Creative Music Therapy with Premature Infants and Their Parents: A Mixed-Method Pilot Study on Parents’ Anxiety, Stress and Depressive Symptoms and Parent–Infant Attachment
Abstract
1. Introduction
2. Materials and Methods
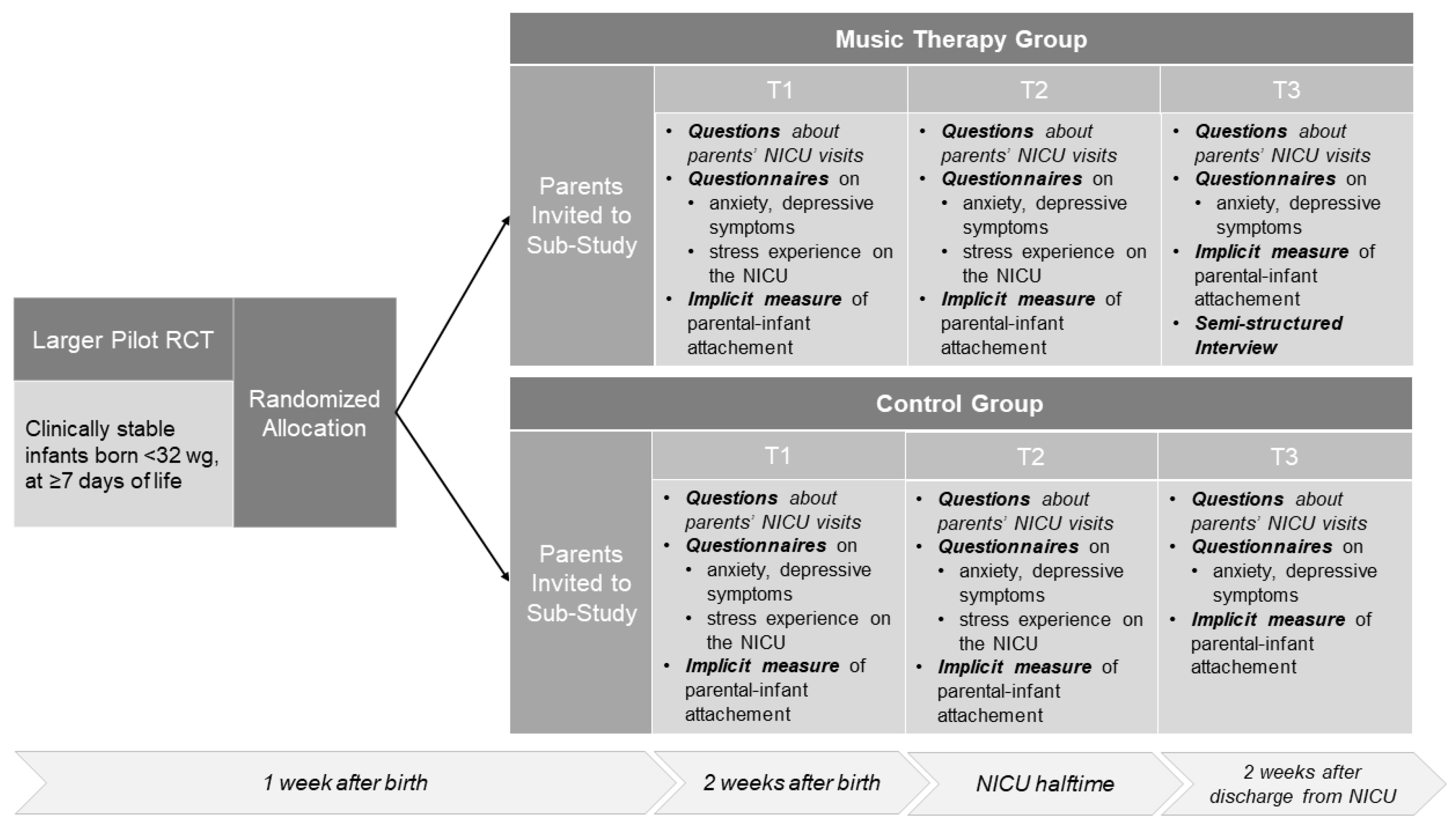
2.1. Overview
2.2. Participants
2.3. Intervention
2.4. Data Acquisition
2.5. Psychological Measures
2.6. Statistical Analysis
2.7. Qualitative Analysis
3. Results
3.1. Sample Characteristics
3.2. Results of the Quantitative Analyses
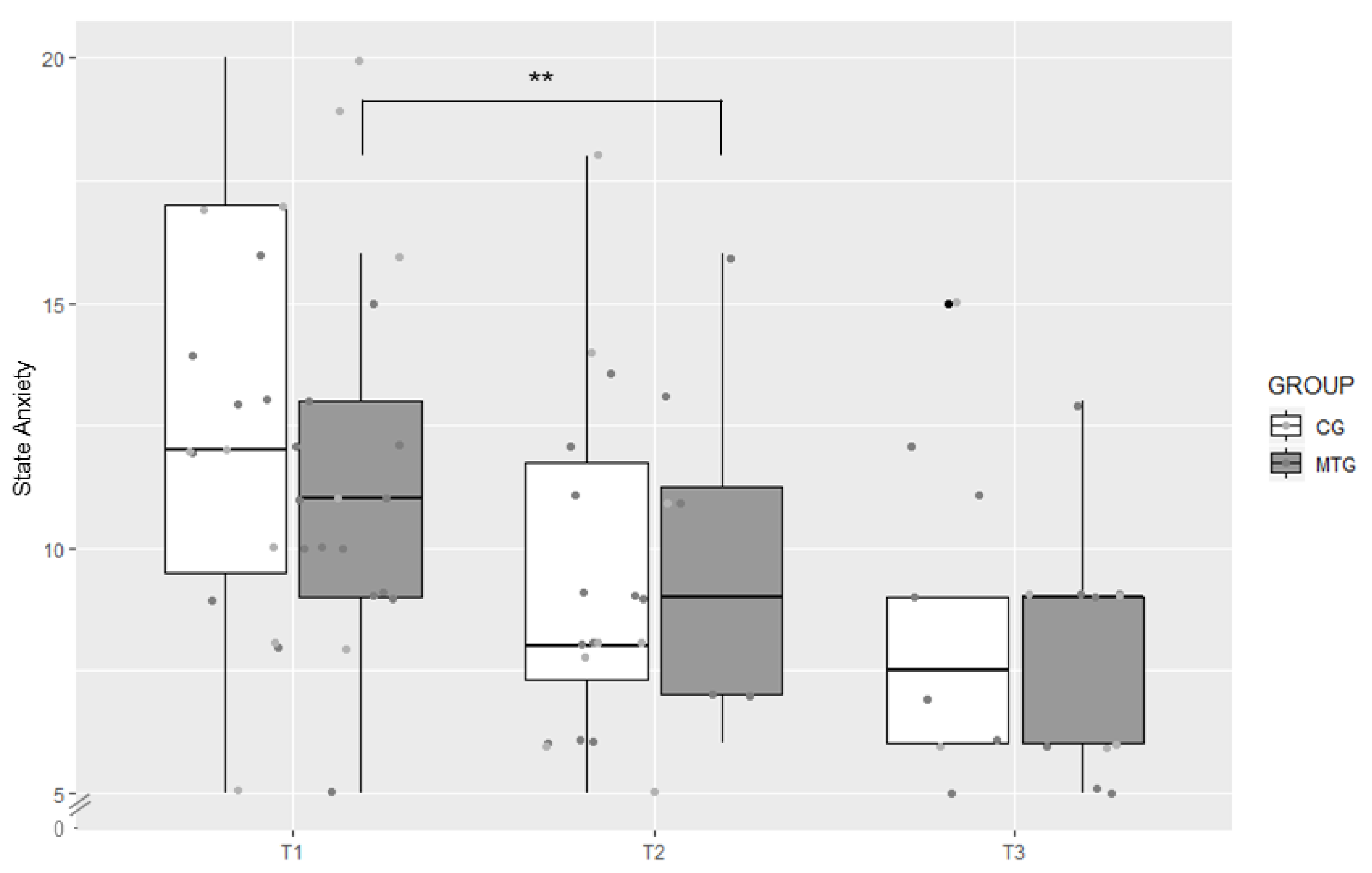
3.2.1. Symptoms of Anxiety
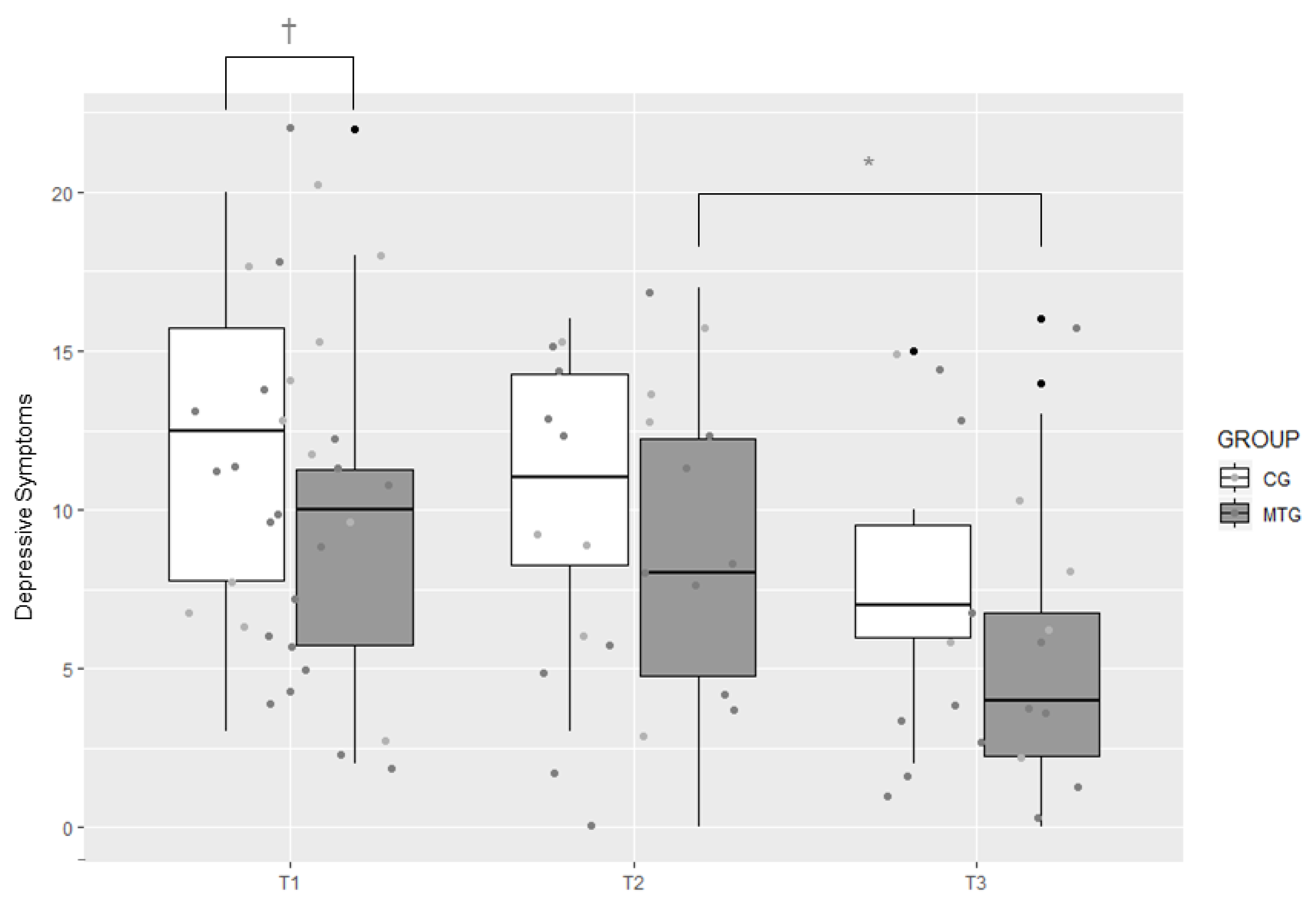
3.2.2. Symptoms of Depression
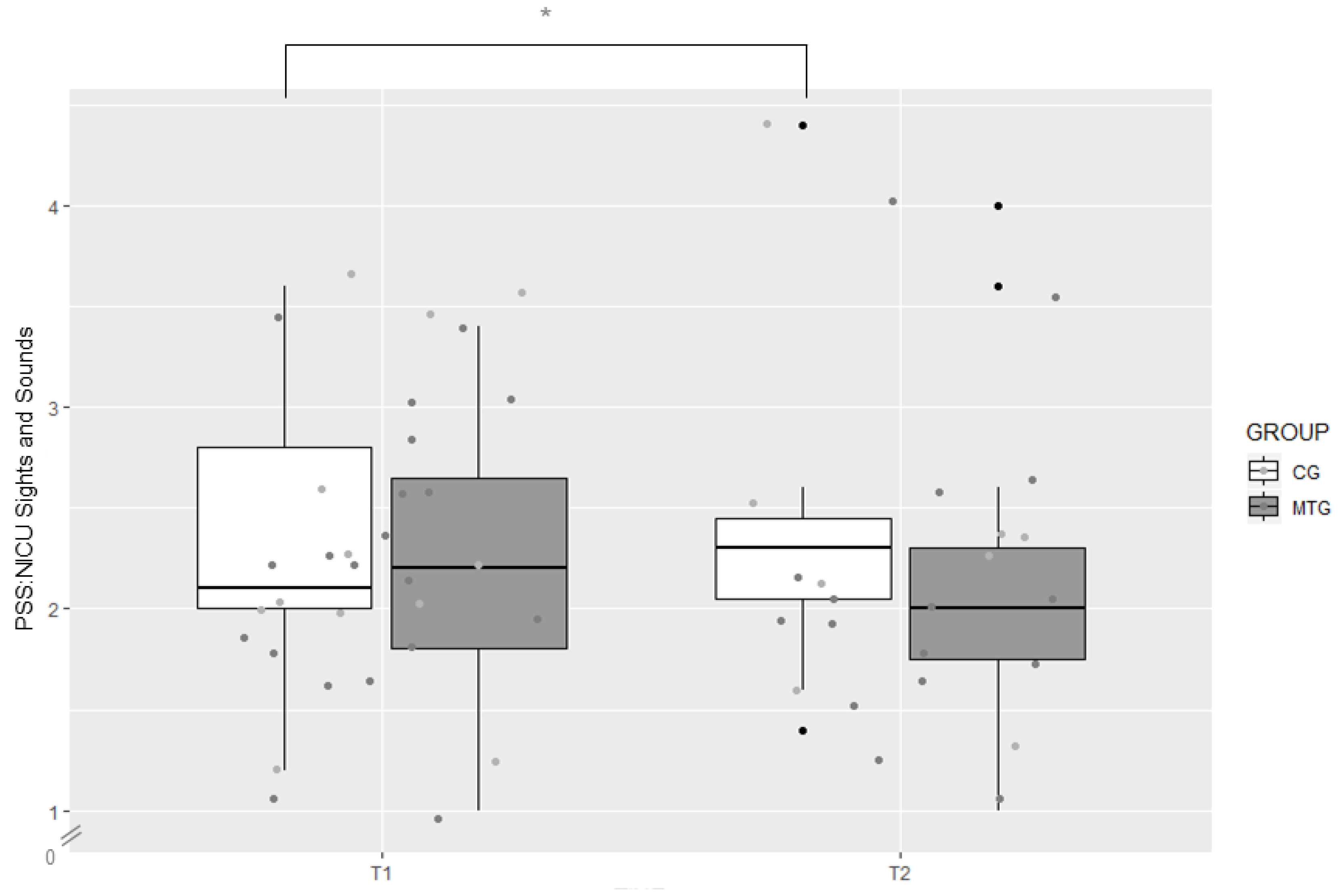
3.2.3. Symptoms of Stress
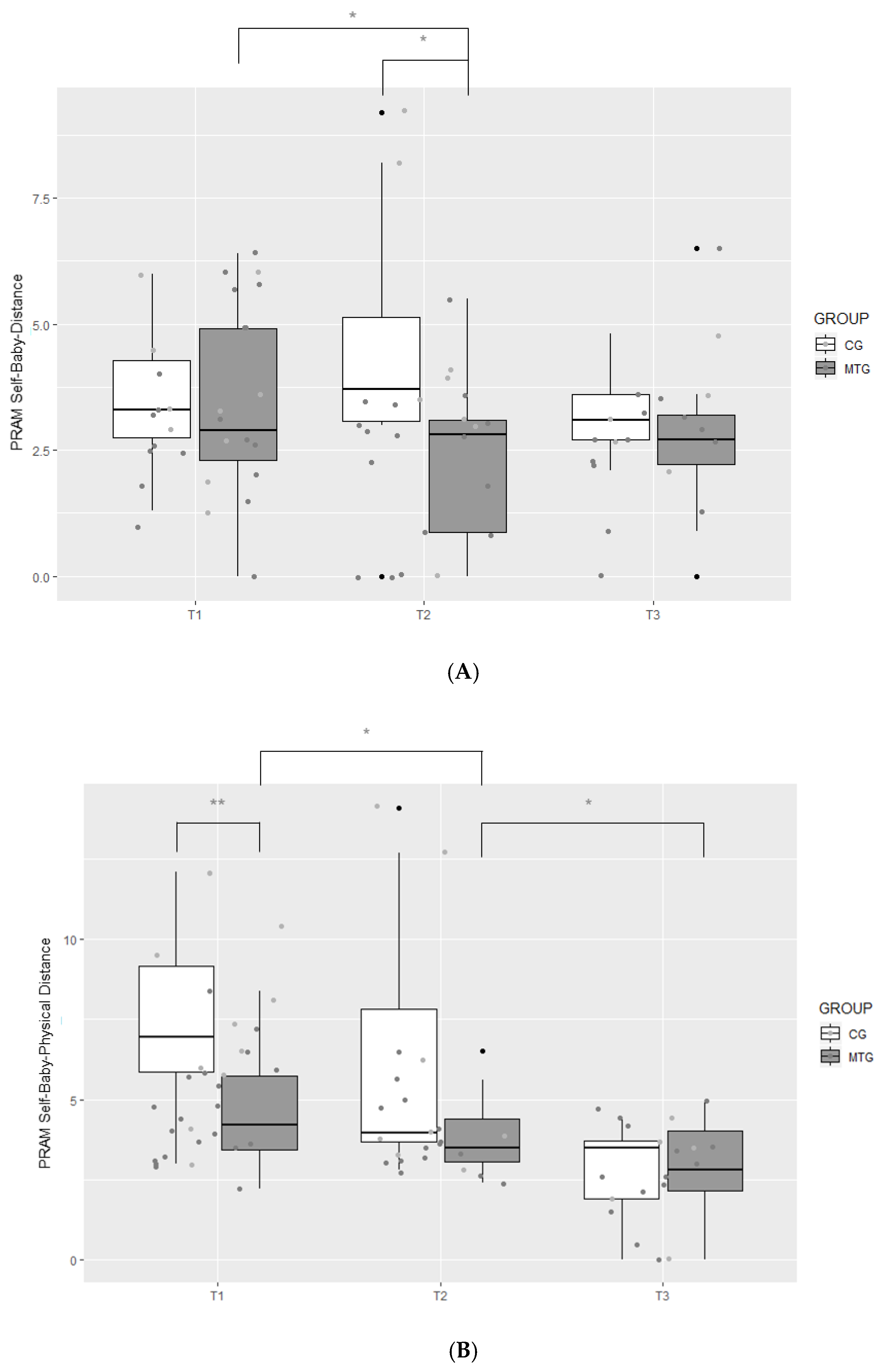
3.2.4. Attachment
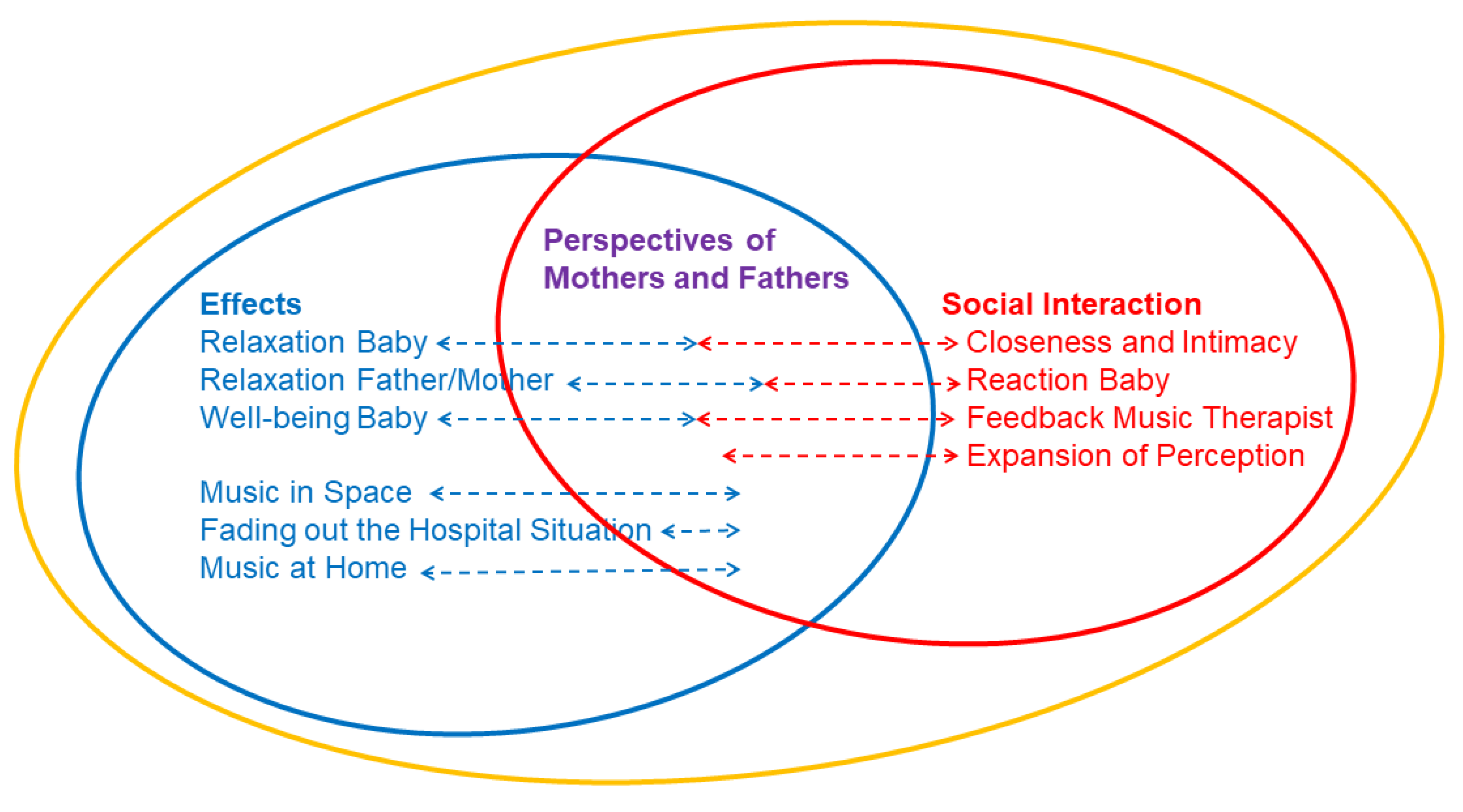
3.3. Results of the Qualitative Analysis
“I have the feeling that he could let himself go. He was so relaxed on top of me and had a satisfied expression to me […].”(M49)
“He had quite a lot of [oxygen] decreases at the beginning and with the music, he really never had any decreases when I was there. That was always reassuring for me, just that it was good for him—I really have the feeling that it was good for him.”(M55)
“That was the moment when you just could relax. I could never do that usually […] Just us—for me, it was really our moment.”(M72)
“You could relax; you also forgot that you are not alone here with S. [daughter] […] You didn’t hear or see the monitors anymore, she [the music therapist] was always watching.”(M72)
“At the IMC [Intermediate Care], you really noticed when music therapy took place. Everyone was relaxed, all caregivers […] It immediately became quiet on the unit. It was radiant.”(M72)
“Now I sing with a feeling that it will surely do him good. I don’t know if I would have perceived it that way before.”(M49)
“I take home with me that we increasingly sing and hum with him […] and not that you have to be a professional musician or a professional singer to sing something to him […] he doesn’t care if you sing out of tune. The most important thing is music.”(M48)
“Yes, you feel more as one, because of the monochord. I can feel the vibrations that go through me to him and the humming in addition—I felt I was more united.”(M48)
“For me, it simply wasn’t so natural in our situation and I was then [during CMT] allowed to simply observe L. [son]—and even a little—get to know him better and also get to know him differently during this time of music therapy.”(M62)
“That [CMT] was always a real highlight. Not only for L. [son]. The music therapist said, he always reacted very well. She explained to me what she saw and then I could observe it […] It also always reassured me and it was good for me, very good.”(M62)
“I enjoy it, also the instrument [bought an instrument for home use after the experience with CMT]. It is a beautiful wooden instrument. I find it a good thing.”(V48)
“Yes, we sing and hum a lot with her [daughter] […] As soon as she is with her daddy in the evening and he begins to hum, she is just quiet. She needs that, she is used to it.”(M72)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Marcos, Z. Arriving too early. Lancet Neurol. 2013, 12, 332–333. [Google Scholar] [CrossRef]
- Als, H.; McAnulty, G.B. The Newborn Individualized Developmental Care and Assessment Program (NIDCAP) with Kangaroo Mother Care (KMC): Comprehensive Care for Preterm Infants. Curr. Womens Health Rev. 2011, 7, 288–301. [Google Scholar] [CrossRef]
- Jotzo, M.; Poets, C.F. Helping parents cope with the trauma of premature birth: An evaluation of a trauma-preventive psychological intervention. Pediatrics 2005, 115, 915–919. [Google Scholar] [CrossRef] [PubMed]
- Trumello, C.; Candelori, C.; Cofini, M.; Cimino, S.; Cerniglia, L.; Paciello, M.; Babore, A. Mothers’ Depression, Anxiety, and Mental Representations After Preterm Birth: A Study During the Infant’s Hospitalization in a Neonatal Intensive Care Unit. Front. Public Health 2018, 6, 359. [Google Scholar] [CrossRef] [PubMed]
- Franck, L.S.; Cox, S.; Allen, A.; Winter, I. Measuring neonatal intensive care unit-related parental stress. J. Adv. Nurs. 2005, 49, 608–615. [Google Scholar] [CrossRef] [PubMed]
- Cruz, M.D.; Fernandes, A.M.; Oliveira, C.R. Epidemiology of painful procedures performed in neonates: A systematic review of observational studies. Eur. J. Pain 2016, 20, 489–498. [Google Scholar] [CrossRef]
- Balice-Bourgois, C.; Zumstein-Shaha, M.; Vanoni, F.; Jaques, C.; Newman, C.J.; Simonetti, G.D. A Systematic Review of Clinical Practice Guidelines for Acute Procedural Pain on Neonates. Clin. J. Pain 2020, 36, 390–398. [Google Scholar] [CrossRef]
- Eccleston, C.; Fisher, E.; Howard, R.F.; Slater, R.; Forgeron, P.; Palermo, T.M.; Birnie, K.A.; Anderson, B.J.; Chambers, C.T.; Crombez, G.; et al. Delivering transformative action in paediatric pain: A Lancet Child & Adolescent Health Commission. Lancet Child. Adolesc. Health 2021, 5, 47–87. [Google Scholar] [CrossRef]
- Shah, P.; Siu, A. Considerations for neonatal and pediatric pain management. Am. J. Health Syst. Pharm. 2019, 76, 1511–1520. [Google Scholar] [CrossRef]
- Kyololo, O.M.; Stevens, B.J.; Songok, J. Mothers’ Perceptions about Pain in Hospitalized Newborn Infants in Kenya. J. Pediatric Nurs. 2019, 47, 51–57. [Google Scholar] [CrossRef]
- Bruns-Neumann, E. How do parents experience the premature birth of their child? Pflege 2006, 19, 146–155. [Google Scholar] [CrossRef] [PubMed]
- Schappin, R.; Wijnroks, L.; Uniken Venema, M.M.; Jongmans, M.J. Rethinking stress in parents of preterm infants: A meta-analysis. PLoS ONE 2013, 8, e54992. [Google Scholar] [CrossRef] [PubMed]
- Ionio, C.; Colombo, C.; Brazzoduro, V.; Mascheroni, E.; Confalonieri, E.; Castoldi, F.; Lista, G. Mothers and Fathers in NICU: The Impact of Preterm Birth on Parental Distress. Eur. J. Psychol. 2016, 12, 604–621. [Google Scholar] [CrossRef] [PubMed]
- Winter, L.; Colditz, P.B.; Sanders, M.R.; Boyd, R.N.; Pritchard, M.; Gray, P.H.; Whittingham, K.; Forrest, K.; Leeks, R.; Webb, L.; et al. Depression, posttraumatic stress and relationship distress in parents of very preterm infants. Arch. Womens Ment. Health 2018, 21, 445–451. [Google Scholar] [CrossRef]
- Kommers, D.; Oei, G.; Chen, W.; Feijs, L.; Bambang Oetomo, S. Suboptimal bonding impairs hormonal, epigenetic and neuronal development in preterm infants, but these impairments can be reversed. Acta Paediatr. 2016, 105, 738–751. [Google Scholar] [CrossRef]
- Feldman, R.; Eidelman, A.I. Maternal postpartum behavior and the emergence of infant-mother and infant-father synchrony in preterm and full-term infants: The role of neonatal vagal tone. Dev. Psychobiol. 2007, 49, 290–302. [Google Scholar] [CrossRef]
- Forcada-Guex, M.; Borghini, A.; Pierrehumbert, B.; Ansermet, F.; Muller-Nix, C. Prematurity, maternal posttraumatic stress and consequences on the mother-infant relationship. Early Hum. Dev. 2011, 87, 21–26. [Google Scholar] [CrossRef]
- Korja, R.; Savonlahti, E.; Ahlqvist-Björkroth, S.; Stolt, S.; Haataja, L.; Lapinleimu, H.; Piha, J.; Lehtonen, L.; PIPARI Study Group. Maternal depression is associated with mother-infant interaction in preterm infants. Acta Paediatr. 2008, 97, 724–730. [Google Scholar] [CrossRef]
- Udry-Jørgensen, L.; Pierrehumbert, B.; Borghini, A.; Habersaat, S.; Forcada-Guex, M.; Ansermet, F.; Muller-Nix, C. Quality of attachment, perinatal risk, and mother-infant interaction in a high-risk premature sample. Infant Ment. Health J. 2011, 32, 305–318. [Google Scholar] [CrossRef]
- Hofer, M.A. Psychobiological roots of early attachment. Curr. Dir. Psychol. Sci. 2006, 15, 84–88. [Google Scholar] [CrossRef]
- Borghini, A.; Habersaat, S.; Forcada-Guex, M.; Nessi, J.; Pierrehumbert, B.; Ansermet, F.; Müller-Nix, C. Effects of an early intervention on maternal post-traumatic stress symptoms and the quality of mother-infant interaction: The case of preterm birth. Infant Behav. Dev. 2014, 37, 624–631. [Google Scholar] [CrossRef] [PubMed]
- Benzies, K.M.; Magill-Evans, J.E.; Hayden, K.A.; Ballantyne, M. Key components of early intervention programs for preterm infants and their parents: A systematic review and meta-analysis. BMC Pregnancy Childbirth 2013, 13 (Suppl. 1), S10. [Google Scholar] [CrossRef] [PubMed]
- Haslbeck, F.B.; Bassler, D. Clinical Practice Protocol of Creative Music Therapy for Preterm Infants and Their Parents in the Neonatal Intensive Care Unit. J. Vis. Exp. 2020, 155, e60412. [Google Scholar] [CrossRef]
- Haslbeck, F.B.; Hugoson, P. Sounding together: Family centered music therapy as facilitator for parental singing during skin-to-skin contact. In Early Vocal Contact and Preterm Infant Brain Development; Filippa, M., Kuhn, P., Westrup, B., Eds.; Springer Nature: Berlin, Germany, 2017; pp. 217–238. ISBN 978-33-1965-075-3. [Google Scholar]
- Haslbeck, F.B. The interactive potential of creative music therapy with premature infants and their parents: A qualitative analysis. Nord. J. Music Ther. 2014, 23, 36–70. [Google Scholar] [CrossRef]
- Nordoff, P.; Robbins, C. Creative Music Therapy: Individualized Treatment for the Handicapped Child; John Day Company: New York, NY, USA, 1977; ISBN 978-03-8197-100-7. [Google Scholar]
- Aldridge, D.; Gustorff, D.; Hannich, H.J. Where am I? Music therapy applied to coma patients. J. R. Soc. Med. 1990, 83, 345–346. [Google Scholar] [CrossRef] [PubMed]
- Haslbeck, F.B. Creative music therapy with premature infants: An analysis of video footage. Nord. J. Music Ther. 2014, 23, 5–35. [Google Scholar] [CrossRef]
- Haslbeck, F.B.; Jakab, A.; Held, U.; Bassler, D.; Bucher, H.U.; Hagmann, C. Creative music therapy to promote brain function and brain structure in preterm infants: A randomized controlled pilot study. Neuroimage Clin. 2020, 25, 102171. [Google Scholar] [CrossRef]
- Bieleninik, Ł.; Ghetti, C.; Gold, C. Music Therapy for Preterm Infants and Their Parents: A Meta-analysis. Pediatrics 2016, 138, e20160971. [Google Scholar] [CrossRef]
- Ettenberger, M.; Rojas Cárdenas, C.; Parker, M.; Odell-Miller, H. Family-centred music therapy with preterm infants and their parents in the Neonatal Intensive Care Unit (NICU) in Colombia—A mixed-methods study. Nord. J. Music Ther. 2017, 26, 207–234. [Google Scholar] [CrossRef]
- Arnon, S.; Diamant, C.; Bauer, S.; Regev, R.; Sirota, G.; Litmanovitz, I. Maternal singing during kangaroo care led to autonomic stability in preterm infants and reduced maternal anxiety. Acta Paediatr. 2014, 103, 1039–1044. [Google Scholar] [CrossRef]
- Schlez, A.; Litmanovitz, I.; Bauer, S.; Dolfin, T.; Regev, R.; Arnon, S. Combining kangaroo care and live harp music therapy in the neonatal intensive care unit setting. Isr. Med. Assoc. J. 2011, 13, 354–358. [Google Scholar] [PubMed]
- Haslbeck, F.B.; Bucher, H.U.; Bassler, D.; Hagmann, C. Creative music therapy to promote brain structure, function and neurobehavioral outcomes in preterm infants: A randomized controlled pilot trial protocol. Pilot Feasibility Stud. 2017, 3, 36. [Google Scholar] [CrossRef] [PubMed]
- Gidron, Y. Trait Anxiety. In Encyclopedia of Behavioral Medicine, 2nd ed.; Gellman, M., Turner, J., Eds.; Springer: New York, NY, USA, 2016. [Google Scholar] [CrossRef]
- Laux, L.; Glanzmann, P.; Schaffner, P.; Spielberger, C.D. Das Deutschsprachige State-Trait-Angstinventar; Beltz: Weinheim, Germany, 1981. [Google Scholar]
- Englert, C.; Bertrams, A.; Dickhäuser, O. Entwicklung der Fünf-Item-Kurzskala STAI-SKD zur Messung von Zustandsangst. Z. Gesundheitspsychol. 2011, 19, 173–180. [Google Scholar] [CrossRef]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef]
- Bergant, A.M.; Nguyen, T.; Heim, K.; Ulmer, H.; Dapunt, O. German language version and validation of the Edinburgh Postnatal Depression Scale. Dtsch. Med. Wochenschr. 1998, 123, 35–40. [Google Scholar] [CrossRef]
- Cox, J. Thirty years with the Edinburgh Postnatal Depression Scale: Voices from the past and recommendations for the future. Br. J. Psychiatry 2019, 214, 127–129. [Google Scholar] [CrossRef]
- Matthey, S.; Barnett, B.; Kavanagh, D.J.; Howie, P. Validation of the Edinburgh Postnatal Depression Scale for men, and comparison of item endorsement with their partners. J. Affect. Disord. 2001, 64, 175–184. [Google Scholar] [CrossRef]
- Miles, M.S.; Funk, S.G.; Carlson, J. Parental Stressor Scale: Neonatal intensive care unit. Nurs. Res. 1993, 42, 148–152. [Google Scholar] [CrossRef]
- Urlesberger, P.; Schienle, A.; Pichler, G.; Baik, N.; Schwaberger, B.; Urlesberger, B.; Pichler-Stachl, E. A new German Scale for Assessing Parental Stress after Preterm Birth. Z. Geburtshilfe Neonatol. 2017, 221, 81–87. [Google Scholar] [CrossRef]
- Pichler-Stachl, E.; Pichler, G.; Baik, N.; Urlesberger, B.; Alexander, A.; Urlesberger, P.; Cheung, P.Y.; Schmölzer, G.M. Maternal stress after preterm birth: Impact of length of antepartum hospital stay. Women Birth 2016, 29, e105–e109. [Google Scholar] [CrossRef]
- Van Bakel, H.J.A.; Maas, A.J.; Vreeswijk, C.M.; Vingerhoets, A.J.J.M. Pictorial representation of attachment: Measuring the parent-fetus relationship in expectant mothers and fathers. BMC Pregnancy Childbirth 2013, 13, 138. [Google Scholar] [CrossRef] [PubMed]
- Hoffenkamp, H.N.; Tooten, A.; Hall, R.A.S.; Croon, M.A.; Braeken, J.; Winkel, F.W.; Vingerhoets, A.J.J.M.; van Bakel, H.J.A. The impact of premature childbirth on parental bonding. Evol. Psychol. 2012, 10, 542–561. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Calkins, A.W.; Rogers, A.H.; Campbell, A.A.; Simon, N.M. Comorbidity of Anxiety and Depression. In Anxiety Disorders; Ressler, K.J., Pine, D.S., Rothbaum Olasov, B., Eds.; Oxford University Press: Oxford, UK, 2015; ISBN 978-019-939-512-5. [Google Scholar]
- Lamers, F.; van Oppen, P.; Comijs, H.C.; Smit, J.H.; Spinhoven, P.; van Balkom, A.J.L.M.; Nolen, W.A.; Zitman, F.G.; Beekman, A.T.F.; Penninx, B.W.J.H. Comorbidity Patterns of Anxiety and Depressive Disorders in a Large Cohort Study: The Netherlands Study of Depression and Anxiety (NESDA). J. Clin. Psychiatry 2011, 72, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Hayes-Skelton, S.A.; Roemer, L.; Orsillo, S.M.; Borkovec, T.D. A Contemporary View of Applied Relaxation for Generalized Anxiety Disorder. Cogn. Behav. Ther. 2013, 42, 292–302. [Google Scholar] [CrossRef] [PubMed]
| Music Therapy Group | Control Group | |
|---|---|---|
| Participants (n) | 20 | 12 |
| Couples (n) | 10 | 6 |
| Maternal age (years) (median (range)) | 31.50 (26.00–43.00) | 30.00 (27.00–35.00) |
| Marital status (% (n)) | ||
| Married | 50 (n = 10) | 58 (n = 7) |
| Unmarried | 50 (n = 10) | 42 (n = 5) |
| Cohabitating (% (n)) | 100 (n = 20) | 100 (n = 12) |
| Maternal nationality (% (n)) | ||
| Swiss | 90 (n = 9) | 50 (n = 3) |
| German | 10 (n = 1) | 17 (n = 1) |
| Jordanian | 17 (n = 1) | |
| Croatian | 17 (n = 1) | |
| Maternal language (% (n)) | ||
| German | 100 (n = 10) | 83 (n = 5) |
| Arabic | 17 (n = 1) | |
| Maternal educational qualification (% (n)) | ||
| Apprenticeship | 40 (n = 4) | 50 (n = 3) |
| University of applied sciences degree | 30 (n = 3) | |
| University degree | 30 (n = 3) | 50 (n = 3) |
| Paternal nationality (% (n)) | ||
| Swiss | 70 (n = 7) | 67 (n = 4) |
| German | 20 (n = 2) | 33 (n = 2) |
| Kosovar | 10 (n = 1) | |
| Paternal language (% (n)) | ||
| German | 90 (n = 9) | 100 (n = 6) |
| Albanian | 10 (n = 1) | |
| Paternal educational qualification (% (n)) | ||
| Apprenticeship | 60 (n = 6) | 50 (n = 3) |
| University of applied sciences degree | 10 (n = 1) | 17 (n = 1) |
| University degree | 30 (n = 3) | 33 (n = 2) |
| Primigravida (% (n)) | 80 (n = 8) | 67 (n = 4) |
| Primiparous (% (n)) | 80 (n = 8) | 67 (n = 4) |
| Sectio Caesarea (% (n)) | 100 (n = 10) | 100 (n = 6) |
| Total number of infants | 11 | 8 |
| Set of twins (% (n)) | 10 (n = 1) | 33 (n = 2) |
| Male infants (% (n)) | 82 (n = 9) | 50 (n = 4) |
| Gestational age at birth (weeks) (median (range)) | 28.43 (24.86–31.43) | 28.29 (25.00–29.00) |
| Birth weight (g) (median (range)) | 1070 (680–1590) | 785.00 (600–1310) |
| Birth size (cm) (median (range)) | 38.00 (33.00–43.00) | 34.50 (32.00–39.00) |
| Apgar score (10 min) (median (range)) | 10 (7–10) | 9 (6–10) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kehl, S.M.; La Marca-Ghaemmaghami, P.; Haller, M.; Pichler-Stachl, E.; Bucher, H.U.; Bassler, D.; Haslbeck, F.B. Creative Music Therapy with Premature Infants and Their Parents: A Mixed-Method Pilot Study on Parents’ Anxiety, Stress and Depressive Symptoms and Parent–Infant Attachment. Int. J. Environ. Res. Public Health 2021, 18, 265. https://doi.org/10.3390/ijerph18010265
Kehl SM, La Marca-Ghaemmaghami P, Haller M, Pichler-Stachl E, Bucher HU, Bassler D, Haslbeck FB. Creative Music Therapy with Premature Infants and Their Parents: A Mixed-Method Pilot Study on Parents’ Anxiety, Stress and Depressive Symptoms and Parent–Infant Attachment. International Journal of Environmental Research and Public Health. 2021; 18(1):265. https://doi.org/10.3390/ijerph18010265
Chicago/Turabian StyleKehl, Selina M., Pearl La Marca-Ghaemmaghami, Marina Haller, Elisabeth Pichler-Stachl, Hans Ulrich Bucher, Dirk Bassler, and Friederike B. Haslbeck. 2021. "Creative Music Therapy with Premature Infants and Their Parents: A Mixed-Method Pilot Study on Parents’ Anxiety, Stress and Depressive Symptoms and Parent–Infant Attachment" International Journal of Environmental Research and Public Health 18, no. 1: 265. https://doi.org/10.3390/ijerph18010265
APA StyleKehl, S. M., La Marca-Ghaemmaghami, P., Haller, M., Pichler-Stachl, E., Bucher, H. U., Bassler, D., & Haslbeck, F. B. (2021). Creative Music Therapy with Premature Infants and Their Parents: A Mixed-Method Pilot Study on Parents’ Anxiety, Stress and Depressive Symptoms and Parent–Infant Attachment. International Journal of Environmental Research and Public Health, 18(1), 265. https://doi.org/10.3390/ijerph18010265






