The Relationship between Adverse Childhood Experiences and Sleep Problems among Adolescent Students: Mediation by Depression or Anxiety
Abstract
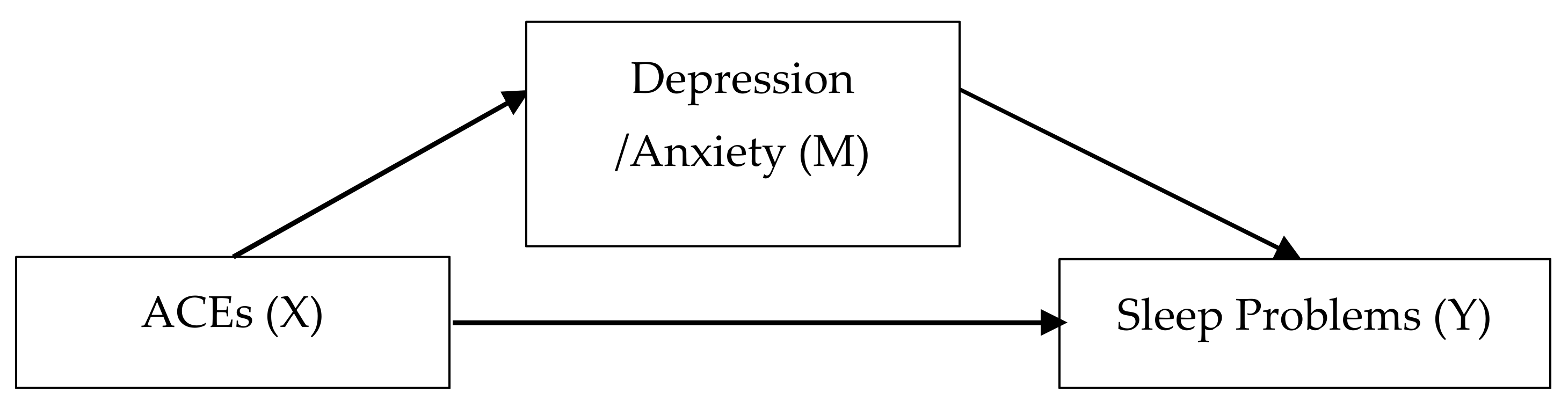
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.2.1. Early Trauma Inventory Self Report–Short Form (ETISR-SF)
2.2.2. List of Threatening Experiences Questionnaire (LTE-Q)
2.2.3. Insomnia Severity Index (ISI)
2.2.4. Epworth Sleepiness Scale (ESS)
2.2.5. School Sleep Habits Survey (SSS)
2.2.6. Children’s Depression Inventory (CDI)
2.2.7. Revised Children’s Manifest Anxiety Scale (RCMAS)
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brindle, R.C.; Cribbet, M.R.; Samuelsson, L.B.; Gao, C.; Frank, E.; Krafty, R.T.; Thayer, J.F.; Buysse, D.J.; Hall, M.H. The Relationship between Childhood Trauma and Poor Sleep Health in Adulthood. Psychosom. Med. 2018, 80, 200–207. [Google Scholar] [CrossRef] [PubMed]
- CDC. Available online: https://www.cdc.gov/violenceprevention/childabuseandneglect/aces/fastfact.html (accessed on 27 May 2020).
- Friedman, E.M.; Montez, J.K.; Sheehan, C.M.D.; Guenewald, T.L.; Seeman, T.E. Childhood Adversities and Adult Cardiometabolic Health: Does the Quantity, Timing, and Type of Adversity Matter? J. Aging Health 2015, 27, 1311–1338. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Raffeld, M.R.; Slopen, N.; Hale, L.; Dunn, E.C. Childhood adversity and insomnia in adolescence. Sleep Med. 2016, 21, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Kwon, J.S.; Kim, D.; Kim, S.W.; Kim, J.J.; Kim, J.H.; Nam, H.J.; Ryu, S.; Park, I.H.; An, S.K.; et al. Prevalence of Metabolic Syndrome in Patients with Schizophrenia in Korea: A Multicenter Nationwide Cross-Sectional Study. Psychiatry Investig. 2017, 14, 44–50. [Google Scholar] [CrossRef]
- Lee, S.Y.; Ahn, K.; Kim, J.; Jang, G.C.; Min, T.K.; Yang, H.J.; Pyun, B.Y.; Kwon, J.W.; Sohn, M.H.; Kim, K.W.; et al. A Multicenter Retrospective Case Study of Anaphylaxis Triggers by Age in Korean Children. Allergy Asthma Immunol. Res. 2016, 8, 535–540. [Google Scholar] [CrossRef]
- Kandel, D.B.; Davies, M. Epidemiology of depressive mood in adolescents: An empirical study. Arch. Gen. Psychiatry 1982, 39, 1205–1212. [Google Scholar] [CrossRef]
- Poole, J.C.; Dobson, K.S.; Pusch, D. Anxiety among adults with a history of childhood adversity: Psychological resilience moderates the indirect effect of emotion dysregulation. J. Affect. Disord. 2017, 217, 144–152. [Google Scholar] [CrossRef]
- Chapman, D.P.; Wheaton, A.G.; Anda, R.F.; Croft, J.B.; Edwards, V.J.; Liu, Y.; Sturgis, S.L.; Perry, G.S. Adverse childhood experiences and sleep disturbances in adults. Sleep Med. 2011, 12, 773–779. [Google Scholar] [CrossRef]
- Koskenvuo, K.; Hublin, C.; Partinen, M.; Paunio, T.; Koskenvuo, M. Childhood adversities and quality of sleep in adulthood: A population-based study of 26,000 Finns. Sleep Med. 2010, 11, 17–22. [Google Scholar] [CrossRef]
- Greenfield, E.A.; Lee, C.; Friedman, E.L.; Springer, K.W. Childhood abuse as a risk factor for sleep problems in adulthood: Evidence from a U.S. National Study. Ann. Behav. Med. 2011, 42, 245–256. [Google Scholar] [CrossRef]
- Kajeepeta, S.; Gelaye, B.; Jackson, C.L.; Williams, M.A. Adverse childhood experiences are associated with adult sleep disorders: A systematic review. Sleep Med. 2015, 16, 320–330. [Google Scholar] [CrossRef] [PubMed]
- Schafer, V.; Bader, K. Relationship between early-life stress load and sleep in psychiatric outpatients: A sleep diary and actigraphy study. Stress Health 2013, 29, 177–189. [Google Scholar] [CrossRef] [PubMed]
- Zhabenko, N.; Wojnar, M.; Brower, K.J. Prevalence and correlates of insomnia in a Polish sample of alcohol-dependent patients. Alcohol. Clin. Exp. Res. 2012, 36, 1600–1607. [Google Scholar] [CrossRef] [PubMed]
- Bader, K.; Schäfer, V.; Schenkel, M.; Nissen, L.; Schwander, J. Adverse childhood experiences associated with sleep in primary insomnia. J. Sleep Res. 2007. [Google Scholar] [CrossRef]
- Kelly-Irving, M.; Lepage, B.; Dedieu, D.; Bartley, M.; Blane, D.; Grosclaude, P.; Lang, T.; Delpierre, C. Adverse childhood experiences and premature all-cause mortality. Eur. J. Epidemiol. 2013, 28, 721–734. [Google Scholar] [CrossRef]
- Koren, D.; Arnon, I.; Lavie, P.; Klein, E. Sleep complaints as early predictors of posttraumatic stress disorder: A 1-year prospective study of injured survivors of motor vehicle accidents. Am. J. Psychiatry 2002, 159, 855–857. [Google Scholar] [CrossRef]
- Bremner, J.D.; Bolus, R.; Mayer, E.A. Psychometric properties of the Early Trauma Inventory-Self Report. J. Nerv. Ment. Dis. 2007, 195, 211–218. [Google Scholar] [CrossRef]
- Jeon, J.R.; Lee, E.H.; Lee, S.W.; Jeong, E.G.; Kim, J.H.; Lee, D.; Jeon, H.J. The early trauma inventory self report-short form: Psychometric properties of the korean version. Psychiatry Investig. 2012, 9, 229–235. [Google Scholar] [CrossRef]
- Park, S. Reliability and Validity of the Early Trauma Inventory Self Report-Short Form among Korean Adolescents. J. Korean Acad. Child. Adolesc. Psychiatry 2018, 29, 2–6. [Google Scholar] [CrossRef]
- Brugha, T.S.; Cragg, D. The List of Threatening Experiences: The reliability and validity of a brief life events questionnaire. Acta Psychiatr. Scand. 1990, 82, 77–81. [Google Scholar] [CrossRef]
- CM, M. Insomnia: Psychological Assessment and Management; Guilford Press: New York, NY, USA, 1993. [Google Scholar]
- Cho, Y.W.; Song, M.L.; Morin, C.M. Validation of a Korean version of the insomnia severity index. J. Clin. Neurol. 2014, 10, 210–215. [Google Scholar] [CrossRef]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef]
- Cho, Y.W.; Lee, J.H.; Son, H.K.; Lee, S.H.; Shin, C.; Johns, M.W. The reliability and validity of the Korean version of the Epworth sleepiness scale. Sleep Breath 2011, 15, 377–384. [Google Scholar] [CrossRef]
- Joo, S.; Shin, C.; Kim, J.; Yi, H.; Ahn, Y.; Park, M.; Kim, J.; Lee, S. Prevalence and correlates of excessive daytime sleepiness in high school students in Korea. Psychiatry Clin. Neurosci. 2005, 59, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Wolfson, A.R.; Carskadon, M.A. Sleep schedules and daytime functioning in adolescents. Child. Dev. 1998, 69, 875–887. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.-C.L.Y. Development of the Korean form of the Kovacs’ Children’s Depression Inventory. J. Korean Neuropsychiatr. Assoc. 1990, 29, 943–956. [Google Scholar]
- Bang, Y.R.; Park, J.H.; Kim, S.H. Cut-Off Scores of the Children’s Depression Inventory for Screening and Rating Severity in Korean Adolescents. Psychiatry Investig. 2015, 12, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Kovacs, M. The Children’s Depression, Inventory (CDI). Psychopharmacol. Bull. 1985, 21, 995–998. [Google Scholar]
- Reynolds, R.B. Factor structure and construct validity of “what I think and feel”: The revised Children’s manifest anxiety scale. J. Pers Assess. 1979, 43, 281–283. [Google Scholar] [CrossRef]
- Choi, J.S.; Cho, C.S. Assessment of anxiety in children: Reliability and validity of revised Children’s manifest anxiety scale. J. Korean Neuropsychiatr. Assoc. 1990, 29, 691–702. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process. Analysis: A Regression-Based Approach; Guilford Press: New York, NY, US, 2013; p. xvii507. [Google Scholar]
- Preacher, K.J.; Rucker, D.D.; Hayes, A.F. Addressing Moderated Mediation Hypotheses: Theory, Methods, and Prescriptions. Mult. Behave. Res. 2007, 42, 185–227. [Google Scholar] [CrossRef] [PubMed]
- Preacher, K.J.; Hayes, A.F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods 2008, 40, 879–891. [Google Scholar] [CrossRef] [PubMed]
- Noll, J.G.; Trickett, P.K.; Susman, E.J.; Putnam, F.W. Sleep disturbances and childhood sexual abuse. J. Pediatr. Psychol. 2006, 31, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Chapman, D.P.; Liu, Y.; Presley-Cantrell, L.R.; Edwards, V.J.; Wheaton, A.G.; Perry, G.S.; Croft, J.B. Adverse childhood experiences and frequent insufficient sleep in 5 U.S. States, 2009: A retrospective cohort study. BMC Public Health 2013, 13, 3. [Google Scholar] [CrossRef]
- Brower, K.J.; Wojnar, M.; Sliwerska, E.; Armitage, R.; Burmeister, M. PER3 polymorphism and insomnia severity in alcohol dependence. Sleep 2012, 35, 571–577. [Google Scholar] [CrossRef]
- Cuddy, M.A.; Belicki, K. Nightmare frequency and related sleep disturbance as indicators of a history of sexual abuse. Dreaming 1992, 2, 15–22. [Google Scholar] [CrossRef]
- Bader, K.; Schafer, V.; Schenkel, M.; Nissen, L.; Kuhl, H.C.; Schwander, J. Increased nocturnal activity associated with adverse childhood experiences in patients with primary insomnia. J. Nerv. Ment. Dis. 2007, 195, 588–595. [Google Scholar] [CrossRef]
- Bader, K.; Schafer, V.; Nissen, L.; Schenkel, M. Heightened beta EEG activity during nonrapid eye movement sleep in primary insomnia patients with reports of childhood maltreatment. J. Clin. Neurophysiol. 2013, 30, 188–198. [Google Scholar] [CrossRef]
- Heitkemper, M.M.; Cain, K.C.; Burr, R.L.; Jun, S.E.; Jarrett, M.E. Is childhood abuse or neglect associated with symptom reports and physiological measures in women with irritable bowel syndrome? Biol. Res. Nurs. 2011, 13, 399–408. [Google Scholar] [CrossRef]
- Gwadz, M.V.; Nish, D.; Leonard, N.R.; Strauss, S.M. Gender differences in traumatic events and rates of post-traumatic stress disorder among homeless youth. J. Adolesc. 2007, 30, 117–129. [Google Scholar] [CrossRef]
- Costello, E.J.; Erkanli, A.; Fairbank, J.A.; Angold, A. The prevalence of potentially traumatic events in childhood and adolescence. J. Trauma Stress 2002, 15, 99–112. [Google Scholar] [CrossRef] [PubMed]
- Tran, Q.A.; Dunne, M.P.; Vo, T.V.; Luu, N.H. Adverse Childhood Experiences and the Health of University Students in Eight Provinces of Vietnam. Asia Pac. J. Public Health 2015, 27, 26s–32s. [Google Scholar] [CrossRef] [PubMed]
- Ryu, J.H.; Lee, J.; Jung, I.; Song, A.; Lee, M. Understanding Connections Among Abuse and Violence in the Life Course (Report No. 2017–49); Korea Institute for Health and Social Affairs: Sejong, Korea, 2017. [Google Scholar]
- Frazier, P.; Anders, S.; Perera, S.; Tomich, P.; Tennen, H.; Park, C.; Tashiro, T. Traumatic Events among Undergraduate Students: Prevalence and Associated Symptoms. J. Counsel. Psychol. 2009, 56, 450–460. [Google Scholar] [CrossRef]
- Valente, S.M. Sexual abuse of boys. J. Child. Adolesc. Psychiatr. Nurs. 2005, 18, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Riemann, D.; Spiegelhalder, K.; Feige, B.; Voderholzer, U.; Berger, M.; Perlis, M.; Nissen, C. The hyperarousal model of insomnia: A review of the concept and its evidence. Sleep Med. Rev. 2010, 14, 19–31. [Google Scholar] [CrossRef]
- Felitti, V.J.; Anda, R.F.; Nordenberg, D.; Williamson, D.F.; Spitz, A.M.; Edwards, V.; Koss, M.P.; Marks, J.S. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am. J. Prev. Med. 1998, 14, 245–258. [Google Scholar] [CrossRef]
- Anda, R.F.; Felitti, V.J.; Bremner, J.D.; Walker, J.D.; Whitfield, C.; Perry, B.D.; Dube, S.R.; Giles, W.H. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. Eur. Arch. Psychiatry Clin. Neurosci. 2006, 256, 174–186. [Google Scholar] [CrossRef]
- Lee, C.; Tsenkova, V.; Carr, D. Childhood trauma and metabolic syndrome in men and women. Soc. Sci. Med. 2014, 105, 122–130. [Google Scholar] [CrossRef]
- Kesebir, S. Metabolic syndrome and childhood trauma: Also comorbidity and complication in mood disorder. World J. Clin. Cases 2014, 2, 332–337. [Google Scholar] [CrossRef]
- Williamson, D.F.; Thompson, T.J.; Anda, R.F.; Dietz, W.H.; Felitti, V. Body weight and obesity in adults and self-reported abuse in childhood. Int. J. Obes. Relat. Metab. Disord. 2002, 26, 1075–1082. [Google Scholar] [CrossRef]
- Dong, M.; Giles, W.H.; Felitti, V.J.; Dube, S.R.; Williams, J.E.; Chapman, D.P.; Anda, R.F. Insights into causal pathways for ischemic heart disease: Adverse childhood experiences study. Circulation 2004, 110, 1761–1766. [Google Scholar] [CrossRef] [PubMed]
- Spilsbury, J.C. Sleep as a mediator in the pathway from violence-induced traumatic stress to poorer health and functioning: A review of the literature and proposed conceptual model. Behav. Sleep Med. 2009, 7, 223–244. [Google Scholar] [CrossRef] [PubMed]
- Dube, S.R.; Anda, R.F.; Felitti, V.J.; Edwards, V.J.; Croft, J.B. Adverse childhood experiences and personal alcohol abuse as an adult. Addict. Behav. 2002, 27, 713–725. [Google Scholar] [CrossRef]
- Dube, S.R.; Felitti, V.J.; Dong, M.; Chapman, D.P.; Giles, W.H.; Anda, R.F. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: The adverse childhood experiences study. Pediatrics 2003, 111, 564–572. [Google Scholar] [CrossRef]
- Wang, J.; Geng, L. Effects of Socioeconomic Status on Physical and Psychological Health: Lifestyle as a Mediator. Int. J. Environ. Res. Public Health 2019, 16, 281. [Google Scholar] [CrossRef]
- Briggs-Gowan, M.J.; Carter, A.S.; Clark, R.; Augustyn, M.; McCarthy, K.J.; Ford, J.D. Exposure to potentially traumatic events in early childhood: Differential links to emergent psychopathology. J. Child. Psychol. Psychiatry 2010, 51, 1132–1140. [Google Scholar] [CrossRef]
- Allen, J.L.; Rapee, R.M.; Sandberg, S. Severe life events and chronic adversities as antecedents to anxiety in children: A matched control study. J. Abnormal Child. Psychol. 2008, 36, 1047. [Google Scholar] [CrossRef]
- Hazel, N.A.; Hammen, C.; Brennan, P.A.; Najman, J. Early childhood adversity and adolescent depression: The mediating role of continued stress. Psychol. Med. 2008, 38, 581–589. [Google Scholar] [CrossRef]
| Variables | ETI+ (N = 576) | ETI− (N = 161) | t, F, χ2 | p | p† | |
|---|---|---|---|---|---|---|
| M (SD), N | M (SD), N | |||||
| Age | 15.06 (1.39) | 15.14(1.30) | −0.673 | 0.501 | — | |
| Sex | Boys | 356 | 92 | 1.148 | 0.284 | 0.284 |
| Girls | 220 | 69 | ||||
| Monthly family income 1 | 270.00 (155.46) | 313.03 (182.20) | −1.099 | 0.274 | ||
| Parental education (years) | Mother | 12.44 (2.45) | 12.67 (2.50) | 0.656 | 0.513 | |
| Father | 12.83 (2.59) | 13.15 (2.69) | 0.765 | 0.445 | ||
| ISI | 5.64(4.23) | 4.22 (3.82) | 3.854 | <0.001 *** | <0.001 *** | |
| ESS | 6.90 (4.24) | 5.60 (3.58) | 3.883 | <0.001 *** | <0.001 *** | |
| SSS_prob | 18.67 (5.78) | 16.61(4.77) | 4.622 | <0.001 *** | <0.001 *** | |
| CDI | 15.51 (7.04) | 13.43 (6.70) | 3.230 | 0.001 ** | 0.001 ** | |
| RCMAS | 14.88 (6.29) | 11.63 (6.05) | 5.832 | <0.001 *** | <0.001 *** | |
| Variables | LTE+ (N = 205) | LTE− (N = 532) | t, F, χ2 | p | p† | |
| M (SD), N | M (SD), N | |||||
| Age | 15.04 (1.38) | 15.10 (1.36) | −0.520 | 0.603 | — | |
| Sex | Boys | 120 | 328 | 0.559 | 0.437 | 0.437 |
| Girls | 85 | 204 | ||||
| Monthly family income 1 | 252.86 (182.28) | 322.48 (174.20) | 2.034 | 0.044 | ||
| Parental education (years) | Mother | 12.51 (2.50) | 12.48 (2.44) | −0.115 | 0.908 | |
| Father | 12.90 (2.59) | 12.88 (2.62) | −0.060 | 0.952 | ||
| ISI | 6.74 (4.77) | 4.79 (3.79) | 5.233 | <0.001 *** | <0.001 *** | |
| ESS | 7.40 (4.00) | 6.30 (4.15) | 3.247 | 0.001 ** | 0.001 ** | |
| SSS_prob | 20.11 (5.90) | 17.50 (5.36) | 5.772 | <0.001 *** | <0.001 *** | |
| CDI | 16.90 (7.16) | 14.34 (6.84) | 4.345 | <0.001 *** | <0.001 *** | |
| RCMAS | 16.56 (6.15) | 13.25 (6.22) | 3.230 | <0.001 *** | <0.001 *** | |
| Model | Variables | Mediator Variable: CDI | Dependent Variable: ISI | ||||
|---|---|---|---|---|---|---|---|
| 1 | B | S.E | t | B | S.E | t | |
| Constant | 12.94 | 0.38 | 34.45 | 2.02 | 0.35 | 5.80 | |
| ETI | 0.57 | 0.07 | 7.76 | 0.28 | 0.04 | 6.56 | |
| CDI | 0.15 | 0.02 | 6.77 | ||||
| = 0.08, F = 60.16, p < 0.001 | = 0.15, F = 62.15, p < 0.001 | ||||||
| Effect | Boot SE | 95% Boot LLCI | 95% Boot ULCI | ||||
| Indirect effect | 0.0831 | 0.0169 | 0.0536 | 0.1207 | |||
| Direct effect | 0.2827 | 0.0431 | 0.1981 | 0.3673 | |||
| 2 | Mediator Variable: RCMAS | Dependent Variable: ISI | |||||
| B | S.E | t | B | S.E | t | ||
| Constant | 11.48 | 0.32 | 36.41 | 1.01 | 0.33 | 3.04 | |
| ETI | 0.73 | 0.06 | 11.72 | 0.16 | 0.04 | 3.61 | |
| RCMAS | 0.26 | 0.02 | 11.34 | ||||
| = 0.16, F = 137.43, p < 0.001 | = 0.22, F = 103.42, p < 0.001 | ||||||
| Effect | Boot SE | 95% Boot LLCI | 95% Boot ULCI | ||||
| Indirect effect | 0.1936 | 0.0240 | 0.1496 | 0.2439 | |||
| Direct effect | 0.1552 | 0.0430 | 0.0709 | 0.2396 | |||
| 3 | Mediator Variable: CDI | Dependent Variable: ISI | |||||
| B | S.E | t | B | S.E | t | ||
| Constant | 14.45 | 0.30 | 47.82 | 2.32 | 0.35 | 6.71 | |
| LTE | 1.63 | 0.39 | 4.16 | 1.12 | 0.22 | 5.15 | |
| CDI | 0.17 | 0.02 | 7.95 | ||||
| = 0.02, F = 17.27, p < 0.001 | = 0.13, F = 52.59, p < 0.001 | ||||||
| Effect | Boot SE | 95% Boot LLCI | 95% Boot ULCI | ||||
| Indirect effect | 0.2728 | 0.0725 | 0.1434 | 0.4229 | |||
| Direct effect | 1.1281 | 0.2184 | 0.6993 | 1.5570 | |||
| 4 | Mediator Variable: RCMAS | Dependent Variable: ISI | |||||
| B | S.E | t | B | S.E | t | ||
| Constant | 13.28 | 0.26 | 51.19 | 1.12 | 0.33 | 3.37 | |
| LTE | 2.38 | 0.34 | 7.10 | 0.76 | 0.21 | 3.68 | |
| RCMAS | 0.28 | 0.02 | 12.55 | ||||
| = 0.06, F = 50.34, p < 0.001 | = 0.22, F = 103.87, p < 0.001 | ||||||
| Effect | Boot SE | 95% Boot LLCI | 95% Boot ULCI | ||||
| Indirect effect | 0.6604 | 0.1071 | 0.4602 | 0.8824 | |||
| Direct effect | 0.7686 | 0.2078 | 0.3606 | 1.1766 | |||
| 5 | Mediator Variable: CDI | Dependent Variable: ESS | |||||
| B | S.E | t | B | S.E | t | ||
| Constant | 12.94 | 0.38 | 34.49 | 4.78 | 0.36 | 13.14 | |
| ETI | 0.57 | 0.07 | 7.76 | 0.16 | 0.04 | 3.51 | |
| CDI | 0.08 | 0.02 | 3.57 | ||||
| = 0.08, F = 60.26, p < 0.001 | = 0.05, F = 17.53, p < 0.001 | ||||||
| Effect | Boot SE | 95% Boot LLCI | 95% Boot ULCI | ||||
| Indirect effect | 0.0457 | 0.0150 | 0.0186 | 0.0776 | |||
| Direct effect | 0.1576 | 0.0449 | 0.0694 | 0.2458 | |||
| 6 | Mediator Variable: RCMAS | Dependent Variable: ESS | |||||
| B | S.E | t | B | S.E | t | ||
| Constant | 11.48 | 0.31 | 36.49 | 3.86 | 0.36 | 10.84 | |
| ETI | 0.73 | 0.06 | 11.74 | 0.09 | 0.05 | 1.88 | |
| RCMAS | 0.17 | 0.02 | 6.89 | ||||
| = 0.15, F = 137.79, p < 0.001 | = 0.09, F = 36.37, p < 0.001 | ||||||
| Effect | Boot SE | 95% Boot LLCI | 95% Boot ULCI | ||||
| Indirect effect | 0.1258 | 0.0224 | 0.0845 | 0.1727 | |||
| Direct effect | 0.0862 | 0.0459 | −0.0040 | 0.1764 | |||
| 7 | Mediator Variable: CDI | Dependent Variable: ESS | |||||
| B | S.E | t | B | S.E | t | ||
| Constant | 14.45 | 0.30 | 47.90 | 4.91 | 0.36 | 13.71 | |
| LTE | 1.63 | 0.39 | 4.16 | 0.70 | 0.23 | 3.13 | |
| CDI | 0.09 | 0.02 | 4.26 | ||||
| = 0.02, F = 17.31, p < 0.001 | = 0.05, F = 16.44, p < 0.001 | ||||||
| Effect | Boot SE | 95% Boot LLCI | 95% Boot ULCI | ||||
| Indirect effect | 0.1486 | 0.0531 | 0.0591 | 0.2686 | |||
| Direct effect | 0.0717 | 0.2255 | 0.2589 | 1.1446 | |||
| 8 | Mediator Variable: RCMAS | Dependent Variable: ESS | |||||
| B | S.E | t | B | S.E | t | ||
| Constant | 13.28 | 0.26 | 51.33 | 3.92 | 0.36 | 11.00 | |
| LTE | 2.38 | 0.34 | 7.10 | 0.27 | 0.22 | 1.20 | |
| RCMAS | 0.18 | 0.02 | 7.73 | ||||
| = 0.06, F = 50.39, p < 0.001 | = 0.08, F = 35.17, p < 0.001 | ||||||
| Effect | Boot SE | 95% Boot LLCI | 95% Boot ULCI | ||||
| Indirect effect | 0.4364 | 0.0826 | 0.2876 | 0.6130 | |||
| Direct effect | 0.2614 | 0.2226 | −.1756 | 0.6984 | |||
| 9 | Mediator Variable: CDI | Dependent Variable: SSS_prob | |||||
| B | S.E | t | B | S.E | t | ||
| Constant | 12.93 | 0.37 | 34.54 | 15.12 | 0.49 | 30.68 | |
| ETI | 0.57 | 0.07 | 7.73 | 0.36 | 0.06 | 5.96 | |
| CDI | 0.11 | 0.03 | 3.60 | ||||
| = 0.08, F = 59.72, p < 0.001 | = 0.09, F = 32.98, p < 0.001 | ||||||
| Effect | Boot SE | 95% Boot LLCI | 95% Boot ULCI | ||||
| Indirect effect | 0.0621 | 0.0198 | 0.0247 | 0.1031 | |||
| Direct effect | 0.3629 | 0.0609 | 0.2434 | 0.4824 | |||
| 10 | Mediator Variable: RCMAS | Dependent Variable: SSS_prob | |||||
| B | S.E | t | B | S.E | t | ||
| Constant | 11.48 | 0.31 | 36.55 | 14.32 | 0.48 | 29.78 | |
| ETI | 0.74 | 0.06 | 11.79 | 0.25 | 0.06 | 3.96 | |
| RCMAS | 0.21 | 0.03 | 6.28 | ||||
| = 0.16, F = 139.05, p < 0.001 | = 0.11, F = 44.60, p < 0.001 | ||||||
| Effect | Boot SE | 95% Boot LLCI | 95% Boot ULCI | ||||
| Indirect effect | 0.1554 | 0.0298 | 0.1000 | 0.2153 | |||
| Direct effect | 0.2454 | 0.0620 | 0.1237 | 0.3671 | |||
| 11 | Mediator Variable: CDI | Dependent Variable: SSS_prob | |||||
| B | S.E | t | B | S.E | t | ||
| Constant | 14.42 | 0.30 | 47.88 | 15.51 | 0.49 | 31.77 | |
| LTE | 1.65 | 0.39 | 4.21 | 1.52 | 0.31 | 4.95 | |
| CDI | 0.14 | 0.03 | 4.59 | ||||
| = 0.03, F = 17.76, p < 0.001 | = 0.07, F = 27.07, p < 0.001 | ||||||
| Effect | Boot SE | 95% Boot LLCI | 95% Boot ULCI | ||||
| Indirect effect | 0.2242 | 0.0736 | 0.0976 | 0.3873 | |||
| Direct effect | 1.5213 | 0.3073 | 0.9179 | 2.1247 | |||
| 12 | Mediator Variable: RCMAS | Dependent Variable: SSS_prob | |||||
| B | S.E | t | B | S.E | t | ||
| Constant | 13.30 | 0.26 | 51.34 | 14.48 | 0.48 | 30.19 | |
| LTE | 2.37 | 0.34 | 7.08 | 1.13 | 0.30 | 3.78 | |
| RCMAS | 0.23 | 0.03 | 7.34 | ||||
| = 0.06, F = 50.06, p < 0.001 | = 0.11, F = 43.90, p < 0.001 | ||||||
| Effect | Boot SE | 95% Boot LLCI | 95% Boot ULCI | ||||
| Indirect effect | 0.5554 | 0.1113 | 0.3540 | 0.7881 | |||
| Direct effect | 1.1323 | 0.2996 | 0.5441 | 1.7204 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, E.-J.; Kim, S.-Y.; Kim, Y.; Sung, D.; Kim, B.; Hyun, Y.; Jung, K.-I.; Lee, S.-Y.; Kim, H.; Park, S.; et al. The Relationship between Adverse Childhood Experiences and Sleep Problems among Adolescent Students: Mediation by Depression or Anxiety. Int. J. Environ. Res. Public Health 2021, 18, 236. https://doi.org/10.3390/ijerph18010236
Park E-J, Kim S-Y, Kim Y, Sung D, Kim B, Hyun Y, Jung K-I, Lee S-Y, Kim H, Park S, et al. The Relationship between Adverse Childhood Experiences and Sleep Problems among Adolescent Students: Mediation by Depression or Anxiety. International Journal of Environmental Research and Public Health. 2021; 18(1):236. https://doi.org/10.3390/ijerph18010236
Chicago/Turabian StylePark, E-Jin, Shin-Young Kim, Yeeun Kim, Dajung Sung, Bora Kim, Yerin Hyun, Kyu-In Jung, Seung-Yup Lee, Hayeon Kim, Subin Park, and et al. 2021. "The Relationship between Adverse Childhood Experiences and Sleep Problems among Adolescent Students: Mediation by Depression or Anxiety" International Journal of Environmental Research and Public Health 18, no. 1: 236. https://doi.org/10.3390/ijerph18010236
APA StylePark, E.-J., Kim, S.-Y., Kim, Y., Sung, D., Kim, B., Hyun, Y., Jung, K.-I., Lee, S.-Y., Kim, H., Park, S., Kim, B.-N., & Park, M.-H. (2021). The Relationship between Adverse Childhood Experiences and Sleep Problems among Adolescent Students: Mediation by Depression or Anxiety. International Journal of Environmental Research and Public Health, 18(1), 236. https://doi.org/10.3390/ijerph18010236






