 84.2% |
| Police Department | 17 | 4.1% |
| Clinic | 49 | 11.7% |
| −2 | −1 | 0 | +1 | +2 | Average | |
|---|---|---|---|---|---|---|
| Healthcare Management | −0.51 | |||||
| Obtain insurance or other healthcare coverage | Has not explored healthcare coverage options (n = 29) | Has not identified healthcare coverage (n = 34) | Has identified eligible healthcare coverage but not yet applied (n = 96) | Applied for coverage but has not yet been approved (n = 28) | Has obtained insurance coverage (n = 12) | −0.20 |
| Establish a primary care provider (PCP) | Using ER for primary care in past 90 days (n = 13) | No identified PCP (n = 48) | Identified PCP but not apt (n = 15) | Has future appointment with PCP (n = 6) | Has PCP and completed at least one appointment (n = 1) | −0.80 |
| Obtain dental care | Not pursuing dental treatment (n = 13) | No provider identified, using alternative methods to manage dental problems (n = 37) | Has identified dental care provider, but does not have appointment (n = 14) | Has appointment scheduled for dental care (n = 2) | Has located dental care provider and completed at least 1 appointment (n = 1) | −0.88 |
| Obtain vision care | Not pursing vision treatment (n = 5) | No vision provider identified, using alternative methods to manage vision problems (n = 19) | Has identified vision provider, but does not have appointment (n = 19) | Has appointment scheduled for vision care (n = 4) | Has located vision provider and completed at least 1 appointment (n = 2) | −0.43 |
| Obtain mental/behavioral health care | Using emergency services for mental health crisis (n = 4) | No identified mental health provider (n = 28) | Identified mental health provider, but no appointment yet scheduled (n = 10) | Has future appointment with mental health provider (n = 1) | Has identified mental health provider and has completed at least one appointment (n = 3) | −0.63 |
| Obtain specialty care | Not pursuing specialty care services (n = 1) | No identified specialty care provider (n = 24) | Has identified type of specialty care needed, but does not have appointment (n = 10) | Has appointment scheduled with specialist (n = 3) | Has completed at least one appointment with specialist (n = 4) | −0.36 |
| Obtain well-woman exam | Has not had a well woman exam in over 2 years (n = 12) | Has no identified provider selected (n = 16) | Has identified appropriate provider but no appointment (n = 8) | Has appointment for well women exam scheduled (n = 2) | Has followed guidelines/recommendations for obtaining regular well woman exams (n = 0) | −1.00 |
| Obtain prescription | Using emergency department for emergency medication needs (n = 2) | Has not identified prescription assistance (n = 19) | Identified prescription assistance but does not have medication (n = 9) | Has obtained prescriptions but does not have plan for ongoing care (n = 2) | Has prescriptions with follow up care in place (n = 2) | −0.5 |
| Obtain other preventative screening | No preventative health screenings in past year (n = 4) | Has not identified provider or location for preventative health screening (n = 8) | Has identified provider/location to receive preventative health screening, but has not made appointment (n = 1) | Has appointment scheduled for preventative health screening (n = 1) | Has followed guidelines for obtaining recommended health screening (n = 1) | −0.87 |
| Obtain supplies needed for health management | Using emergency department for needed. medical equipment/supplies (n = 0) | Has documented medical need for supplies but no resource to obtain them (n = 2) | Has identified resource for help in obtaining needed equipment/supplies; but not yet received them (n = 2) | Has obtained needed supplies but no ongoing resource (n = 2) | Has needed supplies and resource for obtaining ongoing supplies or equipment (n = 0) | 0.00 |
| Safety | −0.05 | |||||
| Address safety at home or in vehicles | Intentionally attempts to escalate conflict/risk at home (n = 2) | No identified methods to increase safety at home (n = 4) | Has identified methods to increase safety at home, but yet to implement them (n = 6) | Has implemented steps to increase safety at home (n = 6) | Has implemented steps to increase safety at home, and identifies one observable benefit (n = 0) | −0.11 |
| Address safety during daily activities | Intentionally attempts to escalate conflict during daily activities (n = 0) | No identified methods to increase safety during daily activities (n = 1) | Has identified methods to increase safety during daily activities, but yet to implement them (n = 1) | Has implemented steps to increase safety during daily activities (n = 1) | Has implemented steps to increase safety during daily activities and identifies one observable benefit (n = 0) | 0.00 |
| Address information safety | Intentionally attempts to escalate risk of information (n = 0) | No identified methods to increase safety of information (n = 0) | Has identified methods to increase information safety, but yet to implement them (n = 0) | Has implemented steps to increase information safety (n = 1) | Has implemented steps to increase information safety and identifies one observable benefit (n = 0) | 1.00 |
| Self-Care | −0.34 | |||||
| Increase self-regulation | Increase in escalated body response, panic attacks (n = 1) | No identified methods for controlling physiological functions (n = 5) | Has identified new method of self-regulation but has not yet implemented it (n = 5) | Has adopted new method to increase self-regulation and implemented into routine (n = 3) | Has adopted a new method to increase self-regulation and can identify one observable benefit (n = 0) | −0.29 |
| Work on personal nutrition | Actively abandoned nutrition goals (n = 0) | No identified nutritional goals (n = 4) | Has created personal nutrition goals, but not yet implemented (n = 5) | Has created personal nutrition goals and implemented those into routine (n = 0) | Actively pursuing nutrition goals and can identify one observable benefit (n = 0) | −0.44 |
| Develop or enhance social support | Socially isolated, only relationships are destructive or dangerous (n = 1) | Has no identified support systems (n = 3) | Has identified potential support system but has not attempted to connect (n = 1) | Has identified potential supports and has made efforts to connect with them (n = 2) | Has identified support system that she regularly engages with for support (n = 0) | −0.43 |
| Develop a strategy to increase physical activity | Significantly decreased amount of physical activity (n = 0) | No identified goals for increasing physical activity (n = 2) | Has identified ways to increase physical activity but not yet implemented (n = 2) | Has increased physical activity (n = 0) | Has increased physical activity and can identify one observable benefit (n = 1) | 0.00 |
| Reduce use of substances or self-medication | Engages in high risk behaviors, significant increase in use of substances (n = 0) | No identified healthy coping skills, slight increase in use of substances (n = 1) | Identified healthy coping skills, no change in use of substances (n = 0) | Has decreased use of substances and increased healthy coping skills (n = 3) | Has decreased use of substances, increased healthy coping skills, and can identify at least one observable benefit (n = 0) | −0.25 |
| Create time for hobby/leisure activities | Abandoned goal of new leisure activity (n = 0) | No identified hobby or leisure activity (n = 1) | Identified new hobby or leisure activity but not yet implemented (n = 2) | Identified new hobby or leisure activity and implemented into routine (n = 0) | Has adopted new hobby/leisure activity and can identify one observable benefit (n = 0) | −0.33 |
| Manage current health condition | Not managing current health condition, using emergency services for maintenance (n = 1) | No identified plan for health maintenance (n = 0) | Has created a health maintenance plan, but not yet implemented (n = 1) | Has implemented a health maintenance plan (n = 1) | Has implemented a health maintenance plan and can identify at least one observable benefit (n = 0) | −0.33 |
| Establish a medication adherence plan | Uses medication in an unsafe manner, often resulting in use of emergency services (n = 0) | No identified plan to improve medication compliance (n = 1) | has identified strategies to improve medication compliance but not yet implemented (n = 0) | Has implemented strategies to improve medication compliance (n = 0) | Has been taking medications as prescribed and can identify one observable benefit (n = 0) | −1.00 |
| Reduce screen time/sedentary time | Abandoned goal of reducing sedentary time (n = 0) | No identified alternatives to screen time/sedentary activity (n = 1) | Has identified alternative activities to sedentary time but not yet implemented them (n = 0) | Has reduced sedentary time (n = 0) | Has reduced sedentary time and can identify one observable benefit (n = 0) | −1.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grace, J.; Walters, S.T.; Gallegos, I.; Thompson, E.L.; Spence, E.E. Use of a Health Advocacy Model for Survivors of Interpersonal Violence. Int. J. Environ. Res. Public Health 2020, 17, 8966. https://doi.org/10.3390/ijerph17238966
Grace J, Walters ST, Gallegos I, Thompson EL, Spence EE. Use of a Health Advocacy Model for Survivors of Interpersonal Violence. International Journal of Environmental Research and Public Health. 2020; 17(23):8966. https://doi.org/10.3390/ijerph17238966
Chicago/Turabian StyleGrace, Jessica, Scott T. Walters, Irene Gallegos, Erika L. Thompson, and Emily E. Spence. 2020. "Use of a Health Advocacy Model for Survivors of Interpersonal Violence" International Journal of Environmental Research and Public Health 17, no. 23: 8966. https://doi.org/10.3390/ijerph17238966
APA StyleGrace, J., Walters, S. T., Gallegos, I., Thompson, E. L., & Spence, E. E. (2020). Use of a Health Advocacy Model for Survivors of Interpersonal Violence. International Journal of Environmental Research and Public Health, 17(23), 8966. https://doi.org/10.3390/ijerph17238966





