Socioeconomic Inequality in the Use of Long-Term Care among European Older Adults: An Empirical Approach Using the SHARE Survey
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gaugler, J.; James, B.; Johnson, T.; Scholz, K.; Weuve, J. 2016 Alzheimer’s Disease Facts and Figures. Alzheimer’s Dement. 2016, 12, 459–509. [Google Scholar] [CrossRef]
- Andreas, S.; Schulz, H.; Volkert, J.; Dehoust, M.; Sehner, S.; Suling, A.; Ausín, B.; Canuto, A.; Crawford, M.; Da Ronch, C.; et al. Prevalence of Mental Disorders in Elderly People: The European MentDis_ICF65+ Study. Br. J. Psychiatry 2017, 210, 125–131. [Google Scholar] [CrossRef] [PubMed]
- European Institute for Gender Equality (EIGE). Gender Equality and Long-Term Care at Home. 2020. Available online: https://eige.europa.eu/publications/gender-equality-and-long-term-care-home (accessed on 29 September 2020).
- Alzheimer’s Disease International. World Alzheimer Report 2019: Attitudes to Dementia; Alzheimer’s Disease International: London, UK, 2019; Available online: https://www.alzint.org/resource/world-alzheimer-report-2019/ (accessed on 29 September 2020).
- European Institute for Gender Equality (EIGE). Gender Equality Index 2019. Work-Life Balance. 2019. Available online: https://eige.europa.eu/publications/gender-equality-index-2019-work-life-balance (accessed on 1 October 2020).
- Schwarzkopf, L.; Menn, P.; Leidl, R.; Wunder, S.; Mehlig, H.; Marx, P.; Graessel, E.; Holle, R. Excess Costs of Dementia Disorders and the Role of Age and Gender—an Analysis of German Health and Long-Term Care Insurance Claims Data. BMC Health Serv. Res. 2012, 12, 1–12. [Google Scholar] [CrossRef]
- World Health Organization. Global Action Plan on the Public Health Response to Dementia 2017–2025; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Spasova, S.; Baeten, R.; Coster, S.; Ghailani, D.; Peña-casas, R.; Vanhercke, B. Challenges in Long-Term Care in Europe: A Study of National Policies; Technical Report; European Commission: Brussels, Belgium, 2018. [Google Scholar]
- Zamora-Kapoor, A.; Coller, X. The Effects of the Crisis: Why Southern Europe? Am. Behav. Sci. 2014, 58, 1511–1516. [Google Scholar] [CrossRef] [PubMed]
- Larsson, K.; Silverstein, M. The Effects of Marital and Parental Status on Informal Support and Service Utilization: A Study of Older Swedes Living Alone. J. Aging Stud. 2004, 18, 231–244. [Google Scholar] [CrossRef]
- Bonsang, E. Does Informal Care from Children to Their Elderly Parents Substitute for Formal Care in Europe? J. Health Econ. 2009, 28, 143–154. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, A.E. Analysing the Importance of Older People’s Resources for the Use of Home Care in a Cash-for-Care Scheme: Evidence from Vienna. Health Soc. Care Community 2017, 25, 514–526. [Google Scholar] [CrossRef] [PubMed]
- Jones, I.R. Social Class, Dementia and the Fourth Age. Sociol. Health Illn. 2017, 39, 303–317. [Google Scholar] [CrossRef] [PubMed]
- Lindgren, E.; Sörenson, J.; Nägga, K.; Wattmo, C. Equity in Dementia Care Focusing on Immigrants in Sweden: A Nationwide Register-Based Study. Eur. J. Public Health 2017, 27, 4556100. [Google Scholar] [CrossRef]
- Korhonen, K.; Einiö, E.; Leinonen, T.; Tarkiainen, L.; Martikainen, P. Time-Varying Effects of Socio-Demographic and Economic Factors on the Use of Institutional Long-Term Care before Dementia-Related Death: A Finnish Register-Based Study. PLoS ONE 2018, 13, e0199551. [Google Scholar] [CrossRef]
- Chuakhamfoo, N.N.; Phanthunane, P.; Chansirikarn, S.; Pannarunothai, S. Health and Long-Term Care of the Elderly with Dementia in Rural Thailand: A Cross-Sectional Survey through Their Caregivers. BMJ Open 2020, 10, e032637. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.; Si, Y.; Li, B. Decomposing Inequality in Long-Term Care Need Among Older Adults with Chronic Diseases in China: A Life Course Perspective. Int. J. Environ. Res. Public Health 2020, 17, 2559. [Google Scholar] [CrossRef] [PubMed]
- Floridi, G.; Carrino, L.; Glaser, K. Socioeconomic Inequalities in Home-Care Use Across Regional Long-Term Care Systems in Europe. J. Gerontol. Ser. B 2020. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, R.; Ilinca, S.; Schmidt, A. Analysing Equity in the Use of Long Term Care in Europe; Research Note 9/2014; European Commission: Brussels, Belgium, 2014. [Google Scholar]
- Ilinca, S.; Rodrigues, R.; Schmidt, A.E. Fairness and Eligibility to Long-Term Care: An Analysis of the Factors Driving Inequality and Inequity in the Use of Home Care for Older Europeans. Int. J. Environ. Res. Public Health 2017, 14, 1224. [Google Scholar] [CrossRef]
- Bähler, C.; Huber, C.A.; Brüngger, B.; Reich, O. Multimorbidity, Health Care Utilization and Costs in an Elderly Community-Dwelling Population: A Claims Data Based Observational Study. BMC Health Serv. Res. 2015, 15, 23. [Google Scholar] [CrossRef]
- Cantarero-Prieto, D.; Pascual-Sáez, M.; Blázquez-Fernández, C. What Is Happening with Quality of Life Among the Oldest People in Southern European Countries? An Empirical Approach Based on the SHARE Data. Soc. Indic. Res. 2017, 140, 1–15. [Google Scholar] [CrossRef]
- Prince, M.; Wimo, A.; Guerchet, M.; Ali, G.; Wu, Y.; Prina, M. World Alzheimer Report 2015. The Global Impact of Dementia: An Analysis of Prevalence, Incidence, Cost and Trends; Alzheimer’s Disease International: London, UK, 2015; Available online: https://doi.org/http://dx.doi.org/10.1007/s00270-010-9954-3 (accessed on 3 October 2020).
- Motel-Klingebiel, A.; Tesch-Roemer, C.; Von Kondratowitz, H.J. Welfare States Do Not Crowd out the Family: Evidence for Mixed Responsibility from Comparative Analyses. Ageing Soc. 2005, 25, 863–882. [Google Scholar] [CrossRef]
- Rodrigues, R.; Schulmann, K.; Schmidt, A.; Kalavrezou, N.; Matsaganis, M. The Indirect Costs of Long-Term Care; Research Note 8/2013; European Centre for Social Welfare Policy and Research: Vienna, Austria, 2013; pp. 1–42. [Google Scholar]
- Zigante, V. Informal Care in Europe. Exploring Formalisation, Availability and Quality; European Commission: Luxembourg, 2018. [Google Scholar]
- Browse by EuroVoc on EUR-Lex Web Site. Available online: https://eur-lex.europa.eu/browse/eurovoc.html?params=72#arrow_72 (accessed on 6 December 2020).
- Maddala, S. Limited-Dependent and Qualitative Variables in Econometrics; Cambridge University Press: Cambridge, UK, 1983. [Google Scholar] [CrossRef]
- Wu, C.-Y.; Hu, H.-Y.; Huang, N.; Fang, Y.-T.; Chou, Y.-J.; Li, C.-P. Determinants of Long-Term Care Services among the Elderly: A Population-Based Study in Taiwan. PLoS ONE 2014, 9, e89213. [Google Scholar] [CrossRef]
- Zhu, H. Unmet needs in long-term care and their associated factors among the oldest old in China. BMC Geriatr. 2015, 15, 46. [Google Scholar] [CrossRef]
- Garner, R.; Tanuseputro, P.; Manuel, D.G.; Sanmartin, C. Transitions to long-term and residential care among older Canadians. Health Rep. 2018, 29, 13–23. [Google Scholar]
- Steinbeisser, K.; Grill, E.; Holle, R.; Peters, A.; Seidl, H. Determinants for utilization and transitions of long-term care in adults 65+ in Germany: Results from the longitudinal KORA-Age study. BMC Geriatr. 2018, 18, 172. [Google Scholar] [CrossRef] [PubMed]
- Wagstaff, A. The Bounds of the Concentration Index When the Variable of Interest Is Binary, with an Application to Immunization Inequality. Health Econ. 2005, 14, 429–432. [Google Scholar] [CrossRef] [PubMed]
- Wagstaff, A.; Paci, P.; van Doorslaer, E. On the Measurement of Inequalities in Health. Soc. Sci. Med. 1991, 33, 545–557. [Google Scholar] [CrossRef]
- Wagstaff, A.; van Doorslaer, E. Measuring and Testing for Inequity in the Delivery of Health Care. J. Hum. Resour. 2000, 35, 716. [Google Scholar] [CrossRef]
- Rodrigues, R.; Ilinca, S.; Schmidt, A. Income-rich and wealth-poor? The impact of measures of socio-economic status in the analysis of the distribution of long-term care use among older people. Health Econ. 2018, 27, 637–646. [Google Scholar] [CrossRef]
- Erreygers, G. Correcting the Concentration Index. J. Health Econ. 2009, 28, 504–515. [Google Scholar] [CrossRef]
- Fu, Y.; Guo, F.; Bai, X.; Wing, E. Factors associated with older people’s long-term care needs: A case study adopting the expanded version of the Anderson Model in China. BMC Geriatr. 2017, 17. [Google Scholar] [CrossRef]
- Armijos-Bravo, G. Socioeconomic inequity in long-term care use in Europe. Cuadernos de Economía 2019, 42. [Google Scholar] [CrossRef]
- Tenand, M.; Bakx, P.; van Doorslaer, E. Eligibility or use? Disentangling the sources of horizontal inequity in home care receipt in the Netherlands. Health Econ. 2020, 29, 1161–1179. [Google Scholar] [CrossRef]
- O’Donnell, O.; van Doorslaer, E.; Wagstaff, A.; Lindelow, M. Analyzing Health Equity Using Household Survey Data: A Guide to Techniques and Their Implementation; The World Bank: Washington, DC, USA, 2008. [Google Scholar]
- Pulok, M.H.; van Gool, K.; Hajizadeh, M.; Allin, S.; Hall, J. Measuring Horizontal Inequity in Healthcare Utilisation: A Review of Methodological Developments and Debates. Eur. J. Health Econ. 2020, 21, 171–180. [Google Scholar] [CrossRef]
- Cantarero-Prieto, D.; Pascual-Sáez, M.; Rodriguez-Sánchez, B. Differences in the Provision of Formal and Informal Care Services after the Implementation of the Dependency Act: The Spanish Case; Instituto de Estudios Fiscales: Madrid, Spain, 2019. [Google Scholar]
- Broese van Groenou, M.; Glaser, K.; Tomassini, C.; Jacobs, T. Socio-Economic Status Differences in Older People’s Use of Informal and Formal Help: A Comparison of Four European Countries. Ageing Soc. 2006, 26, 745–766. [Google Scholar] [CrossRef]
- Albertini, M.; Pavolini, E. Unequal Inequalities: The Stratification of the Use of Formal Care among Older Europeans. J. Gerontol. B Psychol. Sci. Soc. Sci. 2017, 72, 510–521. [Google Scholar] [CrossRef]
- Kjær, A.A.; Siren, A. Formal and Informal Care: Trajectories of Home Care Use among Danish Older Adults. Ageing Soc. 2019, 1–24. [Google Scholar] [CrossRef]
- García-Gómez, P.; Hernández-Quevedo, C.; Jiménez-Rubio, D.; Oliva-Moreno, J. Inequity in Long-Term Care Use and Unmet Need: Two Sides of the Same Coin. J. Health Econ. 2015, 39, 147–158. [Google Scholar] [CrossRef]
- Schmidt, A.E. Older Persons’ Views on Using Cash-for-Care Allowances at the Crossroads of Gender, Socio-Economic Status and Care Needs in Vienna. Soc. Policy Adm. 2018, 52, 710–730. [Google Scholar] [CrossRef]
- Bergmann, M.; Scherpenzeel, A.; Börsch-Supan, A. SHARE Wave 7 Methodology: Panel Innovations and Life Histories; Munich Center for the Economics of Aging (MEA): Munich, Germany, 2019. [Google Scholar]
- Börsch-Supan, A.; Brandt, M.; Hunkler, C.; Kneip, T.; Korbmacher, J.; Malter, F.; Schaan, B.; Stuck, S.; Zuber, S. Data Resource Profile: The Survey of Health, Ageing and Retirement in Europe (Share). Int. J. Epidemiol. 2013, 42, 992–1001. [Google Scholar] [CrossRef] [PubMed]
| Variable | Definition | Coding | Mean | SD |
|---|---|---|---|---|
| Long-Term Care | ||||
| InformalCare | Non-professional help inside or outside the household | 1: if respondent has received non-professional help inside or outside the household; 0: otherwise | 0.2832 | 0.4506 |
| FormalCare | Professional help at home or institutionalization | 1: if respondent has been institutionalized or has received professional help at home; 0: otherwise | 0.0913 | 0.2881 |
| Personal Characteristics | ||||
| Female | Gender of respondent | 1: if respondent’s gender is female; 0: otherwise (male) | 0.5605 | 0.4963 |
| Age | Age of respondent | Age in years | 69.6823 | 9.7148 |
| Single | Marital status | 1: never married, divorced, or widowed; 0: married, living with spouse or not, or registered partnership | 0.2933 | 0.4553 |
| Education | Education level | 1: primary education; 2: secondary education; 3: tertiary education | 1.8250 | 0.7916 |
| NChild | Number of descendants that are still alive | Number of children that are still alive | 2.1526 | 1.2767 |
| Household Characteristics | ||||
| ChHH | Descendants’ living place | 1: If at least one child lives in the same household or the same building as respondent | 0.0041 | 0.0642 |
| HHsize | Household size | Number of people living in the same household as the respondent | 2.0274 | 0.8721 |
| Urban | Respondents’ living area | 1: if respondent lives in an urban area; 0: otherwise | 0.6771 | 0.4676 |
| Health Status | ||||
| SAGHS | Self-assessed good health status | 1: if respondent’s self-assessed good health status is excellent, very good, good, or fair; 0: otherwise (poor) | 0.6321 | 0.4822 |
| ADL | Number of limitations in activities of daily living (ADLs) | Number of limitations in ADLs | 0.2792 | 0.9573 |
| NCD | Number of chronic diseases | Number of chronic diseases | 1.9179 | 1.6332 |
| Formal Care | Informal Care | |||
|---|---|---|---|---|
| Variable | Coef. | Odds Ratio | Coef. | Odds Ratio |
| Personal Characteristics | ||||
| Female | 0.3556 *** | 1.4270*** | 0.1415 *** | 1.1520 *** |
| 0.0478 | 0.0682 | 0.0486 | 0.0560 | |
| Age 66 to 80 years | 0.5817 *** | 1.7890 *** | 0.0423 | 1.0432 |
| 0.0601 | 0.1075 | 0.0628 | 0.0655 | |
| Age 80 plus years | 1.7870 *** | 5.9716 *** | 0.7107 *** | 2.0354 *** |
| 0.0656 | 0.3917 | 0.0761 | 0.1548 | |
| Single | 0.6815 *** | 1.9768 *** | 0.5967 *** | 1.8161 *** |
| 0.0605 | 0.1196 | 0.0666 | 0.1209 | |
| Secondary Education | −0.0919 * | 0.9122 * | 0.0244 | 1.0247 |
| 0.0531 | 0.0484 | 0.0566 | 0.0580 | |
| Tertiary Education | 0.1363 ** | 1.1460 ** | −0.0372 | 0.9635 |
| 0.0598 | 0.0686 | 0.0650 | 0.0627 | |
| NChild | 0.0028 *** | 1.0028 *** | 0.0836 *** | 1.0872 *** |
| 0.0004 | 0.0004 | 0.0183 | 0.0199 | |
| Household Characteristics | ||||
| ChHH | −0.2824 | 0.7540 | −0.3232 | 0.7238 |
| 0.3944 | 0.2974 | 0.2542 | 0.1840 | |
| HHsize | −0.1669 *** | 0.8463 *** | −0.1995 *** | 0.8192 *** |
| 0.0418 | 0.0354 | 0.0464 | 0.0380 | |
| Urban | 0.2344 *** | 1.2642 *** | −0.2925 *** | 0.7464 *** |
| 0.0471 | 0.0596 | 0.0504 | 0.0376 | |
| Health Status | ||||
| SAGHS | −0.7566 *** | 0.4693 *** | −0.5225 *** | 0.5931 *** |
| 0.0500 | 0.0235 | 0.0528 | 0.0313 | |
| ADL | 0.4994 *** | 1.6477 *** | 0.4329 *** | 1.5417 *** |
| 0.0184 | 0.0303 | 0.0328 | 0.0506 | |
| NCD | 0.1347 *** | 1.1441 *** | 0.1663 *** | 1.1810 *** |
| 0.0134 | 0.0154 | 0.0160 | 0.0189 | |
| Country | ||||
| Southern Europe | −1.2364 *** | 0.2904 *** | −0.5970 *** | 0.5505 *** |
| 0.0623 | 0.0181 | 0.0598 | 0.0329 | |
| Eastern Europe | −0.6313 *** | 0.5319 *** | 0.2249 *** | 1.2521 *** |
| 0.0597 | 0.0318 | 0.0637 | 0.0797 | |
| Northern Europe | −0.8903 *** | 0.4105 *** | 0.7492 *** | 2.1154 *** |
| 0.0797 | 0.0327 | 0.0870 | 0.1841 | |
| Constant | −2.8983 *** | 0.0551 *** | −1.1377 *** | 0.3206 *** |
| 0.1330 | 0.0073 | 0.1479 | 0.0474 | |
| Log pseudolikelihood | −8031.1996 | −5767.0237 | ||
| Number of observations | 35,718 | 11,629 | ||
| Ranking Variable | AT | DE | SE | ES | IT | FR | DK | GR | BE | CZ |
|---|---|---|---|---|---|---|---|---|---|---|
| Informal Care | ||||||||||
| HHTotal Income | −0.1875 *** | −0.2038 *** | −0.1634 *** | −0.1254 *** | −0.0936 *** | −0.2159 *** | −0.1672 *** | −0.1250 *** | −0.2164 *** | −0.1689 *** |
| (0.0510) | (0.0361) | (0.0309) | (0.0262) | (0.0221) | (0.0309) | (0.0310) | (0.0205) | (0.0262) | (0.0375) | |
| HH wealth | −0.1499 *** | −0.1674 *** | −0.0967 *** | −0.1332 *** | −0.1160 *** | −0.1331 *** | −0.1475 *** | −0.2045 *** | −0.2367 *** | −0.1843 *** |
| (0.0526) | (0.0364) | (0.0304) | (0.0261) | (0.0234) | (0.0313) | (0.0308) | (0.0214) | (0.0256) | (0.0371) | |
| Formal Care | ||||||||||
| HH Total Income | 0.0176 * | 0.0222 *** | 0.0269 *** | −0.0026 | 0.0154 ** | 0.0003 | 0.0070 | −0.0361 *** | 0.0275 ** | −0.0103 |
| (0.0089) | (0.0085) | (0.0101) | (0.0089) | (0.0072) | (0.0112) | (0.0089) | (0.0087) | (0.0116) | (0.0065) | |
| HH wealth | 0.0209 * | 0.0375 *** | 0.0506 *** | 0.0427 *** | 0.0243 *** | 0.0111 | 0.0161 | −0.0306 *** | 0.0550 *** | −0.0175 *** |
| (0.0086) | (0.0082) | (0.0097) | (0.0086) | (0.0070) | (0.0107) | (0.0087) | (0.0074) | (0.0113) | (0.0057) | |
| Ranking Variable | AT | DE | SE | ES | IT | FR | DK | GR | BE | CZ |
|---|---|---|---|---|---|---|---|---|---|---|
| Informal Care | ||||||||||
| HH Total Income | 0.0880 *** | 0.0775 *** | 0.1221 *** | 0.0944 *** | 0.0487 *** | 0.0914 *** | 0.1001 *** | 0.0487 *** | 0.0901 *** | 0.0761 *** |
| (0.0128) | (0.0084) | (0.0074) | (0.0087) | (0.0068) | (0.0076) | (0.0069) | (0.0059) | (0.0063) | (0.0091) | |
| HH wealth | 0.0994 *** | 0.0681 *** | 0.1018 *** | 0.0732 *** | 0.0539 *** | 0.0789 *** | 0.0797 *** | 0.0585 *** | 0.0727 *** | 0.1024 *** |
| (0.0135) | (0.0091) | (0.0080) | (0.0083) | (0.0068) | (0.0074) | (0.0071) | (0.0058) | (0.0063) | (0.0093) | |
| Formal Care | ||||||||||
| HH Total Income | 0.1277 *** | 0.0923 *** | 0.1363 *** | 0.1051 *** | 0.0616 *** | 0.1081 *** | 0.1463 *** | 0.0660 *** | 0.1167 *** | 0.1044 *** |
| (0.0140) | (0.0090) | (0.0073) | (0.0105) | (0.0082) | (0.0081) | (0.0066) | (0.0075) | (0.0072) | (0.0102) | |
| HH wealth | 0.1360 *** | 0.0899 *** | 0.1017 *** | 0.0918 *** | 0.0721 *** | 0.0935 *** | 0.0982 *** | 0.0972 *** | 0.1034 *** | 0.1150 *** |
| (0.0154) | (0.0093) | (0.0079) | (0.0101) | (0.0083) | (0.0083) | (0.0070) | (0.0073) | (0.0072) | (0.0105) | |
| AT | DE | SE | ES | IT | FR | DK | GR | BE | CZ | |
|---|---|---|---|---|---|---|---|---|---|---|
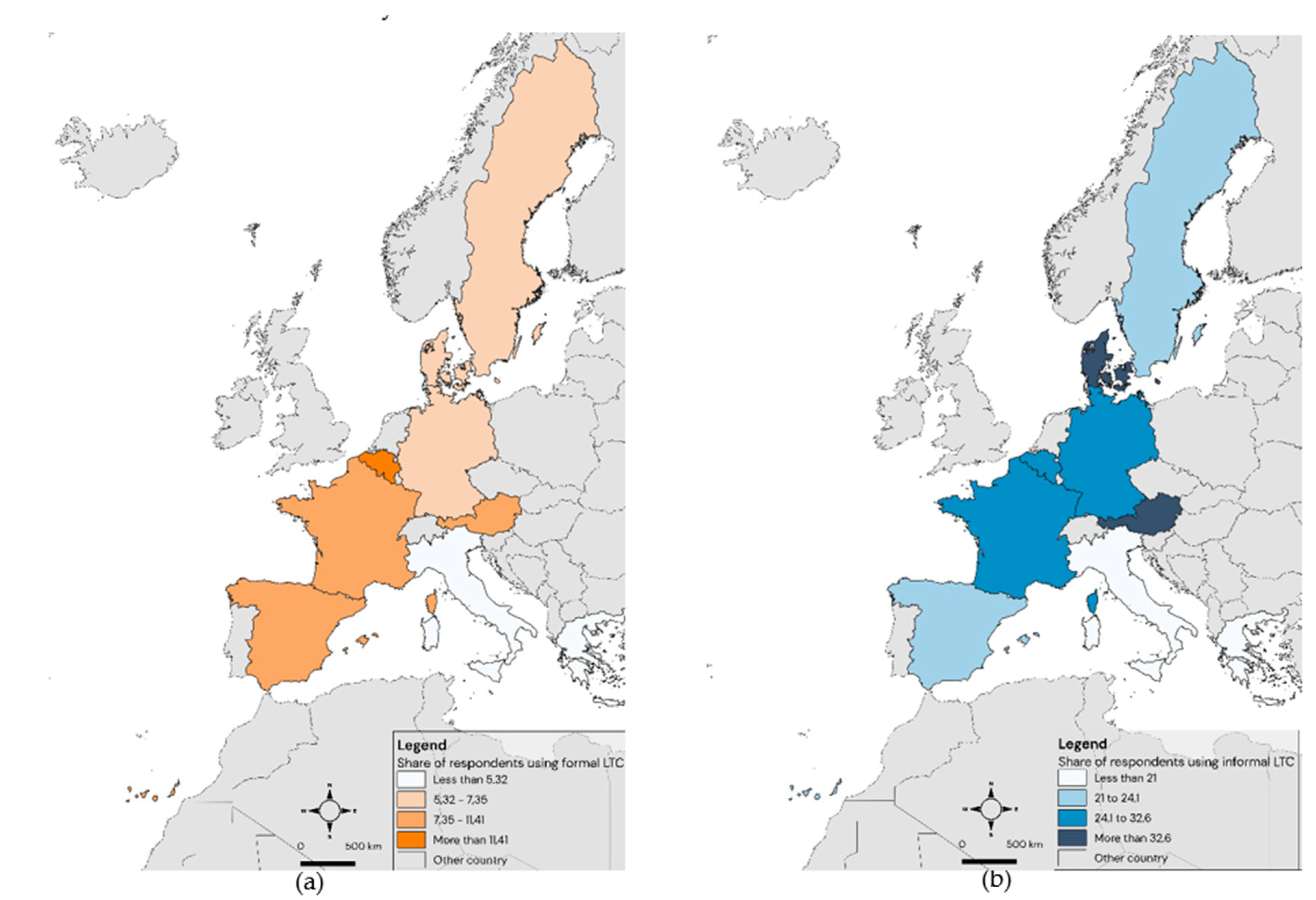
| Informal care (%) | 41.0148 | 32.6139 | 24.1088 | 22.9379 | 20.2936 | 29.6752 | 38.0952 | 20.9694 | 27.5995 | 45.1754 |
| (49.2381) | (46.9080) | (42.7945) | (42.0599) | (40.2313) | (45.7027) | (48.5811) | (40.7198) | (44.7158) | (49.7940) | |
| Formal care (%) | 10.7383 | 7.3471 | 7.3350 | 9.0217 | 5.3239 | 11.4109 | 6.7636 | 4.8249 | 18.9184 | 7.1810 |
| (30.9649) | (26.0942) | (26.0753) | ((28.6524) | (22.4534) | (31.7992) | (25.1160) | (21.4326) | (39.1696) | (25.8204) | |
| Female (%) | 59.0210 | 52.9102 | 53.8172 | 55.6886 | 54.7803 | 57.9745 | 54.1356 | 57.3544 | 55.3472 | 59.9237 |
| (49.1872) | (49.9218) | (49.8619) | (49.6807) | (49.7765) | (49.3675) | (49.8364) | (49.4643) | (49.7184) | (49.0112) | |
| Age (in years) | 70.7449 | 68.1372 | 72.1986 | 71.5682 | 69.1585 | 69.6413 | 67.1915 | 69.6703 | 68.3192 | 70.3550 |
| (9.2835) | (9.3417) | (8.8213) | (10.2876) | (9.6743) | (10.2909) | (9.6754) | (9.3476) | (10.2364) | (8.5431) | |
| Single (%) | 36.3665 | 24.5194 | 28.7465 | 27.6305 | 22.9411 | 34.8696 | 26.1194 | 28.5620 | 32.0008 | 33.1345 |
| (48.1129) | (43.0259) | (45.2651) | (44.7217) | (42.0500) | (47.6630) | (43.9354) | (45.1784) | (46.6527) | (47.0753) | |
| Primary education (%) | 23.3448 | 11.3247 | 33.8674 | 78.5714 | 68.8231 | 38.6598 | 16.6356 | 52.0237 | 36.5135 | 38.0248 |
| (42.3092) | (31.6937) | (47.3333) | (41.0370) | (46.3267) | (48.7044) | (37.2458) | (49.9673) | (48.1518) | (48.5506) | |
| Secondary education (%) | 49.6392 | 56.4656 | 33.2077 | 10.5646 | 23.1398 | 37.0831 | 37.8731 | 29.8124 | 27.6942 | 47.6861 |
| (50.0065) | (49.5867) | (47.1032) | (30.7417) | (42.1773) | (48.3101) | (48.5147) | (45.7510) | (44.7534) | (49.9524) | |
| Tertiary education (%) | 27.0160 | 32.2096 | 32.9249 | 10.8640 | 8.0371 | 24.2571 | 45.4913 | 18.1639 | 35.7923 | 14.2891 |
| (44.4112) | (46.7341) | (47.0014) | (31.1220) | (27.1897) | (42.8703) | (49.8040) | (38.5610) | (47.9439) | (35.0004) | |
| Number of descendants | 2.1064 | 1.9920 | 2.2164 | 2.5501 | 2.0571 | 2.3302 | 2.2384 | 1.8643 | 2.1507 | 2.1155 |
| (1.4066) | (1.2252) | (1.2165) | (1.5972) | (1.2274) | (1.4200) | (1.2377) | (0.9566) | (1.3817) | (0.9270) | |
| Living with descendants (%) | 0.2196 | 0.3687 | 0.1885 | 0.5560 | 0.8170 | 0.2426 | 0.4353 | 0.3620 | 0.4739 | 0.2624 |
| (4.6822) | (6.0618) | (4.3383) | (7.4368) | (9.0026) | (4.9199) | (6.5846) | (6.0064) | (6.8687) | (5.1164) | |
| Household size | 1.8817 | 1.9573 | 1.7908 | 2.2397 | 2.3449 | 1.8924 | 1.8955 | 2.1316 | 1.9825 | 1.9854 |
| (0.8651) | (0.7202) | (0.5652) | (0.9741) | (0.9966) | (0.8111) | (0.6819) | (0.9239) | (0.8694) | (0.9206) | |
| Living in urban areas (%) | 50.7085 | 59.1251 | 62.1395 | 84.6242 | 65.7284 | 51.8461 | 75.4119 | 84.3353 | 67.1958 | 71.1117 |
| (50.0034) | (49.1669) | (48.5121) | (36.0758) | (47.4673) | (49.9737) | (43.0677) | (36.3528) | (46.9550) | (45.3302) | |
| At least good self-assessed health (%) | 61.8136 | 56.9660 | 68.4889 | 55.1112 | 55.7960 | 62.4924 | 73.6629 | 66.8641 | 67.8137 | 67.5573 |
| (48.5920) | (49.5189) | (46.4633) | (49.7434) | (49.6684) | (48.4216) | (44.0530) | (47.0779) | (46.7239) | (46.8216) | |
| Number of ADL limitations | 0.2949 | 0.2499 | 0.1976 | 0.4134 | 0.2826 | 0.2674 | 0.1785 | 0.1612 | 0.3313 | 0.3137 |
| (1.0098) | (0.8489) | (0.7667) | (1.2438) | (1.0316) | (0.9070) | (0.7494) | (0.7394) | (0.9770) | (0.9620) | |
| Number of chronic illnesses | 1.9206 | 2.0716 | 1.6510 | 2.0079 | 1.6410 | 1.8451 | 1.5917 | 1.9197 | 2.0387 | 2.3447 |
| (1.6258) | (1.7347) | (1.4654) | (1.6905) | (1.5338) | (1.5316) | (1.4685) | (1.5968) | (1.6582) | (1.7571) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lera, J.; Pascual-Sáez, M.; Cantarero-Prieto, D. Socioeconomic Inequality in the Use of Long-Term Care among European Older Adults: An Empirical Approach Using the SHARE Survey. Int. J. Environ. Res. Public Health 2021, 18, 20. https://doi.org/10.3390/ijerph18010020
Lera J, Pascual-Sáez M, Cantarero-Prieto D. Socioeconomic Inequality in the Use of Long-Term Care among European Older Adults: An Empirical Approach Using the SHARE Survey. International Journal of Environmental Research and Public Health. 2021; 18(1):20. https://doi.org/10.3390/ijerph18010020
Chicago/Turabian StyleLera, Javier, Marta Pascual-Sáez, and David Cantarero-Prieto. 2021. "Socioeconomic Inequality in the Use of Long-Term Care among European Older Adults: An Empirical Approach Using the SHARE Survey" International Journal of Environmental Research and Public Health 18, no. 1: 20. https://doi.org/10.3390/ijerph18010020
APA StyleLera, J., Pascual-Sáez, M., & Cantarero-Prieto, D. (2021). Socioeconomic Inequality in the Use of Long-Term Care among European Older Adults: An Empirical Approach Using the SHARE Survey. International Journal of Environmental Research and Public Health, 18(1), 20. https://doi.org/10.3390/ijerph18010020





