How to Reduce Excessive Use of the Health Care Service in Medical Aid Beneficiaries: Effectiveness of Community-Based Case Management
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample and Data Source
2.2. Variables
2.3. Analysis
3. Results
3.1. Differences in General Characteristics of the Target Groups for Case Management
3.2. Service Duration and Performance of Case Management by Target Groups
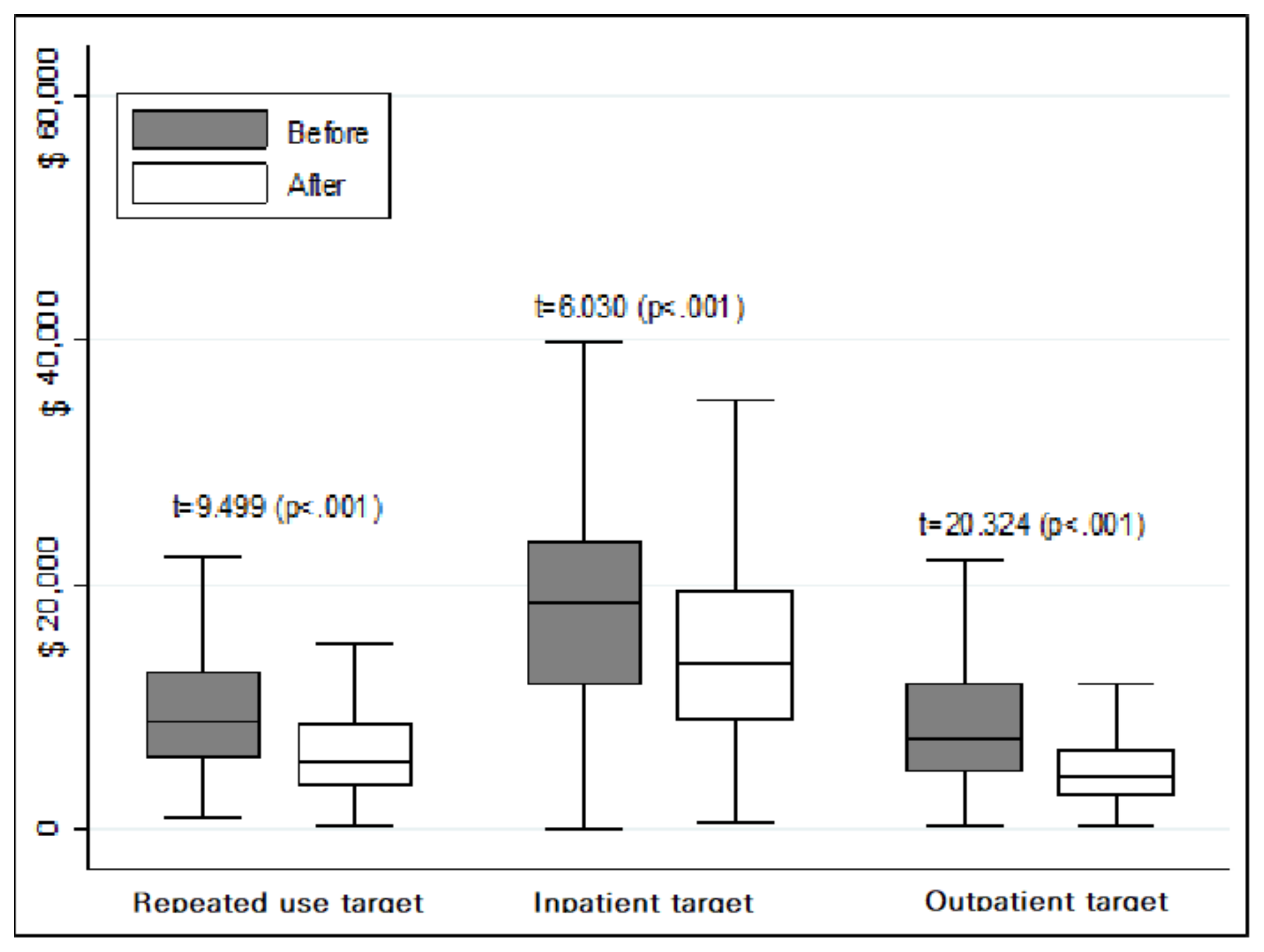
3.3. Changes in Service Outcomes for Case Management
3.4. Comparison of Effect on Case Management by the Target Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ahn, Y.H.; Kim, E.S.; Ham, O.K.; Kim, S.H.; Hwang, S.S.; Chun, S.H.; Gwon, N.Y.; Choi, J.Y. Factors associated with the overuse or underuse of health care services among medical aid beneficiaries in Korea. J. Community Health Nurs. 2011, 28, 190–203. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Shon, C. The effects of health coverage schemes on length of stay and preventable hospitalization in Seoul. Int. J. Environ. Res. Public Health 2018, 15. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.W.; Chu, C. The story of Korean health insurance system. Osong Public Health Res. Perspect. 2017, 8, 235–236. [Google Scholar] [CrossRef] [PubMed]
- Fry, C.E.; Sommers, B.D. Effect of Medicaid expansion on health insurance coverage and access to care among adults with depression. Psychiatr Serv. 2018, 69, 1146–1152. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.W.; Yeo, N.G. Current state and challenges of Medical Aid Programme. Health Welf. Policy Forum 2016, 241, 32–42. (In Korean) [Google Scholar]
- Kim, J.H.; Lee, K.S.; Yoo, K.B.; Park, E.C. The differences in health care utilization between Medical Aid and health insurance: A longitudinal study using propensity score matching. PLoS ONE 2015, 10, e0119939. [Google Scholar] [CrossRef]
- Shin, S.M.; Kim, M.J.; Kim, E.S.; Lee, H.W.; Park, C.G.; Kim, H.K. Medical Aid service overuse assessed by case managers in Korea. J. Adv. Nurs. 2010, 66, 2257–2265. [Google Scholar] [CrossRef]
- Sommers, B.D.; Blendon, R.J.; Orav, E.J.; Epstein, A.M. Changes in utilization and health among low-income adults after Medicaid expansion or expanded private insurance. JAMA Intern. Med. 2016, 176, 1501–1509. [Google Scholar] [CrossRef]
- Kim, J.H.; Lee, S.G.; Lee, K.S.; Jang, S.I.; Cho, K.H.; Park, E.C. Impact of health insurance status changes on healthcare utilisation patterns: A longitudinal cohort study in South Korea. BMJ Open 2016, 6, e0095. [Google Scholar] [CrossRef][Green Version]
- Health Insurance Review & Assessment Service. Available online: https://www.hira.or.kr/dummy.do?pgmid=HIRAA020028000000 (assessed on 1 April 2020).
- Bodenmann, P.; Velonaki, V.S.; Griffin, J.L.; Baggio, S.; Iglesias, K.; Moschetti, K.; Ruggeri, O.; Burnand, B.; Wasserfallen, J.B.; Vu, F.; et al. Case management may reduce emergency department frequent use in a universal health coverage system: A randomized controlled trial. J. Gen. Intern. Med. 2017, 32, 508–515. [Google Scholar] [CrossRef]
- Joo, J.Y.; Liu, M.F. Case management effectiveness in reducing hospital use: A systematic review. Int. Nurs. Rev. 2017, 64, 296–308. [Google Scholar] [CrossRef] [PubMed]
- Hammer, B.J. Community-based case management for positive outcomes. Geriatr. Nurs. 2001, 22, 271–275. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.S.; Oh, J.J. Case management for medical aid beneficiaries in Korea: Findings from case-control study. Asian Nurs. Res. 2014, 8, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Welfare. Available online: http://www.mohw.go.kr/react/gm/sgm0601vw.jsp?PAR_MENU_ID=13&MENU_ID=1304020603&page=1&CONT_SEQ=293443 (assessed on 1 April 2020).
- Einav, L.; Finkelstein, A. Moral hazard in health insurance: What we know and how we know it. J. Eur. Econ. Assoc. 2018, 16, 957–982. [Google Scholar] [CrossRef] [PubMed]
- Fukushima, K.; Mizuoka, S.; Yamamoto, S.; Iizuka, T. Patient cost sharing and medical expenditures for the elderly. J. Health Econ. 2016, 45, 115–130. [Google Scholar] [CrossRef]
- Pickens, G.; Karaca, Z.; Cutler, E.; Dworsky, M.; Eibner, C.; Moore, B.; Gibson, T.; Iyer, S.; Wong, H. Changes in hospital inpatient utilization following health care reform. Health Serv. Res. 2018, 53, 2446–2469. [Google Scholar] [CrossRef]
- Oh, J.; Oh, S. Nurse case managers’ experiences on case management for long-term hospitalization in Korea. Asian Nurs. Res. 2017, 11, 283–289. [Google Scholar] [CrossRef]
- Corvol, A.; Dreier, A.; Prudhomm, J.; Thyrian, J.R.; Hoffmann, W.; Somme, D. Consequences of clinical case management for caregivers: A systematic review. Int. J. Geriatr. Psychiatry 2017, 32, 473–483. [Google Scholar] [CrossRef]
- Weintraub, W.S.; Elliott, D.; Fanari, Z.; Ostertag-Stretch, J.; Muther, A.; Lynahan, M.; Kerzner, R.; Salam, T.; Scherrer, H.; Anderson, S.; et al. The impact of care management information technology model on quality of care after coronary artery bypass surgery: “Bridging the Divides”. Cardiovasc. Revasc. Med. 2018, 19, 106–111. [Google Scholar] [CrossRef]
- Rosella, L.C.; Fitzpatrick, T.; Wodchis, W.P.; Calzavara, A.; Manson, H.; Goel, V. High-cost health careusers in Ontario, Canada: Demographic, socio-economic, and health status characteristics. BMC Health Serv. Res. 2014, 14, 532. [Google Scholar] [CrossRef]
- Blumenthal, D.; Chernof, B.; Fulmer, T.; Lumpkin, J.; Selberg, J. Caring for high-need, highcost patients—An urgent priority. N. Engl. J. Med. 2016, 375, 909–911. [Google Scholar] [CrossRef] [PubMed]
- Guilcher, S.J.; Bronskill, S.E.; Guan, J.; Wodchis, W.P. Who are the high-cost users? A method for person-centred attribution health care spending. PLoS ONE 2016, 11, e0149179. [Google Scholar] [CrossRef] [PubMed]
- Van der Heide, I.; Wang, J.; Droomers, M.; Spreeuwenberg, P.; Rademakers, J.; Uiters, E. The relationship between health, education, and health literacy: Results from the Dutch Adult Literacy and Life Skills Survey. J. Health Commun. 2013, 18, 172–184. [Google Scholar] [CrossRef] [PubMed]
| Variables | Categories | Target Group (n = 1741) | X2 | p-Value | ||
|---|---|---|---|---|---|---|
| Outpatient (n = 1107) | Inpatient (n = 351) | Repeated Use (n = 283) | ||||
| Gender | Women | 729(65.9) | 179(51.0) | 175(61.8) | 25.039 | <0.001 |
| Men | 378(34.1) | 172(49.0) | 108(38.2) | |||
| Age | Under 64 years | 323(29.2) | 133(37.9) | 105(37.1) | 12.950 | 0.002 |
| Over 65 years | 784(70.8) | 218(62.1) | 179(62.9) | |||
| Medical care type | Type1 | 1052(95.0) | 343(97.7) | 272(96.1) | 4.845 | 0.089 |
| Type2 | 55(5.0) | 8(2.3) | 11(3.9) | |||
| Enrollment | Re-enroll | 842(76.1) | 216(61.5) | 198(70.0) | 28.766 | <0.001 |
| First enroll | 265(23.9) | 135(28.5) | 85(30.0) | |||
| Housemate | No | 637(57.5) | 257(73.2) | 171(60.4) | 27.653 | <0.001 |
| Yes | 470(42.5) | 94(26.8) | 112(39.6) | |||
| Education | Pre-primary | 485(43.9) | 135(38.5) | 110(28.9) | 5.530 | 0.478 |
| Primary | 305(27.6) | 99(28.2) | 84(29.7) | |||
| Lower secondary | 143(12.9) | 49(14.0) | 40(14.1) | |||
| Upper secondary | 174(15.6) | 68(19.3) | 49(17.3) | |||
| Region | Metropolitan | 381(34.4) | 127(36.2) | 107(37.8) | 2.358 | 0.670 |
| Non-metropolitan | 375(33.9) | 121(34.5) | 98(34.6) | |||
| Rural | 351(31.7) | 103(29.3) | 78(27.6) | |||
| Main disease | Cardiovascular | 394(35.6) | 107(30.5) | 85(30.0) | 121.952 | <0.001 |
| Musculoskeletal | 209(18.9) | 35(10.0) | 72(25.5) | |||
| Mental disorder | 137(12.4) | 113(32.1) | 39(13.8) | |||
| Endocrine disease | 183(16.5) | 21(6.0) | 42(14.8) | |||
| Neoplasm | 104(9.4) | 55(15.7) | 27(9.5) | |||
| Others | 80(7.2) | 20(5.7) | 18(6.4) | |||
| Variables | Categories | Outpatient Target | Inpatient Target | Repeated Use Target |
|---|---|---|---|---|
| (n = 1107) | (n = 351) | (n = 283) | ||
| Duration (months) | 3 | 5 | within 12 | |
| Frequency of service, n(%) | Total | 9814 | 3651 | 4584 |
| Phone | 4814(49.1) | 1946(53.3) | 2292(50.0) | |
| 2503(25.5) | 784(21.5) | 1078(23.5) | ||
| Home visit | 2278(23.2) | 783(21.4) | 945(20.6) | |
| Transitional care | 160(1.6) | 115(3.1) | 176(3.8) | |
| Hospital visit | 50(0.5) | 3(0.1) | 82(1.8) | |
| Referral to hospital | 9(0.1) | 20(0.5) | 11(0.2) | |
| Number of services per person, mean ± SD | Total | 8.87 ± 1.54 | 10.40 ± 4.10 | 16.20 ± 6.00 |
| Phone | 4.35 ± 0.78 | 5.54 ± 2.58 | 8.10 ± 3.27 | |
| 2.26 ± 1.02 | 2.23 ± 1.42 | 3.81 ± 2.53 | ||
| Home visit | 2.06 ± 0.36 | 2.23 ± 1.11 | 3.34 ± 1.49 | |
| Transitional care | 0.14 ± 0.43 | 0.33 ± 0.61 | 0.62 ± 1.09 | |
| Hospital visit | 0.05 ± 0.24 | 0.01 ± 0.10 | 0.29 ± 1.14 | |
| Referral to hospital | 0.01 ± 0.10 | 0.06 ± 0.23 | 0.04 ± 0.21 | |
| Variables | Group | Before | After | t | p-Value |
|---|---|---|---|---|---|
| (Mean ± SD) | (Mean ± SD) | ||||
| Client-centered outcome | |||||
| Health related QOL | Outpatient target | 17.20 ± 2.98 | 19.33 ± 2.38 | 29.29 | <0.001 |
| Inpatient target | 18.53 ± 4.00 | 19.45 ± 4.14 | 8.675 | <0.001 | |
| Repeated use target * | 0.68 ± 0.14 | 0.78 ± 0.13 | 11.912 | <0.001 | |
| Self-care ability | Outpatient target | 15.41 ± 2.82 | 18.64 ± 2.52 | 37.152 | <0.001 |
| Inpatient target | 12.64 ± 4.12 | 14.05 ± 4.49 | 10.507 | <0.001 | |
| Having support system | Outpatient target | 5.85 ± 1.70 | 6.43 ± 1.45 | 17.054 | <0.001 |
| Inpatient target | 6.32 ± 1.73 | 6.99 ± 1.65 | 9.842 | <0.001 | |
| Health care utilization | |||||
| Inpatient days | Outpatient target | 30.5 ± 23.0 | 10.6 ± 30.7 | 17.766 | <0.001 |
| Inpatient target | 240.2 ± 141.3 | 206.0 ± 117.6 | 3.924 | <0.001 | |
| Repeated use target | 36.1 ± 64.1 | 18.7 ± 49.2 | 5.898 | <0.001 | |
| Outpatient visits | Outpatient target | 128.3 ± 120.4 | 104.7 ± 111.1 | 8.716 | <0.001 |
| Inpatient target | 47.3 ± 93.9 | 34.5 ± 56.1 | 2.540 | 0.012 | |
| Repeated use target | 182.6 ± 137.1 | 138.9 ± 119.6 | 9.821 | <0.001 | |
| Variables | Outpatient Target a | Inpatient Target b | Repeated Use Target c | F | p-Value | Post-hoc |
|---|---|---|---|---|---|---|
| (n = 1107) | (n = 351) | (n = 283) | ||||
| Healthcare utilization | ||||||
| Inpatient days | 19.9 ± 44.6 | 34.3 ± 163.3 | 17.4 ± 49.2 | 4.45 | 0.012 | b > a,c |
| Outpatient visits | 23.3 ± 90.2 | 12.9 ± 93.9 | 43.1 ± 74.5 | 9.73 | 0.000 | c > a,b |
| Healthcare cost, $ | 4007.9 ± 6519.6 | 3592.6 ± 11,002.9 | 3197.0 ± 5621.9 | 1.46 | 0.233 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, M.J.; Lee, E. How to Reduce Excessive Use of the Health Care Service in Medical Aid Beneficiaries: Effectiveness of Community-Based Case Management. Int. J. Environ. Res. Public Health 2020, 17, 2503. https://doi.org/10.3390/ijerph17072503
Kim MJ, Lee E. How to Reduce Excessive Use of the Health Care Service in Medical Aid Beneficiaries: Effectiveness of Community-Based Case Management. International Journal of Environmental Research and Public Health. 2020; 17(7):2503. https://doi.org/10.3390/ijerph17072503
Chicago/Turabian StyleKim, Myung Ja, and Eunhee Lee. 2020. "How to Reduce Excessive Use of the Health Care Service in Medical Aid Beneficiaries: Effectiveness of Community-Based Case Management" International Journal of Environmental Research and Public Health 17, no. 7: 2503. https://doi.org/10.3390/ijerph17072503
APA StyleKim, M. J., & Lee, E. (2020). How to Reduce Excessive Use of the Health Care Service in Medical Aid Beneficiaries: Effectiveness of Community-Based Case Management. International Journal of Environmental Research and Public Health, 17(7), 2503. https://doi.org/10.3390/ijerph17072503





