Abstract
Background: obstetric violence can partially be represented by the high number of interventions and medicalization rates during the birthing process. The objective of the present study was to determine the interventionism and medicalization levels during childbirth in Spain. Methods: a descriptive, retrospective, and cross-sectional study was conducted between January 2018 and June 2019. Results: the intervention percentages were 34.2% for Kristeller maneuver and 39.3% for episiotomy. Differences appeared in public, private, and mixed healthcare settings (p < 0.001). The mean satisfaction, with healthcare in the different settings, was estimated at 6.88 points (SD ± 2.146) in public healthcare, 4.76 points (SD ± 3.968) in private healthcare, and 8.03 points (SD ± 1.930) in mixed healthcare (p < 0.001). No statistically significant differences were found in Spanish autonomous communities. Conclusions: births in Spain seem to be highly intervened. In this study, a certain equity criterion was found concerning interventionism during childbirth in Spain. Healthcare influenced female intervention, satisfaction, and perception levels for obstetric violence; this evidences that female empowerment plays an important role.
1. Introduction
Although no international consensus has been reached regarding a definition of obstetric violence (OV), some Latin American countries have passed laws on this problem [1]. The definition, published in Venezuela in 2007, in the Organic Law on Women’s Right to a Life Free of Violence, defines this concept as “…the appropriation of the body and reproductive processes of women by health personnel, which is expressed as dehumanized treatment, abuse of medication, and converting natural processes into pathological ones, which bring loss of autonomy and the ability to freely decide about their bodies and sexuality, and negatively impact women’s quality of life” [2]. This (and other definitions) refer to abusing medication and interventionism, while giving birth, as OV elements.
A recent literature review classified the unsuitable use of certain procedures and technologies as OV typology [3]. Some of the examples in the review were: iatrogenic procedures, abusive use of oxytocin, being unable to move to bed during childbirth, giving birth in the lithotomy position, routinely performing amniotomy, constant fetal monitoring, women not eating for long periods for no known reasons, unsuitable pain management, not performing skin-to-skin contact, and early umbilical cord clamping [3]. Other classifications exist that indicate excessive or non-consented interventions, as well as medicalization with mistreatment and abuse while giving birth [4].
In 1985, the World Health Organization (WHO)’s Declaration of Strength indicated that all women have the right to suitable prenatal healthcare, and to play a central role in all aspects of this healthcare, including participating in planning, carrying out, and evaluating healthcare [5]. The declaration also indicates the need for competent authorities to prepare specific policies about the use of technology during childbirth, for public and private centers, and to conduct joint surveys to assess healthcare technologies during childbirth [5]. Women formed part of the population to be considered in interviews [5].
Women’s own accounts of childbirth, available in the literature, often describe different obstetric interventions related to OV, such as not being accompanied by anyone, performing unnecessary cesarean sections, routine vaginal palpations, use of oxytocin, or performing the Kristeller maneuver, among other interventions [6,7,8] that are neither recommended nor backed by scientific evidence. Some studies also indicate a lack of respect and a higher level of intervention from the health professional’s point of view [9].
In Venezuela, some constitutive OV actions are considered: making women give birth in the supine position with raised legs; hindering early devotion; denying breastfeeding and skin-to-skin contact; altering the low-risk natural birth process by applying acceleration techniques without obtaining a woman’s voluntary, expressed, and informed consent [2]. In countries such as Brazil, we find that excessive interventions made while giving birth contribute to neonatal/maternal morbidity or mortality [10]. Other studies associate OV perceived by women with the lithotomic position, Kristeller maneuver, while giving birth, denying immediate skin-to-skin contact with their newborn baby [11].
In Croatia, intervention figures represent 54% for the Kristeller maneuver performed during childbirth, 70% for episiotomy, and 78% for using enemas [12]. In Italy, some intervention rates reported during childbirth are striking. Italy presents a rate of 32.54% for cesarean births and 54.24% for episiotomies, plus OV is perceived by 21.2% women [13]. In Spain, very few studies have assessed the interventions and use of technology during childbirth. It is known that the Kristeller maneuver is performed with approximately 25% of women giving birth vaginally [14], even though no scientific evidence exists to support its use. Other interventions, such as no-one accompanying the woman during childbirth, frequent vaginal palpations, using oxytocin, shaving the vulva, or applying episiotomy, are routinely carried out in Spain, and many are not even recorded in women’s medical records [15]. Some reports indicate that cesarean section rates in Spain are high, estimated at roughly 25%, with similar rates for episiotomies and instrumentalized births. Moreover, there is wide variation in Spanish Autonomous Communities (SAC), and between public and private healthcare sectors [16,17].
In Spain, a constitutional right exists that allows free access to the public health system, but the Spanish healthcare management model allows the co-existence of a public healthcare network and privately managed health centers. This means that people who pay for private health insurance can access both public and private healthcare. It is necessary to highlight that a Spanish national survey has reported that 47.3% of those surveyed would choose to pay private insurance, to be attended to during childbirth, or while a family relation does [18].
In 2010, the Spanish Ministry of Health published the Clinical Practice Guidelines for Healthcare during Normal Births, which urged the private health sector to be more transparent regarding birth and maternity healthcare indicators (and not solely reflect cesarean rates) [19]. Yet, since then, very little has been made public about these indicators. For all of these reasons, the objective of the present study was to know the interventionism and medicalization levels during childbirth in Spain, in public, private, and mixed healthcare centers, the distribution by SAC, and how OV is perceived by women.
2. Materials and Methods
2.1. Design, Population, and Sample
A descriptive, retrospective, and cross-sectional study was conducted from January 2018 to June 2019. The methodology is explained in-depth in the previous publication, Part I [20]. This work analyzed the subsample who gave birth during the study period in Spain. Women who were treated during the 2009 to 2018 period, and who completed the survey, were included in the study. The exclusion criteria included those whose childbirth took place at home or in a hospital outside Spanish territory, and the 80% (or more) of the survey forms that were incomplete. Those surveys completed by women from the Ceuta and Melilla SAC were excluded for not being sufficiently representative, as were those who did not answer the province item. The study was designed in accordance with the principles of the Declaration of Helsinki (charity, no maleficence, autonomy, and justice) and with Spanish Organic Law 03/2018 on Protection Personal Data and Guaranteeing Digital Rights. No personal data, IP address, or email that could compromise the participant’s identity was collected; answering the survey implied giving consent. Participants were informed of these aspects before voluntarily answering the survey.
2.2. Data Collection
Data collection took place between February and April 2018 using an ad hoc online survey. Those in charge of handing out surveys to women were healthcare professionals, child rearing associations, breastfeeding support groups, administrators of blogs and the association “El Parto es Nuestro/Birth is Ours” [21]. The link to the survey was forwarded via social networks, such as WhatsApp and Facebook [22,23].
The main study variables were the received healthcare type (public, private, or mixed, understood as women freely choosing between private and public healthcare), and the SAC attended during childbirth. Other variables were: believing they received unnecessary and/or painful interventions (yes, no, do not know); perceiving having suffered OV (yes, no, not know/no answer); feeling satisfied with the received healthcare (visual analogical scale, from 1 not at all satisfied to 10 extremely satisfied); and general view of the received healthcare: (a) empowered and satisfied; (b) insure, vulnerable, guilty, incapable; (c) indifferent; (d) not know/no answer.
Variables related to the interventions that women perceived as being unnecessary during childbirth were added, such as: using cupping glass or forceps, Hamilton maneuver, no one allowed to accompany them, lack of information, shaving vulva, using enemas, not being allowed to eat/drink, limiting movements, amniorrhexis, using oxytocin, constant vaginal palpations, Kristeller maneuver, early umbilical cord clamping, episiotomy, cesarean, manually removing placenta, not allowing skin-to-skin contact, bottle feeding the baby without the mother’s consent, or taking the baby away to perform medical actions. These variables were measured as “yes/no”; more than one variable could be answered.
2.3. Statistical Analysis
Data were processed using the Statistical Package for the Social Sciences (SPSS) v. 25, IBM, Armonk, NK, United States of America. A descriptive analysis was done on all of the variables with frequency and percentage. A bivariate analysis with the Chi squared test was carried out using contingency tables to compare the interventions and medicalization of the birth process in public, private, and mixed healthcare centers, and in the national territory, according to the cluster groups that the analysis gave in Part I, where SAC were classified according to how women perceived OV [20]. In this way, the distribution by cluster groups was as follows: group 1 was made up of SAC Madrid, Basque Country, Principality of Asturias and Castilla y León; group 2 with SAC Catalonia, Valencian Community, Aragón and Castilla-La Mancha; group 3 with Andalusia, Balearics, Canaries and Navarre; group 4 with Murcia Region, Galicia, Extremadura and Cantabria; the last group was formed by only one SAC: La Rioja. Women’s satisfaction with the healthcare they received was analyzed by a one-factor ANOVA.
Finally, a binary logistic regression analysis was performed to verify which obstetric interventions were associated independently with the variable “perceived OV”. Statistical significance was set at p < 0.05.
3. Results
We obtained 17,742 surveys, of which 201 were eliminated (1.13%): 88 (0.49%) for being completed by women who give birth abroad or for not being properly completed; 17 (0.09%) for coming from SAC Ceuta and Melilla; and 96 (0.54%) for not answering the province variable. The final sample comprised 17,541 surveys. Of these, 49.5% (n = 8675) of the women negatively answered if they had received unnecessary and/or painful procedures while giving birth, 44.4% (n = 7786) reported they had, and 6.2% (n = 1080) answered, “don’t know”.
We provide details of the unnecessary and/or painful procedures that women perceived they had undergone (n = 8866): 23.6% (n = 2094) using cupping glass or forceps; 21.5% (n = 1902) Hamilton maneuver; 27.9% (n = 2474) no-one accompanied them; 42.1% (n = 3735) lack of information; 7.7% (n = 687) shaving vulva, 9.1% (n = 803) applying enema; 34.3% (n = 3043) not being allowed to eat/drink during childbirth; 39.5% (n = 3505) restricted movements; 36.3% (n = 3216) amniorrhexis; 48.3% (n = 4281) using oxytocin; 31.9% (n = 2824) constant vaginal palpations; 34.2% (n = 3030) Kristeller maneuver; 21.0% (n = 1864) early umbilical cord clamping; 39.3% (n = 3483) performing episiotomy; 16.9% (n = 1502) unnecessary cesarean; 11.2% (n = 996) manually removed placenta; 36.9% (n = 3274) separating baby for no justified reason; 13.6% (n = 1206) bottle feeding the newborn without consent; 32.1% (n = 2850) taking the baby away for some test or technique; 10.1% (n = 899) other interventions.
3.1. Satisfaction and Interventions while Giving Birth and Their Relation to Received Healthcare Type
Of all the women, 65.3% (n = 11,450) women were attended to by the public healthcare sector and 24.3% (n = 4261) by a mixed public–private healthcare setting. The remaining 10.4% (n = 1830) went to a private healthcare center. Women’s satisfaction scored means of: 6.88 points (SD ± 2.146) for public healthcare; 4.76 points (SD ± 3.968) for private healthcare; and 8.03 points (SD ± 1.930) for mixed healthcare. There were statistically significant differences in groups (p < 0.001). When examining how they felt about the received healthcare, statistically significant differences were observed for the different healthcare types (X2 = 1686.89, df = 6, p < 0.001) (Table 1).

Table 1.
Feelings about the received healthcare depending on healthcare type (n = 17,539).
For healthcare type, 48.6% (n = 5561) of the women reported unnecessary and/or painful procedures in public healthcare, 58.4% (n = 1069) in private healthcare, and 27.1% (n = 7786) in mixed healthcare (X2 = 850.74, df = 4, p < 0.001). Of all the women who answered they had, 74.3% (n = 5077) also reported perceiving OV (X2 = 6862.82, df = 2, p < 0.001). Table 2 shows the analysis of perceiving OV in accordance with having endured unnecessary and/or painful procedures according to healthcare type. Table 3 and Figure 1 depict the descriptive and comparative data of the received interventions and healthcare type.

Table 2.
Descriptive Analysis of perceiving obstetric violence (OV) according to perceiving unnecessary and/or painful procedures and healthcare type (n = 15,783).

Table 3.
Descriptive data of the received interventions while giving birth and healthcare type.
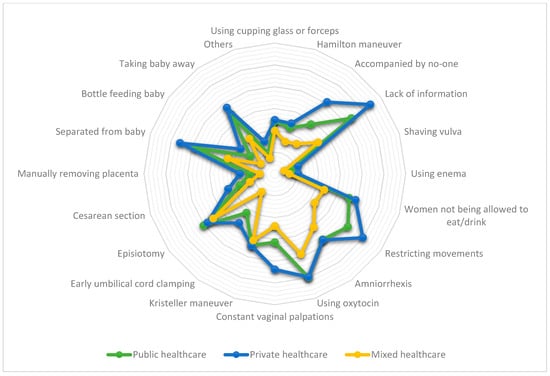
Figure 1.
Interventions while giving birth according to received healthcare type.
3.2. Interventions While Giving Birth and Their Relation to Cluster Groups
In the cluster groups, the following answered “yes” regarding receiving unnecessary and/painful procedures: 42.8% (n = 2930) in cluster 1; 45.3% (n = 2318) in cluster 2; 45.0% (n = 1281) in cluster 3; 46.5% (n = 1223) in cluster 4; 36.2% (n = 34) in cluster 5 (X2 = 23.81, df = 2, p = 0.002).
The analysis of interventions per cluster group showed only five interventions (shaving vulva, using enema, Kristeller maneuver, early umbilical cord clamping, and separated from baby) presented statistically significant differences among groups. The descriptive and comparative analysis results, about interventions during childbirth per cluster group, are found in Table 4 and Figure 2.

Table 4.
Descriptive data of the interventions received during childbirth and the assigned cluster group.
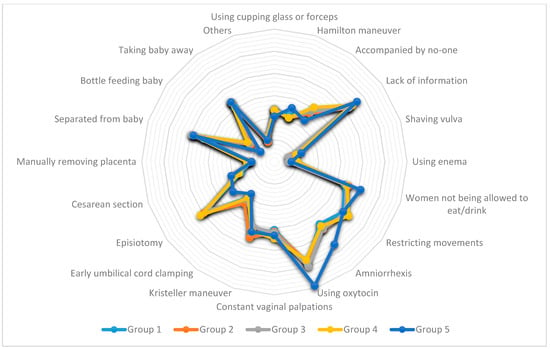
Figure 2.
Interventions during childbirth, according to cluster group.
3.3. Obstetric Interventions Related to Women Perceiving OV
The bivariate analysis between interventions and perceiving OV was significant for all of the studied interventions (p < 0.001). Finally, when considering the obstetric interventions made during childbirth along with women perceiving OV, a statistically significant logistic regression model was obtained (n = 7531, X2 = 2414.36, df = 27, p < 0.001). This model explained 39.2% (Nagelkerke R2 = 0.392) of variance in perceived OV and correctly classified 78.3% of the cases, with a sensitivity of 54.4% and a specificity of 88.0%. Of all the variables employed as predictors, only the cluster group, using enema, not being allowed to eat/drink, amniorrhexis, and using oxytocin, were not statistically significant (see Table 5).

Table 5.
Odds ratio and 95% confidence intervals of the multivariate logistic regression model that analyzed the obstetric interventions related to perceiving OV (n = 7531).
4. Discussion
The present study presents the interventionism and medicalization levels during childbirth in Spain; these levels were assessed in both public and private healthcare sectors. This analysis allowed us to see the interventionism distribution in different SAC by means of previously established cluster groups [20], a certain equity criterion was noted for interventionism and medicalization in the different SAC. Finally, the relation of interventions during childbirth with women’s perceived OV was assessed.
The fact that there is little evidence on interventionism and medicalization levels during pregnancy and childbirth in Spain is worrying. Few reports offer clear information about the rates at which interventions are made during childbirth in Spain. Only a few official reports are available regarding the rates of cesarean sections, perinatal, and/or maternal morbidity or mortality, as valid indicators [24,25], which are practically the only ones found to assess the quality of healthcare received while giving birth in Spain. The present study revealed that the interventionism and medicalization levels of the childbirth process in Spain are high. Techniques that are not recommended by international organizations, such as the WHO, are practiced in Spain. These practices included shaving pubic hair, using enemas, practicing Kristeller maneuver, no-one accompanying women, restricting movements, and lack of information [26]. These techniques are not recommended by the Clinical Practice Guidelines for Healthcare in Spain [15,19], but this seems to make no difference because they continue. Acceptable intervention rates have been set for other techniques to be practiced during childbirth, despite the WHO indicating that setting an acceptable intervention rate is hard with some techniques, such as episiotomy [26]. One technique with a set, suitable intervention rate is the cesarean section. The WHO indicates that its ideal rate must range between 10% and 15% [27]. According to the present study, Spain easily exceeds the recommended rate, and similar data also appear in other reports or studies [15,28].
Certain techniques can have major repercussions on women and a newborn’s health, which is the case with the Kristeller maneuver. This maneuver is neither recommended nor makes the delivery period shorter [19,29]. Its consequences include general bruising, abdominal bruising, fractured ribs, and even uterine tearing [29], which makes the legal repercussions of practicing this maneuver increasingly evident [30]. Notwithstanding, this maneuver is still employed in Spain, and previous reports and studies estimated that it is applied at a rate of around 25% [14,15]. This rate was even higher in the present study, as one third of the women gave a positive response to the question about it. Thus, we reflect that interventions during childbirth can have physical, mental, and emotional repercussions during a woman’s sexual and reproductive life [2,31], and having available, clear evidence for using interventions is essential. Furthermore, this interventionist approach can weaken a woman’s capacity during childbirth [14,32], and have negative effects on her birth experience [33]. It is worth stressing that, while some settings practice a few interventions too late, other women receive too many interventions and too soon [26,34], with possibly fatal consequences for the mother and baby. More studies are required concerning interventions during childbirth, their consequences on the mother’s physical, emotional, and mental health, the possible future conditions for the baby, and the most ideal ways to officially control use of interventions, technologies, and medications while giving birth.
This study determined similar percentages for the interventionism and medicalization rates among SAC in all of the analyzed cluster groups; little variability appeared in birth-related clinical practices. A certain equity criterion was established for interventionism and medicalization during childbirth in Spain. These results differ from previous reports, which indicated that variability in several obstetric interventions made among SAC was present [16,17]. One possible reason for this difference might lie in sources of information, because former reports have taken official medical records and publications as sources to acquire data, while the present study interviewed women, and despite the bias of selection in this study, the findings remain very important. It is true that women’s self-reports can be considered a limitation. Nevertheless, many maneuvers are not recorded in women’s medical records [15]. Given this situation among clusters, female perceptions seem to play a very relevant role in believing they suffered OV or received unnecessary and/or painful interventions. Thus, it is necessary to reflect on the concept that the WHO proposes as a positive delivery experience, which suggests that women wish to physiological labor and birth, and control through involvement in decision making, as well as personal achievements by participating in decision making, even when necessary and desired medical interventions are required [26]. The intention is for any intervention made while giving birth to form part of a security pairing—respect, and good maternal experience—which should be undividable. From this perspective, we ought to bear in mind two important aspects that can promote future works: (a) no available standard or agreement about the OV concept; (b) how the literacy level affects women’s health.
On the OV concept, we found that excessive interventionism and medicalization in physiological processes belong to part of some of their definitions and, hence, this part does not represent a whole. Thus, it seems plausible that, although excessive interventions are representative of the OV concept [35], as our multivariate model demonstrates, they do not represent the whole OV concept. This is why we found some results, such as distributing interventions into cluster groups, which are based on how women perceive OV.
It is possible that some women were unable to identify OV [36], and even take certain obsolete or harmful practices during childbirth as standard practice [10,36,37], which also came across in other areas [38]. Or, perhaps this problem can be more extended than studies actually reveal, and we are currently able to identify only a small part of the problem by taking an iceberg model as a reference, similarly to what other research works have found [39]. This vision invites us to reflect on the literacy concept for health. This concept is defined as the cognitive and social skills that determine motivation and the capacity to access, understand, and employ data that promote and maintain health [40]. Some authors suggest that such literacy includes the social, political and environmental factors that influence health [40]. The differences in the present work among interventions in public/private healthcare, cluster groups, and women perceived having received OV can only be understood from this perspective. As the percentage of OV in Spain is high [20], this perspective can also explain findings, such as this percentage considerably increasing, while bearing in mind the opinions of those women who indicate having suffered unnecessary and/or painful interventions while giving birth, which means that women’s empowerment can play a very important role [41]. Nonetheless, all of these literacy assumptions for health, empowerment, and OV should be confirmed by future studies.
Finally, we ought to focus on the obtained results when comparing healthcare type and obstetric interventions. Apparently, in Spain, a large portion of the population pays for private insurance, to receive the best attention during pregnancy and when giving birth [18]. In international terms, it is worth considering that the private sector attends to a substantial number of women for family planning reasons, such as pregnancies, births, and postpartum periods [42,43]. Thus, as in Spain, in order to improve materno-infant health and well-being, it is important to bear in mind better data collection and minimally controllable public indicators of the materno-infant health services rendered in this sector [19,43]. Furthermore, this study indicates higher interventionism levels in the private sector than in the public one and, in turn, perceived OV is also higher in the private sector [20]. Thus, we should reflect on the technical and human quality of such healthcare in the private health sector, which falls in line with what other authors have reported [44]. This consideration is reinforced by the results obtained for the mixed healthcare type included in the present research work. This mixed type reported a lower interventionism level, more satisfaction, and less perceived OV. It would seem that women’s empowerment plays a fundamental role, as it confers female autonomy to resort to resources and organizations, and to overcome structural or social restrictions [41]. Future studies should assess the use of health services and their type with female empowerment.
This study seems to have correctly assess the interventionism and medicalization phenomenon while giving birth in Spain, by comparing the different, available health sectors in this country (private, public, or mixed). However, this work is not without its limitations, which must be taken into account when interpreting its results. Firstly, we must contemplate that non-probabilistic sampling was carried out, which can affect the sample’s representativeness. A certain selection bias could have come into play as the survey was handed out by groups that might be more sensitive about the studied theme. Some variables were not included, such as age, socioeconomic, and cultural variables, number of children, or date of birth to perform a descriptive sociodemographic analysis in order to make comparisons with other populations. This retrospective study is based on women’s perceived OV, which may lead to memory or information biases. Finally, we stress that the Spanish healthcare model represents a single management model internationally, which means that some of its results cannot be extrapolated to other healthcare systems. Despite all of these limitations, we consider that the findings presented are relevant, offering a global vision of obstetric violence in Spain as a relevant problem that must be addressed by those responsible for the health system.
5. Conclusions
Despite its limitations, this study reports relevant results that have not been previously assessed concerning the interventionism and medicalization levels during childbirth in Spain, and their relation to OV. As we found, high levels of intervention can occur during childbirth in Spain, as, among others, maneuvers are applied that can pose a risk for women and babies’ health and lives (such as the Kristeller maneuver). It is very interesting to find that no statistically significant differences appeared among SAC in Spain nationwide, and this interventionism acts as an equity criterion in clinical practice in different SAC.
This interventionism (while giving birth) presents major differences when receiving public, private, or mixed healthcare (understood as that which each woman chooses when being attended to by public or private healthcare). As such, private healthcare has a high interventionism rate, less satisfaction, women feel more insecure and vulnerable, and they perceive more OV. Conversely, mixed healthcare presents lower intervention levels, more satisfaction, and fewer women perceiving OV, which allows us to think that female empowerment plays a very important role. Finally, the logistic regression model shows that most analyzed interventions are representative of OV, without forgetting that interventionism and medicalization during childbirth form only a small part of the OV problem.
Author Contributions
Conceptualization, S.I.-C. and D.M.-T.; methodology, V.M.G.-C., S.I.-C., Á.C.-G., and D.M.-T.; formal analysis, M.J.V.-C. and D.M.-T.; writing—original draft preparation, D.M.-T., L.A.-P.; writing—review and editing, all of the authors; project administration, D.M.-T.; funding acquisition, D.M.-T. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Universitat Jaume I; grant number UJI-A2019-06.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
The authors thank the Universitat Jaume I for supporting them in carrying out this project. They also wish to stress the importance of the female responses and participation in this study, because the intention is to improve the quality of the health system, and the required support lies in these responses.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Williams, C.R.; Jerez, C.; Klein, K.; Correa, M.; Belizán, J.M.; Cormick, G. Obstetric Violence: A Latin American Legal Response to Mistreatment during Childbirth. BJOG Int. J. Obstet. Gynaecol. 2018, 125, 1208–1211. [Google Scholar] [CrossRef]
- Pérez D’gregorio, R. Obstetric Violence: A New Legal Term Introduced in Venezuela. Int. J. Gynecol. Obstet. 2010, 111, 201–202. [Google Scholar] [CrossRef]
- Jardim, D.M.B.; Modena, C.M. Obstetric Violence in the Daily Routine of Care and Its Characteristics. Rev. Lat. Am. Enfermagem 2018, 26, e3069. [Google Scholar] [CrossRef]
- Bohren, M.A.; Vogel, J.P.; Hunter, E.C.; Lutsiv, O.; Makh, S.K.; Souza, J.P.; Aguiar, C.; Saraiva Coneglian, F.; Diniz, A.L.A.; Tunçalp, Ö.; et al. The Mistreatment of Women during Childbirth in Health Facilities Globally: A Mixed-Methods Systematic Review. PLoS Med. 2015, 12, e1001847. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Appropriate Technology for Birth. Lancet 1985, 24, 436–437. [Google Scholar]
- Šimonović, D. A Human Rights-Based Approach to Mistreatment and Violence against Women in Reproductive Health Services with a Focus on Childbirth and Obstetric Violence; New York, 2019. Available online: https://digitallibrary.un.org/record/3823698 (accessed on 29 December 2020).
- Vallana Sala, V.V. “It’s Nice to Make Them but Not Have Them”: Analysis of Obstetric Violence during Delivery Care in Colombia. Rev. Ciencias la Salud 2019, 17, 128–144. [Google Scholar] [CrossRef]
- Brandão, T.; Cañadas, S.; Galvis, A.; de los Ríos, M.M.; Meijer, M.; Falcon, K. Childbirth Experiences Related to Obstetric Violence in Public Health Units in Quito, Ecuador. Int. J. Gynecol. Obstet. 2018, 143, 84–88. [Google Scholar] [CrossRef] [PubMed]
- Begley, C.; Sedlicka, N.; Daly, D. Respectful and Disrespectful Care in the Czech Republic: An Online Survey. Reprod. Health 2018, 15, 198. [Google Scholar] [CrossRef] [PubMed]
- Lansky, S.; de Souza, K.V.; de Morais Peixoto, E.R.; Oliveira, B.J.; Diniz, C.S.G.; Vieira, N.F.; de Oliveira Cunha, R.; de Lima Friche, A.A. Obstetric Violence: Influences of the Senses of Birth Exhibition in Pregnant Women Childbirth Experience. Ciência e Saúde Coletiva 2019, 24, 2811–2824. [Google Scholar] [CrossRef]
- Cunha Rodrigues, F.A.; Gama Lira, S.V.; Magalhães, P.H.; Freitas, A.L.e.V.; da Silva Mitros, V.M.; Almeida, P.C. Violência Obstétrica No Processo de Parturição Em Maternidades Vinculadas à Rede Cegonha. Reprod. e Clim. 2017, 32, 78–84. [Google Scholar] [CrossRef]
- Šimonović, D. Report to the United Nations Special Rapporteur on Violence Against Women in Response to Her Call for Submissions Due 17 May 2019; RODA-Parents in Action: Zagreb, Croatia, 2019. Available online: https://www.ohchr.org/Documents/Issues/Women/SR/ReproductiveHealthCare/Roda%20%E2%80%93%20Parents%20in%20Action%20Croatia.pdf (accessed on 29 December 2020).
- Ravaldi, C.; Skoko, E.; Battisti, A.; Cericco, M.; Vannacci, A. Abuse and Disrespect in Childbirth Assistance in Italy: A Community-Based Survey. Eur. J. Obstet. Gynecol. Reprod. Biol. 2018, 224, 208–209. [Google Scholar] [CrossRef] [PubMed]
- Rubashkin, N.; Torres, C.; Escuriet, R.; Dolores Ruiz-Berdún, M. “Just a Little Help”: A Qualitative Inquiry into the Persistent Use of Uterine Fundal Pressure in the Second Stage of Labor in Spain. Birth 2019, 46, 517–522. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Sanidad Servicios Sociales e Igualdad. Informe Sobre La Atención Al Parto y Nacimiento En El Sistema Nacional de Salud; Madrid, Spain, 2012. Available online: https://www.mscbs.gob.es/organizacion/sns/planCalidadSNS/pdf/InformeFinalEAPN_revision8marzo2015.pdf (accessed on 29 December 2020).
- Salgado Barreira, Á.; Maceira Rozas, M.; López Ratón, M.; Atienza Merino, G. Variabilidad Del Parto En España. Análisis Del Conjunto Mínimo Básico de Datos Al Alta Hospitalaria. Progresos Obstet. y Ginecol. 2010, 53, 215–222. [Google Scholar] [CrossRef]
- Ministerio de Ciencia e Innovación. Labour Care in Healthy Women. Study of Variability and Systematic Review; Ministerio de Ciencia e Innovación: Madrid, Spain, 2009.
- Ministerio de Sanidad Consumo y Bienestar Social. Barómetro Sanitario 2018; Madrid, Spain, 2018. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/BarometroSanitario/Barom_Sanit_2018/BS2018_mar.pdf (accessed on 29 December 2020).
- Ministerio de Sanidad. Guía de Práctica Clínica Sobre La Atención Al Parto Normal; Vitoria-Gasteiz, Spain, 2010. Available online: https://www.mscbs.gob.es/organizacion/sns/planCalidadSNS/pdf/equidad/guiaPracClinPartoCompleta.pdf (accessed on 29 December 2020).
- Mena-Tudela, D.; Iglesias-Casás, S.; González-Chordá, V.M.; Cervera-Gasch, A.; Andreu-Pejó, L.; Valero-Chilleron, M.J. Obstetric Violence in Spain (Part I): Women’s Perception and Interterritorial Differences. Int. J. Environ. Res. Public Health 2020, 17, 7726. [Google Scholar] [CrossRef] [PubMed]
- Villarmea, S.; Olza, I.; Recio, A. El Parto Es Nuestro: El Impacto de Una Asociación de Usuarias En La Reforma Del Sistema Obstétrico de España. Dilemata 2015, 7, 157–183. [Google Scholar]
- Pedersen, E.R.; Kurz, J. Using Facebook for Health-Related Research Study Recruitment and Program Delivery. Curr. Opin. Psychol. 2016, 9, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Christensen, T.; Riis, A.H.; Hatch, E.E.; Wise, L.A.; Nielsen, M.G.; Rothman, K.J.; Sørensen, H.T.; Mikkelsen, E.M. Costs and Efficiency of Online and Offline Recruitment Methods: A Web-Based Cohort Study. J. Med. Internet Res. 2017, 19. [Google Scholar] [CrossRef]
- Ministerio de Sanidad Consumo y Bienestar Social. Portal Estadístico. Sistema de Información del Área de Especializada. Available online: https://pestadistico.inteligenciadegestion.mscbs.es/publicoSNS/C/siae/siae/hospitales/actividad-asistencial/actividad-obstetrica (accessed on 6 November 2020).
- Minsierio de Sanidad Consumo y Bienestar Social. Indicadores Clave del Sistema Nacional de Salud. Available online: http://inclasns.msssi.es/main.html (accessed on 30 July 2020).
- World Health Organization. WHO Recommendations: Intrapartum Care for a Positive Childbirth Experience. World Health Organization, 2018. Available online: https://www.who.int/reproductivehealth/publications/intrapartum-care-guidelines/en/ (accessed on 29 December 2020).
- World Health Organization. WHO Statement on Caesarean Section Rates. Geneva, Switzerland, 2015. Available online: https://apps.who.int/iris/bitstream/handle/10665/161442/WHO_RHR_15.02_eng.pdf?sequence=1 (accessed on 29 December 2020).
- Vila-Candel, R.; Martín, A.; Escuriet, R.; Castro-Sánchez, E.; Soriano-Vidal, F.J. Analysis of Caesarean Section Rates Using the Robson Classification System at a University Hospital in Spain. Int. J. Environ. Res. Public Health 2020, 17, 1575. [Google Scholar] [CrossRef]
- Hofmeyr, G.J.; Vogel, J.P.; Cuthbert, A.; Singata, M. Fundal Pressure during the Second Stage of Labour. Cochrane Database Syst. Rev. 2017, 3, CD006067. [Google Scholar] [CrossRef]
- Malvasi, A.; Zaami, S.; Tinelli, A.; Trojano, G.; Montanari Vergallo, G.; Marinelli, E. Kristeller Maneuvers or Fundal Pressure and Maternal/Neonatal Morbidity: Obstetric and Judicial Literature Review. J. Matern. Neonatal Med. 2019, 32, 2598–2607. [Google Scholar] [CrossRef]
- Guillén, F.F. What Is Obstetric Violence? Some Social, Ethical and Legal Aspects. ILEMATA 2015, 7, 113–128. [Google Scholar]
- Borges, M.T. A Violent Birth: Reframing Coerced Procedures During Childbirth as Obstetric Violence. Duke Law J. 2018, 67, 827–862. [Google Scholar] [PubMed]
- Renfrew, M.J.; McFadden, A.; Bastos, M.H.; Campbell, J.; Channon, A.A.; Cheung, N.F.; Silva, D.R.A.D.; Downe, S.; Kennedy, H.P.; Malata, A.; et al. Midwifery and Quality Care: Findings from a New Evidence-Informed Framework for Maternal and Newborn Care. Lancet 2014, 384, 1129–1145. [Google Scholar] [CrossRef]
- Miller, S.; Abalos, E.; Chamillard, M.; Ciapponi, A.; Colaci, D.; Comandé, D.; Diaz, V.; Geller, S.; Hanson, C.; Langer, A.; et al. Beyond Too Little, Too Late and Too Much, Too Soon: A Pathway towards Evidence-Based, Respectful Maternity Care Worldwide. Lancet 2016, 388, 2176–2192. [Google Scholar] [CrossRef]
- Sadler, M.; Santos, M.J.; Ruiz-Berdún, D.; Rojas, G.L.; Skoko, E.; Gillen, P.; Clausen, J.A. Moving beyond Disrespect and Abuse: Addressing the Structural Dimensions of Obstetric Violence. Reprod. Health Matters 2016, 24, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Flores, Y.Y.R.; Ledezma, A.G.M.; Ibarra, L.E.H.; Acevedo, C.E.G. Social Construction of Obstetric Violence of Tenek and Nahuatl Women in Mexico. Rev. Esc. Enferm. 2019, 53, e03464. [Google Scholar] [CrossRef]
- Bowser, D.; Hill, K. Exploring Evidence for Disrespect and Abuse in Facility-Based Childbirth Report of a Landscape Analysis. Harvard School of Public Health: University Research Co., Boston, MA, USA, 2010, doi:10.1624/105812410X514413. Available online: https://cdn1.sph.harvard.edu/wp-content/uploads/sites/2413/2014/05/Exploring-Evidence-RMC_Bowser_rep_2010.pdf (accessed on 29 December 2020).
- Mena-Tudela, D.; González-Chordá, V.M.; Soriano-Vidal, F.J.; Bonanad-Carrasco, T.; Centeno-Rico, L.; Vila-Candel, R.; Castro-Sánchez, E.; Cervera Gasch, Á. Changes in Health Sciences Students’ Perception of Obstetric Violence after an Educational Intervention. Nurse Educ. Today 2020, 88, 104364. [Google Scholar] [CrossRef]
- Mena-Tudela, D.; Cervera-Gasch, Á.; Alemany-Anchel, M.J.; Andreu-Pejó, L.; González-Chordá, V.M. Design and Validation of the PercOV-S Questionnaire for Measuring Perceived Obstetric Violence in Nursing, Midwifery and Medical Students. Int. J. Environ. Res. Public Health 2020, 17, 8022. [Google Scholar] [CrossRef]
- Nutbeam, D. Health Literacy as a Public Health Goal: A Challenge for Contemporary Health Education and Communication Strategies into the 21st Century. Health Promot. Int. 2000, 15, 259–267. [Google Scholar] [CrossRef]
- Diamond-Smith, N.; Treleaven, E.; Murthy, N.; Sudhinaraset, M. Women’s Empowerment and Experiences of Mistreatment during Childbirth in Facilities in Lucknow, India: Results from a Cross-Sectional Study. BMC Pregnancy Childbirth 2017, 17 (Suppl. 2), 335. [Google Scholar] [CrossRef]
- Dennis, M.L.; Benova, L.; Owolabi, O.O.; Campbell, O.M.R. Meeting Need vs. Sharing the Market: A Systematic Review of Methods to Measure the Use of Private Sector Family Planning and Childbirth Services in Sub-Saharan Africa. BMC Health Serv. Res. 2018, 18, 699. [Google Scholar] [CrossRef] [PubMed]
- Campbell, O.M.R.; Benova, L.; Macleod, D.; Baggaley, R.F.; Rodrigues, L.C.; Hanson, K.; Powell-Jackson, T.; Penn-Kekana, L.; Polonsky, R.; Footman, K.; et al. Family Planning, Antenatal and Delivery Care: Cross-Sectional Survey Evidence on Levels of Coverage and Inequalities by Public and Private Sector in 57 Low- and Middle-Income Countries. Trop. Med. Int. Health 2016, 21, 486–503. [Google Scholar] [CrossRef] [PubMed]
- Hirose, A.; Yisa, I.O.; Aminu, A.; Afolabi, N.; Olasunmbo, M.; Oluka, G.; Muhammad, K.; Hussein, J. Technical Quality of Delivery Care in Private- and Public-Sector Health Facilities in Enugu and Lagos States, Nigeria. Health Policy Plan. 2018, 33, 666–674. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).