Environmental Correlates of Reaching a Centenarian Age: Analysis of 144,665 Deaths in Washington State for 2011−2015
Abstract
1. Introduction
2. Methods
2.1. Outcome Variable
2.2. Explanatory Variables
2.2.1. Demographics Variable
2.2.2. Contextual Variables
3. Statistical Analysis
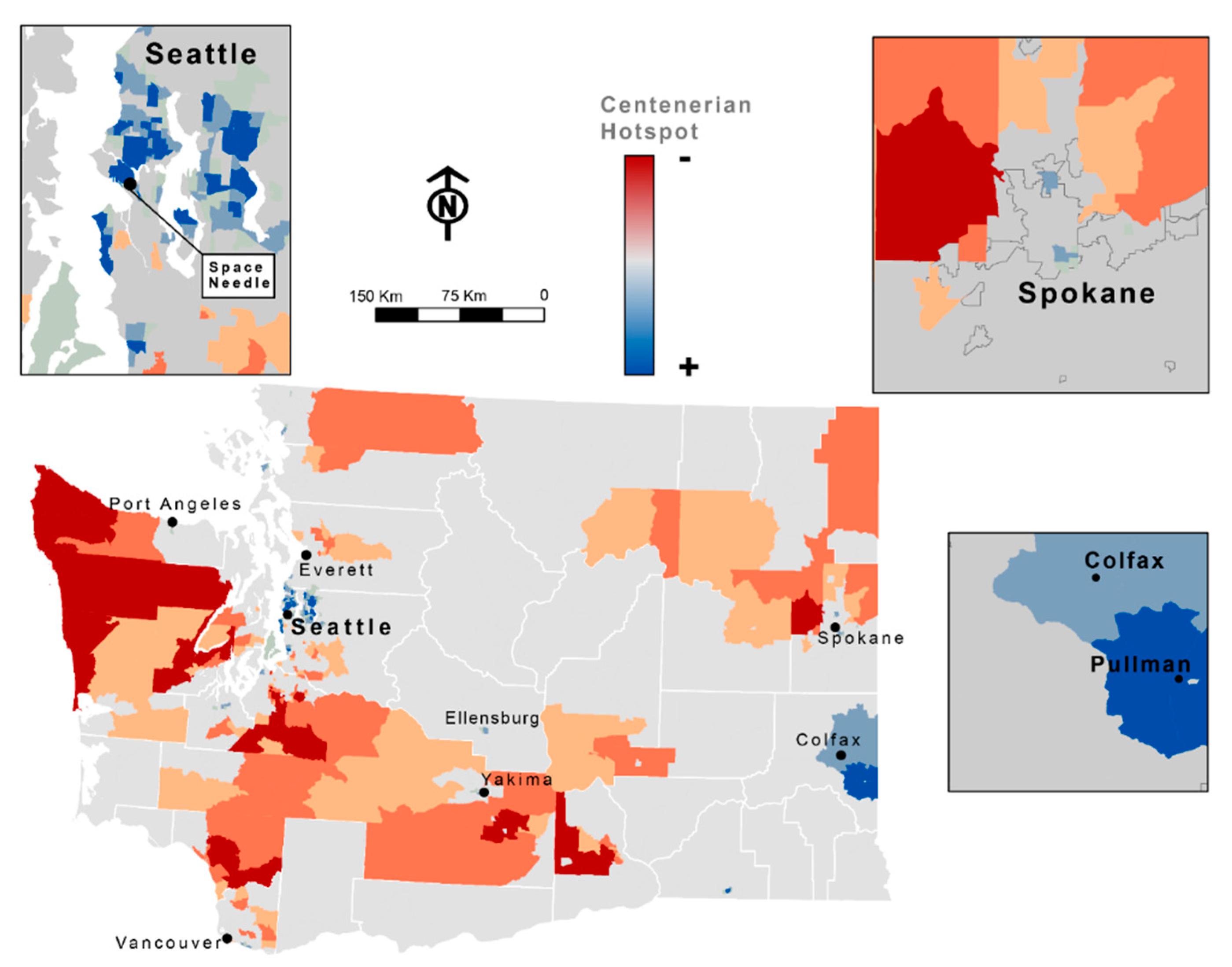
Spatial Analysis and Mapping
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World’s Centenarian Population Projected to Grow Eightfold by 2050. Available online: https://www.pewresearch.org/fact-tank/2016/04/21/worlds-centenarian-population-projected-to-grow-eightfold-by-2050/ (accessed on 21 April 2016).
- Xu, J. Mortality Among Centenarians in the United States, 2000−2014. Nchs Data Brief No. 233 2016, 1–8. [Google Scholar]
- Christensen, K.; Vaupel, J.W. Determinants of longevity: Genetic, environmental and medical factors. J. Intern. Med. 1996, 240, 333–341. [Google Scholar] [CrossRef] [PubMed]
- Mortality in the United States: Past, Present, and Future. Penn Wharton University of Pennsylvania: Philadelphia, PA, USA, 27 June 2016. Available online: https://budgetmodel.wharton.upenn.edu/issues/2016/1/25/mortality-in-the-united-states-past-present-and-future (accessed on 21 March 2020).
- Shadyab, A.H.; Lacroix, A.Z. Genetic factors associated with longevity: A review of recent findings. Ageing Res. Rev. 2015, 19, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Why Study Centenarians? An Overview. The New England Centenarian Study. Boston Medical Center: Boston, MA, USA. Available online: https://www.bumc.bu.edu/centenarian/overview/ (accessed on 21 March 2020).
- WHO. What is Healthy Ageing? Available online: https://www.who.int/ageing/healthy-ageing/en/ (accessed on 29 October 2019).
- Kim, J.I.; Kim, G. Factors affecting the survival probability of becoming a centenarian for those aged 70, based on the human mortality database: Income, health expenditure, telephone, and sanitation. BMC Geriatr. 2014, 14, 113. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, C.; Bonafè, M. Centenarians as a model for healthy aging. Biochem. Soc. Trans. 2003, 31, 457–461. [Google Scholar] [CrossRef] [PubMed]
- Silva, V.D.L.; Cesse, E.; Ângela, P.; Albuquerque, M.D.F.P.M.D. Social determinants of death among the elderly: A systematic literature review. Rev. Bras. Epidemiol 2014, 17 (Suppl. 2), 178–193. [Google Scholar] [CrossRef]
- Death Data - Vital Statistics: Washington State Department of Health: Tumwater, WA, USA. Available online: https://www.doh.wa.gov/DataandStatisticalReports/HealthStatistics/Death (accessed on 9 November 2019).
- Krieger, N.; Rehkopf, D.H.; Chen, J.T.; Waterman, P.D.; Marcelli, E.; Kennedy, M. The Fall and Rise of US Inequities in Premature Mortality: 1960–2002. Plos Med. 2008, 5, e46. [Google Scholar] [CrossRef]
- Weinstein, M.C. Health and the War on Poverty: A Ten-Year Appraisal. Med. Care. 1980, 18, 124. [Google Scholar] [CrossRef]
- Kawachi, I.; Adler, N.E.; Dow, W.H. Money, schooling, and health: Mechanisms and causal evidence. Ann. Ny Acad. Sci. 2010, 1186, 56–68. [Google Scholar] [CrossRef]
- Gardner, J.W.; Sanborn, J.S. Years of Potential Life Lost (YPLL)—What Does it Measure? Epidemiology 1990, 1, 322–329. [Google Scholar] [CrossRef]
- Singh, G.K. Area Deprivation and Widening Inequalities in US Mortality, 1969–1998. Am. J. Public Health 2003, 93, 1137–1143. [Google Scholar] [CrossRef] [PubMed]
- Knighton, A.J.; Savitz, L.; Belnap, T.; Stephenson, B.; Vanderslice, J. Introduction of an Area Deprivation Index Measuring Patient Socioeconomic Status in an Integrated Health System: Implications for Population Health. eGEMs (Gener. Évid. Methods Improv. Patient Outcomes) 2016, 4, 1238. [Google Scholar]
- Kind, A.J.; Buckingham, W.R. Making Neighborhood-Disadvantage Metrics Accessible—The Neighborhood Atlas. N. Engl. J. Med. 2018, 378, 2456–2458. [Google Scholar] [CrossRef] [PubMed]
- Walkability Index. United States Environmental Protection Agency. Available online: https://edg.epa.gov/metadata/catalog/search/resource/details.page?uuid=%7B251AFDD9-23A7-4068-9B27-A3048A7E6012%7D (accessed on 10 November 2019).
- Schuurman, N.; Bérubé, M.; Crooks, V. Measuring potential spatial access to primary health care physicians using a modified gravity model. Can. Geogr. 2010, 54, 29–45. [Google Scholar] [CrossRef]
- AMA Physician Masterfile. American Medical Association: Chicago, IL, USA. Available online: https://www.ama-assn.org/practice-management/masterfile/ama-physician-masterfile (accessed on 21 March 2020).
- Amiri, S.; Espenschied, J.R.; Roll, J.M.; Amram, O. Access to Primary Care Physicians and Mortality in Washington State: Application of a 2-Step Floating Catchment Area. J. Rural. Health. 2019, 35, 1–8. [Google Scholar] [CrossRef]
- Rural-Urban Commuting Area Codes (RUCAs). United States Department of Agriculture: Washington, D.C., USA. Last updated 24 October 2019. Available online: https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/ (accessed on 10 November 2019).
- Particulate Matter (PM) Basics. United States Environmental Protection Agency. Available online: https://www.epa.gov/pm-pollution/particulate-matter-pm-basics (accessed on 21 March 2020).
- What is Open Space/Green Space? Available online: https://www3.epa.gov/region1/eco/uep/openspace.html (accessed on 21 March 2020).
- Dudley, W.N.; Wickham, R.; Coombs, M.N. An Introduction to Survival Statistics: Kaplan-Meier Analysis. J. Adv. Pract. Oncol. 2016, 7, 91–100. [Google Scholar]
- Kishore, J.; Goel, M.K.; Khanna, P. Understanding survival analysis: Kaplan-Meier estimate. Int. J. Ayurveda Res. 2010, 1, 274–278. [Google Scholar] [CrossRef]
- Press, E. Linear Referencing in ArcGIS: ArcGIS 9; Esri Press: Redlands, CA, USA, 2005. [Google Scholar]
- Grant, T.L.; Edwards, N.; Sveistrup, H.; Andrew, C.; Egan, M. Neighborhood Walkability: Older People’s Perspectives from Four Neighborhoods in Ottawa, Canada. J. Aging Phys. Act. 2010, 18, 293–312. [Google Scholar] [CrossRef]
- Calise, T.V.; Chow, W.; Ryder, A.; Wingerter, C. Food Access and Its Relationship to Perceived Walkability, Safety, and Social Cohesion. Health Promot. Pract. 2019, 20, 858–867. [Google Scholar] [CrossRef]
- Cao, X.; Mokhtarian, P.L.; Handy, S. Neighborhood Design and the Accessibility of the Elderly: An Empirical Analysis in Northern California. Int. J. Sustain. Transp. 2010, 4, 347–371. [Google Scholar] [CrossRef]
- Litman, T.A. Economic Value of Walkability; Victoria Transit Policy Institute: Victoria, BC, Canada, 2018. [Google Scholar]
- Smart Location Mapping. Available online: https://www.epa.gov/smartgrowth/smart-location-mapping (accessed on 10 November 2019).
- Creatore, M.I.; Glazier, R.; Moineddin, R.; Fazli, G.S.; Johns, A.; Gozdyra, P.; Matheson, F.I.; Kaufman-Shriqui, V.; Rosella, L.C.; Manuel, D.G.; et al. Association of Neighborhood Walkability With Change in Overweight, Obesity, and Diabetes. JAMA 2016, 315, 2211. [Google Scholar] [CrossRef] [PubMed]
- Reis, R.S.; Hino, A.A.F.; Rech, C.R.; Kerr, J.; Hallal, P.C. Walkability and physical activity: Findings from Curitiba, Brazil. Am. J. Prev. Med. 2013, 45, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Sallis, J.F.; Saelens, B.E.; Frank, L.D.; Conway, T.L.; Slymen, N.J.; Cain, K.; Chapman, J.E.; Kerr, J. Neighborhood built environment and income: Examining multiple health outcomes. Soc. Sci. Med. 2009, 68, 1285–1293. [Google Scholar] [CrossRef] [PubMed]
- King, A.C.; Sallis, J.F.; Frank, L.D.; Saelens, B.E.; Cain, K.; Conway, T.L.; Chapman, J.E.; Ahn, D.K.; Kerr, J. Aging in neighborhoods differing in walkability and income: Associations with physical activity and obesity in older adults. Soc. Sci. Med. 2011, 73, 1525–1533. [Google Scholar] [CrossRef]
- James, P.; Kioumourtzoglou, M.-A.; Hart, J.E.; Banay, R.F.; Kloog, I.; Laden, F. Interrelationships Between Walkability, Air Pollution, Greenness, and Body Mass Index. Epidemiology 2017, 28, 780–788. [Google Scholar] [CrossRef]
- Garrett, M.; Poulain, M. Geography of Aging: The Science of Belonging. J. Psychol. 2018, 5, 73–83. [Google Scholar]
- Glicksman, A.; Ring, L.; Kleban, M.H.; Hoffman, C. Is “Walkability” A Useful Concept for Gerontology? J. Hous. Elder. 2013, 27, 241–254. [Google Scholar] [CrossRef]
- Buettner, D.; Skemp, S. Blue Zones: Lessons from the World’s Longest Lived. Am. J. Lifestyle Med. 2016, 10, 318–321. [Google Scholar] [CrossRef]
- Masters, R.K.; Hummer, R.A.; Powers, D.A. Educational Differences in U.S. Adult Mortality: A Cohort Perspective*. Am. Sociol. Rev. 2012, 77, 548–572. [Google Scholar] [CrossRef]
- Montez, J.K.; Hummer, R.A.; Hayward, M.D. Educational Attainment and Adult Mortality in the United States: A Systematic Analysis of Functional Form. Demography 2012, 49, 315–336. [Google Scholar] [CrossRef]
- Hayward, M.D.; Hummer, R.A.; Sasson, I. Trends and group differences in the association between educational attainment and U.S. adult mortality: Implications for understanding education’s causal influence. Soc. Sci. Med. 2015, 127, 8–18. [Google Scholar] [CrossRef] [PubMed]
- Ross, C.E.; Wu, C.-L. The Links between Education and Health. Am. Sociol. Rev. 1995, 60, 719. [Google Scholar] [CrossRef]
- Hummer, R.A.; Hernandez, E.M. The Effect of Educational Attainment on Adult Mortality in the United States*. Popul. Bull. 2013, 68, 1–16. [Google Scholar] [PubMed]
- Kitagawa, E.M.; Hauser, P.M. Differential Mortality in the United States. In Differential Mortality in the United States: A Study in Socioeconomic Epidemiology; Harvard University Press: Cambridge, MA, USA, 1973. [Google Scholar]
- Feldman, J.; Makuc, D.M.; Kleinman, J.C.; Cornoni-Huntley, J. National trends in educational differentials in mortality. Am. J. Epidemiol. 1989, 129, 919–933. [Google Scholar] [CrossRef] [PubMed]
- Pappas, G.; Queen, S.; Hadden, W.; Fisher, G. The Increasing Disparity in Mortality between Socioeconomic Groups in the United States, 1960 and 1986. N. Engl. J. Med. 1993, 329, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Preston, S.H.; Elo, I.T. Are Educational Differentials in Adult Mortality Increasing in the United States? J. Aging Health 1995, 7, 476–496. [Google Scholar] [CrossRef] [PubMed]
- Berkson, J. Mortality and Marital Status. Reflections on the Derivation of Etiology from Statistics. Am. J. Public Health Nations Health 1962, 52, 1318–1329. [Google Scholar] [CrossRef]
- Kaplan, R.M.; Kronick, R.G. Marital status and longevity in the United States population. J. Epidemiol. Commun. Health 2006, 60, 760–765. [Google Scholar] [CrossRef]
- Burgoa, M.; Regidor, E.; Rodriguez, C.; Gutierrez-Fisac, J.L. Mortality by cause of death and marital status in Spain. Eur. J. Public Health 1998, 8, 37–42. [Google Scholar] [CrossRef]
- Goldman, N.; Korenman, S.; Weinstein, R. Marital status and health among the elderly. Soc. Sci. Med. 1995, 40, 1717–1730. [Google Scholar] [CrossRef]
- Hu, Y.; Goldman, N. Mortality Differentials by Marital Status: An International Comparison. Demography 1990, 27, 233–250. [Google Scholar] [CrossRef] [PubMed]
- Robards, J.; Evandrou, M.; Falkingham, J.; Vlachantoni, A. Marital status, health and mortality. Maturitas 2012, 73, 295–299. [Google Scholar] [CrossRef] [PubMed]
- Williams, K.; Umberson, D. Marital status, marital transitions, and health: A gendered life course perspective. J. Health Soc. Behav. 2004, 45, 81–98. [Google Scholar] [CrossRef]
- Temby, O.; Smith, K.R. The association between adult mortality risk and family history of longevity: The moderating effects of socioeconomic status. J. Biosoc. Sci. 2014, 46, 703–716. [Google Scholar] [CrossRef] [PubMed]
- Gu, D.; Yang, F.; Sautter, J.M. Socioeconomic status as a moderator between frailty and mortality at old ages. Bmc Geriatr. 2016, 16, 151. [Google Scholar]
- Lantz, P.M.; House, J.S.; Lepkowski, J.M.; Williams, D.R.; Mero, R.P.; Chen, J. Socioeconomic factors, health behaviors, and mortality: Results from a nationally representative prospective study of US adults. JAMA 1998, 279, 1703–1708. [Google Scholar] [CrossRef]
- Ettner, S.L. New evidence on the relationship between income and health. J. Health Econ. 1996, 15, 67–85. [Google Scholar] [CrossRef]
- Kawachi, I.; Kennedy, B.P. Income inequality and health: Pathways and mechanisms. Health Serv. Res. 1999, 34, 215–227. [Google Scholar]
- Marmot, M. The Influence Of Income On Health: Views Of An Epidemiologist. Health Aff. (Millwood). 2002, 21, 31–46. [Google Scholar] [CrossRef]
- Lantz, P.M.; Golberstein, E.; House, J.S.; Morenoff, J. Socioeconomic and behavioral risk factors for mortality in a national 19-year prospective study of U.S. adults. Soc. Sci. Med. 2010, 70, 1558–1566. [Google Scholar] [CrossRef]
- Ulf, G.G.; Johannesson, M. Absolute Income, Relative Income, Income Inequality, and Mortality. J. Hum. Resour. 2004, 39, 228–247. [Google Scholar]
- Ortiz-Ospina, E.; Beltekian, D. Why do women live longer than men? Available online: https://ourworldindata.org/why-do-women-live-longer-than-men (accessed on 10 November 2019).
- Goldin, C.; Lleras-Muney, A. XX > XY?: The changing female advantage in life expectancy. J. Health Econ. 2019, 67, 102224. [Google Scholar] [CrossRef]
- Schünemann, J.; Strulik, H.; Trimborn, T. The gender gap in mortality: How much is explained by behavior? J. Health Econ. 2017, 54, 79–90. [Google Scholar] [CrossRef] [PubMed]
- Elo, I.T.P.; Samuel, H. Racial and Ethnic Differences in Mortality at Older Ages. In National Research Council (US) Committee on Population; National Academies Press (US): Washington, DC, USA, 1997. [Google Scholar]
- Beydoun, M.A.; Beydoun, H.A.; Mode, N.; Dore, G.A.; Canas, J.A.; Eid, S.M.; Zonderman, A. Racial disparities in adult all-cause and cause-specific mortality among us adults: Mediating and moderating factors. BMC Public Health 2016, 16, 1113. [Google Scholar] [CrossRef] [PubMed]
- Hummer, R.A.; Chinn, J.J. Race/Ethnicity and U.S. Adult Mortality: Progress, Prospects, and New Analyses. Du Bois Rev. 2011, 8, 5–24. [Google Scholar] [CrossRef] [PubMed]
- Day, J.C.; Hays, D.; Smith, A.A. Glance at the Age Structure and Labor Force Participation of Rural America. Available online: https://www.census.gov/newsroom/blogs/random-samplings/2016/12/a_glance_at_the_age.html (accessed on 10 November 2019).
- National Center for Health Statistics (US). Health, United States, 2010 with Special Feature on Death and Dying; Office of the Secretary: Pennsylvania, DC, USA, 2011.
- Singh, G.K.; Siahpush, M. Widening Rural–Urban Disparities in All-Cause Mortality and Mortality from Major Causes of Death in the USA, 1969–2009. J. Urban Health 2014, 91, 272–292. [Google Scholar] [CrossRef]
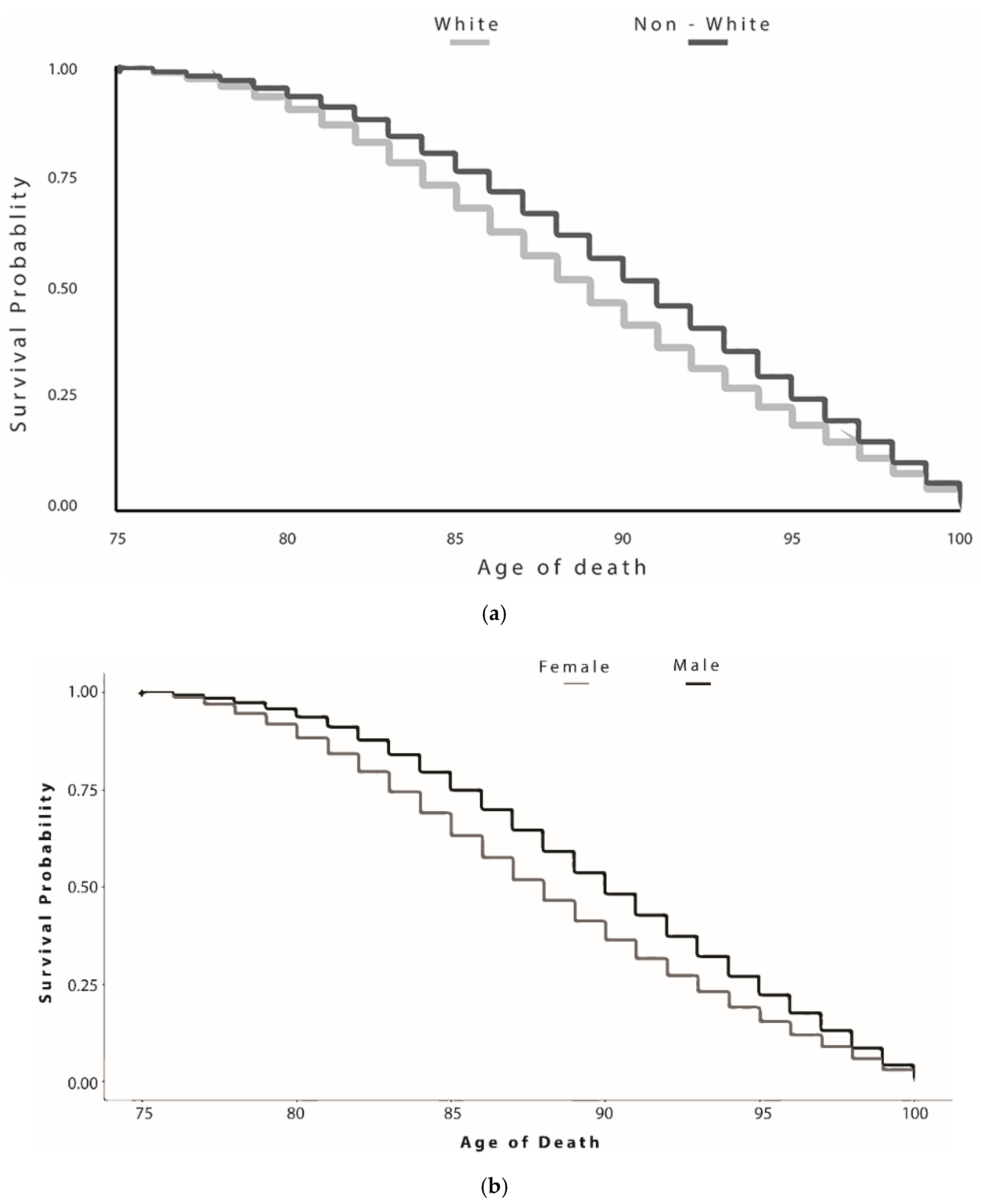
| Characteristics | All Decedents (144,665 (98.1%)) | 75−99 Years Old (141,967 (98.1%)) | ≥100 Years Old (2698 (1.8%)) | p-Value |
|---|---|---|---|---|
| Demographic Variables | ||||
| Age (Median (IQR) | 86 (81−91) | 86 (81−91) | 101 (100−102) | <0.001 |
| Gender (no. (%)) | ||||
| Female | 81,168 (56.1) | 79,026 (55.7) | 2142 (79.4) | <0.001 |
| Male | 63,497 (43.9) | 62,941 (44.3) | 556 (20.6) | |
| Race (no. (%)) | ||||
| Nonwhite | 9873 (6.8) | 9721 (6.8) | 152 (5.6) | 0.01 |
| White | 134,414 (92.9) | 131,872 (92.9) | 2542 (94.2) | |
| NA | 378 (0.3) | 374 (0.3) | 4 (0.1) | |
| Marital Status (no. (%)) | ||||
| Married | 47,996 (33.2) | 47,877 (33.7) | 119 (4.4) | <0.001 |
| Never Married | 3951 (2.7) | 3878 (2.7) | 73 (2.7) | |
| Divorced or Separated | 15,771 (10.9) | 15,660 (11) | 111 (4.1) | |
| Widowed | 76,575 (52.9) | 74,185 (52.3) | 2390 (88.6) | |
| NA | 372 (0.3) | 367 (0.3) | 5 (0.2) | |
| Education Level (no. (%)) | ||||
| No High School Diploma | 24,094 (16.7) | 23,487 (16.5) | 607 (22.5) | <0.001 |
| High School Diploma | 82,082 (56.7) | 80,660 (56.8) | 1422 (52.7) | |
| Associate Degree or Above | 36,915 (25.5) | 36,273 (25.6) | 642 (23.8) | |
| NA | 1574 (1.1) | 1547 (1.1) | 27 (1) | |
| Contextual Variables | ||||
| Urban vs. Rural (no. (%)) | ||||
| Metropolitan Area | 122,314 (84.5) | 120,031 (84.5) | 2283 (84.6) | 0.96 |
| Micropolitan Area | 12,235 (8.5) | 12,005 (8.5) | 230 (8.5) | |
| Small Town or Rural | 10116 (7) | 9931 (7) | 185 (6.9) | |
| Access to Public Transportation (Median (IQR) | 0 (0−0.06) | 0 (0−0.06) | 0.02 (0−0.08) | <0.001 |
| Walkability (Median (IQR) | 9.83 (6.7−14) | 9.67 (6.5−14) | 10.83 (7.5−14.7) | <0.001 |
| Area deprivation index (Median (IQR) | 6 (3−8) | 6 (3−8) | 5 (3−8) | <0.001 |
| Access to primary care Physicians (Median (IQR) | 9.42 (6.9−12) | 9.41 (6.9−12) | 9.8 (7.1−12.4) | <0.001 |
| Percent of Working Age (Median (IQR) | 0.78 (0.8−0.8) | 0 (0−0.06) | 0.79 (0.8−0.8) | <0.001 |
| Greenspace (NDVI) (Median (IQR) | 0.52 (0.4−0.6) | 0.52 (0.4−0.6) | 0.5 (0.4−0.6) | <0.001 |
| Air Pollution (PM 2.5) (Median (IQR) | 6.6 (5.9−7.4) | 6.5 (5.9−7.4) | 6.7 (6−7.5) | <0.001 |
| Characteristics | Unadjusted HR (95%CI) | p-value | Adjusted HR (95%CI) | p-Value |
|---|---|---|---|---|
| Demographic Variables | ||||
| Gender | ||||
| Female | Reference | Reference | ||
| Male | 0.33 (0.30−0.36) | <0.001 | 0.56 (0.50−0.63) | <0.001 |
| Race | ||||
| White | Reference | Reference | ||
| Nonwhite | 0.81 (0.67−0.98) | 0.03 | 0.71 (0.58−0.87) | <0.001 |
| Marital Status | ||||
| Married | Reference | Reference | ||
| Never Married | 7.51 (5.61−10.06) | <0.001 | 6.44 (4.68−8.85) | <0.001 |
| Divorced or Separated | 2.85 (2.18−3.71) | <0.001 | 2.53 (1.89−3.39) | <0.001 |
| Widowed | 12.77 (10.64−15.34) | <0.001 | 9.72 (7.90−11.96) | <0.001 |
| Education Level | ||||
| No High School Diploma | Reference | Reference | ||
| High School Diploma | 0.68 (0.62−0.75) | <0.001 | 0.61 (0.55−0.68) | <0.001 |
| Associate Degree or Above | 0.69 (0.61−0.77) | <0.001 | 0.73 (0.64−0.84) | <0.001 |
| Contextual Variables | ||||
| Urban Versus Rural | ||||
| Metropolitan Area | Reference | Reference | ||
| Micropolitan Area | 1.01 (0.87−1.17) | 0.9 | 0.93 (0.74−1.17) | 0.5 |
| Small Town or Rural | 0.98 (0.82−1.16) | 0.8 | 0.43 (0.21−0.88) | 0.02 |
| Access to Public Transportation | 2.14 (1.09−4.23) | 0.03 | 0.73 (0.33−1.58) | 0.4 |
| Walkability | 1.04 (1.03−1.06) | <0.001 | 1.03 (1.01−1.05) | <0.001 |
| Area Deprivation Index (ADI) | 0.97 (0.96−0.99) | 0.006 | 0.96 (0.94−0.98) | <0.001 |
| Access to Primary Care Physicians | 1.04 (1.02−1.05) | <0.001 | 0.99 (0.96−1.01) | 0.3 |
| Percent Working Age | 15.18 (6.69−34.45) | <0.001 | 13.02 (5.28−32.09) | <0.001 |
| Greenspace (NDVI) | 0.47 (0.33−0.66) | <0.001 | 0.85 (0.48−1.53) | 0.6 |
| Air Pollution (PM2.5) | 1.07 (1.03−1.12) | 0.002 | 0.99 (0.93−1.05) | 0.6 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bhardwaj, R.; Amiri, S.; Buchwald, D.; Amram, O. Environmental Correlates of Reaching a Centenarian Age: Analysis of 144,665 Deaths in Washington State for 2011−2015. Int. J. Environ. Res. Public Health 2020, 17, 2828. https://doi.org/10.3390/ijerph17082828
Bhardwaj R, Amiri S, Buchwald D, Amram O. Environmental Correlates of Reaching a Centenarian Age: Analysis of 144,665 Deaths in Washington State for 2011−2015. International Journal of Environmental Research and Public Health. 2020; 17(8):2828. https://doi.org/10.3390/ijerph17082828
Chicago/Turabian StyleBhardwaj, Rajan, Solmaz Amiri, Dedra Buchwald, and Ofer Amram. 2020. "Environmental Correlates of Reaching a Centenarian Age: Analysis of 144,665 Deaths in Washington State for 2011−2015" International Journal of Environmental Research and Public Health 17, no. 8: 2828. https://doi.org/10.3390/ijerph17082828
APA StyleBhardwaj, R., Amiri, S., Buchwald, D., & Amram, O. (2020). Environmental Correlates of Reaching a Centenarian Age: Analysis of 144,665 Deaths in Washington State for 2011−2015. International Journal of Environmental Research and Public Health, 17(8), 2828. https://doi.org/10.3390/ijerph17082828






