A Two-Year Longitudinal Study of the Association between Oral Frailty and Deteriorating Nutritional Status among Community-Dwelling Older Adults
Abstract
1. Introduction
2. Materials and Methods
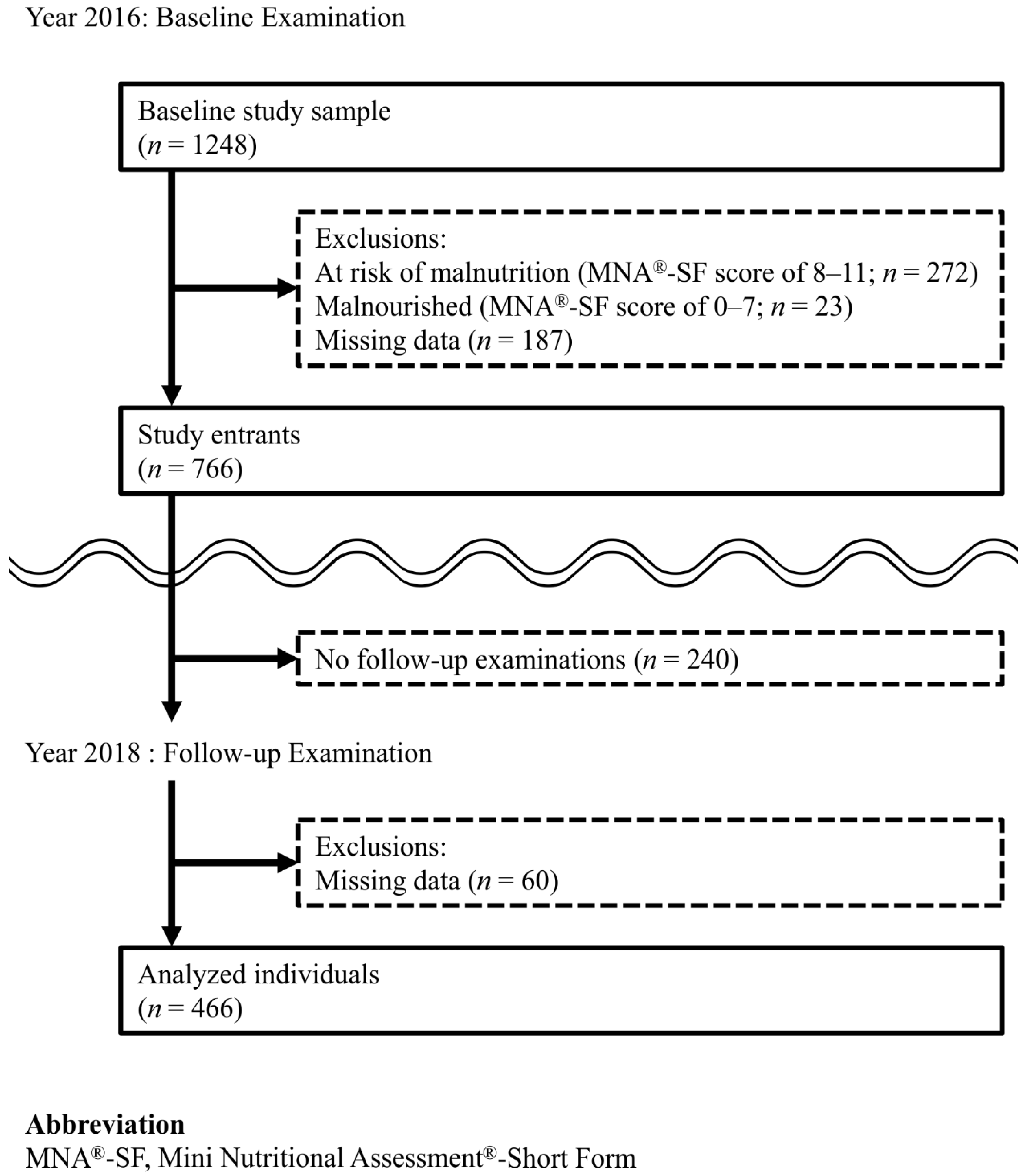
2.1. Study Population
2.2. Assessment of Nutritional Status
2.3. Assessment of Oral Health Status
2.4. Questionnaire Survey
2.5. Medical Interviews
2.6. Anthropometric Measurement
2.7. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- De Marchi, R.J.; Hugo, F.N.; Hilgert, J.B.; Padilha, D.M. Association between oral health status and nutritional status in south Brazilian independent-living older people. Nutrition 2008, 24, 546–553. [Google Scholar] [CrossRef] [PubMed]
- Kikutani, T.; Yoshida, M.; Enoki, H.; Yamashita, Y.; Akifusa, S.; Shimazaki, Y.; Hirano, H.; Tamura, F. Relationship between nutrition status and dental occlusion in community-dwelling frail elderly people. Geriatr. Gerontol. Int. 2013, 13, 50–54. [Google Scholar] [CrossRef] [PubMed]
- Okabe, Y.; Furuta, M.; Akifusa, S.; Takeuchi, K.; Adachi, M.; Kinoshita, T.; Kikutani, T.; Nakamura, S.; Yamashita, Y. Swallowing Function and Nutritional Status in Japanese Elderly People Receiving Home-care Services: A 1-year Longitudinal Study. J. Nutr. Health Aging 2016, 20, 697–704. [Google Scholar] [CrossRef] [PubMed]
- Okada, K.; Enoki, H.; Izawa, S.; Iguchi, A.; Kuzuya, M. Association between masticatory performance and anthropometric measurements and nutritional status in the elderly. Geriatr. Gerontol. Int. 2010, 10, 56–63. [Google Scholar] [CrossRef]
- Syrjala, A.M.; Pussinen, P.I.; Komulainen, K.; Nykanen, I.; Knuuttila, M.; Ruoppi, P.; Hartikainen, S.; Sulkava, R.; Ylostalo, P. Salivary flow rate and risk of malnutrition—A study among dentate, community-dwelling older people. Gerodontology 2013, 30, 270–275. [Google Scholar] [CrossRef]
- Iwasaki, M.; Yoshihara, A.; Ogawa, H.; Sato, M.; Muramatsu, K.; Watanabe, R.; Ansai, T.; Miyazaki, H. Longitudinal association of dentition status with dietary intake in Japanese adults aged 75 to 80 years. J. Oral Rehabil. 2016, 43, 737–744. [Google Scholar] [CrossRef]
- Ritchie, C.S.; Joshipura, K.; Hung, H.C.; Douglass, C.W. Nutrition as a mediator in the relation between oral and systemic disease: Associations between specific measures of adult oral health and nutrition outcomes. Crit. Rev. Oral Biol. Med. 2002, 13, 291–300. [Google Scholar] [CrossRef]
- Petersen, P.E.; Yamamoto, T. Improving the oral health of older people: The approach of the WHO Global Oral Health Programme. Community Dent. Oral Epidemiol. 2005, 33, 81–92. [Google Scholar] [CrossRef]
- Iwasaki, M.; Motokawa, K.; Watanabe, Y.; Shirobe, M.; Inagaki, H.; Edahiro, A.; Ohara, Y.; Hirano, H.; Shinkai, S.; Awata, S. Association Between Oral Frailty and Nutritional Status Among Community-Dwelling Older Adults: The Takashimadaira Study. J. Nutr. Health Aging 2020. [Google Scholar] [CrossRef]
- Tanaka, T.; Takahashi, K.; Hirano, H.; Kikutani, T.; Watanabe, Y.; Ohara, Y.; Furuya, H.; Tetsuo, T.; Akishita, M.; Iijima, K. Oral Frailty as a Risk Factor for Physical Frailty and Mortality in Community-Dwelling Elderly. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2018, 73, 1661–1667. [Google Scholar] [CrossRef] [PubMed]
- Correia, M.I.; Waitzberg, D.L. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin. Nutr. 2003, 22, 235–239. [Google Scholar] [CrossRef]
- Kaiser, M.J.; Bauer, J.M.; Ramsch, C.; Uter, W.; Guigoz, Y.; Cederholm, T.; Thomas, D.R.; Anthony, P.S.; Charlton, K.E.; Maggio, M.; et al. Frequency of malnutrition in older adults: A multinational perspective using the mini nutritional assessment. J. Am. Geriatr. Soc. 2010, 58, 1734–1738. [Google Scholar] [CrossRef] [PubMed]
- Sahyoun, N.R.; Jacques, P.F.; Dallal, G.; Russell, R.M. Use of albumin as a predictor of mortality in community dwelling and institutionalized elderly populations. J. Clin. Epidemiol. 1996, 49, 981–988. [Google Scholar] [CrossRef]
- Higashiguchi, M.; Nakaya, N.; Ohmori, K.; Shimazu, T.; Sone, T.; Hozawa, A.; Kuriyama, S.; Tsuji, I. Malnutrition and the risk of long-term care insurance certification or mortality. A cohort study of the Tsurugaya project. Nihon Koshu Eisei Zasshi (Jpn. J. Public Health) 2008, 55, 433–439. [Google Scholar] [CrossRef]
- Kaiser, M.; Bandinelli, S.; Lunenfeld, B. Frailty and the role of nutrition in older people. A review of the current literature. Acta Biomed. 2010, 81 (Suppl. 1), 37–45. [Google Scholar]
- Beaudart, C.; Sanchez-Rodriguez, D.; Locquet, M.; Reginster, J.-Y.; Lengelé, L.; Bruyère, O. Malnutrition as a Strong Predictor of the Onset of Sarcopenia. Nutrients 2019, 11, 2883. [Google Scholar] [CrossRef]
- Taniguchi, Y.; Watanabe, Y.; Osuka, Y.; Kitamura, A.; Seino, S.; Kim, H.; Kawai, H.; Sakurai, R.; Inagaki, H.; Awata, S.; et al. Characteristics for gait parameters of community-dwelling elderly Japanese with lower cognitive function. PLoS ONE 2019, 14, e0212646. [Google Scholar] [CrossRef]
- Rubenstein, L.Z.; Harker, J.O.; Salva, A.; Guigoz, Y.; Vellas, B. Screening for undernutrition in geriatric practice: Developing the short-form mini-nutritional assessment (MNA-SF). J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M366–M372. [Google Scholar] [CrossRef]
- Montejano Lozoya, R.; Martinez-Alzamora, N.; Clemente Marin, G.; Guirao-Goris, S.J.A.; Ferrer-Diego, R.M. Predictive ability of the Mini Nutritional Assessment Short Form (MNA-SF) in a free-living elderly population: A cross-sectional study. PeerJ 2017, 5, e3345. [Google Scholar] [CrossRef]
- Nokubi, T.; Yasui, S.; Yoshimuta, Y.; Kida, M.; Kusunoki, C.; Ono, T.; Maeda, Y.; Nokubi, F.; Yokota, K.; Yamamoto, T. Fully automatic measuring system for assessing masticatory performance using beta-carotene-containing gummy jelly. J. Oral Rehabil. 2013, 40, 99–105. [Google Scholar] [CrossRef]
- Ito, K.; Yoshihara, A.; Takano, N.; Ishigami, K.; Seida, Y.; Inoue, M.; Kitahara, M.; Miyazaki, H. A Comparison of Methods for the Measurement of Oral Diadochokinesis. Ronen Shika Igaku 2009, 24, 48–54. [Google Scholar] [CrossRef]
- Tsuga, K.; Yoshikawa, M.; Oue, H.; Okazaki, Y.; Tsuchioka, H.; Maruyama, M.; Yoshida, M.; Akagawa, Y. Maximal voluntary tongue pressure is decreased in Japanese frail elderly persons. Gerodontology 2012, 29, e1078–e1085. [Google Scholar] [CrossRef] [PubMed]
- The Ministry of Health, Labour and Welfare. The Manuals of the Evaluation for Ability to Perform Daily Activities on Preventive Care. 2009. Available online: https://www.mhlw.go.jp/topics/2007/03/dl/tp0313-1a-11.pdf (accessed on 20 November 2020).
- Wilson, M.M.; Thomas, D.R.; Rubenstein, L.Z.; Chibnall, J.T.; Anderson, S.; Baxi, A.; Diebold, M.R.; Morley, J.E. Appetite assessment: Simple appetite questionnaire predicts weight loss in community-dwelling adults and nursing home residents. Am. J. Clin. Nutr. 2005, 82, 1074–1081. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, E.; Fujiwara, Y.; Fukaya, T.; Nishi, M.; Saito, M.; Shinkai, S. Social support availability and psychological well-being among the socially isolated elderly. Differences by living arrangement and gender. Nihon Koshu Eisei Zasshi 2011, 58, 446–456. [Google Scholar] [PubMed]
- Iwasa, H.; Masui, Y.; Inagaki, H.; Yoshida, Y.; Shimada, H.; Otsuka, R.; Kikuchi, K.; Nonaka, K.; Yoshida, H.; Yoshida, H.; et al. Assessing competence at a higher level among older adults: Development of the Japan Science and Technology Agency Index of Competence (JST-IC). Aging Clin. Exp. Res. 2018, 30, 383–393. [Google Scholar] [CrossRef]
- Schreiner, A.S.; Hayakawa, H.; Morimoto, T.; Kakuma, T. Screening for late life depression: Cut-off scores for the Geriatric Depression Scale and the Cornell Scale for Depression in Dementia among Japanese subjects. Int. J. Geriatr. Psychiatry 2003, 18, 498–505. [Google Scholar] [CrossRef] [PubMed]
- Masnoon, N.; Shakib, S.; Kalisch-Ellett, L.; Caughey, G.E. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017, 17, 230. [Google Scholar] [CrossRef] [PubMed]
- Chavarro-Carvajal, D.; Reyes-Ortiz, C.; Samper-Ternent, R.; Arciniegas, A.J.; Gutierrez, C.C. Nutritional assessment and factors associated to malnutrition in older adults: A cross-sectional study in Bogota, Colombia. J. Aging Health 2015, 27, 304–319. [Google Scholar] [CrossRef] [PubMed]
- Boulos, C.; Salameh, P.; Barberger-Gateau, P. Factors associated with poor nutritional status among community dwelling Lebanese elderly subjects living in rural areas: Results of the AMEL study. J. Nutr. Health Aging 2014, 18, 487–494. [Google Scholar] [CrossRef]
- Favaro-Moreira, N.C.; Krausch-Hofmann, S.; Matthys, C.; Vereecken, C.; Vanhauwaert, E.; Declercq, A.; Bekkering, G.E.; Duyck, J. Risk Factors for Malnutrition in Older Adults: A Systematic Review of the Literature Based on Longitudinal Data. Adv. Nutr. 2016, 7, 507–522. [Google Scholar] [CrossRef]
- Boulos, C.; Salameh, P.; Barberger-Gateau, P. Social isolation and risk for malnutrition among older people. Geriatr. Gerontol. Int. 2017, 17, 286–294. [Google Scholar] [CrossRef] [PubMed]
- Hernan, M.A.; Hernandez-Diaz, S.; Robins, J.M. A structural approach to selection bias. Epidemiology 2004, 15, 615–625. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, Y.; Hirano, H.; Arai, H.; Morishita, S.; Ohara, Y.; Edahiro, A.; Murakami, M.; Shimada, H.; Kikutani, T.; Suzuki, T. Relationship Between Frailty and Oral Function in Community-Dwelling Elderly Adults. J. Am. Geriatr. Soc. 2017, 65, 66–76. [Google Scholar] [CrossRef] [PubMed]
- Savoca, M.R.; Arcury, T.A.; Leng, X.; Chen, H.; Bell, R.A.; Anderson, A.M.; Kohrman, T.; Gilbert, G.H.; Quandt, S.A. Association between dietary quality of rural older adults and self-reported food avoidance and food modification due to oral health problems. J. Am. Geriatr. Soc. 2010, 58, 1225–1232. [Google Scholar] [CrossRef] [PubMed]
- Yoshihara, A.; Watanabe, R.; Nishimuta, M.; Hanada, N.; Miyazaki, H. The relationship between dietary intake and the number of teeth in elderly Japanese subjects. Gerodontology 2005, 22, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, M.; Taylor, G.W.; Manz, M.C.; Yoshihara, A.; Sato, M.; Muramatsu, K.; Watanabe, R.; Miyazaki, H. Oral health status: Relationship to nutrient and food intake among 80-year-old Japanese adults. Community Dent. Oral Epidemiol. 2014, 42, 441–450. [Google Scholar] [CrossRef]
- Iwasaki, M.; Yoshihara, A.; Ito, K.; Sato, M.; Minagawa, K.; Muramatsu, K.; Watanabe, R.; Manz, M.C.; Ansai, T.; Miyazaki, H. Hyposalivation and dietary nutrient intake among community-based older Japanese. Geriatr. Gerontol. Int. 2016, 16, 500–507. [Google Scholar] [CrossRef]
- Bassim, C.; Mayhew, A.J.; Ma, J.; Kanters, D.; Verschoor, C.P.; Griffith, L.E.; Raina, P. Oral Health, Diet, and Frailty at Baseline of the Canadian Longitudinal Study on Aging. J. Am. Geriatr. Soc. 2020, 68, 959–966. [Google Scholar] [CrossRef]
- Iwasaki, M.; Kimura, Y.; Yoshihara, A.; Ogawa, H.; Yamaga, T.; Takiguchi, T.; Wada, T.; Sakamoto, R.; Ishimoto, Y.; Fukutomi, E.; et al. Association between dental status and food diversity among older Japanese. Community Dent. Health 2015, 32, 104–110. [Google Scholar]
- Chen, C.C.; Schilling, L.S.; Lyder, C.H. A concept analysis of malnutrition in the elderly. J. Adv. Nurs. 2001, 36, 131–142. [Google Scholar] [CrossRef]
- Oliveira, M.R.; Fogaça, K.C.; Leandro-Merhi, V.A. Nutritional status and functional capacity of hospitalized elderly. Nutr. J. 2009, 8, 54. [Google Scholar] [CrossRef] [PubMed]
- Izawa, S.; Enoki, H.; Hasegawa, J.; Hirose, T.; Kuzuya, M. Factors associated with deterioration of mini nutritional assessment-short form status of nursing home residents during a 2-year period. J. Nutr. Health Aging 2014, 18, 372–377. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.C.; Tsai, A.C. Mini-Nutritional Assessment predicts functional decline of elderly Taiwanese: Result of a population-representative sample. Br. J. Nutr. 2012, 107, 1707–1713. [Google Scholar] [CrossRef] [PubMed]
| Component | Prevalence, n (%) |
|---|---|
| 1. Few remaining teeth: Number of teeth < 20 | 150 (32.2%) |
| 2. Low masticatory performance: Increased surface area of comminuted gummy jelly; men, <1178 mm2; women, <1743 mm2) | 78 (16.7%) |
| 3. Low articulatory oral motor skill: Oral-DDK “ta”; men < 5.2 times/s; women, 5.4 times/s | 69 (14.8%) |
| 4. Low TP: men, <27.4 kPa; women, <26.5 kPa | 81 (17.4%) |
| 5. Difficulties chewing tough foods: An answer of “yes” to the question “Do you have any difficulties chewing tough foods compared to six months ago?” | 70 (15.0%) |
| 6. Difficulties in swallowing tea or soup: An answer of “yes” to the question “Have you choked on your tea or soup recently?” | 108 (23.2%) |
| Total | Oral Frailty | |||
|---|---|---|---|---|
| (-) | (+) | |||
| n = 466 | n = 399 | n = 67 | p-Value | |
| n of teeth, median (IQR) | 24 (16–27) | 25 (20–27) | 11 (6–18) | <0.01 |
| Masticatory performance (mm2), median (IQR) | 4396 (2570–5656) | 4643 (3251–5834) | 1343 (499–3374) | <0.01 |
| Oral-DDK ‘‘ta’’ (times/s), median (IQR) | 6.1 (0.8) | 6.1 (0.7) | 5.7 (1.1) | <0.01 |
| TP (kPa), median (IQR) | 33.7 (8.2) | 34.3 (7.8) | 30.4 (9.7) | <0.01 |
| Difficulties eating tough foods, n (%) | 70 (15.0%) | 33 (8.3%) | 37 (55.2%) | <0.01 |
| Difficulties in swallowing tea or soup, n (%) | 108 (23.2%) | 74 (18.5%) | 34 (50.7%) | <0.01 |
| Denture use, n (%) | 217 (46.6%) | 163 (40.9%) | 54 (80.6%) | <0.01 |
| Age, mean (SD) | 76.4 (4.1) | 76.3 (4.1) | 76.8 (4.3) | 0.39 |
| Sex, n (%) | 0.35 | |||
| Women | 275 (59.0%) | 232 (58.1%) | 43 (64.2%) | |
| Men | 191 (41.0%) | 167 (41.9%) | 24 (35.8%) | |
| Body weight (kg), mean (SD) | 58.2 (8.9) | 58.3 (9.1) | 57.6 (8.3) | 0.55 |
| Height (cm), mean (SD) | 156.2 (8.6) | 156.4 (8.7) | 154.9 (7.8) | 0.21 |
| BMI (kg/m2), mean (SD) | 23.8 (2.6) | 23.8 (2.6) | 24.0 (2.7) | 0.59 |
| Educational status (years of schooling), median (IQR) | 12 (12–16) | 12 (12–16) | 12 (12–14) | 0.22 |
| Annual income < 3 million JPY, n (%) | 271 (58.2%) | 225 (56.4%) | 46 (68.7%) | 0.06 |
| Current smoker, n (%) | 35 (7.5%) | 26 (6.5%) | 9 (13.4%) | 0.05 |
| Daily drinker, n (%) | 62 (13.3%) | 53 (13.3%) | 9 (13.4%) | 0.97 |
| Low physical activity, n (%) | 310 (66.5%) | 258 (64.7%) | 52 (77.6%) | 0.04 |
| Poor appetite, n (%) | 165 (35.4%) | 131 (32.8%) | 34 (50.7%) | 0.01 |
| Social isolation, n (%) | 178 (38.2%) | 149 (37.3%) | 29 (43.3%) | 0.35 |
| Living alone, n (%) | 164 (35.2%) | 134 (33.6%) | 30 (44.8%) | 0.08 |
| JST-IC, median (IQR) | 11 (9–13) | 12 (10–13) | 10 (9–12) | <0.01 |
| Number of comorbidities, median (IQR) | 2 (1–3) | 2 (1–2) | 2 (1–3) | 0.10 |
| Polypharmacy, n (%) | 119 (25.5%) | 104 (26.1%) | 15 (22.4%) | 0.52 |
| Depressive symptoms, n (%) | 60 (12.9%) | 40 (10.0%) | 20 (29.9%) | <0.01 |
| Cognitive impairment, n (%) | 19 (4.1%) | 18 (4.5%) | 1 (1.5%) | 0.25 |
| Variables b | Unadjusted ORs | 95% CIs | p-Value |
|---|---|---|---|
| MNA®-SF (per one increase) | 0.40 | (0.28–0.57) | <0.01 |
| Age (per one increase) | 1.02 | (0.95–1.09) | 0.58 |
| Men (vs. women) | 0.86 | (0.48–1.54) | 0.61 |
| Years of schooling (per one increase) | 0.94 | (0.85–1.05) | 0.29 |
| Annual income < 3 million JPY | 1.07 | (0.60–1.91) | 0.82 |
| Current smoker | 0.80 | (0.23–2.79) | 0.73 |
| Daily drinker | 1.40 | (0.65–2.98) | 0.39 |
| Low physical activity level | 1.51 | (0.81–2.80) | 0.20 |
| Poor appetite | 2.28 | (1.29–4.04) | <0.01 |
| Social isolation | 1.33 | (0.75–2.37) | 0.33 |
| Living alone | 0.92 | (0.51–1.69) | 0.80 |
| JST-IC score (per one increase) | 0.85 | (0.77–0.94) | <0.01 |
| Number of comorbidities (per one increase) | 1.10 | (0.87–1.37) | 0.42 |
| Polypharmacy | 1.16 | (0.61–2.23) | 0.65 |
| Depressive symptoms | 2.38 | (1.19–4.76) | 0.01 |
| Cognitive impairment | 2.41 | (0.82–7.05) | 0.11 |
| Outcome = Having MNA®-SF Score of < 12 at Two-Year Follow-Up Assessment | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 (Oral Frailty Only) | Model 2 (Model 1 + Other Variables that Yielded p-Values < 0.05 in the Crude Model) | Model 3 (Fully Adjusted Model) | |||||||
| Variables b | ORs | 95% CI | p-Value | ORs | 95% CI | p-Value | ORs | 95% CI | p-Value |
| Oral frailty | 2.57 | (1.32–4.99) | 0.01 | 2.13 | (1.05–4.33) | 0.04 | 2.24 | (1.08–4.63) | 0.03 |
| MNA®-SF (per one increase) | 0.42 | (0.28–0.63) | <0.01 | 0.43 | (0.28–0.65) | <0.01 | |||
| Age (per one increase) | 1.01 | (0.94–1.08) | 0.86 | ||||||
| Men (vs. women) | 0.71 | (0.36–1.39) | 0.32 | ||||||
| Years of schooling (per one increase) | 1.03 | (0.91–1.16) | 0.64 | ||||||
| Annual income < 3 million JPY | 1.00 | (0.47–2.14) | 1.00 | ||||||
| Current smoker | 0.50 | (0.16–1.57) | 0.23 | ||||||
| Daily drinker | 1.47 | (0.65–3.35) | 0.36 | ||||||
| Low physical activity level | 1.26 | (0.63–2.50) | 0.52 | ||||||
| Poor appetite | 1.51 | (0.82–2.79) | 0.18 | 1.56 | (0.85–2.85) | 0.15 | |||
| Social isolation | 1.30 | (0.68–2.47) | 0.43 | ||||||
| Living alone | 0.61 | (0.27–1.39) | 0.24 | ||||||
| JST-IC score (per one increase) | 0.88 | (0.79–0.98) | 0.02 | 0.88 | (0.78–0.99) | 0.04 | |||
| Number of comorbidities (per one increase) | 1.05 | (0.81–1.36) | 0.70 | ||||||
| Polypharmacy | 1.07 | (0.50–2.26) | 0.87 | ||||||
| Depressive symptoms | 0.96 | (0.42–2.19) | 0.91 | 1.18 | (0.49–2.86) | 0.71 | |||
| Cognitive impairment | 2.03 | (0.58–7.19) | 0.27 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iwasaki, M.; Motokawa, K.; Watanabe, Y.; Shirobe, M.; Inagaki, H.; Edahiro, A.; Ohara, Y.; Hirano, H.; Shinkai, S.; Awata, S. A Two-Year Longitudinal Study of the Association between Oral Frailty and Deteriorating Nutritional Status among Community-Dwelling Older Adults. Int. J. Environ. Res. Public Health 2021, 18, 213. https://doi.org/10.3390/ijerph18010213
Iwasaki M, Motokawa K, Watanabe Y, Shirobe M, Inagaki H, Edahiro A, Ohara Y, Hirano H, Shinkai S, Awata S. A Two-Year Longitudinal Study of the Association between Oral Frailty and Deteriorating Nutritional Status among Community-Dwelling Older Adults. International Journal of Environmental Research and Public Health. 2021; 18(1):213. https://doi.org/10.3390/ijerph18010213
Chicago/Turabian StyleIwasaki, Masanori, Keiko Motokawa, Yutaka Watanabe, Maki Shirobe, Hiroki Inagaki, Ayako Edahiro, Yuki Ohara, Hirohiko Hirano, Shoji Shinkai, and Shuichi Awata. 2021. "A Two-Year Longitudinal Study of the Association between Oral Frailty and Deteriorating Nutritional Status among Community-Dwelling Older Adults" International Journal of Environmental Research and Public Health 18, no. 1: 213. https://doi.org/10.3390/ijerph18010213
APA StyleIwasaki, M., Motokawa, K., Watanabe, Y., Shirobe, M., Inagaki, H., Edahiro, A., Ohara, Y., Hirano, H., Shinkai, S., & Awata, S. (2021). A Two-Year Longitudinal Study of the Association between Oral Frailty and Deteriorating Nutritional Status among Community-Dwelling Older Adults. International Journal of Environmental Research and Public Health, 18(1), 213. https://doi.org/10.3390/ijerph18010213





