Relationship between Individual Social Capital and Functional Ability among Older People in Anhui Province, China
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Collection
2.2. Measures
2.2.1. Measurement of Functional Disability
2.2.2. Measurement of Social Capital
2.2.3. Measurement of other Variables
2.3. Statistical Analysis
3. Results
3.1. Results of Descriptive Analysis
3.2. Results of Logistic Analysis
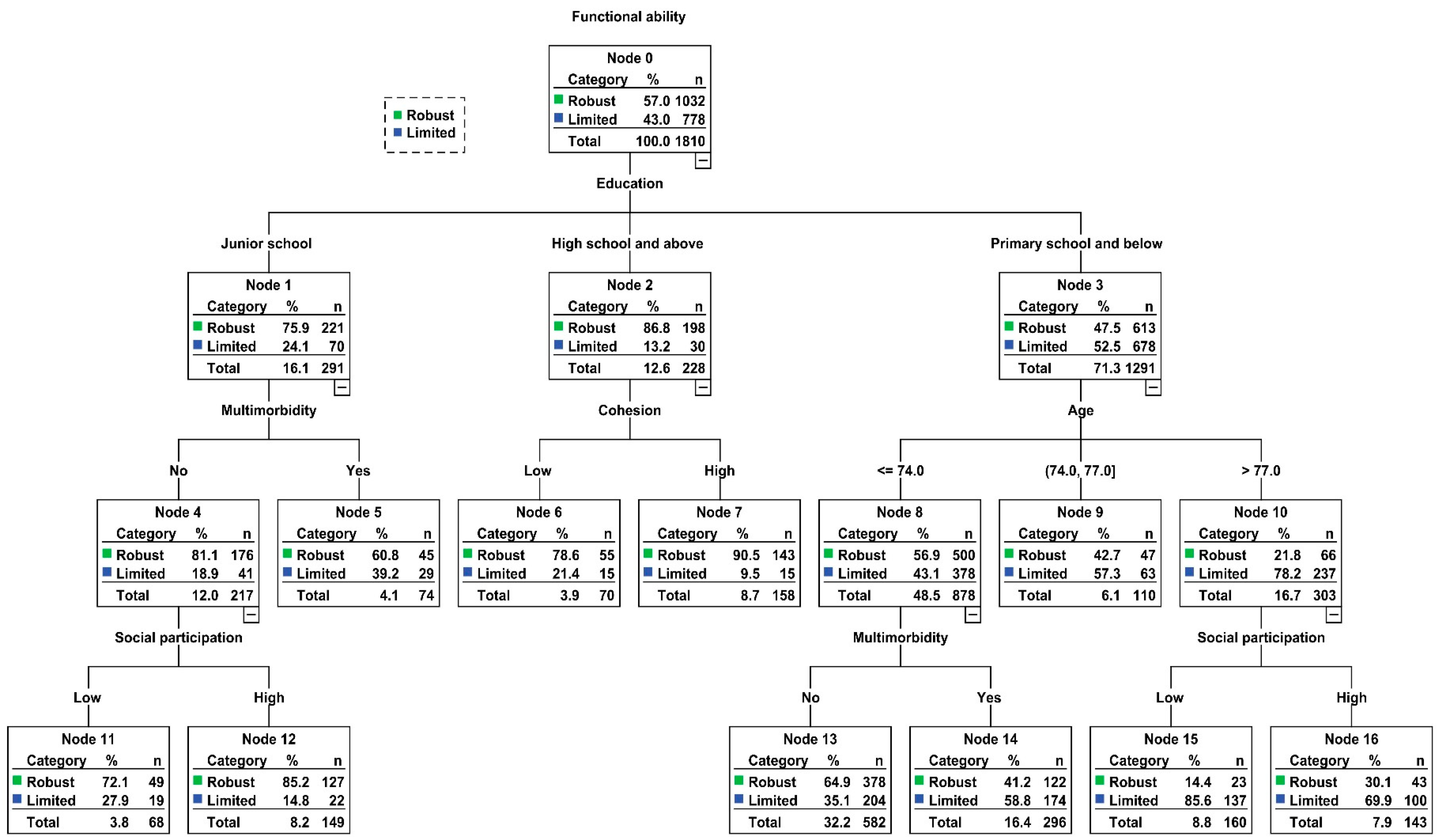
3.3. Results of Classification and Regression Tree Model
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Beard, J.R.; Bloom, D.E. Towards a comprehensive public health response to population ageing. Lancet (London, England) 2015, 385, 658–661. [Google Scholar] [CrossRef]
- Bartels, S.J. Why collaborative care matters for older adults in China. Lancet Psychiatry 2015, 2, 286–287. [Google Scholar] [CrossRef]
- Su, P.; Ding, H.; Zhang, W.; Duan, G.; Yang, Y.; Chen, R.; Duan, Z.; Du, L.; Xie, C.; Jin, C.; et al. The association of multimorbidity and disability in a community-based sample of elderly aged 80 or older in Shanghai, China. BMC Geriatr. 2016, 16, 178. [Google Scholar] [CrossRef] [PubMed]
- Imamura, H.; Hamano, T.; Michikawa, T.; Takeda-Imai, F.; Nakamura, T.; Takebayashi, T.; Nishiwaki, Y. Relationships of Community and Individual Level Social Capital with Activities of Daily Living and Death by Gender. Int. J. Environ. Res. Public Health 2016, 13, 860. [Google Scholar] [CrossRef]
- World Health Organization. WHO Global Disability Action Plan 2014–2021: Better Health for All People with Disability; World Health Organization: Gevena, Switzerland, 2015. [Google Scholar]
- Hermsen, L.A.H.; Leone, S.S.; Smalbrugge, M.; Dekker, J.; van der Horst, H.E. Frequency, severity and determinants of functional limitations in older adults with joint pain and comorbidity: Results of a cross-sectional study. Arch. Gerontol. Geriatr. 2014, 59, 98–106. [Google Scholar] [CrossRef]
- Falk, H.; Johansson, L.; Östling, S.; Thøgersen Agerholm, K.; Staun, M.; Høst Dørfinger, L.; Skoog, I. Functional disability and ability 75-year-olds: A comparison of two Swedish cohorts born 30 years apart. Age Ageing 2014, 43, 636–641. [Google Scholar] [CrossRef]
- Lestari, S.K.; Ng, N.; Kowal, P.; Santosa, A. Diversity in the Factors Associated with ADL-Related Disability among Older People in Six Middle-Income Countries: A Cross-Country Comparison. Int. J. Environ. Res. Public Health 2019, 16, 1341. [Google Scholar] [CrossRef]
- Chen, S.; Qin, J.; Li, Y.; Wei, Y.; Long, B.; Cai, J.; Tang, J.; Xu, X.; Yu, G.; Zhang, Z. Disability and Its Influencing Factors among the Elderly in a County, Guangxi Province, China. Int. J. Environ. Res. Public Health 2018, 15, 1967. [Google Scholar] [CrossRef]
- Ran, L.; Jiang, X.; Li, B.; Kong, H.; Du, M.; Wang, X.; Yu, H.; Liu, Q. Association among activities of daily living, instrumental activities of daily living and health-related quality of life in elderly Yi ethnic minority. BMC Geriatr. 2017, 17, 74. [Google Scholar] [CrossRef]
- Cwirlej-Sozanska, A.B.; Sozanski, B.; Wisniowska-Szurlej, A.; Wilmowska-Pietruszynska, A. An assessment of factors related to disability in ADL and IADL in elderly inhabitants of rural areas of south-eastern Poland. Ann. Agric. Environ. Med. AAEM 2018, 25, 504–511. [Google Scholar] [CrossRef]
- Kojima, G. Frailty as a predictor of disabilities among community-dwelling older people: A systematic review and meta-analysis. Disabil. Rehabilit. 2017, 39, 1897–1908. [Google Scholar] [CrossRef] [PubMed]
- Teo, N.; Gao, Q.; Nyunt, M.S.Z.; Wee, S.L.; Ng, T.-P. Social Frailty and Functional Disability: Findings from the Singapore Longitudinal Ageing Studies. J. Am. Med. Dir. Assoc. 2017, 18, 637.e13–637.e19. [Google Scholar] [CrossRef] [PubMed]
- Imai, H.; Chen, W.L.; Fukutomi, E.; Okumiya, K.; Wada, T.; Sakamoto, R.; Fujisawa, M.; Ishimoto, Y.; Kimura, Y.; Chang, C.M.; et al. Depression and subjective economy7 among elderly people in Asian communities: Japan, Taiwan, and Korea. Arch. Gerontol. Geriatr. 2015, 60, 322–327. [Google Scholar] [CrossRef] [PubMed]
- Stuck, A.E.; Walthert, J.M.; Nikolaus, T.; Büla, C.J.; Hohmann, C.; Beck, J.C. Risk factors for functional status decline in community-living elderly people: A systematic literature review. Soc. Sci. Med. 1999, 48, 445–469. [Google Scholar] [CrossRef]
- Downer, B.; Crowe, M.; Markides, K.S. Influence of Type II Diabetes and High Depressive Symptoms on the Likelihood for Developing Activities of Daily Living (ADL) Disability and Mortality in Older Puerto Ricans. J. Aging Health 2017, 29, 1079–1095. [Google Scholar] [CrossRef] [PubMed]
- Bleijenberg, N.; Zuithoff, N.P.A.; Smith, A.K.; de Wit, N.J.; Schuurmans, M.J. Disability in the Individual ADL, IADL, and Mobility among Older Adults: A Prospective Cohort Study. J. Nutr. Health Aging 2017, 21, 897–903. [Google Scholar] [CrossRef]
- Bourdieu, P.; Richardson, J.G. Handbook of Theory and Research for the Sociology of Education; Greenwood: New York, NY, USA, 1986; pp. 241–258. [Google Scholar]
- Xu, Q.; Norstrand, J.A.; Du, Y. Effects of Living Alone on Social Capital and Health among Older Adults in China. Int. J. Aging Hum. Dev. 2015, 82, 30–53. [Google Scholar] [CrossRef]
- Liu, G.G.; Xue, X.; Yu, C.; Wang, Y. How does social capital matter to the health status of older adults? Evidence from the China Health and Retirement Longitudinal Survey. Econ. Hum. Biol. 2016, 22, 177–189. [Google Scholar] [CrossRef]
- Lu, N.; Lum, T.Y.; Lou, V.W. The impacts of community social capital on the life satisfaction of older adults in Hong Kong: The moderator role of intergenerational family capital. Aging Ment. Health 2016, 20, 1213–1220. [Google Scholar] [CrossRef]
- Gontijo, C.F.; Mambrini, J.V.; Luz, T.C.B.; Loyola, A.I.F. Association between disability and social capital among community-dwelling elderly. Rev. Bras. Epidemiol. Braz. J. Epidemiol. 2016, 19, 471–483. [Google Scholar] [CrossRef]
- Fujihara, S.; Tsuji, T.; Miyaguni, Y.; Aida, J.; Saito, M.; Koyama, S.; Kondo, K. Does Community-Level Social Capital Predict Decline in Instrumental Activities of Daily Living? A JAGES Prospective Cohort Study. Int. J. Environ. Res. Public Health 2019, 16, 828. [Google Scholar] [CrossRef] [PubMed]
- Tomioka, K.; Kurumatani, N.; Hosoi, H. Age and gender differences in the association between social participation and instrumental activities of daily living among community-dwelling elderly. BMC Geriatr. 2017, 17, 99. [Google Scholar] [CrossRef] [PubMed]
- Hao, X.; Gu, J.; Ying, X.; Bo, T.; Fu, W. Social support and care needs of the disabled elderly population: An empirical study based on survey data from Beijing, China. Biosci. Trends 2017, 11, 507–515. [Google Scholar] [CrossRef] [PubMed]
- Cassidy, J.; Jones, J.D.; Shaver, P.R. Contributions of attachment theory and research: A framework for future research, translation, and policy. Develop. Psychopathol. 2013, 25, 1415–1434. [Google Scholar] [CrossRef]
- Lawton, M.P.; Brody, E.M. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef]
- Han, S.; Lee, H.S. Social capital and depression: Does household context matter? Asia Pac. J. Public Health 2015, 27, 2008–2018. [Google Scholar] [CrossRef]
- Hu, F.; Niu, L.; Chen, R.; Ma, Y.; Qin, X.; Hu, Z. The association between social capital and quality of life among type 2 diabetes patients in Anhui province, China: A cross-sectional study. BMC Public Health 2015, 15, 786. [Google Scholar] [CrossRef]
- Maselko, J.; Hughes, C.; Cheney, R. Religious social capital: Its measurement and utility in the study of the social determinants of health. Soc. Sci. Med. 2011, 73, 759–767. [Google Scholar] [CrossRef]
- Ito, T.; Okuyama, K.; Abe, T.; Takeda, M.; Hamano, T.; Nakano, K.; Nabika, T. Relationship between Individual Social Capital and Cognitive Function among Older Adults by Gender: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2019, 16, 2142. [Google Scholar] [CrossRef]
- George, L.K.; Fillenbaum, G.G. OARS Methodology. J. Am. Geriatr. Soc. 1985, 33, 607–615. [Google Scholar] [CrossRef]
- Fillenbaum, G.G.; Smyer, M.A. The development, validity, and reliability of the OARS multidimensional functional assessment questionnaire. J. Gerontol. 1981, 36, 428–434. [Google Scholar] [CrossRef] [PubMed]
- Machuca, C.; Vettore, M.V.; Krasuska, M.; Baker, S.R.; Robinson, P.G. Using classification and regression tree modelling to investigate response shift patterns in dentine hypersensitivity. BMC Med. Res. Methodol. 2017, 17, 120. [Google Scholar] [CrossRef] [PubMed]
- Connolly, D.; Garvey, J.; McKee, G. Factors associated with ADL/IADL disability in community dwelling older adults in the Irish longitudinal study on ageing (TILDA). Disabil. Rehabilit. 2017, 39, 809–816. [Google Scholar] [CrossRef] [PubMed]
- Spector, W.D.; Fleishman, J.A. Combining activities of daily living with instrumental activities of daily living to measure functional disability. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 1998, 53, S46–S57. [Google Scholar] [CrossRef]
- Cao, J.; Rammohan, A. Social capital and healthy ageing in Indonesia. BMC Public Health 2016, 16, 631. [Google Scholar] [CrossRef]
- Hsu, H.C.; Chang, W.C. Social connections and happiness among the elder population of Taiwan. Aging Ment. Health 2015, 19, 1131–1137. [Google Scholar] [CrossRef]
- Ohrnberger, J.; Fichera, E.; Sutton, M. The relationship between physical and mental health: A mediation analysis. Soc. Sci. Med. 2017, 195, 42–49. [Google Scholar] [CrossRef]
- Mendoza-Núñez, V.M.; González-Mantilla, F.; Correa-Muñoz, E.; Retana-Ugalde, R. Relationship between Social Support Networks and Physical Functioning in Older Community-Dwelling Mexicans. Int. J. Environ. Res. Public Health 2017, 14, 993. [Google Scholar] [CrossRef]
- Villalonga-Olives, E.; Kawachi, I. The measurement of social capital. Gac. Sanit. 2015, 29, 62–64. [Google Scholar] [CrossRef]
- Feng, Q.; Zhen, Z.; Gu, D.; Wu, B.; Duncan, P.W.; Purser, J.L. Trends in ADL and IADL disability in community-dwelling older adults in Shanghai, China, 1998–2008. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2013, 68, 476–485. [Google Scholar] [CrossRef]
- Zhang, J.; Lu, N. What Matters Most for Community Social Capital among Older Adults Living in Urban China: The Role of Health and Family Social Capital. Int. J. Environ. Res. Public Health 2019, 16, 558. [Google Scholar] [CrossRef] [PubMed]
- Joe, W.; Perkins, J.M.; Subramanian, S.V. Community involvement, trust, and health-related outcomes among older adults in India: A population-based, multilevel, cross-sectional study. Age Ageing 2019, 48, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Amemiya, A.; Saito, J.; Saito, M.; Takagi, D.; Haseda, M.; Tani, Y.; Kondo, K.; Kondo, N. Social Capital and the Improvement in Functional Ability among Older People in Japan: A Multilevel Survival Analysis Using JAGES Data. Int. J. Environ. Res. Public Health 2019, 16, 1310. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.-I.; Lin, T.-F. Social capital and preventive care use among the elderly under Taiwan’s National Health Insurance. Arch. Gerontol. Geriatr. 2018, 75, 28–36. [Google Scholar] [CrossRef]
- Thompson, W.W.; Zack, M.M.; Krahn, G.L.; Andresen, E.M.; Barile, J.P. Health-related quality of life among older adults with and without functional limitations. Am. J. Public Health 2012, 102, 496–502. [Google Scholar] [CrossRef]
| Variables | Total n = 1810 | Robust n = 1032 | Limited n = 778 | χ2 | p-Value * |
|---|---|---|---|---|---|
| Age, years, N (%) | 130.366 | <0.001 | |||
| 60–64 | 399 (22.0) | 281 (27.2) | 118 (15.2) | ||
| 65–69 | 424 (23.4) | 267 (25.9) | 157 (20.2) | ||
| 70–74 | 421 (23.3) | 262 (25.4) | 159 (20.4) | ||
| 75–79 | 282 (15.6) | 135 (13.1) | 147 (18.9) | ||
| ≥80 | 284 (15.7) | 87 (8.4) | 197 (25.3) | ||
| Gender N (%) | 57.518 | <0.001 | |||
| Male | 770 (42.5) | 518 (50.2) | 252 (32.4) | ||
| Female | 1040 (57.5) | 514 (49.8) | 526 (67.6) | ||
| BMI, kg/m2, N (%) | 26.910 | <0.001 | |||
| <18.5 | 189 (10.4) | 88 (8.5) | 101 (13.0) | ||
| 18.5–22.9 | 825 (45.6) | 439 (42.5) | 386 (49.6) | ||
| 23.0–27.4 | 644 (35.6) | 411 (39.8) | 233 (29.9) | ||
| ≥27.5 | 152 (8.4) | 94 (9.1) | 58 (7.5) | ||
| Residence N (%) | 91.924 | <0.001 | |||
| Urban | 801 (44.3) | 557 (54.0) | 244 (31.4) | ||
| Rural | 1009 (55.7) | 475 (46.0) | 534 (68.6) | ||
| Living status N (%) | 1.418 | 0.234 | |||
| Living with others | 1567 (86.6) | 902 (87.4) | 665 (85.5) | ||
| Living alone | 243 (13.4) | 130 (12.6) | 113 (14.5) | ||
| Marital status N (%) | 41.402 | <0.001 | |||
| Married/Cohabited | 1402 (77.5) | 856 (82.9) | 546 (70.2) | ||
| Single | 408 (22.5) | 176 (17.1) | 232 (29.8) | ||
| Education N (%) | 173.182 | <0.001 | |||
| Primary school and below | 1291 (71.3) | 613 (59.4) | 678 (87.1) | ||
| Junior school | 291 (16.1) | 221 (21.4) | 70 (9.0) | ||
| High school and above | 228 (12.6) | 198 (19.2) | 30 (3.9) | ||
| Smoking status N (%) | 43.239 | <0.001 | |||
| Nonsmoking | 1412 (78.0) | 752 (72.9) | 660 (84.8) | ||
| Former smoking | 99 (5.5) | 59 (5.7) | 40 (5.1) | ||
| Current Smoking | 299 (16.5) | 221 (21.4) | 78 (10.0) | ||
| Drinking status N (%) | 23.469 | <0.001 | |||
| Nondrinking | 1484 (82.0) | 816 (79.1) | 668 (85.9) | ||
| Former drinking | 70 (3.9) | 35 (3.4) | 35 (4.5) | ||
| Current Drinking | 256 (14.1) | 181 (17.5) | 75 (9.6) | ||
| Multimorbidity N (%) | 66.651 | <0.001 | |||
| No | 1244 (68.7) | 789 (76.5) | 455 (58.5) | ||
| Yes | 566 (31.3) | 243 (23.5) | 323 (41.5) | ||
| Social participation N (%) | 48.281 | <0.001 | |||
| High | 1043 (57.6) | 667 (64.6) | 376 (48.3) | ||
| Low | 767 (42.4) | 365 (35.4) | 402 (51.7) | ||
| Social support N (%) | 0.373 | 0.541 | |||
| High | 906 (50.1) | 523 (50.7) | 383 (49.2) | ||
| Low | 904 (49.9) | 509 (49.3) | 395 (50.8) | ||
| Social connection N (%) | 45.604 | <0.001 | |||
| High | 1279 (70.7) | 794 (76.9) | 485 (62.3) | ||
| Low | 531 (29.3) | 238 (23.1) | 293 (37.7) | ||
| Trust N (%) | 6.069 | 0.014 | |||
| High | 1023 (56.5) | 609 (59.0) | 414 (53.2) | ||
| Low | 787 (43.5) | 423 (41.0) | 364 (46.8) | ||
| Cohesion N (%) | 9.802 | 0.002 | |||
| High | 1078 (59.6) | 647 (62.7) | 431 (55.4) | ||
| Low | 732 (40.4) | 385 (37.3) | 347 (44.6) | ||
| Reciprocity N (%) | 13.368 | <0.001 | |||
| High | 978 (54.0) | 596 (57.8) | 382 (49.1) | ||
| Low | 832 (46.0) | 436 (42.2) | 396 (50.9) |
| Crude OR (95% CI) | Adjusted OR (95% CI) | |
|---|---|---|
| Age, years | ||
| 60–64 | (reference) | (reference) |
| 65–69 | 1.40 (1.05–1.87) * | 1.18 (0.85–1.64) |
| 70–74 | 1.45 (1.08–1.93) * | 1.49 (1.06–2.07) * |
| 75–79 | 2.59 (1.89–3.56) ** | 2.97 (2.04–4.34) ** |
| ≥80 | 5.39 (3.87–7.51) ** | 6.01 (4.03–8.97) ** |
| Gender | ||
| Male | (reference) | (reference) |
| Female | 2.10 (1.73–2.55) ** | 1.74 (1.31–2.31) ** |
| BMI, kg/m2 | ||
| 18.5–22.9 = normal weight | (reference) | (reference) |
| <18.5 = underweight | 1.31 (0.95–1.79) | 0.91 (0.63–1.33) |
| 23.0–27.4 = overweight | 0.64 (0.52–0.80) ** | 0.73 (0.57–0.94) ** |
| ≥27.5 = obese | 0.70 (0.49–1.00) | 0.61 (0.40–0.92) ** |
| Residence | ||
| Urban | (reference) | (reference) |
| Rural | 2.57 (2.11–3.12) ** | 2.29 (1.80–2.91) ** |
| Living status | ||
| Living with others | (reference) | (reference) |
| Living alone | 1.18 (0.90–1.55) | 0.44 (0.30–0.65) ** |
| Marital status | ||
| Married/Cohabited | (reference) | (reference) |
| Single | 2.07 (1.65–2.58) ** | 1.55 (1.12–2.14) * |
| Education | ||
| High school and above | (reference) | (reference) |
| Junior school | 2.09 (1.31–3.34) * | 1.87 (1.12–3.11) * |
| Primary school and below | 7.30 (4.90–10.88) ** | 4.67 (2.98–7.31) ** |
| Smoking status | ||
| Nonsmoking | (reference) | (reference) |
| Former smoking | 0.77 (0.51–1.17) | 0.93 (0.52–1.64) |
| Current Smoking | 0.40 (0.30–0.53) ** | 0.52 (0.36–0.76) * |
| Drinking status | ||
| Nondrinking | (reference) | (reference) |
| Former drinking | 1.22 (0.76–1.97) | 2.03 (1.05–3.91) * |
| Current Drinking | 0.51 (0.38–0.68) ** | 0.90 (0.62–1.29) |
| Multimorbidity | ||
| No | (reference) | (reference) |
| Yes | 2.30 (1.88–2.82) ** | 2.32 (1.83–2.95) ** |
| Social participation | ||
| High | (reference) | (reference) |
| Low | 1.95 (1.62–2.36) ** | 1.60 (1.26–2.03) ** |
| Social support | ||
| High | (reference) | (reference) |
| Low | 1.06 (0.88–1.28) | 0.73 (0.57–0.94) * |
| Social connection | ||
| High | (reference) | (reference) |
| Low | 2.02 (1.64–2.47) ** | 1.74 (1.34–2.25) ** |
| Trust | ||
| High | (reference) | (reference) |
| Low | 1.27 (1.05–1.53) * | 0.95 (0.73–1.24) |
| Cohesion | ||
| High | (reference) | (reference) |
| Low | 1.35 (1.12–1.64) * | 0.90 (0.69–1.18) |
| Reciprocity | ||
| High | (reference) | (reference) |
| Low | 1.42 (1.18–1.71) ** | 1.16 (0.89–1.52) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bai, Z.; Wang, Z.; Shao, T.; Qin, X.; Hu, Z. Relationship between Individual Social Capital and Functional Ability among Older People in Anhui Province, China. Int. J. Environ. Res. Public Health 2020, 17, 2775. https://doi.org/10.3390/ijerph17082775
Bai Z, Wang Z, Shao T, Qin X, Hu Z. Relationship between Individual Social Capital and Functional Ability among Older People in Anhui Province, China. International Journal of Environmental Research and Public Health. 2020; 17(8):2775. https://doi.org/10.3390/ijerph17082775
Chicago/Turabian StyleBai, Zhongliang, Zijing Wang, Tiantai Shao, Xia Qin, and Zhi Hu. 2020. "Relationship between Individual Social Capital and Functional Ability among Older People in Anhui Province, China" International Journal of Environmental Research and Public Health 17, no. 8: 2775. https://doi.org/10.3390/ijerph17082775
APA StyleBai, Z., Wang, Z., Shao, T., Qin, X., & Hu, Z. (2020). Relationship between Individual Social Capital and Functional Ability among Older People in Anhui Province, China. International Journal of Environmental Research and Public Health, 17(8), 2775. https://doi.org/10.3390/ijerph17082775





