Big Data and Digitalization in Dentistry: A Systematic Review of the Ethical Issues
Abstract
1. Introduction
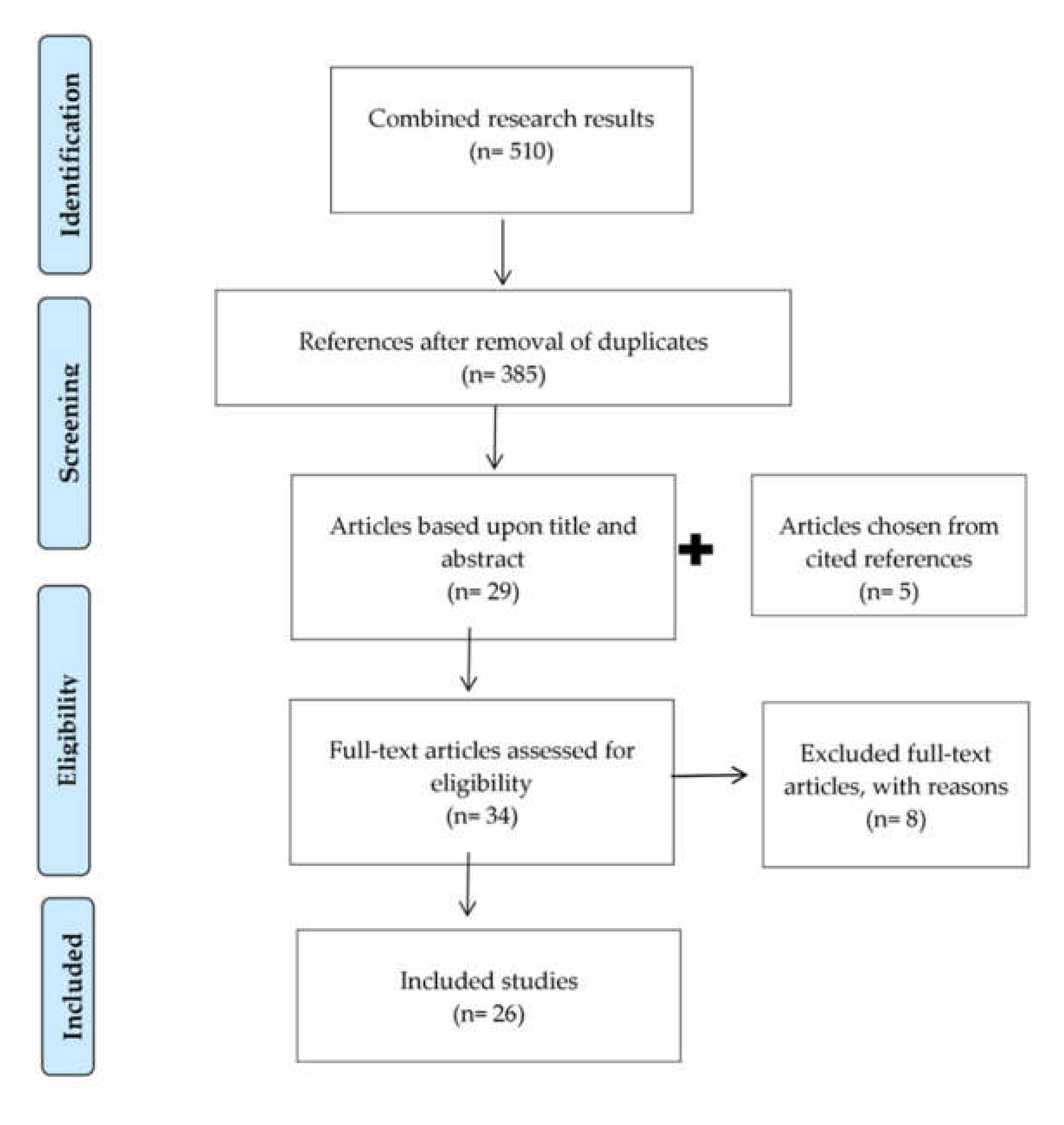
2. Materials and Methods
3. Results
3.1. Implementation of Digital Technologies in Dentistry
3.2. Big Data and Data Analytics
3.2.1. Electronic Health Records (EHRs)
3.2.2. mHealth and Teledentistry
3.2.3. Personalized Medicine and Data Linkage
3.3. Digital Communication and Social Media in Dentistry
3.4. Digital Photography and Radiography
3.5. Digital Dentistry Might Solve Ethical Issues
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lynch, C. How do your data grow? Nature 2008, 455, 28–29. [Google Scholar] [CrossRef]
- Boyd, D.; Crawford, K. CRITICAL QUESTIONS FOR BIG DATA. Info. Commun. Soc. 2012, 15, 662–679. [Google Scholar] [CrossRef]
- Mertz, L. Saving Lives and Money with Smarter Hospitals: Streaming analytics, other new tech help to balance costs and benefits. IEEE Pulse 2014, 5, 33–36. [Google Scholar] [CrossRef] [PubMed]
- Cohen, I.G.; Amarasingham, R.; Shah, A.; Xie, B.; Lo, B. The Legal And Ethical Concerns That Arise From Using Complex Predictive Analytics In Health Care. Heal. Aff. 2014, 33, 1139–1147. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.H.; Yoon, H.-J. Medical big data: promise and challenges. Kidney Res. Clin. Pr. 2017, 36, 3–11. [Google Scholar] [CrossRef]
- Liu, X.; Faes, L.; Kale, A.U.; Wagner, S.K.; Fu, D.J.; Bruynseels, A.; Mahendiran, T.; Moraes, G.; Shamdas, M.; Kern, C.; et al. A comparison of deep learning performance against health-care professionals in detecting diseases from medical imaging: a systematic review and meta-analysis. Lancet Digit. Heal. 2019, 1, e271–e297. [Google Scholar] [CrossRef]
- Nilsen, W.J.; Kumar, S.; Shar, A.; Varoquiers, C.; Wiley, T.; Riley, W.T.; Pavel, M.; Atienza, A.A. Advancing the Science of mHealth. J. Heal. Commun. 2012, 17, 5–10. [Google Scholar] [CrossRef]
- Fasbinder, D.J. Digital dentistry: innovation for restorative treatment. Compend. Contin. Educ. Dent. 2010, 31, 2–11. [Google Scholar]
- Joda, T.; Wolfart, S.; Reich, S.; Zitzmann, N.U. Virtual Dental Patient: How Long Until It’s Here? Curr. Oral Heal. Rep. 2018, 5, 116–120. [Google Scholar] [CrossRef]
- Finkelstein, J.; Ba, F.Z.; Bs, S.A.L.; Cappelli, D. Using big data to promote precision oral health in the context of a learning healthcare system. J. Public Heal. Dent. 2020, 80, S43–S58. [Google Scholar] [CrossRef]
- Joda, T.; Waltimo, T.; Pauli-Magnus, C.; Probst-Hensch, N.; Zitzmann, N.U. Population-Based Linkage of Big Data in Dental Research. Int. J. Environ. Res. Public Heal. 2018, 15, 2357. [Google Scholar] [CrossRef] [PubMed]
- Joda, T.; Waltimo, T.; Probst-Hensch, N.; Pauli-Magnus, C.; Zitzmann, N.U. Health Data in Dentistry: An Attempt to Master the Digital Challenge. Public Heal. Genom. 2019, 22, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Hogan, R.; Goodwin, M.; Boothman, N.; Iafolla, T.; Pretty, I.A. Further opportunities for digital imaging in dental epidemiology. J. Dent. 2018, 74, S2–S9. [Google Scholar] [CrossRef] [PubMed]
- Vandenberghe, B. The digital patient – Imaging science in dentistry. J. Dent. 2018, 74, S21–S26. [Google Scholar] [CrossRef]
- Brodt, E.D.; Skelly, A.C.; Dettori, J.R.; Hashimoto, R.E. Administrative Database Studies: Goldmine or Goose Chase? Evid Based Spine Care J. 2014, 5, 74–76. [Google Scholar] [CrossRef]
- Liang, H.; Tsui, B.Y.; Ni, H.; Valentim, C.C.S.; Baxter, S.L.; Liu, G.; Cai, W.; Kermany, D.S.; Sun, X.; Chen, J.; et al. Evaluation and accurate diagnoses of pediatric diseases using artificial intelligence. Nat. Med. 2019, 25, 433–438. [Google Scholar] [CrossRef]
- Ioannidis, J.P. Informed consent, big data, and the oxymoron of research that is not research. Am. J. Bioeth. 2013, 13, 40–42. [Google Scholar] [CrossRef]
- Martani, A.; Geneviève, L.D.; Pauli-Magnus, C.; McLennan, S.; Elger, B.S. Regulating the Secondary Use of Data for Research: Arguments Against Genetic Exceptionalism. Front. Genet. 2019, 10, 1254. [Google Scholar] [CrossRef]
- Francis, J.G.; Francis, L.P. Privacy, Confidentiality, and Justice. J. Soc. Philos. 2014, 45, 408–431. [Google Scholar] [CrossRef]
- Schneble, C.O.; Elger, B.S.; Shaw, D. The Cambridge Analytica affair and Internet-mediated research. EMBO Rep. 2018, 19, e46579. [Google Scholar] [CrossRef]
- Schneble, C.O.; Elger, B.S.; Shaw, D. Google’s Project Nightingale highlights the necessity of data science ethics review. EMBO Mol. Med. 2020, 12(3), e12053. [Google Scholar] [CrossRef] [PubMed]
- McMahon, A.; Buyx, A.; Prainsack, B. Big Data Governance Needs More Collective Responsibility: The Role of Harm Mitigation in the Governance of Data Use in Medicine and Beyond. Med Law Rev. 2019, 28, 155–182. [Google Scholar] [CrossRef] [PubMed]
- Choudhury, S.; Fishman, J.R.; McGowan, M.L.; Juengst, E. Big data, open science and the brain: lessons learned from genomics. Front. Hum. Neurosci. 2014, 8, 239. [Google Scholar] [CrossRef] [PubMed]
- Favaretto, M.; De Clercq, E.; Elger, B.S. Big Data and discrimination: perils, promises and solutions. A systematic review. J. Big Data 2019, 6, 12. [Google Scholar] [CrossRef]
- Geneviève, L.D.; Martani, A.; Shaw, D.M.; Elger, B.S.; Wangmo, T. Structural racism in precision medicine: leaving no one behind. BMC Med Ethic 2020, 21, 1–13. [Google Scholar] [CrossRef]
- Martani, A.; Shaw, D.; Elger, B.S. Stay fit or get bit - ethical issues in sharing health data with insurers’ apps. Swiss Med Wkly. 2019, 149, w20089. [Google Scholar] [CrossRef]
- Martin, K.E.M. Ethical Implications and Accountability of Algorithms. SSRN Electron. J. 2018, 160, 835–850. [Google Scholar] [CrossRef]
- Mittelstadt, B.D.; Floridi, L. The ethics of big data: current and foreseeable issues in biomedical contexts. Sci. Eng. Ethics 2016, 22, 303–341. [Google Scholar] [CrossRef]
- Esfandiari, S.; Feine, J. Health technology assessment in oral health. Int. J. Oral Maxillofac. Implant. 2011, 26, 93–100. [Google Scholar]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.G.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Rodgers, M.; Sowden, A.; Petticrew, M.; Arai, L.; Roberts, H.M.; Britten, N.; Popay, J. Testing Methodological Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. Evaluation 2009, 15, 49–73. [Google Scholar] [CrossRef]
- Gross, D.; Gross, K.; Wilhelmy, S. Digitalization in dentistry: ethical challenges and implications. Quintessence Int. 2019, 50, 830–838. [Google Scholar] [PubMed]
- Knott, N.J. The use of information and communication technology (ICT) in dentistry. Br. Dent. J. 2013, 214, 151–153. [Google Scholar] [CrossRef] [PubMed]
- Day, P.F.; Petherick, E.; Godson, J.; Owen, J.; Douglas, G. A feasibility study to explore the governance processes required for linkage between dental epidemiological, and birth cohort, data in the UK. Community Dent. Health 2018, 35, 228–234. [Google Scholar]
- Zijlstra-Shaw, S.; Stokes, C.W. Learning analytics and dental education; choices and challenges. Eur. J. Dent. Educ. 2018, 22, e658–e660. [Google Scholar] [CrossRef]
- Eng, G.; Chen, A.; Vess, T.; Ginsburg, G.S. Genome technologies and personalized dental medicine. Oral Dis. 2011, 18, 223–235. [Google Scholar] [CrossRef]
- Boden, D.F. What Guidance Is There for Ethical Records Transfer and Fee Charges? J. Am. Dent. Assoc. 2008, 139, 197–198. [Google Scholar] [CrossRef]
- A Cederberg, R.; A Valenza, J. Ethics and the electronic health record in dental school clinics. J. Dent. Educ. 2012, 76, 584–589. [Google Scholar]
- Szekely, D.G.; Milam, S.; A Khademi, J. Legal issues of the electronic dental record: Security and confidentiality. J. Dent. Educ. 1996, 60, 19–23. [Google Scholar]
- Da Costa, A.L.P.; Silva, A.A.; Pereira, C.B. Tele-orthodontics: Tool aid to clinical practice and continuing education. Dental Press J. Orthod. Rev. 2012, 16, 15–21. [Google Scholar]
- Cvrkel, T. The ethics of mHealth: Moving forward. J. Dent. 2018, 74, S15–S20. [Google Scholar] [CrossRef] [PubMed]
- Nutalapati, R.; Boyapati, R.; Jampani, N.D.; Dontula, B.S.K. Applications of teledentistry: A literature review and update. J. Int. Soc. Prev. Community Dent. 2011, 1, 37–44. [Google Scholar] [CrossRef]
- Cederberg, R.; Walji, M.; Valenza, J. Electronic Health Records in Dentistry: Clinical Challenges and Ethical Issues; Springer Science and Business Media LLC: Cham, Switzerland, 2014; pp. 1–12. [Google Scholar]
- Chambers, D.W. Position paper on digital communication in dentistry. J. Am. Coll. Dent. 2012, 79, 19–30. [Google Scholar] [PubMed]
- Neville, P.; Waylen, A.E. Social media and dentistry: some reflections on e-professionalism. Br. Dent. J. 2015, 218, 475–478. [Google Scholar] [CrossRef] [PubMed]
- Oakley, M.; Spallek, H. Social media in dental education: a call for research and action. J. Dent. Educ. 2012, 76, 279–287. [Google Scholar] [PubMed]
- Peltier, B.; Curley, A. The ethics of social media in dental practice: Ethical tools and professional responses. J. Calif. Dent. Assoc. 2013, 41, 507–513. [Google Scholar] [PubMed]
- Spallek, H.; Turner, S.P.; Donate-Bartfield, E.; Chambers, D.; McAndrew, M.; Zarkowski, P.; Karimbux, N. Social Media in the Dental School Environment, Part A: Benefits, Challenges, and Recommendations for Use. J. Dent. Educ. 2015, 79, 1140–1152. [Google Scholar]
- Sykes, L.M.; Harryparsad, A.; Evans, W.G.; Gani, F. Social Media and Dentistry: Part 8: Ethical, legal, and professional concerns with the use of internet sites by health care professionals. SADJ 2017, 72, 132–136. [Google Scholar]
- Swirsky, E.S.; Michaels, C.; Stuefen, S.; Halasz, M. Hanging the digital shingle. J. Am. Dent. Assoc. 2018, 149, 81–85. [Google Scholar] [CrossRef]
- Calberson, F.L.; Hommez, G.M.; De Moor, R.J. Fraudulent Use of Digital Radiography: Methods to Detect and Protect Digital Radiographs. J. Endod. 2008, 34, 530–536. [Google Scholar] [CrossRef]
- Indu, M.; Sunil, S.; Rathy, R.; Binu, M. Imaging and image management: A survey on current outlook and awareness in pathology practice. J. Oral Maxillofac. Pathol. 2015, 19, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, P. Photo-editing in Orthodontics: How Much is Too Much? Int. J. Orthod. 2015, 26, 17–23. [Google Scholar]
- Khelemsky, R. The ethics of routine use of advanced diagnostic technology. J. Am. Coll. Dent. 2011, 78, 35–39. [Google Scholar] [PubMed]
- Luther, F. Scientific Misconduct. J. Dent. Res. 2010, 89, 1364–1367. [Google Scholar] [CrossRef]
- Rao, S.; Singh, N.; Kumar, R.; Thomas, A. More than meets the eye: Digital fraud in dentistry. J. Indian Soc. Pedod. Prev. Dent. 2010, 28, 241. [Google Scholar] [CrossRef]
- Stieber, J.C.; Nelson, T.M.; E Huebner, C. Considerations for use of dental photography and electronic media in dental education and clinical practice. J. Dent. Educ. 2015, 79, 432–438. [Google Scholar]
- Wentworth, R.B. What ethical responsibilities do I have with regard to radiographs for my patients? J. Am. Dent. Assoc. 2010, 141, 718–720. [Google Scholar] [CrossRef]
- Peppet, S.R. Regulating the internet of things: first steps toward managing discrimination, privacy, security and consent. Tex. L. Rev. 2014, 93, 85. [Google Scholar]
- Hoffman, S. Employing e-health: the impact of electronic health records on the workplace. Kan. JL Pub. Pol’y 2009, 19, 409. [Google Scholar]
- Starkbaum, J.; Felt, U. Negotiating the reuse of health-data: Research, Big Data, and the European General Data Protection Regulation. Big Data Soc. 2019, 6, 2053951719862594. [Google Scholar] [CrossRef]
- Valenza, J.A.; Taylor, D.; Walji, M.F.; Johnson, C.W. Assessing the benefit of a personalized EHR-generated informed consent in a dental school setting. J. Dent. Educ. 2014, 78, 1182–1193. [Google Scholar] [PubMed]
- Benovsky, J. The Limits of Photography. Int. J. Philos. Stud. 2014, 22, 716–733. [Google Scholar] [CrossRef]
- Hopkins, R. Factive Pictorial Experience: What’s Special about Photographs? Nous 2010, 46, 709–731. [Google Scholar] [CrossRef]
- Alcarez, A.L. Epistemic function and ontology of analog and digital images. CA 2015, 13, 11. [Google Scholar]
- Cromey, D. Avoiding twisted pixels: ethical guidelines for the appropriate use and manipulation of scientific digital images. Sci. Eng. Ethic 2010, 16, 639–667. [Google Scholar] [CrossRef]
- Greysen, R.; Kind, T.; Chretien, K.C. Online Professionalism and the Mirror of Social Media. J. Gen. Intern. Med. 2010, 25, 1227–1229. [Google Scholar] [CrossRef]
- Ventola, C.L. Social Media and Health Care Professionals: Benefits, Risks, and Best Practices. J. Formul. Manag. 2014, 39, 491–520. [Google Scholar]
- Fitzgerald, C.; Hurst, S. Implicit bias in healthcare professionals: A systematic review. BMC Med. Ethics 2017, 18, 19. [Google Scholar] [CrossRef]
- Garrison, N.O.; Ibañez, G.E. Attitudes of Health Care Providers toward LGBT Patients: The Need for Cultural Sensitivity Training. Am. J. Public Heal. 2016, 106, 570. [Google Scholar] [CrossRef]
- McCarley, D.H. ADA Principles of Ethics and Code of Professional Conduct. Tex. Dent. J. 2011, 128, 728–732. [Google Scholar]
- Shetty, V.; Yamamoto, J.; Yale, K. Re-architecting oral healthcare for the 21st century. J. Dent. 2018, 74, S10–S14. [Google Scholar] [CrossRef] [PubMed]
- Shaw, D.M. Weeping and wailing and gnashing of teeth: The legal fiction of water fluoridation. Med Law Int. 2012, 12, 11–27. [Google Scholar] [CrossRef]
- Shaw, D.; Conway, D. Pascal’s Wager, infective endocarditis and the “no-lose” philosophy in medicine. Heart 2009, 96, 15–18. [Google Scholar] [CrossRef] [PubMed]
| No. | Match Search Terms | Pub Med | Web of Science | Scopus | Cinahl |
|---|---|---|---|---|---|
| 1 | (“big data” OR “digital data” OR “data linkage” OR “electronic health record*” OR “EHR” OR “digital*” OR “artificial intelligence” OR “data analytics” OR “information technology”) | 251,004 | 4,682,526 | 1,750,766 | 67,116 |
| 2 | (“dentist*” OR “dental *” OR “oral health” OR “orthodont*”) | 827,547 | 1,409,796 | 613,348 | 158,231 |
| 3 | (“ethic *” OR “moral*”) | 334,537 | 582,299 | 528,738 | 98,246 |
| 4 | 1 AND 2 AND 3 | 190 | 186 | 71 | 63 |
| Author, Year, Country | Design | Participants | Technology Discussed | Field of Application | Ethical Issues |
|---|---|---|---|---|---|
| Boden (2008), USA | Theoretical | Digital transfer of patient records | Dental practice | Justice and autonomy- high charges for the patient prevent beneficial use of records for future patient treatment | |
| Calberson et al. (2008), Belgium | Theoretical | Digital radiography | General | Fraudulent use of radiographs | |
| Cederberg and Valenza (2012), USA | Theoretical | EHR (in dental schools) | Dental school | Justice, patient privacy and security, shift in doctor patient relationship, misconduct from students | |
| Chambers (2012), USA | Theoretical | Digital Communication | Dental practice | Shift in doctor patient relationship, patient privacy and security, professionalism | |
| Cvrker (2018), USA | Theoretical | mHealth | General | Patient access, data ownership, patient privacy and security, bystanders | |
| da Costa et al. (2012), Brazil | Theoretical | Teleorthodontics | General | Patient privacy and security | |
| Day et al. (2018), UK | Feasibility Study | Birth cohort in the United Kingdom | Data linkage | Research | Anonymization, data ownership |
| Eng et al. (2012), USA | Theoretical | Personalized dentistry | General | Discrimination, confidentiality | |
| Gross et al. (2019), Germany | Theoretical | Digitalization in dentistry | General | Shift in doctor patient relationship, data literacy, responsibility and accountability for AI, digital footprint | |
| Indu et al. (2015), India | Empirical | A sample of postgraduate students and teaching faculties of oral pathology in India | Digital photography | General | Anonymity and security |
| Jampani et al (2011), India | Theoretical | Teledentistry | General | Confidentiality, patient privacy and security, consent | |
| Kapoor (2015), India | Empirical | Digital photography and radiology | General | Fraudulent use of radiographs/photographs, scientific misconduct | |
| Khelemsky (2011), USA | Theoretical | CBCT | Dental practice | Harm to patient, consent | |
| Knott (2013), UK | Theoretical | ICT | Dental practice | Anonymity, data security, patient privacy | |
| Luther (2010), UK | Theoretical | Digital forensics | Research | Fraudulent use of images, scientific misconduct, | |
| Neville and Waylen (2015), UK | Theoretical | Social Media | Dental practice | Shift in doctor patient relationship, patient Confidentiality, privacy, anonymity | |
| Oakley and Spallek (2012), USA | Theoretical | Social Media | Dental School | Shift in doctor patient relationship, patient privacy and confidentiality, miscommunication, boundary violation | |
| Peltier and Curley (2013), USA | Theoretical | Social Media | Dental practice | Dishonest/unlawful advertising, patient confidentiality | |
| Rao et al. (2010), India | Empirical | A sample of randomly selected clinicians in India | Digital photography | General | Fraudulent use of photographs, scientific misconduct |
| Spallek er al. (2015), USA | Theoretical | Social Media | Dental School | Shift in doctor patient relationship, patient privacy and confidentiality, miscommunication, boundary violation | |
| Stieber et al. (2015), USA | Theoretical | Electronic media and digital photography | Dental School | Patient privacy and confidentiality, autonomy and consent | |
| Swirsky at al. (2018), USA | Theoretical | Search engine optimization | Dental practice | Beneficence, autonomy, consent, conflict of interest and undue influence | |
| Sykes et al (2017), South Africa | Theoretical | Social Media | Dental practice | Patient privacy, anonymity, confidentiality and consent, professionalism, shift in patient doctor relationship, misleading advertisement | |
| Szekely et al. (1996), USA | Theoretical | EHR | Dental practice | Patient privacy and confidentiality, security | |
| Wenworth (2010), USA | Theoretical | Digital Radiography | Dental practice | Patient privacy and confidentiality, misleading advertisement | |
| Zijlstra-Shaw and Stokes (2018), UK | Theoretical | Big Data analytics (in dental education) | Dental school | Consent and data ownership |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Favaretto, M.; Shaw, D.; De Clercq, E.; Joda, T.; Elger, B.S. Big Data and Digitalization in Dentistry: A Systematic Review of the Ethical Issues. Int. J. Environ. Res. Public Health 2020, 17, 2495. https://doi.org/10.3390/ijerph17072495
Favaretto M, Shaw D, De Clercq E, Joda T, Elger BS. Big Data and Digitalization in Dentistry: A Systematic Review of the Ethical Issues. International Journal of Environmental Research and Public Health. 2020; 17(7):2495. https://doi.org/10.3390/ijerph17072495
Chicago/Turabian StyleFavaretto, Maddalena, David Shaw, Eva De Clercq, Tim Joda, and Bernice Simone Elger. 2020. "Big Data and Digitalization in Dentistry: A Systematic Review of the Ethical Issues" International Journal of Environmental Research and Public Health 17, no. 7: 2495. https://doi.org/10.3390/ijerph17072495
APA StyleFavaretto, M., Shaw, D., De Clercq, E., Joda, T., & Elger, B. S. (2020). Big Data and Digitalization in Dentistry: A Systematic Review of the Ethical Issues. International Journal of Environmental Research and Public Health, 17(7), 2495. https://doi.org/10.3390/ijerph17072495





