New Insights about Chronic Pelvic Pain Syndrome (CPPS)
Abstract
1. Overview on Women with CPPS
2. Materials and Methods
Search Strategy
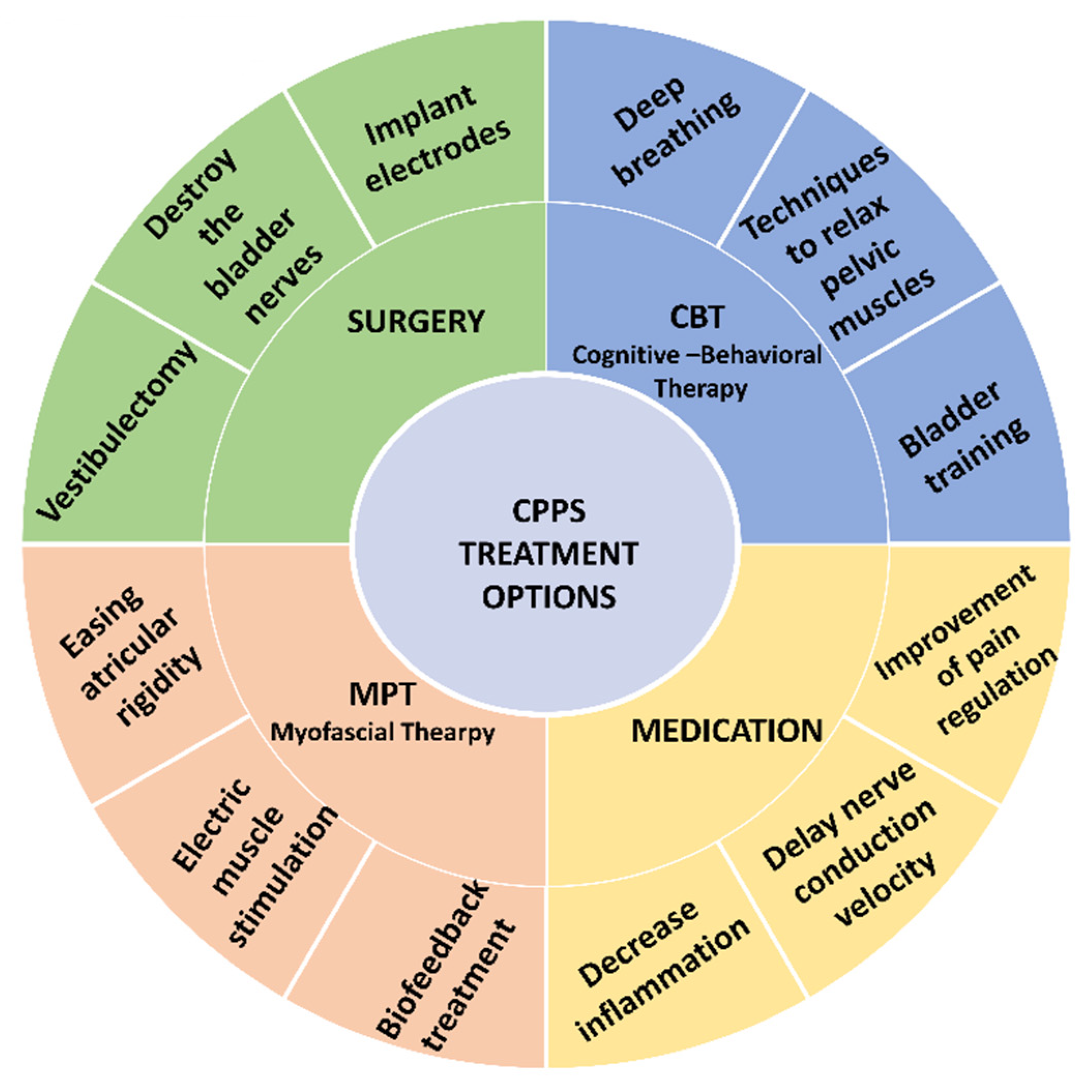
- Cognitive behavioral therapy (CBT) includes deep breathing, learning techniques to control (contract and relax) pelvic muscles, and bladder training. Bladder training teaches patients to control the disease (for example, by prolonging periods between urinations by using various mind distracting methods) and has been proven to increase urine volumes and decrease urination frequency [20,22,24];
- Medications include drugs such as tricyclides and sodium pentosanpolysulfate (which inhibits histamine release from mast cells) or drugs that are injected into the bladder (for example, glycosaminoglycans that are part of the bladder’s natural protection layer; resiniferatoxin and capsaicin that bind to nerve-ending receptors and desensitize pain fibers; and botolonium toxin that inhibits the secretion of inflammatory agents such as substance p and nerve growth factor and prevents higher tonus of pelvic muscles). Most drugs tested on CPPS patients showed good short-term results [30], but only a few were found to have long-term results [20,22]. There is evidence of some success in response to hormone therapy administered orally, by ointment, or by injection [54,55,56]. The various drugs are administered systemically or locally, and they can be classified by their action mechanisms: (1) Improvement of pain regulation (assuming the pain is neuropathic) by drugs that inhibit reuptake of noradrenaline and serotonin, and improve functioning of the downward pain-processing conduits [57,58]; (2) Preparations that delay nerve conduction velocity by using anesthetics; these have been tested by a number of studies, and were found to have limited effectiveness [59]; and (3) Drugs that inhibit production of prostaglandins, or steroid-type drugs, administered due to the assumption that CPPS has an inflammatory source [41] (Table 1);
- Surgery is a last resort when traditional treatment has failed. Some surgeries of PBS women destroy the bladder nerves and others implant electrodes that electrically stimulate the nerve roots. However, this treatment, as is the case in other chronic diseases, provides only a partial solution, and is not based on empiric guidelines. Therefore, the mechanisms at the root of CPPS must be understood to identify which women are suitable for this kind of treatment [20,60]. Women with PVD are sometimes offered a vestibulectomy, in which the mucous membrane of the vagina, the hymen, and some glands in the area are removed [54,61,62,63]; and
3. Myofascial Physical Therapy (MPT)
4. Psychological Factors and Pain
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
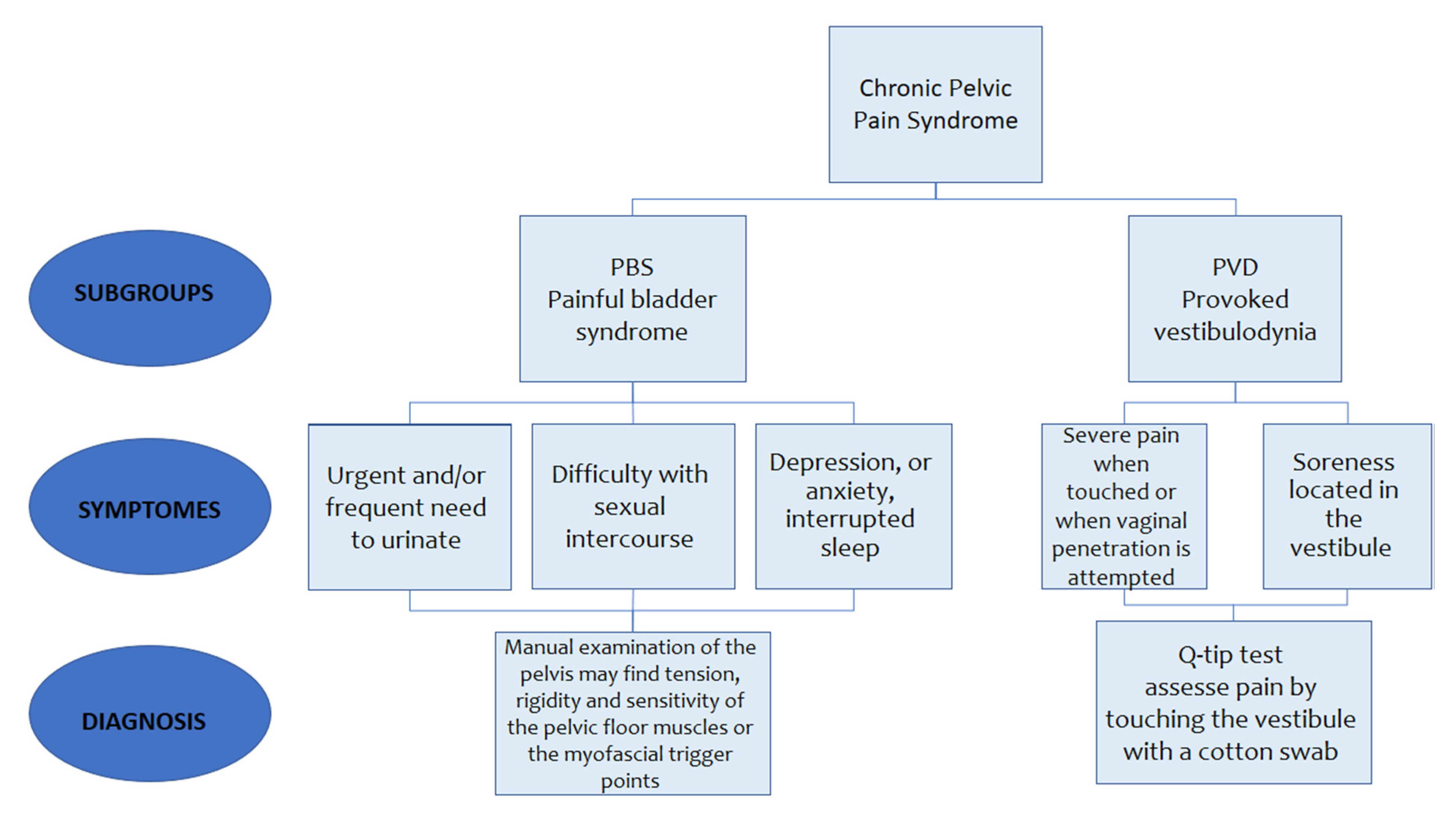
| CPPS | Chronic pelvic pain syndrome |
| PBS | Painful bladder syndrome |
| PVD | Provoked vestibulodynia |
| GAG | Glycosaminoglycan |
| ACC | Anterior cingulate cortex |
| CBT | Cognitive behavioral therapy |
| MPT | Mechanical pain threshold |
| MMT | Myofascial manual therapy |
| IBS- | Inflammatory bowel syndrome |
| PCS | Pain catastrophizing scale |
| FA | Fear-avoidance |
References
- Grinberg, K.; Granot, M.; Lowenstein, L.; Abramov, L.; Weissman-Fogel, I. A common pro-nociceptive pain modulation profile typifying subgroups of chronic pelvic pain syndromes is interrelated with enhanced clinical pain. Pain 2017, 158, 1021–1029. [Google Scholar] [CrossRef] [PubMed]
- Klotz, S.G.R.; Ketels, G.; Richardsen BLowe, B.; Brumahi, C.A. Physiotherapeutic assessment of chronic pelvic pain syndrome. Development of a standardized physiotherapeutic assessment instrument for interprofessional cooperation in patients with chronic pelvic pain syndrome. Man. Med. 2019, 57, 181–187. [Google Scholar] [CrossRef]
- Speer, L.M.; Mushkbar, S.; Erbele, T. Chronic pelvic pain in women. Am. Fam. Phys. 2016, 93, 380–387. [Google Scholar]
- Ahangari, A. Prevalence of Chronic Pelvic Pain among Women: An Updated Review. Pain Phys. 2014, 17, 141–147. [Google Scholar]
- Mathias, S.D.; Kuppermann, M.; Liberman, R.F.; Lipschutz, R.C.; Steege, J.E. Chronic pelvic pain: Prevalence, health-related quality of life, and economic correlates. Obstet. Gynecol. 1996, 87, 321–327. [Google Scholar] [CrossRef]
- Zivi, A.; Sagie-Maor, A.; Ben-Shushan, A.; Rozensky, N. Chronic pelvic pain and Allen masteres syndrome. Harefua 2009, 148, 424–426. [Google Scholar]
- Stones, R.W.; Cheong, Y.C.; Howard, F.M.; Singh, S. Interventions for treating chronic pelvic pain in women (Review). Cochrane Collab. 2010, 11, 1–43. [Google Scholar]
- Giamberardino, M.; Tana, C.; Costantini, R. Pain threshold in women with chronic pelvic pain. Curr. Opin. Obstet. Gynecol. 2014, 26, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Nickel, J.C.; Tripp, D.A.; Pontari, M.; Moldwin, R.; Mayer, R.; Carr, L.K.; Doggweiler, R.; Yang, C.; Mishra, N.; Nordling, J. Psychosocial Phenotyping in Women With Interstitial Cystitis/Painful Bladder Syndrome: A Case Control Study. J. Urol. 2010, 183, 167–172. [Google Scholar] [CrossRef]
- Katz, L.; Tripp, D.A.; Curtis-Nickel, J.; Mayer, R.; Reimann, M.; Ophoven, V.A. Disability in women suffering from interstitial cystitis/ painful bladder syndrome. Br. J. Urol. Int. 2012, 111, 114–121. [Google Scholar] [CrossRef]
- Warren, J.W.; Brown, J.; Tracy, K.; Langenberg, P.; Wesselmann, U.; Greenberg, I. Evidence-Based Criteria for Pain of Interstitial Cystitis/Painful Bladder Syndrome in Women. Urology 2008, 71, 441–448. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, E.G. Vulvar vestibulitis syndrome. J. Reprod. Med. 1987, 32, 110–114. [Google Scholar] [PubMed]
- Naess, I.; Bo, K. Pelvic floor muscle function in women with provoked vestibulodynia and asymptomatic controls. Int. Urogenecol. J. 2015, 26, 1467–1473. [Google Scholar] [CrossRef] [PubMed]
- Heddini, U.; Bohm-Starke, N.; Nilsson, K.W.; Johannesson, U. Provoked vestibulodynia-medical factors and comorbidity associated with treatment outcome. J. Sex. Med. 2012, 9, 1400–1406. [Google Scholar] [CrossRef]
- Ghizzani, A.; Di Sabatino, V.; Suman, L.A.; Biasi, G.; Santarcangelo, E.L.; Carli, G. Pain symptoms in fibromyalgia patients with and without provoked vestibulodynia. Pain Res. Treat. 2014, 2014, 457618. [Google Scholar]
- Farage, M.A.; Miller, K.W.; Ledger, W. Localized Provoked Vestibulodynia: Do Multiple Etiologic Triggers Manifest as Neurogenic Vulvar Pain? J. Genit. Syst. Disord. 2014, 3, 1–6. [Google Scholar] [CrossRef]
- Moyal-Barracco, M.; Lynch, P.J. Terminology and classification of vulvodynia: A historical perspective. J. Reprod. Med. 2004, 49, 772–777. [Google Scholar]
- Sutton, K.S.; Pukall, C.F.; Chamberlain, S. Diffuse noxious inhibitory control function in women with provoked vestibulodynia. Clin. J. Pain 2012, 28, 667–674. [Google Scholar] [CrossRef]
- Andersson, K.E.; Nomiya, M.; Sawada, N.; Yamaguchi, O. Pharmacological treatment of chronic pelvic ischemia. Ther. Adv. Urol. 2014, 6, 105–114. [Google Scholar] [CrossRef]
- Hanno, P.; Nordling, J.; Fall, M. Bladder Pain Syndrome. Med. Clin. N. Am. 2011, 95, 55–73. [Google Scholar] [CrossRef]
- Homma, Y.; Udea, T.; Tomoe, H.; Lin, A.T.; Kuo, H.C.; Lee, M.H.; Lee, J.G.; Yoon-Kim, D.; Lee, K.S. Clinical guidelines for interstitial cystitis and hypersensitive bladder syndrome. Int. J. Urol. 2009, 16, 597–615. [Google Scholar] [CrossRef]
- Stones, R.W.; Mountfield, J. Interventions for treating chronic pelvic pain in women. Cochrane Database Syst. Rev. 2004, 387–391. [Google Scholar] [CrossRef]
- Dumoulin, C.; Bourbonnais, D.; Lemieux, M.C. Development of a dynamometer for measuring the isometric force of the pelvic floor musculature. Neurourol. Urodyn. 2003, 22, 648–653. [Google Scholar] [CrossRef]
- Van-Lankveld, J.J.D.M.; Granot, M.; Weijmar-Schultz, W.C.M.; Binik, Y.M.; Wesselmann, U.; Pukall, C.; Bohm-Starke, N.; Achtrari, C. Women’s sexual pain disorders. J. Sex. Med. 2010, 7, 615–631. [Google Scholar] [CrossRef] [PubMed]
- Forrest, J.B.; Mishell, D.R. Breaking the cycle of pain in interstitial cystitis/painful bladder syndrome: Toward standartization of early diagnosis and treatment-consensus panel recommendations. J. Reprod. Med. 2009, 54, 3–14. [Google Scholar] [PubMed]
- Bohm-Starke, N.; Hilliges, M.; Brodda-Jansen, G.; Rylander, E.; Torebjork, E. Psychophysical evidence of nociceptor sensitization in vulvar vestibulitis syndrome. Pain 2001, 94, 177–183. [Google Scholar] [CrossRef]
- Treede, R.D.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.; First, M.; et al. Chronic pain as a symptom or a disease: The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain 2018, 160, 19–27. [Google Scholar] [CrossRef]
- Ness, T.J.; Lloyd, L.K.; Fillingim, R.B. An endogenous pain control system is altered in subjects with interstitial cystitis. J. Urol. 2014, 191, 364–370. [Google Scholar] [CrossRef]
- Lowenstein, L.; Kenton, K.; Mueller, E.R.; Brubaker, L.; Heneghan, M.; Senka, J.; Fitzgerald, P. Patients with painful bladder syndrome have altered response to thermal stimuli and catastrophic reaction to painful experiences. Neurourol. Urodyn. 2009, 28, 400–404. [Google Scholar] [CrossRef]
- Stav, K. Painful Bladder Syndrome—It is worth knowing. Harefua 2011, 150, 168–174. [Google Scholar]
- FitzGerald, M.P.; Brensinger, C.; Brubaker, L.; Propert, K. What is the pain of interstitial cystitis like? Int. Urogynecol. J. Pelvic Floor Dysfunct. 2006, 17, 69–72. [Google Scholar] [CrossRef] [PubMed]
- Granot, M.; Goldstein-Ferber, S. Prediction of post-operative pain intensity by assessment of pain catastrophizing scale and anxiety. Clin. J. Pain 2005, 21, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Granot, M.; Friedman, M.; Yarnitsky, D.; Zimmer, E. Enhancement of the perception of systemic pain in women with vulvar vestibulitis. Int. J. Obstet. Gynaecol. 2002, 109, 863–866. [Google Scholar] [CrossRef] [PubMed]
- Johannesson, U.; Nygren de Boussard, C.; Jansen, J.B.; Bohm Starke, N. Evidence of diffuse noxious inhibitory controld (DNIC) elicited by cold noxious stimulation in patients with provoked vestibulodynia. Pain 2007, 130, 31–39. [Google Scholar] [CrossRef]
- Kaya, S.; Hemans, L.; Willems, T. Central sensitization in urogynecological chronic pelvic pain: A systematic literature review. Pain Phys. 2013, 16, 291–308. [Google Scholar]
- Ness, T.J.; Powell-Boone, T.; Cannon, R.; Lloyd, L.K.; Fillingim, R.B. Psychophysical evidence of hypersensitivity in subjects with interstitial cystitis. J. Urol. 2005, 173, 1983–1987. [Google Scholar] [CrossRef]
- Harlow, B.L.; Stewart, B.G. A population-based assessment of chronic unexplained vulvar pain: Have we underestimated the prevalence of vulvodynia? J. Am. Med. Women Assoc. 2003, 58, 82–88. [Google Scholar]
- Pukall, C.F.; Baron, M.; Amsel, R.; Khalife, S.; Binik, Y.M. Tender point examination in women with vulvar vestibulitis syndrome. Clin. J. Pain 2006, 22, 601–609. [Google Scholar] [CrossRef]
- Hampson, J.P.; Reed, B.D.; Clauw, D.J.; Bhavsar, R.; Gracely, R.H.; Haefner, H.K.; Harris, R.E. Augmented Central Pain Processing in Vulvodynia. J. Pain 2013, 14, 579–589. [Google Scholar] [CrossRef]
- As Sanie, S.; Harris, R.E.; Napadov, V.; Kim, J.; Neshewat, G.; Kairys, A.; Williams, D.; Clauw, D.J.; Schmidt-Wilcke, T. Changes in regional gray matter volume in woman with chronic pelvic pain: A voxel based morphometry study. Pain 2012, 153, 1006–1014. [Google Scholar] [CrossRef]
- Davis, N.F.; Brady, C.M.; Creagh, T. Interstitial cystitis/painful bladder syndrome: Epidemiology pathophysiology and evidence based treatment options. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 175, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Wilcke, T.; Leinisch, E.; Ganssbauer, S.; Draganski, B.; Bogdahn, U.; Altmeppen, J. Affective components and intensity of pain correlate with structural differences in gray matter in chronic back pain patients. Pain 2006, 125, 89–97. [Google Scholar] [CrossRef]
- Schmidt-Wilcke, T.; Ganssbauer, S.; Neuner, T.; Bogdahn, U.; May, A. A subtle gray matter changes between migraine patients and healthy controls. Cephalagia 2008, 28, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Hsu, M.C.; Harris, R.E.; Sundgren, P.C.; Welsh, R.C.; Fernandes, C.R.; Clauw, D.J. No consistent difference in a gray matter volume between individuals with fibromyalgia and age matched healthy subjects when controlling for affective disorder. Pain 2009, 143, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Gyang, A.; Hartman, M.; Lamu, G. Musculoskeletal causes of chronic pelvic pain. Obstet. Gynecol. 2013, 121, 645–650. [Google Scholar] [CrossRef]
- Apkarian, A.V.; Bushnell, M.C.; Treede, R.D.; Zubieta, J.K. Human brain mechanisms of pain perception and regulation in health and disease. Eur. J. Pain 2004, 9, 463–484. [Google Scholar] [CrossRef] [PubMed]
- Nimnuan, C.; Rabe-Hesketh, S.; Wessely, S.; Hotopf, M. How many functional syndromes? J. Psychosom. Res. 2001, 51, 549–557. [Google Scholar] [CrossRef]
- Warren, J.; Morozov, V.; Howard, F. Could chronic pelvic pain be a functional somatic syndrome? Am. J. Obstet. Gynecol. 2011, 205, 199-e1. [Google Scholar] [CrossRef]
- Krieger, J.N.; Stephens, A.J.; Landis, J.R.; Clemens, J.Q.; Kreder, K.; Lai, H.H.; Afari, N.; Rodríguez, L.; Schaeffer, A.; Mackey, S.; et al. Relationship between chronic nonurological associated somatic syndromes and symptom severity in urological chronic pelvic pain syndromes: Baseline evaluation of the MAPP study. J. Urol. 2015, 193, 1254–1262. [Google Scholar] [CrossRef]
- Hughes, L. Physical and Psychological Variables That Influence Pain in Patients with Fibromyalgia. Orthop. Nurs. 2006, 25, 112–119. [Google Scholar] [CrossRef]
- Jones, K.D.; Maxwell, C.; Mist, S.D.; King, V.; Denman, M.A.; Gregory, W.T. Pelvic Floor and Urinary Distress in Women with Fibromyalgia. Pain Manag. Nurs. 2015, 16, 834–840. [Google Scholar] [CrossRef] [PubMed]
- Grinberg, K.; Granot, M.; Lowenstein, L.; Abramov, L.; Weissman-Fogel, I. Negative Illness Perceptions are Associated with a Pro-nociceptive Modulation Profile and Augmented Pelvic Pain. Clin. J. Pain 2018, 34, 1141–1148. [Google Scholar] [CrossRef] [PubMed]
- Kronenberg, R.; Ludin, S.; Fischer, L. Severe Case of Chronic Pelvic Pain Syndrome: Recovery after Injection of Procaine into the Vesicoprostatic Plexus—Case Report and Discussion of Pathophysiology and Mechanisms of Action. Case Rep. Urol. 2018, 2018, 9137215. [Google Scholar] [CrossRef] [PubMed]
- Andrews, J.C. Vulvodynia Interventions—Systematic Review and Evidence Grading. Obstet. Gynecol. Surv. 2011, 66, 299–315. [Google Scholar] [CrossRef]
- Bergeron, S.; Binik, Y.M.; Khalife, S.; Pgidas, K.; Glazer, H.I.; Meana, M.; Amsel, R. Arandomized comparison of group cognitive-behavioral therapy, surface electromyographic biofeedback, and vestibulectomy in the treatment of dyspareunia resulting from vulvar vestibulitis. Pain 2001, 91, 297–306. [Google Scholar] [CrossRef]
- Fugl-Meyer, K.S.; Boham-Starke, N.; Petersen, C.D.; Fugl-Meyer, A.; Parish, S.; Giraldi, A. Standard Operating Procedures for Female Genital Sexual Pain. J. Sex. Med. 2013, 10, 83–93. [Google Scholar] [CrossRef]
- Mandal, D.; Nunns, D.; Byrne, M.; McLelland, J.; Rani, R.; Cullimore, J.; Bansal, D.; Brackenbury, F.; Kirtschig, G.; Wier, M.; et al. Guidelines for the management of vulvodynia. Br. J. Dermatol. 2010, 162, 1180–1185. [Google Scholar] [CrossRef]
- Reed, B.D.; Caron, A.M.; Gorenflo, D.W.; Haefner, H.K. Treatment of vulvodynia with tricyclic antidepressants: Efficacy and associated factors. Obstet. Gynecol. Surv. 2007, 62, 26–27. [Google Scholar] [CrossRef]
- Zolnoun, D.; Hartmann, K.; Lamvu, G.; As-Sanie, S.; Maixner, W.; Steege, J. A conceptual model for the pathophysiology of vulvar vestibulitis syndrome. Obstet. Gynecol. Surv. 2006, 61, 395–401. [Google Scholar] [CrossRef]
- Argoff, C.E.; Albrecht, P.; Irving, G.; Rice, F. Multimodal analgesia for chronic pain: Rationale and future directions. Pain Med. 2009, 10, S53–S66. [Google Scholar] [CrossRef]
- Al-Abbadey, M.; Liossi, C.; Curran, N.; Schoth, D.E.; Graham, C.A. Treatment of female sexual pain disorders: A systematic review. J. Sex Marital Ther. 2016, 42, 99–142. [Google Scholar] [CrossRef]
- Bohm-Starke, N.; Rylander, E. Surgery for localized, provoked vestibulodynia: A long-term follow-up study. J. Reprod. Med. 2008, 53, 83–89. [Google Scholar] [PubMed]
- Goldstein, A.; Klingman, D.; Christopher, K.; Johnson, C.; Marinoff, S. Surgical treatment of vulvar vestibulitis syndrome: Outcome assessment derived from a postoperative questionnaire. J. Sex. Med. 2006, 3, 923–931. [Google Scholar] [CrossRef] [PubMed]
- FitzGerald, M.P.; Anderson, R.U.; Potts, J.; Payne, C.K.; Peters, K.M.; Clemens, Q.; Kotarino, R.; Fraser, L.; Cosby, A.; Fortman, C.; et al. Randomized multicenter feasibility trial of myofascial physical therapy for the treatment of urological chronic pelvic pain syndromes. J. Urol. 2009, 182, 570–580. [Google Scholar] [CrossRef]
- Rosenbaum, T.Y.; Owens, A. The role of pelvic floor physical therapy in treatment of pelvic and genital pain related sexual dysfunction. J. Sex. Med. 2008, 5, 513–523. [Google Scholar] [CrossRef]
- Sadownick, L. Etiology, diagnosis, and clinical management of vulvodynia. Int. J. Women Health 2014, 6, 437–449. [Google Scholar] [CrossRef]
- Weijmar-Schultz, W.C.M.; Gianotten, W.L.; Van Der Meijden, W.I.; Van De Wiel, H.B.M.; Blindeman, L.; Chadha, S.; Drogendijk, A.C. Behavioral approach with or without surgical intervention for the vulvar vestibulitis syndrome: A prospective randomized and non-randomized study. J. Psychosom. Obstet. Gynecol. 1996, 17, 143–148. [Google Scholar] [CrossRef]
- King, H.H. Manual Therapy May Benefit Women With Interstitial Cystitis and Pelvic Floor Pain. J. Am. Osteopath. Assoc. 2013, 113, 360–361. [Google Scholar]
- Ailliet, L.; Rubinstein, S.M.; Knol, D. Somatization is associated with worse outcome in a chiropractic patient population with neck pain and low back pain. Man. Ther. 2016, 21, 170–176. [Google Scholar] [CrossRef]
- Kotarinos, R.K. Pelvic floor physical therapy in urogynecologic disorders. Curr. Women Health Rep. 2003, 3, 334–339. [Google Scholar]
- Kotarinos, R.K. Myofascial Pelvic Pain: Rationale and Treatment. Curr. Bladder Dysfunct. Rep. 2015, 10, 87–94. [Google Scholar] [CrossRef]
- Thomten, J.; Karlsson, A. Psychological factors in genital pain: The role of fear avoidance, pain catastrophizing and anxiety sensitivity among women living in sweden. Scand. J. Pain 2014, 5, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Bruckenthal, P. Chronic pelvic pain: Approaches to diagnosis and treatment. Pain Manag. Nurs. 2010, 12, S4–S10. [Google Scholar] [CrossRef]
- George, S.E.; Clinton, S.C.; Borello-France, D.F. Physical therapy management of female chronic pelvic pain: Anatomic considerations. Clin. Anat. 2013, 26, 77–88. [Google Scholar] [CrossRef] [PubMed]
- Glazer, H.; Rodke, G.; Swencions, C.; Hertz, R.; Alexander, W. Treatment of Vulvar Vestibulitis Syndrome with Electromyographic Biofeedback of Pelvic Floor Musculature. Obstet. Gynecol. Surv. 1995, 50, 658–659. [Google Scholar] [CrossRef]
- Anderson, R.U.; Sawyer, T.; Wise, D.; Morey, A.; Nathanson, B.H.; Krieger, J.N. Painful myofascial trigger points and pain sites in men with chronic prostatitis/chronic pelvic pain syndrome. J. Urol. 2009, 182, 2753–2758. [Google Scholar] [CrossRef] [PubMed]
- Tu, F.F.; Holt, J.; Gonzales, J.; Fitzgerald, C.M. Physical therapy evaluation of patients with chronic pelvic pain: A controlled study. Gen. Gynecol. 2008, 198, 272–277. [Google Scholar] [CrossRef]
- Peters, K.M.; Carrico, D.; Kalinowski, S.E.; Ibrahim, I.A. Prevalence of pelvic floor dysfunction in patients with interstitial cystitis. Ault Urol. 2007, 70, 16–20. [Google Scholar] [CrossRef]
- Adams, N.; Field, L. Pain management 1: Psychological and social aspects of pain. Br. J. Nurs. 2001, 10, 903–911. [Google Scholar] [CrossRef]
- Sullivan, M.J.L.; Bishop, S.; Pivik, J. The pain catastophizing scale: Development and validation. Psychol. Assess. 1995, 7, 524–532. [Google Scholar] [CrossRef]
- Sullivan, M.J.L.; Thorn, B.; Haythornthwaite, J.A.; Keefe, F.; Martin, M.; Bradley, L.A.; Lefebvre, J. Theoretical perspectives on relation between catastrophizing and pain. Clin. J. Pain 2001, 17, 52–64. [Google Scholar] [CrossRef] [PubMed]
- Quartana, P.J.; Campbell, C.M.; Edwards, R.R. Pain catastrophizing: A critical review. Expert Rev. Neurother. 2009, 9, 745–758. [Google Scholar] [CrossRef]
- Lowenstein, L.; Fitzgerald, M.P.; Kenton, K.; Hachett Durazo-Arvizu, R.; Mueller, E.R.; Goldman, K.; Brubaker, L. Evaluation of urgency in women with a validated urgency, severity and impact questionnaire (USIQ). Int. Urogynecol. 2009, 20, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Tripp, D.A.; Curtis, N.; Fitzgerald, M.P.; Mayer, R.; Stechyson, N. Sexual functioning, catastrophizing, depression, and pain, as predictors of quality of life in women with interstitial cystitis/painful bladder syndrome. Female Urol. 2009, 75, 987–992. [Google Scholar] [CrossRef] [PubMed]
- Granot, M.; Lavee, Y. Psychological factors associated with perception of experimental pain in vulvar vestibulitis syndrome. J. Sex Marital Ther. 2005, 31, 285–302. [Google Scholar] [CrossRef] [PubMed]
- Curtis-Nickel, J.; Shoskes, D.; Irvin-Bird, K. Clinical Phenotyping of Women with Interstitial Cystitis/Painful Bladder Syndrome: A Key to Classification and Potentially Improved Management. J. Urol. 2009, 182, 155–160. [Google Scholar] [CrossRef]
- Kuile, M.M.; Weijenborg, P.T.M.; Spinhoven, P. Sexual functioning in women with chronic pelvic pain: The role of anxiety and depression. J. Sex. Med. 2010, 7, 1901–1910. [Google Scholar] [CrossRef]
- Vlayen, J.W.S.; Linton, S.J. Fear avoidance and its consequences in chronic musculoskeletal pain: A state of the art. Pain 2002, 85, 317–322. [Google Scholar] [CrossRef]
- Payne, K.A.; Binik, Y.M.; Pukall, C.F.; Thaler, L.; Amsel, R.; Khalife, S. Effects of sexual arousal on genital and nongenital sensation: A comparison of women with vulvar vestibulitis syndrome and healthy controls. Arch. Sex. Behav. 2007, 36, 289–300. [Google Scholar] [CrossRef]
- Bair, M.J.; Robinson, R.L.; Katon, W.; Kroenke, K. Depression and pain comorbidity. Arch. Intern. Med. 2003, 163, 2433–2445. [Google Scholar] [CrossRef]
- Katon, W.; Lin, E.H.B.; Kroenke, K. The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Gen. Hosp. Psychiatry 2007, 29, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Romano, A.P.M.S.; Gorayeb, R.; Romano, S.; Poli-Neto, O.B.; Dos Reis, C.; Rosa e Silva, J.C.; Nogueira, A.A. High levels of anxiety and depression have a negative effect on quality of life of women with chronic pelvic pain. Int. J. Clin. Pract. 2009, 63, 707–711. [Google Scholar] [CrossRef] [PubMed]
- Miller-Matero, L.R.; Saulino, C.; Clark, S.; Bugensk, M.; Eshelman, A.; Eisenstein, D. When treating the pain is not enough: A multidisciplinary approach for chronic pelvic pain. Arch. Women Ment. Health 2016, 19, 349–354. [Google Scholar] [CrossRef] [PubMed]
- Birket-Smith, M. Somatization and chronic pain. Acta Anaesthesiol. Scand. 2001, 45, 1114–1120. [Google Scholar] [CrossRef]
- Wilson, L.; Dworkin, S.F.; Whitney, C.; LeResche, L. Somatization and pain dispersion in chronic temporomandibular disorder pain. Pain 1994, 57, 55–61. [Google Scholar] [CrossRef]
- Van Oudenhove, L.; Tornblom, H.; Storsud, S.; Tack, J.; Simren, M. Depression and Somatization are Associated with Increased Postprandial Symptoms in Patients with Irritable Bowel Syndrome. Gastroenterology 2016, 150, 866–874. [Google Scholar] [CrossRef]
- Sertel-Berk, H.O. The biopsychosocial factors that serve as predictors for the outcome of surgical modalities for chronic pain. AGRI 2010, 22, 93–97. [Google Scholar]
| Potential Medication | Action Mechanisms | Therapeutics Intervention |
|---|---|---|
| Tricyclic antidepressants; sodium pentosapolysulfate | Inhibit reuptake of noradrenaline and serotonin | Improves pain regulation; improves functioning of the downward pain-processing conduits |
| Resiniferatoxin; capsaicin | Bind to nerve-ending receptors and desensitize pain fibers | Delays nerve conduction velocity |
| Botulinum toxin | Inhibits the secretion of inflammatory agents such as substance p and nerve growth factors; inhibits production of prostaglandins | Administered due to the assumption that CPPS has an inflammatory source; prevents higher tonus of pelvic muscles |
| Hormone therapy | Releases hormone agonists | Some success in response to hormone therapy; pain is related to the menstrual cycle and hormonal changes |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grinberg, K.; Sela, Y.; Nissanholtz-Gannot, R. New Insights about Chronic Pelvic Pain Syndrome (CPPS). Int. J. Environ. Res. Public Health 2020, 17, 3005. https://doi.org/10.3390/ijerph17093005
Grinberg K, Sela Y, Nissanholtz-Gannot R. New Insights about Chronic Pelvic Pain Syndrome (CPPS). International Journal of Environmental Research and Public Health. 2020; 17(9):3005. https://doi.org/10.3390/ijerph17093005
Chicago/Turabian StyleGrinberg, Keren, Yael Sela, and Rachel Nissanholtz-Gannot. 2020. "New Insights about Chronic Pelvic Pain Syndrome (CPPS)" International Journal of Environmental Research and Public Health 17, no. 9: 3005. https://doi.org/10.3390/ijerph17093005
APA StyleGrinberg, K., Sela, Y., & Nissanholtz-Gannot, R. (2020). New Insights about Chronic Pelvic Pain Syndrome (CPPS). International Journal of Environmental Research and Public Health, 17(9), 3005. https://doi.org/10.3390/ijerph17093005





