Mapping Assessments Instruments for Headache Disorders against the ICF Biopsychosocial Model of Health and Disability
Abstract
1. Introduction
2. Materials and Methods
3. Results
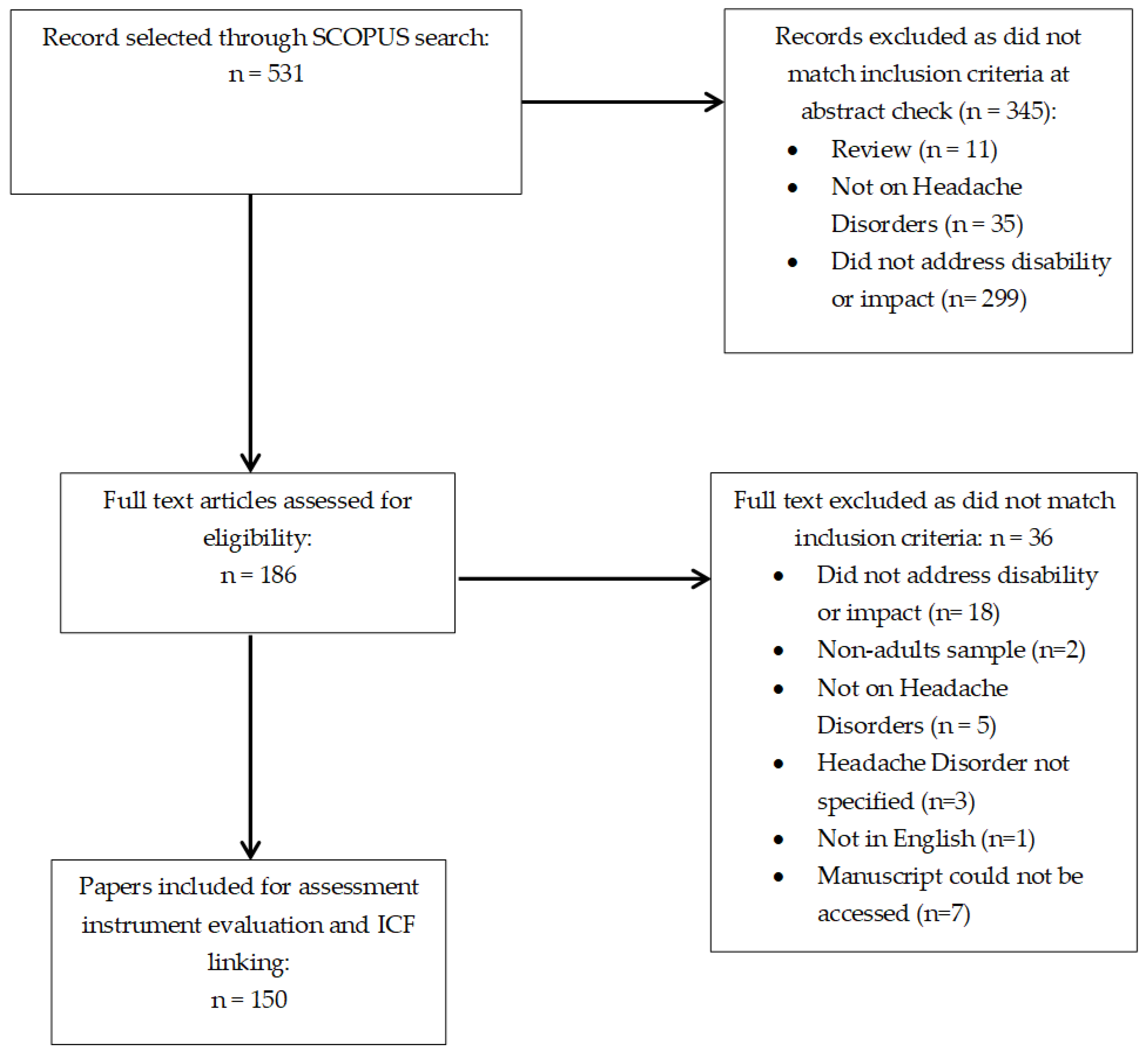
3.1. Overview of Literature Search
3.2. Assessment Instruments Used in Migraine, TTH, and CH Research
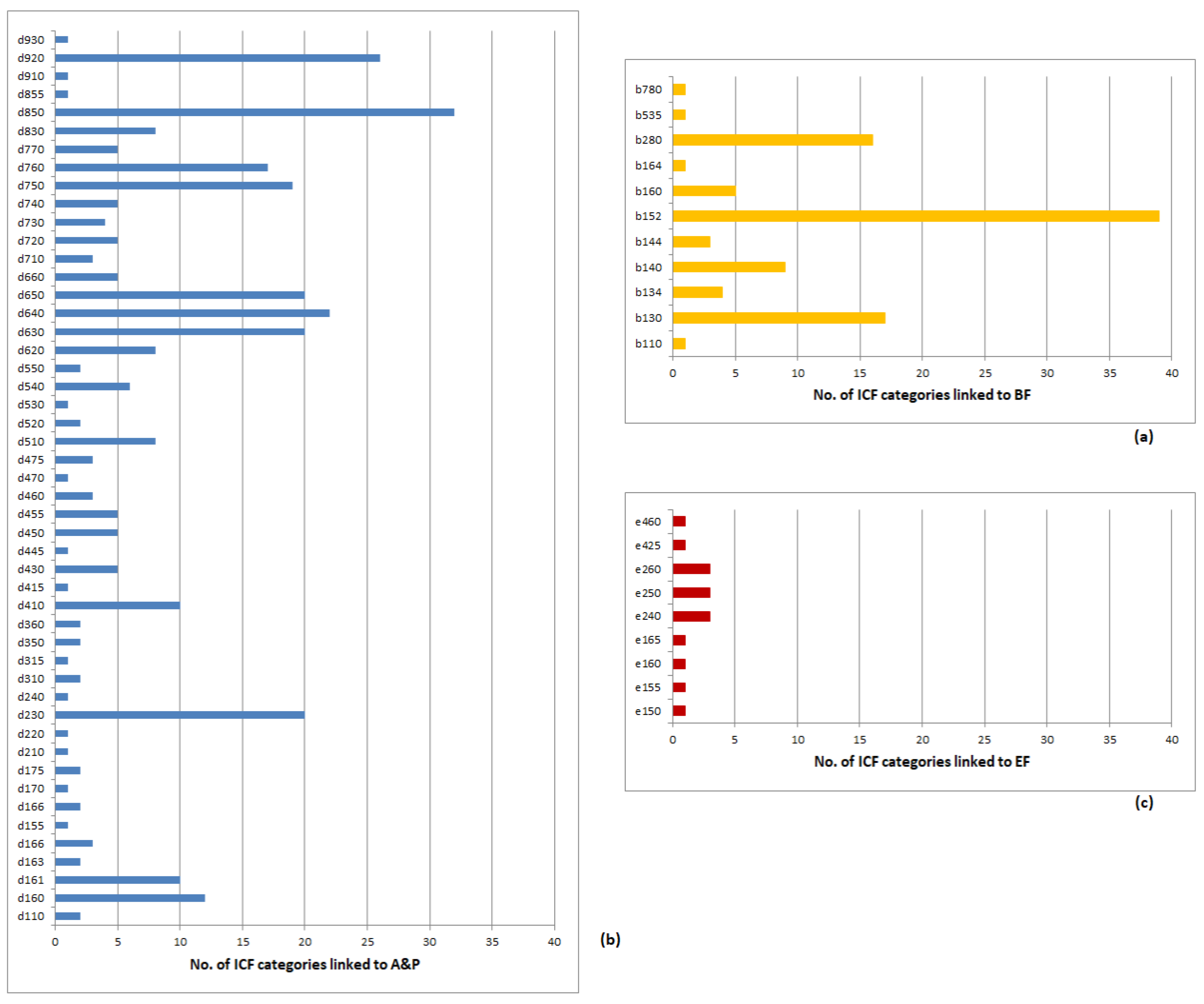
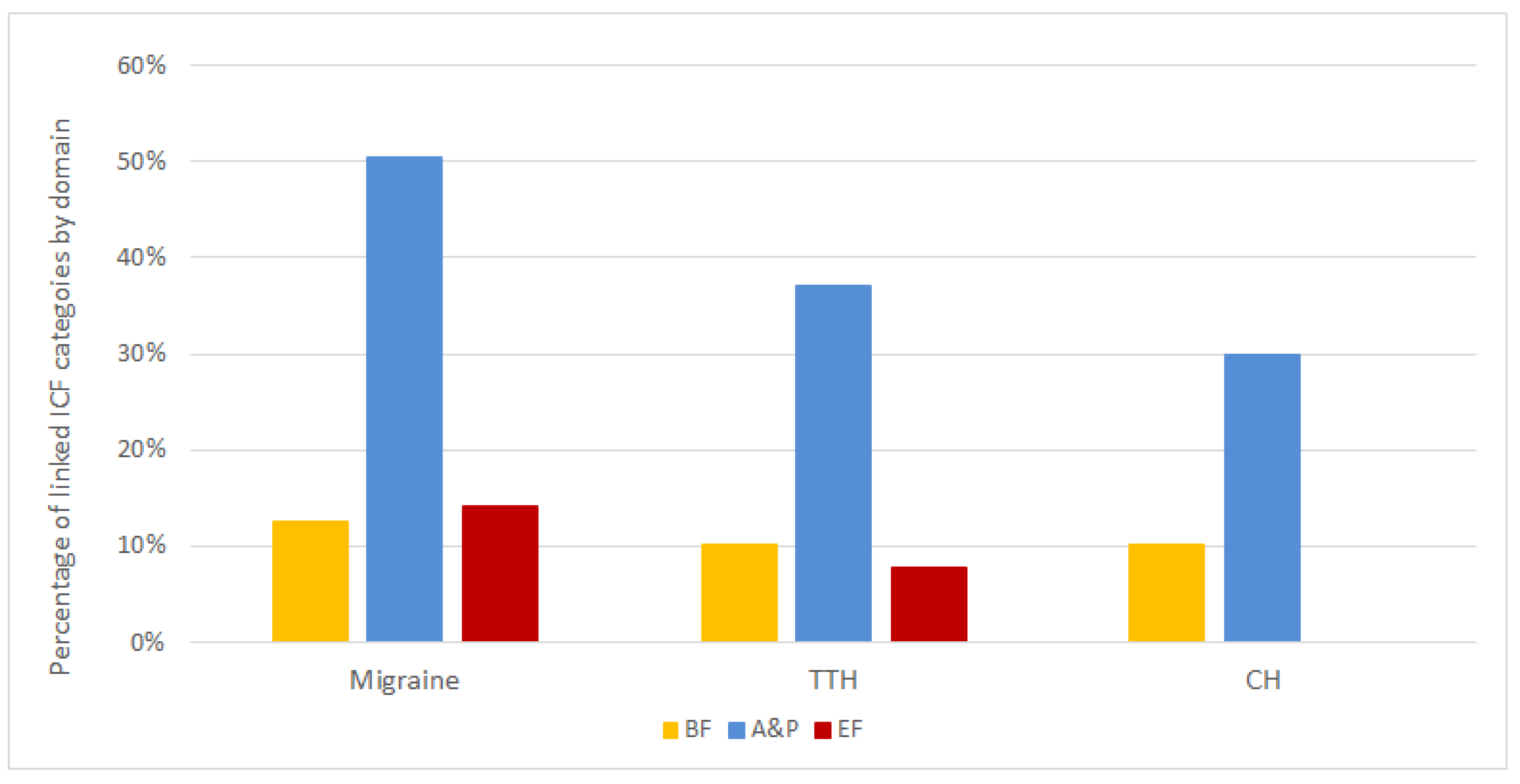
3.3. Common and Disease-Specific Elements of Functioning Covered by the Assessment Instruments
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef]
- GBD 2017 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1859–1922. [Google Scholar] [CrossRef]
- Raggi, A.; Giovannetti, A.M.; Quintas, R.; D’Amico, D.; Cieza, A.; Sabariego, C.; Bickenbach, J.E.; Leonardi, M. A systematic review of the psychosocial difficulties relevant to patients with migraine. J. Headache Pain 2012, 13, 595–606. [Google Scholar] [CrossRef]
- Raggi, A.; Covelli, V.; Leonardi, M.; Grazzi, L.; Curone, M.; D’Amico, D. Difficulties in work-related activities among migraineurs are scarcely collected: Results from a literature review. Neurol. Sci. 2014, 35, 23–26. [Google Scholar] [CrossRef]
- Leonardi, M.; Raggi, A. A narrative review on the burden of migraine: When the burden is the impact on people’s life. J. Headache Pain 2019, 20, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Stewart, W.F.; Lipton, R.B.; Kolodner, K.; Liberman, J.; Sawyer, J. Reliability of the Migraine Disability Assessment Score in A Population-Based Sample of Headache Sufferers. Cephalalgia 1999, 19, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Kosinski, M.R.; Bayliss, M.; Bjorner, J.; Ware, J.E., Jr.; Garber, W.; Batenhorst, A.; Cady, R.; Dahlöf, C.; Dowson, A.; Tepper, S. A six-item short-form survey for measuring headache impact: The HIT-6™. Qual. Life Res. 2003, 12, 963–974. [Google Scholar] [CrossRef] [PubMed]
- Martin, B.C.; Pathak, D.S.; Sharfman, M.I.; Adelman, J.U.; Taylor, F.R.; Kwong, W.J.; Jhingran, P. Validity and reliability of the migraine-specific quality of life questionnaire (MSQ Version 2.1). Headache J. Head Face Pain 2000, 40, 204–216. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, D.; Raggi, A.; Grazzi, L.; Lambru, G. Disability, Quality of Life, and Socioeconomic Burden of Cluster Headache: A Critical Review of Current Evidence and Future Perspectives. Headache J. Head Face Pain 2020, 60, 809–818. [Google Scholar] [CrossRef] [PubMed]
- May, A.; Leone, M.; Áfra, J.; Linde, M.; Sándor, P.S.; Evers, S.; Goadsby, P.J. EFNS guidelines on the treatment of cluster headache and other trigeminal-autonomic cephalalgias. Eur. J. Neurol. 2006, 13, 1066–1077. [Google Scholar] [CrossRef]
- Martelletti, P.; Jensen, R.; Antal, A.; Arcioni, R.; Brighina, F.; De Tommaso, M.; Franzini, A.; Fontaine, D.; Heiland, M.; Jürgens, T.P.; et al. Neuromodulation of chronic headaches: Position statement from the European Headache Federation. J. Headache Pain 2013, 14, 86. [Google Scholar] [CrossRef] [PubMed]
- Raggi, A.; Grazzi, L.; Grignani, E.; Leonardi, M.; Sansone, E.; Scaratti, C.; D’Amico, D. The use of MIDAS in patients with chronic migraine and medication-overuse headache: Should we trust it? Neurol. Sci. 2018, 39, 125–127. [Google Scholar] [CrossRef]
- WHO. International Classification of Functioning, Disability and Health: ICF; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Cabello, M.; Mellor-Marsá, B.; Sabariego, C.; Cieza, A.; Bickenbach, J.; Ayuso-Mateos, J.L. Psychosocial features of depression: A systematic literature review. J. Affect. Disord. 2012, 141, 22–33. [Google Scholar] [CrossRef]
- Świtaj, P.; Anczewska, M.; Chrostek, A.; Sabariego, C.; Cieza, A.; Bickenbach, J.; Chatterji, S. Disability and schizophrenia: A systematic review of experienced psychosocial difficulties. BMC Psychiatry 2012, 12, 193. [Google Scholar] [CrossRef]
- Levola, J.; Kaskela, T.; Holopainen, A.; Sabariego, C.; Tourunen, J.; Cieza, A.; Pitkänen, T. Psychosocial difficulties in alcohol dependence: A systematic review of activity limitations and participation restrictions. Disabil. Rehabil. 2013, 36, 1227–1239. [Google Scholar] [CrossRef]
- Quintas, R.; Raggi, A.; Giovannetti, A.M.; Pagani, M.; Sabariego, C.; Cieza, A.; Leonardi, M. Psychosocial difficulties in people with epilepsy: A systematic review of literature from 2005 until 2010. Epilepsy Behav. 2012, 25, 60–67. [Google Scholar] [CrossRef]
- Cieza, A.; Geyh, S.; Chatterji, S.; Kostanjsek, N.; Üstün, B.; Stucki, G. ICF linking rules: An update based on lessons learned. J. Rehabil. Med. 2005, 37, 212–218. [Google Scholar] [CrossRef]
- Renner, T.; Sollmann, N.; Heinen, F.; Albers, L.; Trepte-Freisleder, F.; Klose, B.; König, H.; Krieg, S.M.; Bonfert, M.V.; Landgraf, M.N. Alleviation of migraine symptoms by application of repetitive peripheral magnetic stimulation to myofascial trigger points of neck and shoulder muscles—A randomized trial. Sci. Rep. 2020, 10, 1–11. [Google Scholar] [CrossRef]
- Sohn, J.-H.; Park, J.-W.; Lee, M.J.; Chung, P.-W.; Chu, M.K.; Chung, J.M.; Ahn, J.-Y.; Kim, B.-K.; Kim, S.-K.; Choi, Y.-J.; et al. Clinical factors influencing the impact of cluster headache from a prospective multicenter study. Sci. Rep. 2020, 10, 1–7. [Google Scholar] [CrossRef]
- Griauzdaitė, K.; Maselis, K.; Žvirblienė, A.; Vaitkus, A.; Jančiauskas, D.; Banaitytė-Baleišienė, I.; Kupčinskas, L.; Rastenytė, D. Associations between migraine, celiac disease, non-celiac gluten sensitivity and activity of diamine oxidase. Med. Hypotheses 2020, 142, 109738. [Google Scholar] [CrossRef]
- Seminowicz, D.A.; Burrowes, S.A.; Kearson, A.; Zhang, J.; Krimmel, S.R.; Samawi, L.; Furman, A.J.; Keaser, M.L.; Gould, N.F.; Magyari, T.; et al. Enhanced mindfulness-based stress reduction in episodic migraine. Pain 2020, 161, 1837–1846. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Fernández, A.; Vega, M.R.; Quintas, S.; Heras, M.D.T.; De Terán, J.D.; González, G.L.; García, O.T.; Vivancos, J.; Gago-Veiga, A. Psychosocial repercussion of migraine: Is it a stigmatized disease? Neurol. Sci. 2020, 41, 2207–2213. [Google Scholar] [CrossRef] [PubMed]
- Fuensalida-Novo, S.; Parás-Bravo, P.; Jiménez-Antona, C.; Castaldo, M.; Wang, K.; Benito-González, E.; Arendt-Nielsen, L.; Fernández-De-Las-Peñas, C. Gender differences in clinical and psychological variables associated with the burden of headache in tension-type headache. Women Health 2019, 60, 652–663. [Google Scholar] [CrossRef] [PubMed]
- Khorsha, F.; Mirzababaei, A.; Togha, M.; Mirzaei, K. Association of drinking water and migraine headache severity. J. Clin. Neurosci. 2020, 77, 81–84. [Google Scholar] [CrossRef]
- Ba, J.J.; Ye, W.; Nichols, R.; Jackson, J.; Cotton, S.; Joshi, S. A Real-World Analysis of Patient Characteristics, Treatment Patterns, and Level of Impairment in Patients with Migraine Who are Insufficient Responders vs Responders to Acute Treatment. Headache J. Head Face Pain 2020, 60, 1325–1339. [Google Scholar] [CrossRef]
- Gibbs, S.N.; Shah, S.; Deshpande, C.G.; Bensink, M.E.; Broder, M.S.; Ba, P.K.D.; Buse, D.C.; Vo, P.; Schwedt, T.J. United States Patients’ Perspective of Living with Migraine: Country-Specific Results from the Global “My Migraine Voice” Survey. Headache J. Head Face Pain 2020, 60, 1351–1364. [Google Scholar] [CrossRef]
- Delussi, M.; Vecchio, E.; Libro, G.; Quitadamo, S.; De Tommaso, M. Failure of preventive treatments in migraine: An observational retrospective study in a tertiary headache center. BMC Neurol. 2020, 20, 1–12. [Google Scholar] [CrossRef]
- Russo, A.; Silvestro, M.; Di Clemente, F.S.; Trojsi, F.; Bisecco, A.; Bonavita, S.; Tessitore, A.; Tedeschi, G. Multidimensional assessment of the effects of erenumab in chronic migraine patients with previous unsuccessful preventive treatments: A comprehensive real-world experience. J. Headache Pain 2020, 21, 1–14. [Google Scholar] [CrossRef]
- Wong, L.P.; Alias, H.; Bhoo-Pathy, N.; Chung, I.; Chong, Y.C.; Kalra, S.; Shah, Z.U.B.S. Impact of migraine on workplace productivity and monetary loss: A study of employees in banking sector in Malaysia. J. Headache Pain 2020, 21, 1–11. [Google Scholar] [CrossRef]
- Minen, M.T.; Jalloh, A.; De Dhaem, O.B.; Seng, E. Behavioral Therapy Preferences in People with Migraine. Headache J. Head Face Pain 2020, 60, 1093–1102. [Google Scholar] [CrossRef]
- Kumar, A.; Bhatia, R.; Sharma, G.; Dhanlika, D.; Vishnubhatla, S.; Singh, R.K.; Dash, D.; Tripathi, M.; Srivastava, M.P. Effect of yoga as add-on therapy in migraine (CONTAIN). Neurology 2020, 94, e2203–e2212. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, L.; Khan, N.; Dobson, J.; Randall, M.; Idrovo, L. Multiple Cranial Nerve Blocks as an Alternative Preventative Therapy for Chronic Migraine. Headache J. Head Face Pain 2020, 60, 981–987. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; Achana, F.; Carnes, D.; Eldridge, S.; Ellard, D.R.; Griffiths, F.; Haywood, K.; Hee, S.W.; Mistry, D.; Mistry, H.; et al. Usual care and a self-management support programme versus usual care and a relaxation programme for people living with chronic headache disorders: A randomised controlled trial protocol (CHESS). BMJ Open 2020, 10, e033520. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.; Lee, M.J.; Park, H.R.; Kim, S.; Joo, E.Y.; Chung, C.-S. Effect of Sleep Quality on Headache-Related Impact in Primary Headache Disorders. J. Clin. Neurol. 2020, 16, 237–244. [Google Scholar] [CrossRef]
- Guglielmetti, M.; Raggi, A.; Ornello, R.; Sacco, S.; D’Amico, D.; Leonardi, M.; Martelletti, P. The clinical and public health implications and risks of widening the definition of chronic migraine. Cephalalgia 2019, 40, 407–410. [Google Scholar] [CrossRef]
- Mukhopadhyay, K.; Joseph, N.E.; Barkondaj, B.; Mukherjee, S.; Chatterjee, C.; Chakraborty, S. A clinical study on presenting features and prescription pattern for migraine in a tertiary care hospital of Eastern India. J. Indian Med. Assoc. 2020, 118, 23–26. [Google Scholar]
- Hutchinson, S.; Lipton, R.B.; Ailani, J.; Reed, M.L.; Fanning, K.M.; Adams, A.M.; Buse, D.C. Characterization of Acute Prescription Migraine Medication Use. Mayo Clin. Proc. 2020, 95, 709–718. [Google Scholar] [CrossRef]
- He, Q.; Zhang, Y.; Wang, F.; Li, C.; Guo, R.; Li, X.; Luan, B.; Zhao, H.; Meng, L.; Chen, H.; et al. Impact of right-to-left shunt and transcatheter closure on the clinical features of migraine. Int. J. Neurosci. 2019, 130, 270–275. [Google Scholar] [CrossRef]
- Pérez-Benito, F.J.; Conejero, J.A.; Sáez, C.; García-Gómez, J.M.; Navarro-Pardo, E.; Florencio, L.L.; Fernández-De-Las-Peñas, C. Subgrouping Factors Influencing Migraine Intensity in Women: A Semi-automatic Methodology Based on Machine Learning and Information Geometry. Pain Pract. 2019, 20, 297–309. [Google Scholar] [CrossRef]
- Lipton, R.B.; Lombard, L.; Ruff, D.D.; Krege, J.H.; Loo, L.S.; Buchanan, A.; Melby, T.E.; Buse, D.C. Trajectory of migraine-related disability following long-term treatment with lasmiditan: Results of the GLADIATOR study. J. Headache Pain 2020, 21, 1–15. [Google Scholar] [CrossRef]
- Rodríguez-Almagro, D.; Achalandabaso-Ochoa, A.; Rus, A.; Obrero-Gaitán, E.; Zagalaz-Anula, N.; Lomas-Vega, R. Validation of the Spanish version of the migraine disability assessment questionnaire (MIDAS) in university students with migraine. BMC Neurol. 2020, 20, 1–7. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, D.; Grazzi, L.; Grignani, E.; Leonardi, M.; Sansone, E.; Raggi, A.; The HEADWORK Study Group. HEADWORK Questionnaire: Why Do We Need a New Tool to Assess Work-Related Disability in Patients with Migraine? Headache J. Head Face Pain 2020, 60, 497–504. [Google Scholar] [CrossRef] [PubMed]
- Pearl, T.A.; Dumkrieger, G.; Chong, C.D.; Dodick, D.W.; Schwedt, T.J. Impact of Depression and Anxiety Symptoms on Patient-Reported Outcomes in Patients with Migraine: Results from the American Registry for Migraine Research (ARMR). Headache J. Head Face Pain 2020, 60, 1910–1919. [Google Scholar] [CrossRef] [PubMed]
- Houle, M.; Marchand, A.-A.; Descarreaux, M. Can Headache Profile Predict Future Disability. Clin. J. Pain 2020, 36, 594–600. [Google Scholar] [CrossRef]
- Ashkan, K.; Sokratous, G.; Göbel, H.; Mehta, V.; Gendolla, A.; Dowson, A.; Wodehouse, T.; Heinze, A.; Gaul, C. Peripheral nerve stimulation registry for intractable migraine headache (RELIEF): A real-life perspective on the utility of occipital nerve stimulation for chronic migraine. Acta Neurochir. 2020, 162, 3201–3211. [Google Scholar] [CrossRef]
- Tepper, S.J.; Vasudeva, R.; Krege, J.H.; Rathmann, S.S.; Doty, E.; Vargas, B.B.; Magis, D.; Komori, M. Evaluation of 2-Hour Post-Dose Efficacy of Lasmiditan for the Acute Treatment of Difficult-to-Treat Migraine Attacks. Headache J. Head Face Pain 2020, 60, 1601–1615. [Google Scholar] [CrossRef]
- Ciuffini, R.; Stratta, P.; Pacitti, F.; Bologna, M.; Marrelli, A. Emotional dysregulation, affective status and personality traits in a sample of migraine patients. J. Psychopatol. 2020, 26, 141–146. [Google Scholar] [CrossRef]
- Speck, R.M.; Collins, E.M.; Ma, L.L.; Ayer, D.W. A Qualitative Study to Assess the Content Validity of the 24-Hour Migraine Quality of Life Questionnaire in Patients with Migraine. Headache J. Head Face Pain 2020, 60, 1982–1994. [Google Scholar] [CrossRef]
- Grazzi, L.; Usai, S.; Bolognini, N.; Grignani, E.; Sansone, E.; Tramacere, I.; Maravita, A.; Lauria, G. No efficacy of transcranial direct current stimulation on chronic migraine with medication overuse: A double blind, randomised clinical trial. Cephalalgia 2020, 40, 1202–1211. [Google Scholar] [CrossRef]
- Zhang, Y.; Xu, T.; Wang, Z.; Li, D.; Du, J.; Wen, Y.; Zhao, Y.; Liao, H.; Liang, F.; Zhao, L. Differences in topological properties of functional brain networks between menstrually-related and non-menstrual migraine without aura. Brain Imaging Behav. 2020, 1–10. [Google Scholar] [CrossRef]
- Khasiyev, F.; Arsava, E.M.; Topcuoglu, M.A. Cerebral vasomotor reactivity in migraine: Effect of patent foramen ovale and aerogenic microembolism. Neurol. Res. 2020, 42, 795–804. [Google Scholar] [CrossRef]
- Alharbi, F.G.; Alateeq, M.A. Quality of life of migraine patients followed in neurology clinics in Riyadh, Saudi Arabia. J Fam. Community Med. 2020, 27, 37–45. [Google Scholar]
- Kumar, A.; Mattoo, B.; Bhatia, R.; Kumaran, S.; Bhatia, R. Neuronavigation based 10 sessions of repetitive transcranial magnetic stimulation therapy in chronic migraine: An exploratory study. Neurol. Sci. 2020. [Google Scholar] [CrossRef]
- Taşlı, N.G.; Ersoy, A. Altered Macular Vasculature in Migraine Patients without Aura: Is It Associated with Ocular Vasculature and White Matter Hyperintensities? J. Ophthalmol. 2020, 2020, 1–8. [Google Scholar] [CrossRef]
- Klan, T.; Bräscher, A.-K.; Vales, A.; Liesering-Latta, E.; Witthöft, M.; Gaul, C. Determination of psychosocial factors in cluster headache—Construction and psychometric properties of the Cluster Headache Scales (CHS). Cephalalgia 2020, 40, 1240–1249. [Google Scholar] [CrossRef]
- Alpuente, A.; Gallardo, V.J.; Torres-Ferrús, M.; Álvarez-Sabin, J.; Pozo-Rosich, P. Early efficacy and late gain in chronic and high-frequency episodic migraine with onabotulinumtoxinA. Eur. J. Neurol. 2019, 26, 1464–1470. [Google Scholar] [CrossRef]
- Yu, S.; Ran, Y.; Wan, Q.; Yang, X.; Chen, H.; Wang, H.; Hu, X.; Mao, S.; Yu, T.; Luo, G.; et al. Efficacy and Safety of Toutongning Capsule in Patients with Migraine: A Multicenter, Randomized, Double-Blind, Placebo-Controlled Trial. J. Altern. Complement. Med. 2019, 25, 1215–1224. [Google Scholar] [CrossRef]
- Kim, B.-S.; Park, J.W.; Sohn, J.-H.; Lee, M.J.; Chu, M.K.; Ahn, J.-Y.; Choi, Y.-J.; Song, T.-J.; Chung, P.-W.; Oh, K.; et al. Associated Factors and Clinical Implication of Cutaneous Allodynia in Patients with Cluster Headache: A Prospective Multicentre Study. Sci. Rep. 2019, 9, 6548. [Google Scholar] [CrossRef]
- Glavor, K.D.; Titlić, M.; Vuletić, G.; Mrđen, A.; Šimunić, M.M. Quality of life assessment in migraine and relapsing remitting multiple sclerosis: Self-perceived health is similar. Neurol. Sci. 2019, 40, 2549–2554. [Google Scholar] [CrossRef]
- Gil-Martínez, A.; Navarro-Fernández, G.; Mangas-Guijarro, M.Á.; Díaz-De-Terán, J. Hyperalgesia and Central Sensitization Signs in Patients with Cluster Headache: A Cross-Sectional Study. Pain Med. 2019, 20, 2562–2570. [Google Scholar] [CrossRef] [PubMed]
- He, Y.-D.; Yan, X.-L.; Qin, C.; Zhang, P.; Guo, Z.-N.; Yang, Y. Transcatheter Patent Foramen Ovale Closure Is Effective in Alleviating Migraine in a 5-Year Follow-Up. Front. Neurol. 2019, 10, 1224. [Google Scholar] [CrossRef]
- Seng, E.; Singer, A.B.; Metts, C.; Grinberg, A.S.; Patel, Z.S.; Ma, M.M.; Ma, L.R.; Day, M.; Minen, M.T.; Lipton, R.B.; et al. Does Mindfulness-Based Cognitive Therapy for Migraine Reduce Migraine-Related Disability in People with Episodic and Chronic Migraine? A Phase 2b Pilot Randomized Clinical Trial. Headache J. Head Face Pain 2019, 59, 1448–1467. [Google Scholar] [CrossRef]
- Shaygan, M.; Rahmanian, S.; Emadi, F.; Rakhshan, M. Predictive Factors for Disability in Patients with Acute and Chronic Headache. Shiraz E Med. J. 2019, 20, 87499. [Google Scholar] [CrossRef]
- Togha, M.; Haghdoost, F.; Khorsha, F.; Jahromi, S.R.; Ghorbani, Z. Body Mass Index and its Association with Migraine Characteristics in Female Patients. Arch. Iran Med. 2019, 22, 554–559. [Google Scholar]
- Bragatto, M.M.; Bevilaqua-Grossi, D.; Benatto, M.T.; Lodovichi, S.S.; Pinheiro, C.F.; Carvalho, G.F.; Dach, F.; Fernández-De-Las-Peñas, C.; Florencio, L.L. Is the presence of neck pain associated with more severe clinical presentation in patients with migraine? A cross-sectional study. Cephalalgia 2019, 39, 1500–1508. [Google Scholar] [CrossRef]
- Friedman, D.I.; Rajan, B.; Seidmann, A. A randomized trial of telemedicine for migraine management. Cephalalgia 2019, 39, 1577–1585. [Google Scholar] [CrossRef]
- Kawata, A.K.; Hareendran, A.; Shaffer, S.; Mannix, S.; Thach, A.; Desai, P.; Mikol, D.D.; Ortmeier, B.; Bayliss, M.; Buse, D.C. Evaluating the Psychometric Properties of the Migraine Functional Impact Questionnaire (MFIQ). Headache J. Head Face Pain 2019, 59, 1253–1269. [Google Scholar] [CrossRef] [PubMed]
- Ford, J.H.; Ayer, D.W.; Zhang, Q.; Carter, J.N.; Leroux, E.; Skljarevski, V.; Aurora, S.K.; Tockhorn-Heidenreich, A.; Lipton, R.B. Two randomized migraine studies of galcanezumab. Neurology 2019, 93, e508–e517. [Google Scholar] [CrossRef]
- Karan, V.; Pradeep, R.; Sundarmurthy, H.; Kulkarni, P. Prevalence and predictors of female sexual dysfunction in migraine. Ann. Indian Acad. Neurol. 2019, 22, 291–294. [Google Scholar] [CrossRef]
- Fernández-De-Las-Peñas, C.; Ambite-Quesada, S.; Florencio, L.L.; Palacios-Ceña, M.; Ordás-Bandera, C.; Arendt-Nielsen, L. Catechol-O-Methyltransferase Val158Met Polymorphism Is Associated with Anxiety, Depression, and Widespread Pressure Pain Sensitivity in Women with Chronic, but Not Episodic, Migraine. Pain Med. 2018, 20, 1409–1417. [Google Scholar] [CrossRef]
- Nielsen, M.; Carlsen, L.N.; Munksgaard, S.B.; Engelstoft, I.M.S.; Jensen, R.H.; Bendtsen, L. Complete withdrawal is the most effective approach to reduce disability in patients with medication-overuse headache: A randomized controlled open-label trial. Cephalalgia 2019, 39, 863–872. [Google Scholar] [CrossRef] [PubMed]
- De Tommaso, M.; Brighina, F.; Delussi, M. Effects of Botulinum Toxin A on Allodynia in Chronic Migraine: An Observational Open-Label Two-Year Study. Eur. Neurol. 2019, 81, 37–46. [Google Scholar] [CrossRef]
- Hjalte, F.; Olofsson, S.; Persson, U.; Linde, M. Burden and costs of migraine in a Swedish defined patient population—A questionnaire-based study. J. Headache Pain 2019, 20, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Lipton, R.B.; Tepper, S.J.; Reuter, U.; Silberstein, S.; Stewart, W.F.; Nilsen, J.; Leonardi, D.K.; Desai, P.; Cheng, S.; Mikol, D.D.; et al. Erenumab in chronic migraine. Neurology 2019, 92, e2250–e2260. [Google Scholar] [CrossRef] [PubMed]
- Sajobi, T.; Amoozegar, F.; Wang, M.; Wiebe, N.; Fiest, K.M.; Patten, S.; Jetté, N. Global assessment of migraine severity measure: Preliminary evidence of construct validity. BMC Neurol. 2019, 19, 53. [Google Scholar] [CrossRef] [PubMed]
- Vasudha, M.; Manjunath, N.; Nagendra, H. Changes in MIDAS, Perceived Stress, Frontalis Muscle Activity and Non-Steroidal Anti-Inflammatory Drugs Usage in Patients with Migraine Headache without Aura following Ayurveda and Yoga Compared to Controls: An Open Labeled Non-Randomized Study. Ann. Neurosci. 2018, 25, 250–260. [Google Scholar] [CrossRef]
- Khazraee, H.; Omidi, A.; Kakhki, R.D.; Zanjani, Z.; Sehat, M. Effectiveness of acceptance and commitment therapy in cognitive emotion regulation strategies, headache-related disability, and headache intensity in patients with chronic daily headache. Iran. Red. Crescent Med. J. 2018, 20, e57151. [Google Scholar] [CrossRef]
- Palacios-Ceña, M.; Wang, K.; Castaldo, M.; Ordás-Bandera, C.; Torelli, P.; Arendt-Nielsen, L.; Fernández-De-Las-Peñas, C. Variables Associated with the Use of Prophylactic Amitriptyline Treatment in Patients with Tension-type Headache. Clin. J. Pain 2019, 35, 315–320. [Google Scholar] [CrossRef]
- Peres, M.F.P.; Oliveira, A.B.; Mercante, J.P.; Kamei, H.H.; Tobo, P.R.; Rozen, T.D.; Levin, M.; Buse, D.C.; Lucchetti, G. Optimism, Pessimism, and Migraine: A Cross-Sectional, Population-Based Study. Headache J. Head Face Pain 2019, 59, 205–214. [Google Scholar] [CrossRef]
- Ruscheweyh, R.; Pereira, D.; Hasenbring, M.; Straube, A. Pain-related avoidance and endurance behaviour in migraine: An observational study. J. Headache Pain 2019, 20, 9. [Google Scholar] [CrossRef]
- Zivkovic-Zaric, R.; Janković, S.M.; Csépány, É.; Gyüre, T.; Ertsey, C.; Andjelkovic, M. Psychometric properties of the Headache Under-Response to Treatment (HURT) questionnaire and the Migraine Disability Assessment Test (MIDAS) translated to Serbian. Vojn. Pregl. 2019, 76, 1162–1168. [Google Scholar] [CrossRef]
- Lillis, J.; Thomas, J.G.; Lipton, R.B.; Rathier, L.; Roth, J.; Pavlovic, J.; O’Leary, K.C.; Bond, D.S. The Association of Changes in Pain Acceptance and Headache-Related Disability. Ann. Behav. Med. 2019, 53, 686–690. [Google Scholar] [CrossRef] [PubMed]
- Ersoy, S.; Benli, A.R. Continue or stop applying wet cupping therapy (al-hijamah) in migraine headache: A randomized controlled trial. Complement. Ther. Clin. Pract. 2020, 38, 101065. [Google Scholar] [CrossRef] [PubMed]
- Jung, Y.; Won, B.; Lee, M.; Chung, J.; Han, S.J.; Kim, M. The Efficacy of Shinbaro for the Preventive Treatment of Migraine: A Pilot Study. Evid. Based Complement. Altern. Med. 2019, 2019, 2363420. [Google Scholar] [CrossRef] [PubMed]
- Lampl, C.; Rudolph, M.; Bräutigam, E. OnabotulinumtoxinA in the treatment of refractory chronic cluster headache. J. Headache Pain 2018, 19, 1–6. [Google Scholar] [CrossRef]
- Barloese, M.; Petersen, A.; Stude, P.; Jürgens, T.; Jensen, R.; May, A. Sphenopalatine ganglion stimulation for cluster headache, results from a large, open-label European registry. J. Headache Pain 2018, 19, 1–8. [Google Scholar] [CrossRef]
- Sengul, Y.; Sengul, H.S.; Tunç, A. Psychoform and somatoform dissociative experiences in migraine: Relationship with pain perception and migraine related disability. Ideggyógyászati Szle 2018, 71, 385–392. [Google Scholar] [CrossRef]
- Vetvik, K.G.; MacGregor, E.A.; Lundqvist, C.; Russell, M.B. Symptoms of premenstrual syndrome in female migraineurs with and without menstrual migraine. J. Headache Pain 2018, 19, 97–107. [Google Scholar] [CrossRef]
- Caronna, E.; Gallardo, V.J.; Hernández-Beltrán, N.; Torres-Ferrús, M.; Pozo-Rosich, P. OnabotulinumtoxinA: An Effective Tool in the Therapeutic Arsenal for Chronic Migraine with Medication Overuse. Front. Neurol. 2018, 9, 808. [Google Scholar] [CrossRef] [PubMed]
- Kucukdurmaz, F.; Inanc, Y.; Inanc, Y.; Resim, S. Sexual dysfunction and distress in premenopausal women with migraine: Association with depression, anxiety and migraine-related disability. Int. J. Impot. Res. 2018, 30, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Buse, D.C.; Lipton, R.B.; Hallström, Y.; Reuter, U.; Tepper, S.J.; Zhang, F.; Sapra, S.; Picard, H.; Mikol, D.D.; Lenz, R.A. Migraine-related disability, impact, and health-related quality of life among patients with episodic migraine receiving preventive treatment with erenumab. Cephalalgia 2018, 38, 1622–1631. [Google Scholar] [CrossRef]
- Aguila, M.-E.R.; Rebbeck, T.; Pope, A.; Ng, K.; Leaver, A. Six-month clinical course and factors associated with non-improvement in migraine and non-migraine headaches. Cephalalgia 2017, 38, 1672–1686. [Google Scholar] [CrossRef] [PubMed]
- Kristoffersen, E.S.; Grande, R.B.; Aaseth, K.; Russell, M.B.; Lundqvist, C. Medication-overuse headache detoxification reduces headache disability—The Akershus study of chronic headache. Eur. J. Neurol. 2018, 25, 1140–1147. [Google Scholar] [CrossRef] [PubMed]
- Thakur, E.R.; Recober, A.; Turvey, C.L.; Dindo, L.N. Benefits of an on-line migraine education video for patients with co-occurring migraine and depression. J. Psychosom. Res. 2018, 112, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Ayer, D.W.; Skljarevski, V.; Ford, J.H.; Nyhuis, A.W.; Lipton, R.B.; Aurora, S.K. Measures of Functioning in Patients with Episodic Migraine: Findings from a Double-Blind, Randomized, Placebo-Controlled Phase 2b Trial with Galcanezumab. Headache J. Head Face Pain 2018, 58, 1225–1235. [Google Scholar] [CrossRef] [PubMed]
- Shim, E.; Park, A.; Park, S.-P. The relationship between alexithymia and headache impact: The role of somatization and pain catastrophizing. Qual. Life Res. 2018, 27, 2283–2294. [Google Scholar] [CrossRef]
- Whealy, M.A.; Nanda, S.; Vincent, A.; Mandrekar, J.N.; Cutrer, F.M. Fibromyalgia in migraine: A retrospective cohort study. J. Headache Pain 2018, 19, 61. [Google Scholar] [CrossRef]
- Ayele, B.A.; Yifru, Y.M. Migraine-related disability and co-morbid depression among migraineurs in Ethiopia: A cross-sectional study. BMC Neurol. 2018, 18, 95. [Google Scholar] [CrossRef]
- Hanson, L.L.; Ahmed, Z.; Katz, B.J.; Warner, J.E.; Crum, A.V.; Zhang, Y.; Zhang, Y.; Baggaley, S.; Pippitt, K.; Cortez, M.M.; et al. Patients with Migraine Have Substantial Reductions in Measures of Visual Quality of Life. Headache J. Head Face Pain 2018, 58, 1007–1013. [Google Scholar] [CrossRef]
- Velasco-Juanes, F.; Gomez-Esteban, J.C.; Fernández-Valle, T.; Matute-Nieves, A.; Almeida-Velasco, J.; Lloret-Villas, M.I.; Ugarriza-Serrano, I. Clinical treatment of chronic and episodic migraine with onabotulinumtoxinA in a real-world setting. Drugs Ther. Perspect. 2018, 34, 335–343. [Google Scholar] [CrossRef]
- Inanç, Y.; Orhan, F.O.; Inanc, Y. The effects of Maras powder use on patients with migraine. Neuropsychiatr. Dis. Treat. 2018, 14, 1143–1148. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Zhao, L.-P.; Zhang, C.S.; Zeng, L.; Wang, K.; Zhao, J.; Wang, L.; Jing, X.; Li, B. Acupuncture as prophylaxis for chronic migraine: A protocol for a single-blinded, double-dummy randomised controlled trial. BMJ Open 2018, 8, e020653. [Google Scholar] [PubMed]
- Starling, A.J.; Tepper, S.J.; Marmura, M.J.; Shamim, E.A.; Robbins, M.S.; Hindiyeh, N.; Charles, A.C.; Goadsby, P.J.; Lipton, R.B.; Silberstein, S.D.; et al. A multicenter, prospective, single arm, open label, observational study of sTMS for migraine prevention (ESPOUSE Study). Cephalalgia 2018, 38, 1038–1048. [Google Scholar] [CrossRef] [PubMed]
- Jangid, R.K.; Nagpal, M.; Rao, T.S.S. A comparative study of the sexual functioning of women with primary headache in India. Indian J. Psychiatry 2018, 60, 224–228. [Google Scholar] [CrossRef]
- Zeybek, S.; Kisabay, A.; Sari, U.S.; Selcuki, D. Evaluation of the effect of botulinum neurotoxin type A (BoNT/A) on daily activity performance in chronic migraine patients using VAS, MIDAS AND HIT-6 tests. Neurol. Asia 2018, 23, 35–43. [Google Scholar]
- Leroux, E.; Beaudet, L.; Boudreau, G.; Eghtesadi, M.; Marchand, L.; Pim, H.; Chagnon, M. A Nursing Intervention Increases Quality of Life and Self-Efficacy in Migraine: A 1-Year Prospective Controlled Trial. Headache J. Head Face Pain 2017, 58, 260–274. [Google Scholar] [CrossRef]
- Kumar, S.; Singh, S.; Kumar, N.; Verma, R. The Effects of Repetitive Transcranial Magnetic Stimulation at Dorsolateral Prefrontal Cortex in the Treatment of Migraine Comorbid with Depression: A Retrospective Open Study. Clin. Psychopharmacol. Neurosci. 2018, 16, 62–66. [Google Scholar] [CrossRef]
- Yigit, M.; Sogut, O.; Tataroglu, Ö.; Yamanoglu, A.; Yiğit, E.; Guler, E.M.; Ozer, O.F.; Koçyiğit, A. Oxidative/antioxidative status, lymphocyte DNA damage, and urotensin-2 receptor level in patients with migraine attacks. Neuropsychiatr. Dis. Treat. 2018, 14, 367–374. [Google Scholar] [CrossRef]
- Raggi, A.; Covelli, V.; Guastafierro, E.; Leonardi, M.; Scaratti, C.; Grazzi, L.; Bartolini, M.; Viticchi, G.; Cevoli, S.; Pierangeli, G.; et al. Validation of a self-reported instrument to assess work-related difficulties in patients with migraine: The HEADWORK questionnaire. J. Headache Pain 2018, 19, 85. [Google Scholar] [CrossRef]
- Giampetro, D.; Ruiz-Velasco, V.; Pruett, A.; Wicklund, M.; Knipe, R. The Effect of Propofol on Chronic Headaches in Patients Undergoing Endoscopy. Pain Res. Manag. 2018, 2018, 1–7. [Google Scholar] [CrossRef]
- Georgoudis, G.; Felah, B.; Nikolaidis, P.; Papandreou, M.; Mitsiokappa, E.; Mavrogenis, A.F.; Rosemann, T.; Knechtle, B. The effect of physiotherapy and acupuncture on psychocognitive, somatic, quality of life, and disability characteristics in TTH patients. J. Pain Res. 2018, 11, 2527–2535. [Google Scholar] [CrossRef]
- Cha, M.-J.; Kim, B.K.; Moon, H.-S.; Ahn, J.-Y.; Oh, K.; Kim, J.Y.; Sohn, J.-H.; Chung, J.-M.; Song, T.-J.; Kim, J.; et al. Stress Is Associated with Poor Outcome of Acute Treatment for Chronic Migraine: A Multicenter Study. Pain Med. 2017, 19, 1832–1838. [Google Scholar] [CrossRef]
- Sarchielli, P.; Romoli, M.; Corbelli, I.; Bernetti, L.; Verzina, A.; Brahimi, E.; Eusebi, P.; Caproni, S.; Calabresi, P. Stopping Onabotulinum Treatment after the First Two Cycles Might Not Be Justified: Results of a Real-life Monocentric Prospective Study in Chronic Migraine. Front. Neurol. 2017, 8, 655. [Google Scholar] [CrossRef]
- Pires, R.D.C.C.K.; Da Rocha, N.S.; Esteves, J.E.; Rodrigues, M.E. Use of pressure dynamometer in the assessment of the pressure pain threshold in trigger points in the craniocervical muscles in women with unilateral migraine and tension-type headache: An observational study. Int. J. Osteopat. Med. 2017, 26, 28–35. [Google Scholar] [CrossRef]
- Dahri, M.; Hashemilar, M.; Jafarabadi, M.A.; Tarighat-Esfanjani, A. Efficacy of coenzyme Q10 for the prevention of migraine in women: A randomized, double-blind, placebo-controlled study. Eur. J. Integr. Med. 2017, 16, 8–14. [Google Scholar] [CrossRef]
- Matharu, M.; Halker, R.; Pozo-Rosich, P.; Degryse, R.; Adams, A.M.; Aurora, S.K. The impact of onabotulinumtoxinA on severe headache days: PREEMPT 56-week pooled analysis. J. Headache Pain 2017, 18, 1–8. [Google Scholar] [CrossRef]
- Grazzi, L.; Sansone, E.; Raggi, A.; D’Amico, D.; De Giorgio, A.; Leonardi, M.; De Torres, L.; Salgado-García, F.; Andrasik, F. Mindfulness and pharmacological prophylaxis after withdrawal from medication overuse in patients with Chronic Migraine: An effectiveness trial with a one-year follow-up. J. Headache Pain 2017, 18, 1–12. [Google Scholar] [CrossRef]
- Moon, H.-J.; Seo, J.-G.; Park, S.-P. Perceived stress in patients with migraine: A case-control study. J. Headache Pain 2017, 18, 1–7. [Google Scholar] [CrossRef]
- Palacios-Ceña, M.; Fernández-Muñoz, J.J.; Castaldo, M.; Wang, K.; Guerrero-Peral, Á.; Arendt-Nielsen, L.; Fernández-De-Las-Peñas, C. The association of headache frequency with pain interference and the burden of disease is mediated by depression and sleep quality, but not anxiety, in chronic tension type headache. J. Headache Pain 2017, 18, 1–8. [Google Scholar] [CrossRef]
- Guerzoni, S.; Pellesi, L.; Baraldi, C.; Cainazzo, M.M.; Negro, A.; Martelletti, P.; Pini, L.A. Long-term Treatment Benefits and Prolonged Efficacy of OnabotulinumtoxinA in Patients Affected by Chronic Migraine and Medication Overuse Headache over 3 Years of Therapy. Front. Neurol. 2017, 8, 586. [Google Scholar] [CrossRef]
- Bøe, M.G.; Thortveit, E.; Vatne, A.; Mygland, Å. Chronic headache with medication overuse: Long-term prognosis after withdrawal therapy. Cephalalgia 2017, 37, 1215–1221. [Google Scholar] [CrossRef] [PubMed]
- Nasiri, F.S.M.; Pakdaman, S.; Dehghani, M.; Togha, M. The Relationship between Pain Catastrophizing and Headache-Related Disability: The Mediating Role of Pain Intensity. Jpn. Psychol. Res. 2017, 59, 266–274. [Google Scholar] [CrossRef]
- Kawata, A.K.; Hsieh, R.; Bender, R.; Shaffer, S.; Revicki, D.A.; Bayliss, M.; Buse, D.C.; Desai, P.; Sapra, S.; Ortmeier, B.; et al. Psychometric Evaluation of a Novel Instrument Assessing the Impact of Migraine on Physical Functioning: The Migraine Physical Function Impact Diary. Headache J. Head Face Pain 2017, 57, 1385–1398. [Google Scholar] [CrossRef]
- Singh, S.; Sarda, K.; Hegde, R. A Pan-India Study to Assess the Quality of Life, Symptom Profile and Management Trends in Patients with Migraine: A Cross-Sectional Study. J. Assoc. Phys. India 2017, 65, 63–69. [Google Scholar]
- Fontaine, D.; Blond, S.; Lucas, C.; Regis, J.; Donnet, A.; Derrey, S.; Guegan-Massardier, E.; Jarraya, B.; Dang-Vu, B.; Bourdain, F.; et al. Occipital nerve stimulation improves the quality of life in medically-intractable chronic cluster headache: Results of an observational prospective study. Cephalalgia 2017, 37, 1173–1179. [Google Scholar] [CrossRef]
- Raggi, A.; Grazzi, L.; Ayadi, R.; Leonardi, M.; Proietti, A.; Schiavolin, S.; Scaratti, C.; Usai, S.; D’Amico, D. Clinical and psychosocial features of frequent relapsers (FR) among patients with chronic migraine and medication overuse. Neurol. Sci. 2017, 38, 169–171. [Google Scholar] [CrossRef]
- Miller, S.; Watkins, L.; Matharu, M. Treatment of intractable chronic cluster headache by occipital nerve stimulation: A cohort of 51 patients. Eur. J. Neurol. 2016, 24, 381–390. [Google Scholar] [CrossRef]
- Palacios-Ceña, M.; Castaldo, M.; Wang, K.; Catena, A.; Torelli, P.; Arendt-Nielsen, L.; Fernández-De-Las-Peñas, C. Relationship of active trigger points with related disability and anxiety in people with tension-type headache. Medicine 2017, 96, e6548. [Google Scholar] [CrossRef]
- Raggi, A.; Giovannetti, A.M.; Leonardi, M.; Sansone, E.; Schiavolin, S.; Curone, M.; Grazzi, L.; Usai, S.; D’Amico, D. Predictors of 12-Months Relapse After Withdrawal Treatment in Hospitalized Patients with Chronic Migraine Associated with Medication Overuse: A Longitudinal Observational Study. Headache J. Head Face Pain 2016, 57, 60–70. [Google Scholar] [CrossRef]
- Xing, Y.-Q.; Guo, Y.-Z.; Gao, Y.-S.; Guo, Z.-N.; Niu, P.-P.; Yang, Y. Effectiveness and Safety of Transcatheter Patent Foramen Ovale Closure for Migraine (EASTFORM) Trial. Sci. Rep. 2016, 6, 39081. [Google Scholar] [CrossRef]
- Santangelo, G.; Russo, A.; Trojano, L.; Falco, F.; Marcuccio, L.; Siciliano, M.; Conte, F.; Garramone, F.; Tessitore, A.; Tedeschi, G. Cognitive dysfunctions and psychological symptoms in migraine without aura: A cross-sectional study. J. Headache Pain 2016, 17, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Janković, S.M.; Anđelković, M.; Zivkovic-Zaric, R.; Vasic, M.; Csépány, É.; Gyüre, T.; Ertsey, C. The psychometric properties of the Comprehensive Headache-related Quality of life Questionnaire (CHQQ) translated to Serbian. SpringerPlus 2016, 5, 1416. [Google Scholar] [CrossRef] [PubMed]
- Wang, N.; Huang, H.-L.; Zhou, H.; Yu, C.-Y. Cognitive impairment and quality of life in patients with migraine-associated vertigo. Eur. Rev. Med. Pharmacol. Sci. 2016, 20, 4913–4917. [Google Scholar] [PubMed]
- Abu Bakar, N.; Torkamani, M.; Tanprawate, S.; Lambru, G.; Matharu, M.; Jahanshahi, M. The development and validation of the Cluster Headache Quality of life scale (CHQ). J. Headache Pain 2016, 17, 79. [Google Scholar] [CrossRef] [PubMed]
- Demiryürek, B.E.; Ertem, D.H.; Tekin, A.; Ceylan, M.; Aras, Y.G.; Gungen, B.D. Effects of onabotulinumtoxinA treatment on efficacy, depression, anxiety, and disability in Turkish patients with chronic migraine. Neurol. Sci. 2016, 37, 1779–1784. [Google Scholar] [CrossRef] [PubMed]
- Shehata, H.S.; Esmail, E.H.; Abdelalim, A.; El-Jaafary, S.I.; Elmazny, A.; Sabbah, A.; Shalaby, N.M. Repetitive transcranial magnetic stimulation versus botulinum toxin injection in chronic migraine prophylaxis: A pilot randomized trial. J. Pain Res. 2016, 9, 771–777. [Google Scholar] [CrossRef]
- Happe, S.; Peikert, A.; Siegert, R.; Evers, S. The efficacy of lymphatic drainage and traditional massage in the prophylaxis of migraine: A randomized, controlled parallel group study. Neurol. Sci. 2016, 37, 1627–1632. [Google Scholar] [CrossRef]
- Lipton, R.B.; Rosen, N.L.; Ailani, J.; DeGryse, R.E.; Gillard, P.J.; Varon, S.F. OnabotulinumtoxinA improves quality of life and reduces impact of chronic migraine over one year of treatment: Pooled results from the PREEMPT randomized clinical trial program. Cephalalgia 2016, 36, 899–908. [Google Scholar] [CrossRef]
- Rocha-Filho, P.A.S.; Marques, K.S.; Torres, R.C.S.; Leal, K.N.R. Migraine, Osmophobia, and Anxiety. Pain Med. 2016, 17, 776–780. [Google Scholar] [CrossRef] [PubMed]
- Rafie, S.; Namjoyan, F.; Golfakhrabadi, F.; Yousefbeyk, F.; Hassanzadeh, A. Effect of lavender essential oil as a prophylactic therapy for migraine: A randomized controlled clinical trial. J. Herb. Med. 2016, 6, 18–23. [Google Scholar] [CrossRef]
- Walker, A.K.; Lyle, R. Passive Infrared Hemoencephalography (pIR HEG) for the Treatment of Migraine without Aura. NeuroRegulation 2016, 3, 78–91. [Google Scholar] [CrossRef]
- Sujan, M.U.; Rao, M.R.; Kisan, R.; Abhishekh, H.A.; Nalini, A.; Raju, T.R.; Sathyaprabha, T.N. Influence of hydrotherapy on clinical and cardiac autonomic function in migraine patients. J. Neurosci. Rural Pract. 2016, 7, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Karaca, E.E.; Koçer, E.B.; Ozdek, S.; Akçam, H.T.; Ercan, M.B. Choroidal thickness measurements in migraine patients during attack-free period. Neurol. Sci. 2015, 37, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Mahmoudzadeh Zarandi, F.; Raiesifar, A.; Ebadi, A. The Effect of Orem’s Self-Care Model on Quality of Life in Patients with Migraine: A Randomized Clinical Trial. Acta Med. Iran 2016, 54, 159–164. [Google Scholar]
- Russo, A.; Tessitore, A.; Conte, F.; Marcuccio, L.; Giordano, A.; Tedeschi, G. Transcutaneous supraorbital neurostimulation in de novo patients with migraine without aura: The first Italian experience. J. Headache Pain 2015, 16, 69. [Google Scholar] [CrossRef]
- Seo, J.-G.; Park, S.-P. Validation of the Patient Health Questionnaire-9 (PHQ-9) and PHQ-2 in patients with migraine. J. Headache Pain 2015, 16, 65. [Google Scholar] [CrossRef]
- Seo, J.-G.; Park, S.-P. Validation of the Generalized Anxiety Disorder-7 (GAD-7) and GAD-2 in patients with migraine. J. Headache Pain 2015, 16, 97. [Google Scholar] [CrossRef]
- Kinfe, T.M.; Pintea, B.; Muhammad, S.; Zaremba, S.; Roeske, S.; Simon, B.J.; Vatter, H. Cervical non-invasive vagus nerve stimulation (nVNS) for preventive and acute treatment of episodic and chronic migraine and migraine-associated sleep disturbance: Preliminary findings from a prospective observational cohort study. J. Headache Pain 2015, 16, 1–11. [Google Scholar] [CrossRef]
- Manandhar, K.; Risal, A.; Linde, M.; Steiner, T. The burden of headache disorders in Nepal: Estimates from a population-based survey. J. Headache Pain 2015, 17, 1–10. [Google Scholar] [CrossRef]
- Negro, A.; Curto, M.; Lionetto, L.; Crialesi, D.; Martelletti, P. OnabotulinumtoxinA 155 U in medication overuse headache: A two years prospective study. SpringerPlus 2015, 4, 1–8. [Google Scholar] [CrossRef]
- Negro, A.; Curto, M.; Lionetto, L.; Martelletti, P. A two years open-label prospective study of OnabotulinumtoxinA 195 U in medication overuse headache: A real-world experience. J. Headache Pain 2015, 17, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Gaul, C.; Diener, H.-C.; Danesch, U. Improvement of migraine symptoms with a proprietary supplement containing riboflavin, magnesium and Q10: A randomized, placebo-controlled, double-blind, multicenter trial. J. Headache Pain 2015, 16, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Beldarrain, M.; Anton-Ladislao, A.; Aguirre-Larracoechea, U.; Oroz, I.; Garcia-Monco, J.C. Low cognitive reserve is associated with chronic migraine with medication overuse and poor quality of life. Cephalalgia 2014, 35, 683–691. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, D.; Grazzi, L.; Curone, M.; Di Fiore, P.; Cecchini, A.P.; Leonardi, M.; Scaratti, C.; Raggi, A. Difficulties in work activities and the pervasive effect over disability in patients with episodic and chronic migraine. Neurol. Sci. 2015, 36, 9–11. [Google Scholar] [CrossRef]
- Raggi, A.; Schiavolin, S.; Leonardi, M.; Grazzi, L.; Usai, S.; Curone, M.; D’Amico, D. Approaches to treatments of chronic migraine associated with medication overuse: A comparison between different intensity regimens. Neurol. Sci. 2015, 36, 5–8. [Google Scholar] [CrossRef]
- Pavlović, J.M.; Stewart, W.F.; Bruce, C.A.; Gorman, J.A.; Sun, H.; Buse, D.C.; Lipton, R.B. Burden of migraine related to menses: Results from the AMPP study. J. Headache Pain 2015, 16, 1–11. [Google Scholar] [CrossRef]
- Dindo, L.; Recober, A.; Marchman, J.; O’Hara, M.; Turvey, C. Depression and Disability in Migraine: The Role of Pain Acceptance and Values-Based Action. Int. J. Behav. Med. 2014, 22, 109–117. [Google Scholar] [CrossRef]
- Buse, D.C.; Serrano, D.; Reed, M.L.; Kori, S.H.; Cunanan, C.M.; Adams, A.M.; Lipton, R.B. Adding Additional Acute Medications to a Triptan Regimen for Migraine and Observed Changes in Headache-Related Disability: Results from the American Migraine Prevalence and Prevention (AMPP) Study. Headache J. Head Face Pain 2015, 55, 825–839. [Google Scholar] [CrossRef]
- Gil-Gouveia, R.; Gouveia-Oliveira, R.; Martins, I.P. The impact of cognitive symptoms on migraine attack-related disability. Cephalalgia 2015, 36, 422–430. [Google Scholar] [CrossRef]
- Smitherman, T.A.; Davis, R.E.; Walters, A.B.; Young, J.; Houle, T.T. Anxiety sensitivity and headache: Diagnostic differences, impact, and relations with perceived headache triggers. Cephalalgia 2014, 35, 710–721. [Google Scholar] [CrossRef]
- Shin, Y.-W.; Park, H.J.; Shim, J.-Y.; Oh, M.-J.; Kim, M. Seasonal Variation, Cranial Autonomic Symptoms, and Functional Disability in Migraine: A Questionnaire-Based Study in Tertiary Care. Headache J. Head Face Pain 2015, 55, 1112–1123. [Google Scholar] [CrossRef] [PubMed]
- Rocha-Filho, P.A.S.; Marques, K.S.; Torres, R.C.S.; Leal, K.N.R. Osmophobia and Headaches in Primary Care: Prevalence, Associated Factors, and Importance in Diagnosing Migraine. Headache J. Head Face Pain 2015, 55, 840–845. [Google Scholar] [CrossRef]
- D’Amico, D.; Grazzi, L.; Bussone, G.; Curone, M.; Di Fiore, P.; Usai, S.; Leonardi, M.; Giovannetti, A.M.; Schiavolin, S.; Raggi, A. Are Depressive Symptomatology, Self-Efficacy, and Perceived Social Support Related to Disability and Quality of Life in Patients with Chronic Migraine Associated to Medication Overuse? Data from a Cross-Sectional Study. Headache J. Head Face Pain 2015, 55, 636–645. [Google Scholar] [CrossRef]
- Raggi, A.; Schiavolin, S.; Leonardi, M.; Giovannetti, A.M.; Bussone, G.; Curone, M.; Di Fiore, P.; Grazzi, L.; Usai, S.; D’Amico, D. Chronic migraine with medication overuse: Association between disability and quality of life measures, and impact of disease on patients’ lives. J. Neurol. Sci. 2015, 348, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Black, A.K.; Fulwiler, J.C.; Smitherman, T.A. The Role of Fear of Pain in Headache. Headache J. Head Face Pain 2015, 55, 669–679. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Huang, X.; Fan, Y.; Wang, Y.; Ma, K. Efficacy of Pulsed Radiofrequency on Cervical 2-3 Posterior Medial Branches in Treating Chronic Migraine: A Randomized, Controlled, and Double-Blind Trial. Evid. Based Complement. Altern. Med. 2015, 2015, 1–7. [Google Scholar] [CrossRef]
- Maasumi, K.; Thompson, N.R.; Kriegler, J.S.; Tepper, S.J. Effect of OnabotulinumtoxinA Injection on Depression in Chronic Migraine. Headache J. Head Face Pain 2015, 55, 1218–1224. [Google Scholar] [CrossRef]
- Üstün, T.B.; Chatterji, S.; Kostanjsek, N.; Rehm, J.; Kennedy, C.; Epping-Jordan, J.; Saxena, S.; Von Korff, M.; Pull, C. Developing the World Health Organization Disability Assessment Schedule 2.0. Bull. World Health Organ. 2010, 88, 815–823. [Google Scholar] [CrossRef]
- Garin, O.; Ayuso, J.L.; Almansa, J.; Nieto, M.; Chatterji, S.; Vilagut, G.; Alonso, J.; Cieza, A.; Svestkova, O.; Burger, H.; et al. Validation of the World Health Organization Disability Assessment Schedule, WHODAS-2 in patients with chronic diseases. Health Qual. Life Outcomes 2010, 8, 51. [Google Scholar] [CrossRef]
- Ware, J.J. SF-36 Health Survey. Manual and Interpretation Guide; The Health Institute, New England Medical Center: Boston, MA, USA, 1993. [Google Scholar]
- Reilly, M.C.; Zbrozek, A.S.; Dukes, E.M. The Validity and Reproducibility of a Work Productivity and Activity Impairment Instrument. PharmacoEconomics 1993, 4, 353–365. [Google Scholar] [CrossRef]
- Hartmaier, S.L.; Santanello, N.C.; Epstein, R.S.; Silberstein, S.D. Development of a Brief 24-Hour Migraine-Specific Quality of Life Questionnaire. Headache J. Head Face Pain 1995, 35, 320–329. [Google Scholar] [CrossRef] [PubMed]
- Santanello, N.C.; Hartmaier, S.L.; Epstein, R.S.; Silberstein, S.D. Validation of a New Quality of Life Questionnaire for Acute Migraine Headache. Headache J. Head Face Pain 1995, 35, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, G.P.; Ramadan, N.M.; Aggarwal, S.K.; Newman, C.W. The Henry Ford Hospital Headache Disability Inventory (HDI). Neurology 1994, 44, 837. [Google Scholar] [CrossRef]
- Dodick, D. Migraine. Lancet 2018, 391, 1315–1330. [Google Scholar] [CrossRef]
- Terrin, A.; Mainardi, F.; Lisotto, C.; Mampreso, E.; Fuccaro, M.; Maggioni, F.; Zanchin, G. A prospective study on osmophobia in migraine versus tension-type headache in a large series of attacks. Cephalalgia 2019, 40, 337–346. [Google Scholar] [CrossRef] [PubMed]
- Schenck, L.A.-M.; Andrasik, F. Behavioral and psychological aspects of cluster headache: An overview. Neurol. Sci. 2019, 40, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Luerding, R.; Henkel, K.; Gaul, C.; Dresler, T.; Lindwurm, A.; Paelecke-Habermann, Y.; Leinisch, E.; Jürgens, T.P. Aggressiveness in different presentations of cluster headache: Results from a controlled multicentric study. Cephalalgia 2012, 32, 528–536. [Google Scholar] [CrossRef] [PubMed]
- Brancato, G.; Macchia, S.; Murgia, M.; Signore, M.; Simeoni, G.; Blanke, K.; Körner, T.; Nimmergut, A.; Lima, P.; Paulino, R.; et al. Handbook of Recommended Practices for Questionnaire Development and Testing in the European Statistical System; European Commission: Brussels, Belgium, 2006; Available online: http://www.istat.it/en/files/2013/12/Handbook_questionnaire_development_2006.pdf (accessed on 11 September 2020).
- Lombard, L.; Farrar, M.; Ye, W.; Kim, Y.; Cotton, S.; Buchanan, A.; Jackson, J.; Joshi, S. A global real-world assessment of the impact on health-related quality of life and work productivity of migraine in patients with insufficient versus good response to triptan medication. J. Headache Pain 2020, 21, 1–16. [Google Scholar] [CrossRef]
- Ueda, K.; Ye, W.; Lombard, L.; Kuga, A.; Kim, Y.; Cotton, S.; Jackson, J.; Treuer, T. Real-world treatment patterns and patient-reported outcomes in episodic and chronic migraine in Japan: Analysis of data from the Adelphi migraine disease specific programme. J. Headache Pain 2019, 20, 1–11. [Google Scholar] [CrossRef]
- GBD 2016 Headache Collaborators. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018, 17, 954–976. [Google Scholar] [CrossRef]
- Woods, K.; Ostrowski-Delahanty, S.; Cieplinski, T.; Winkelman, J.; Polk, P.; Victorio, M.C. Psychosocial and Demographic Characteristics of Children and Adolescents with Headache Presenting for Treatment in a Headache Infusion Center. Headache J. Head Face Pain 2019, 59, 858–868. [Google Scholar] [CrossRef] [PubMed]
- Al-Hashel, J.Y.; Alroughani, R.; Shauibi, S.; Alashqar, A.; Alhamdan, F.; Althufairi, H.; Owayed, S.; Ahmed, S.F. Impact of primary headache disorder on quality of life among school students in Kuwait. J. Headache Pain 2020, 21, 1–6. [Google Scholar] [CrossRef] [PubMed]
| Assessment Instruments | Primary Headache | ||
|---|---|---|---|
| Migraine | TTH | CH | |
| Disability Assessments | |||
| MIDAS | N = 80 [19,21,25,26,28,29,30,31,32,36,37,38,39,40,41,42,44,46,47,48,50,52,54,55,57,63,64,65,66,67,69,70,71,73], [75,76,77,80,81,82,84,85,88,89,90,91,92,94,98,99,102,103,105,106,108,109,110,116,118,119,125], [130,132,133,136,141,142,144], [147,148,149,154,155,156,157,159,162,164,165,167] | N = 4 [94,105,112,133] | N = 2 [126,128] |
| HIT-6 | N = 56 [22,23,29,32,33,34,35,39,43,46,50,51,52,58,62,68,74,75,83,89,92,93,96,97,100,101,103,104,106,107,111,114,115,116,117,118], [121,124,131,132,137,139,140,142,143], [146,147,148,151,152,153,157,160,161,166,168] | N = 8 [35,45,93,97,111], [115,161,166] | N = 7 [20,59,61,86,87], [126,128] |
| HDI | N = 6 [63,93,123,137,138,158] | N = 6 [24,78,79,93,120,129] | N = 1 [56] |
| WHODAS 2.0; WHODAS-12 | N = 11 [36,93,95,110,127,130,155], [156,158,164,165] | N = 1 [93] | |
| HURT | N = 3 [72,82,133] | N = 2 [72,133] | |
| PDI | N = 2 [81,168] | ||
| PROMIS-PI 6a; PROMIS-PI 6b | N = 2 [44,75] | ||
| PROMIS-PF 10a | N = 2 [68,124] | ||
| NDI | N = 1 [45] | ||
| HDQ | N = 1 [93] | N = 1 [93] | |
| CHS | N = 1 [56] | ||
| MFIQ | N = 1 [68] | ||
| MPFID | N = 1 [124] | ||
| Work-related difficulties assessments | |||
| WPAI | N = 3 [27,30,44] | ||
| HEADWORK | N = 2 [43,110] | ||
| Quality of life assessments | |||
| MSQ | N = 27 [34,36,38,53,68,69,75,92,96,100,103], [110,116,119,124,125,127,130,139,147], [148,154,155,156,158,164,165] | N = 1 [135] | |
| SF-36; SF-12; SF-8 | N = 10 [34,42,60,97,121,122], [134,145,154,158] | N = 4 [97,112,120,122] | N = 4 [61,87,128,135] |
| EQ-5D-5L | N = 4 [34,74,113,168] | N = 2 [126,135] | |
| CHQQ | N = 1 [133] | N = 1 [133] | |
| EUROHIS-QOL 8-item | N = 2 [72,150] | N = 2 [72,150] | |
| 24-h MQoLQ | N = 1 [49] | ||
| CHQ | N = 1 [135] | ||
| Assessment Instruments | ICF Domain | No. of Linked ICF Categories | ||
|---|---|---|---|---|
| BF | A&P | EF | ||
| Disability assessments | ||||
| MIDAS | b280 | d620,d640,d650,d660,d750,d760,d830,d850,d920 | 10 | |
| HIT-6 | b130,b152,b280, | d160,d230,d640,d650,d620,d830,d850,d920 | 11 | |
| HDI | b130,b152,b140,b160,b164,b780 | d160,d161,d163,d166,d230,d470,d475,d730,d740,d750,d760,d920 | 18 | |
| WHODAS 2.0 | b140,b144,b152 | d160,d161,d155,d175,d315,d350,d410,d415,d450,d460,d510,d540,d550,d630,d640,d650,d720,d730,d750,d760,d770,d850,d910,d920,d930 | e150,e155,e160,e165,e460 | 33 |
| HURT | d630,d640,d650,d750,d760,d850,d830,d920 | 8 | ||
| PDI | d550,d630,d640,d650,d660,d770,d850,d855,d920 | 9 | ||
| PROMIS-PI 6a | d230,d630,d640,d650,d920 | 5 | ||
| PROMIS-PI 6b | b140 | d160,d161,d230,d430,d620,d630,d640,d650,d720,d730,d740,d750,d920 | 14 | |
| PROMIS-PF 10a; | d410,d430,d445,d450,d455,d510,d530,d540,d620,d640,d920 | 11 | ||
| NDI | b134,b140,b280 | d160,d161,d166,d430,d475,d510,d540,d850,d920 | 12 | |
| HDQ | b280 | d630,d640,d650,d750,d760,d830,d850,d920 | 9 | |
| CHS | b130,b152 | d230,d920 | 4 | |
| MFIQ | b130,b152 | d160,d161,d230,d410,d510,d520,d620,d630,d640,d650,d660,d740,d750,d760,d770, d830,d850,d920 | e240,e250,e260 | 23 |
| MPFID | b140 | d160,d161,d230,d410,d630,d640,d650,d710,d720 | 10 | |
| Work-related difficulties assessments | ||||
| WPAI | d230,d850 | 2 | ||
| HEADWORK | b140 | d160,d161,d166,d170,d175,d210,d220,d240,d310,d350,d360,d460,d475,d710,d720,d740,d750 | e240,e250,e260,e425 | 22 |
| Quality of life assessments | ||||
| MSQ | b130,b152 | d160,d166,d230,d630,d640,d650,d750,d760,d850,d920 | 12 | |
| SF-36 | b130,b152,b280 | d410,d430,d445,d450,d455,d510,d540,d620,d630,d640,d650,d750,d760,d850,d920 | 18 | |
| EQ-5D-5L | b152,b280 | d450,d510,d540,d630,d640,d650,d660,d830,d850,d920 | 12 | |
| CHQQ | b130,b140,b152,b160 | d160,d161,d163,d630,d640,d650,d750,d760,d770,d850,d920 | 15 | |
| EUROHIS-QOL 8-item | b130 | d230,d750,d760 | 4 | |
| 24-h MQoLQ | b110,b130,b134,b152,b280,b535 | d620,d640,d650,d710,d720,d730,d740,d750,d760,d830,d850 | e240,e250 | 19 |
| CHQ | b130,b134,b140,b144,b152,b160,b280 | d110,d160,d161,d166,d230,d510,d520,d540,d750,d760,d770,d850,d920 | e215,e250 | 22 |
| ICF Domains and Categories | Primary Headache | Common to the Three Disorders | ||
|---|---|---|---|---|
| Migraine | TTH | CH | ||
| Body Functions | ||||
| b130-Energy and drive | √ | √ | √ | √ |
| b140-Attention | √ | √ | ||
| b152-Emotional functions | √ | √ | √ | √ |
| b280-Pain | √ | √ | √ | √ |
| Activities and Participation | ||||
| d160-Focusing attention | √ | √ | √ | √ |
| d161-Directing attention | √ | √ | √ | √ |
| d166-Reading | √ | √ | ||
| d230-Carrying out daily routine | √ | √ | √ | √ |
| d510-Washing oneself | √ | √ | ||
| d540-Dressing | √ | |||
| d620-Acquisition of goods and services | √ | √ | √ | √ |
| d630-Preparing meals | √ | √ | √ | √ |
| d640-Doing housework | √ | √ | √ | √ |
| d650-Caring for household objects | √ | √ | √ | √ |
| d750-Informal social relationships | √ | √ | √ | √ |
| d760-Family relationships | √ | √ | √ | √ |
| d830-Higher education | √ | √ | √ | √ |
| d850-Remunerative employment | √ | √ | √ | √ |
| d920-Recreation and leisure | √ | √ | √ | √ |
| Total no. of ICF categories | 16 | 18 | 18 | 15 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
D'Amico, D.; Tepper, S.J.; Guastafierro, E.; Toppo, C.; Leonardi, M.; Grazzi, L.; Martelletti, P.; Raggi, A. Mapping Assessments Instruments for Headache Disorders against the ICF Biopsychosocial Model of Health and Disability. Int. J. Environ. Res. Public Health 2021, 18, 246. https://doi.org/10.3390/ijerph18010246
D'Amico D, Tepper SJ, Guastafierro E, Toppo C, Leonardi M, Grazzi L, Martelletti P, Raggi A. Mapping Assessments Instruments for Headache Disorders against the ICF Biopsychosocial Model of Health and Disability. International Journal of Environmental Research and Public Health. 2021; 18(1):246. https://doi.org/10.3390/ijerph18010246
Chicago/Turabian StyleD'Amico, Domenico, Stewart J. Tepper, Erika Guastafierro, Claudia Toppo, Matilde Leonardi, Licia Grazzi, Paolo Martelletti, and Alberto Raggi. 2021. "Mapping Assessments Instruments for Headache Disorders against the ICF Biopsychosocial Model of Health and Disability" International Journal of Environmental Research and Public Health 18, no. 1: 246. https://doi.org/10.3390/ijerph18010246
APA StyleD'Amico, D., Tepper, S. J., Guastafierro, E., Toppo, C., Leonardi, M., Grazzi, L., Martelletti, P., & Raggi, A. (2021). Mapping Assessments Instruments for Headache Disorders against the ICF Biopsychosocial Model of Health and Disability. International Journal of Environmental Research and Public Health, 18(1), 246. https://doi.org/10.3390/ijerph18010246





