Interventions to Reduce the Risk of Cardiovascular Disease among Workers: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Search Strategy and Ethical Considerations
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
2.4. Quality Assessment
2.5. Data Analysis
3. Results
3.1. Study Characteristics
3.2. Characteristics of the Interventions
3.3. Risk of Bias
3.4. Synthesis by Outcomes
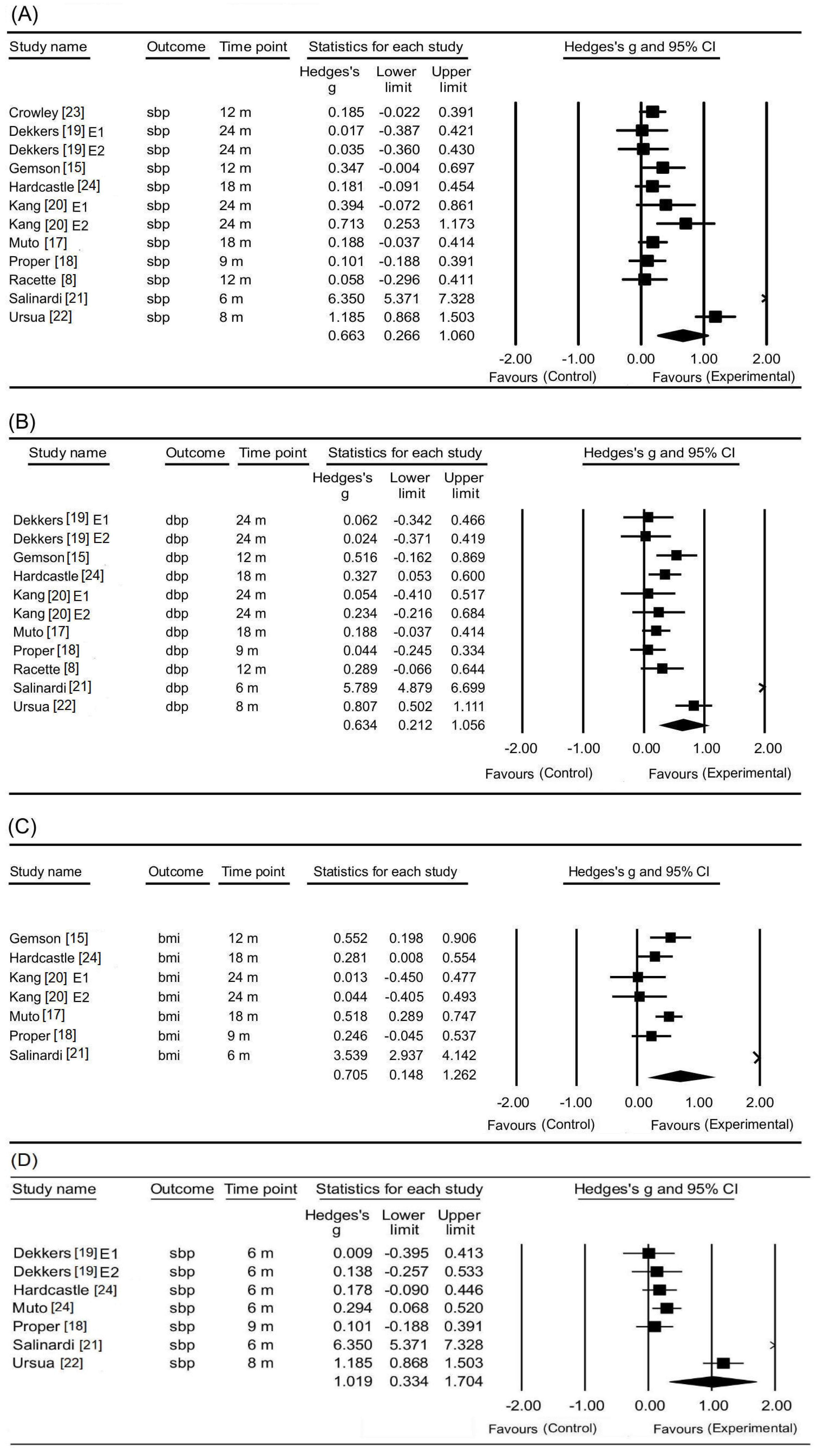
3.4.1. Changes in Systolic Blood Pressure
3.4.2. Changes in Diastolic Blood Pressure
3.4.3. Changes in BMI
3.4.4. Changes in Weight
3.4.5. Changes in LDL-Cholesterol
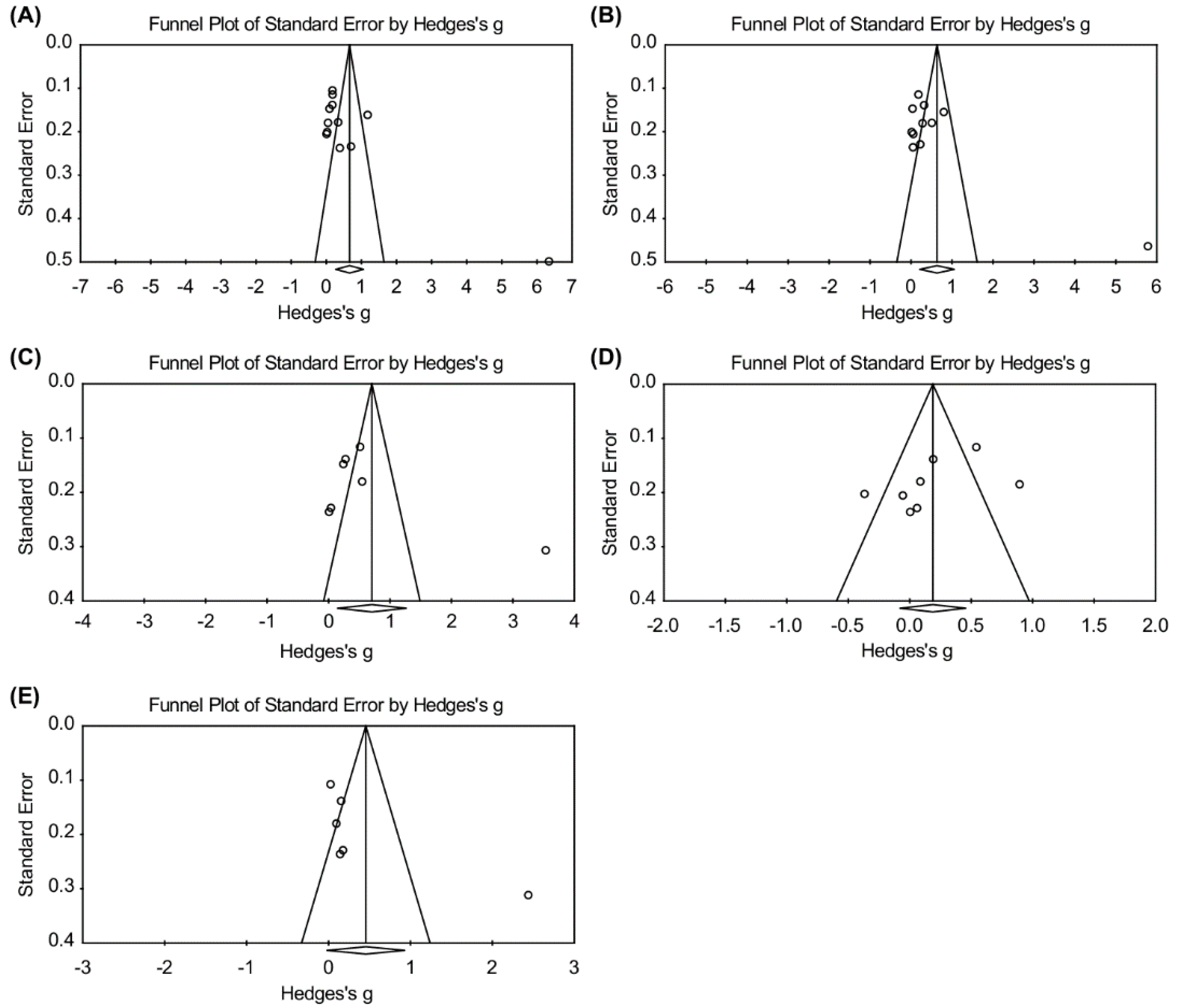
3.5. Publication Bias
3.6. Subgroup Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A. Study Quality Ratings
| Controlled Trial | Cambein [16]) | Crowley [23] | Dekkers [19] | Gemson [15]) | Hardcastle [24] | Kang [20] | Muto [17] | Proper [18] | Racette [8] | Salinardi [21] | Ursua [22] |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1.1 The study addresses an appropriate and clearly focused question. | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 1.2 The assignment of subjects to treatment groups is randomized. | Y | Y | Y | N/A | Y | Y | Y | Y | Y | Y | Y |
| 1.3 An adequate concealment method is used. | N | N | Y | N/A | Y | N | N | Y | N | N | N |
| 1.4 The design keeps subjects and investigators ‘blind’ about treatment allocation. | N | Y | Y | N/A | Y | ? | N | Y | N | N | N |
| 1.5 The treatment and control groups are similar at the start of the trial. | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 1.6 The only difference between groups is the treatment under investigation. | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 1.7 All relevant outcomes are measured in a standard, valid, and reliable way. | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 1.8 What percentage of the individuals or clusters recruited into each treatment arm of the study dropped out before the study was completed? | Overall 38.7% (2 yrs) | Overall 9.1% (1 yrs) | Overall 29.0% (1 yr)/ 48.9% (2 yr) | Overall 74.5% (1 yr) | Overall 36.8% (6 m)/ 34.7% (1 yr) | 8.0%* (1 yr)/ Overall 0.0% (2 yr) | Overall 7.4% (18m) | Overall 33.3% (9m) | Overall 18.5% (1 yr) | Overall 74.7% (6 m) | Overall 40.7% (8 m) |
| 1.9 All the subjects are analyzed in the groups to which they were randomly allocated (often referred to as intention to treat analysis). | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 1.10 Where the study is carried out at more than one site, results are comparable for all sites. | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Overall assessment of the study | - | + | ++ | + | ++ | + | + | ++ | + | + | + |
References
- World Health Organization. The Top 10 Causes of Death 2012. Available online: http://www.who.int/mediacentre/factsheets/fs310/en/ (accessed on 10 December 2015).
- Centers for Disease Control and Prevention. Chronic Diseases Factbook. Available online: http://www.cdc.go.kr/ (accessed on 10 December 2015).
- Korea Occupational Safety and Health Agency. Occupational Injuries and Illnesses for 2011 [Internet]. Gwacheon: Ministry of Employment and Labor. Available online: http://www.kosha.or.kr/www/boardView.do?contentId=343906&menuId=554&boardType=A2/ (accessed on 10 December 2015).
- Kim, N.J. Relation between Employees’ Life Patterns and Health Conditions. Korean J. Health Educ. Promot. 2007, 24, 63–75. [Google Scholar]
- Hwang, W.J.; Hong, O. Work-related cardiovascular disease risk factors using a socioecological approach: Implications for practice and research. Eur. J. Cardiovasc. Nurs. 2012, 11, 114–126. [Google Scholar] [CrossRef] [PubMed]
- Schultz, A.B.; Edington, D.W. Metabolic Syndrome in a Workplace: Prevalence, Co-morbidities, and Economic Impact. Metab. syndr. Relat. Disord. 2009, 7, 459–468. [Google Scholar] [CrossRef] [PubMed]
- Sook, C.E.; Ja, J.K. The Management Strategies of Metabolic Syndrome among Workers through the Literature Review. Korean J. Occup. Health Nurs 2005, 14, 138–152. [Google Scholar]
- Racette, S.B.; Deusinger, S.S.; Inman, C.L.; Burlis, T.L.; Highstein, G.R.; Buskirk, T.D.; Steger-May, K.; Peterson, L.R. Worksite Opportunities for Wellness (WOW): Effects on Cardiovascular Disease Risk Factors After 1 Year. Prev. Med. 2009, 49, 108–114. [Google Scholar] [CrossRef] [PubMed]
- Hwang, W.J.; Park, Y.H.; Kim, J.A. A Systematic Review of Interventions for Workers with Cardiovascular Disease Risk Factors: Using an Ecological Model. Korean J. Occup. Health Nurs. 2016, 25, 41–54. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-analysis: The PRISMA Statement. PloS Med. 2009, 151, 264–269. [Google Scholar]
- Scottish Intercollegiate Guidelines Network. Sign 50: A Guideline Developer’s Handbook. Available online: http://www.sign.ac.uk (accessed on 1 August 2019).
- Weibe, N.; Vandermeer, B.; Platt, R.W.; Klassen, T.P.; Moher, D.; Barrowman, N.J. A Systematic Review Identifies a Lack of Standardization in Methods for Handling Missing Variance Data. J. Clin. Epidemiol. 2011, 59, 342–353. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. Cochrane, 2019. Available online: www.training.cochrane.org/handbook (accessed on 10 January 2019).
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in Meta-analysis Detected by Simple, Graphical test. BMJ 1997, 13, 629–634. [Google Scholar] [CrossRef]
- Gemson, D.H.; Commisso, R.; Fuente, J.; Newman, J.; Benson, S. Promoting Weight Loss and Blood Pressure Control at Work: Impact of an Education and Intervention Program. J. Occup. Environ. Med. 2008, 50, 272–281. [Google Scholar] [CrossRef]
- Cambien, F.; Richard, J.; Ducimetiere, P.; Warnet, J.; Kahn, J. The Paris Cardiovascular Risk Factor Prevention Trial. Effects of Two Years of Intervention in a Population of Young Men. J. Epidemiol. Commun. Health 1981, 35, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Muto, T.; Yamauchi, K. Evaluation of a Multicomponent Workplace Health Promotion Program Conducted in Japan for Improving Employees’ Cardiovascular Disease Risk Factors. Prev. Med. 2001, 33, 571–577. [Google Scholar] [CrossRef] [PubMed]
- Proper, K.I.; Hildebrandt, V.H.; Van der Beek, A.J.; Twisk, J.W.; Van Mechelen, W. Effect of Individual Counseling on Physical Activity Fitness and Health: A Randomized Controlled Trial in a Workplace Setting. Am. J. Prev. Med. 2003, 24, 218–226. [Google Scholar] [CrossRef]
- Dekkers, J.C.; van Wier, M.F.; Ariens, G.A.; Hendriksen, I.J.; Pronk, N.P.; Smid, T.; van Mechelen, W. Comparative Effectiveness of Lifestyle Interventions on Cardiovascular Risk Factors among a Dutch Overweight Working Population: A Randomized Controlled Trial. BMC Public Health 2011, 11, 49. [Google Scholar] [CrossRef]
- Kang, J.Y.; Cho, S.W.; Sung, S.H.; Park, Y.K.; Paek, Y.M.; Choi, T.I. Effect of a Continuous Diabetes Lifestyle Intervention Program on Male Workers in Korea. Diabetes Res. Clin. Pract. 2010, 90, 26–33. [Google Scholar] [CrossRef]
- Salinardi, T.C.; Batra, P.; Roberts, S.B.; Urban, L.E.; Robinson, L.M.; Pittas, A.G.; Lichtenstein, A.H.; Deckersbach, T.; Saltzman, E.; Das, S.K. Lifestyle Intervention Reduces Body Weight and Improves Cardiometabolic Risk Factors in Worksites. Am. J. Clin. Nutr. 2013, 97, 667–676. [Google Scholar] [CrossRef]
- Ursua, R.A.; Aguilar, D.E.; Wyatt, L.C.; Trinh-Shevrin, C.; Gamboa, L.; Valdellon, P.; Perrella, E.G.; Dimaporo, M.Z.; Nur, P.Q.; Tandon, S.D.; et al. A Community Health Worker Intervention to Improve Blood Pressure among Filipino Americans with Hypertension: A Randomized Controlled Trial. Prev. Med. Rep. 2018, 11, 42–48. [Google Scholar] [CrossRef]
- Crowley, M.J.; Powers, B.J.; Olsen, M.K.; Grubber, J.M.; Koropchak, C.; Rose, C.M.; Gentry, P.; Bowlby, L.; Trujillo, G.; Maciejewski, M.L.; et al. The Cholesterol, Hypertension, and Glucose Education (CHANGE) Study: Results from a Randomized Controlled Trial in African Americans with Diabetes. Am. Heart J. 2013, 166, 179–186. [Google Scholar] [CrossRef]
- Hardcastle, S.J.; Taylor, A.H.; Bailey, M.P.; Harley, R.A.; Hagger, M.S. Effectiveness of a Motivational Interviewing Intervention on Weight Loss, Physical Activity and Cardiovascular Disease Risk Factors: A Randomized Controlled Trial With a 12-month Post-intervention Follow-up. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 40. [Google Scholar] [CrossRef]
- Chen, L.; Pei, J.H.; Kuang, J.; Chen, H.M.; Chen, Z.; Li, Z.W.; Yang, H.Z. Effect of Lifestyle Intervention in Patients with Type 2 Diabetes: A Meta-analysis. Metabolism 2013, 64, 338–347. [Google Scholar] [CrossRef]
- Zhang, X.; Devlin, H.M.; Smith, B.; Imperatore, G.; Thomas, W.; Lobelo, F.; Ali, M.K.; Norris, K.; Gruss, S.; Bardenheier, B.; et al. Effect of Lifestyle Interventions on Cardiovascular Risk Factors Among Adults without Impaired Glucose Tolerance or Diabetes: A Systematic Review and Meta-analysis. PLoS ONE 2017, 12, e0176436. [Google Scholar] [CrossRef] [PubMed]
- Angermayr, L.; Melchart, D.; Linde, K. Multifactorial Lifestyle interventions in the Primary and Secondary Prevention of Cardiovascular Disease and Type 2 Diabetes Mellitus: A Systematic Review of Randomized Controlled Trials. Ann. Behav. Med. 2010, 40, 49–64. [Google Scholar] [CrossRef] [PubMed]
- Artinian, N.T.; Fletcher, G.F.; Mozaffarian, D.; Kris-Etherton, P.; Van Horn, L.; Lichtenstein, A.H.; Kumanyika, S.; Kraus, W.E.; Fleg, J.L.; Redeker, N.S.; et al. American Heart Association Prevention Committee of the Council on Cardiovascular Nursing. Interventions to Promote Physical Activity and Dietary Lifestyle Changes for Cardiovascular Risk Factor Reduction in Adults: A Scientific Statement from the American Heart Association. Circulation 2010, 122, 406–441. [Google Scholar] [PubMed]
- Bouton, M.E. Why Behavior Change is Difficult to Sustain. Prev. Med. 2014, 68, 29–36. [Google Scholar] [CrossRef]
- Hwang, W.J.; Kim, J.A. Developing a Health-Promotion Program Based on the Action Research Paradigm to Reduce Cardiovascular Disease Risk Factors among Blue Collar Workers. Int. J. Environ. Res. Public Health 2019, 16, 4958. [Google Scholar] [CrossRef]
- LaMontagne, A.D.; Keegel, T.; Louie, A.; Ostry, A.; Landsbergis, P.A. A Systematic Review of the Job-stress Intervention Evaluation Literature, 1990–2005. Int. J. Occup. Environ. Health 2007, 13, 268–280. [Google Scholar] [CrossRef]
- Montano, D.; Hoven, H.; Siegrist, J. Effects of Organizational-level Interventions at Work on Employees’ Health: A Systematic Review. BMC Public Health 2014, 14, 135. [Google Scholar] [CrossRef]

| 1st Author (yr); Ref country | Design | Participants | Settings | No of Participants | Age(yr) Mean ± SD/ Gender = Male (%) | Intervention | Session/ Type | Length Time (minutes) | Duration (Months)/ Follow up Data Points | Outcomes | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cambein [16] (1981); France | 2-arm RCT | Civil servants | Administration department | Exp = 663 Con = 629 | Exp 29 ± 3 Con 29 ± 3/ Gender = Not reported | I: Individual lifestyle change program: diet, smoking, physical activity using audio and visual materials C: Not reported | Not reported/ Remote | Not reported | 12 months/ Baseline, 12 months, 24 months | Ht, BP(S), Smoking Cholesterol | - |
| Crowley [23] (2013); USA | 2-arm RCT | African Americans with type 2 DM Employees | 2 clinics | Exp = 182 Con = 177 | Exp 57 ± 12 Con 56 ± 12/ Gender = Male Intervention: 31%, Control:25% | I: Telephone-based nurse-delivered intervention for DM self-management and medication adherence C: Written education materials | Total 12, average 9.9/ Remote | 17.1 ± 7.3 | 12 months/Baseline, 12 months | Primary: BP(S), HbA1c, LDL-C Secondary: medication adherence | + |
| Dekkers [19] (2011); Netherlands | 3-arm RCT | Adults with over-weight (BMI ≥ 25 kg/m2) Employees | 7 companies (IT, hospital, Insurance, and bank) | Exp1 = 91 Exp2 = 93 Con = 92 | Exp1 43 ± 10 Exp2 45 ± 9 Con. 44 ± 9/ Gender = Male Overall: 69.2% | I: Distance-counseling lifestyle intervention by dietician and movement scientists for weight, physical activity and healthy diet Exp1: Phone; Exp2: Internet C: Usual care | Not reported, 10 (max)/ Remote | Not reported | 6 months/ Baseline, 6 months, 24 months | BP(S/D), BMI, Wt. Ht, WC, TC, Aerobic fitness level: [VO2 max], Sum of skinfolds | ++ |
| Gemson [15] (2008); USA | Quasi-experimental | Hypertension adults Employees (BP ≥ 140 or ≥ 90) | 5 sites, 7 financial companies | Exp = 47 (IT, hospital, Insurance, and bank) | Exp 45 ± 9 Con 48 ± 12/ Gender = Male Intervention: 46.8%, Control:51.1% | I: Tailored blood pressure and weight reduction program by nurse based on BP/BMI measuring + pedometer C: Information except physical information | Not available/ Remote | Not available | 12 months/ Baseline, 12 months | BP(S/D), BMI, Wt. physical activity, and diet and nutrition behaviors (self-reported) | + |
| Hardcastle [24] (2013); USA | 2 -arm RCT | Adults with CVD risk factors | Primary care center | Exp = 203 Con = 131 | Exp 50 ± 1 Con 50 ± 1/ Gender = Not reported | I: Individual motivational intervention by physical activity specialist and dietician for physical activity and nutrition C: Written information | Total 5, average 2/ Remote +on-site | 20–30 | 6 months/ Baseline, 6 months, 18 months | BP(S/D), BMI, Wt, TC, HDL/LDL-C, TG, Physical activity, Nutrition intake | + |
| Kang [20] (2010); Korea | 3 -arm RCT | Male workers with DM risk factors (FPG ≥ 5.6 mmol) | Hospital | Exp1 = 25 Exp2 = 25 Con = 75 | Exp1 46 ± 6 Exp2 46 ± 5 Con 47 ± 6/ Gender = Male (100%) | I: Lifestyle intervention for main intervention (3 months) + e-mail nutrition follows- up Exp1: one-year follow-up Exp2: two-year follow-up C: No intervention | 5 (counseling)/ Remote | 20-30/ | 12 months/ Baseline, 24 months | BP(S/D), BMI, Wt, TC, HDL/LDL-C, WC, HbA1c, Nutrition intake | + |
| Muto [17] (2001); Japan | 2 -arm RCT | Blue-collar male workers with at least one abnormality in CVD risk factors | Building maintenance company’s worksite branches | Exp = 152 Con = 150 | Exp 42 ± 5 Con 43 ± 3/ Gender: Male (100%) | I: Diet and physical activity intervention by health providers (physician, exercise trainer, and coordinators). Individual, group discussion, practice, etc. C: No intervention, written information + annual health checkup | Not available/ Remote +on site | 4 days, Every 3 month | 12 months/ Baseline, 6, 12 months | BP(S/D), BMI, Wt TC, HDL-C, TG, FB | + |
| Proper [18] (2003); Netherlands | 2-arm RCT | Office employees | 3 municipal service | Exp = 131 Con = 168 | Exp 44 ± 1 Con 44 ± 1/ Gender = Male Intervention: 74.4%, Control:61.5% | I: Individual counselling on physical activity, nutrition and lifestyle factors; Individual based on PACE protocol C: Written information | 7/ Remote +on-site | 20 | 9 months/ Baseline, 9 months | Primary: Energy expenditure, Sport and Leisure-time index, Submaximal HR, Secondary: BMI, TC, BP (S/D), Body fat | ++ |
| Racette [8] (2009); USA | 2 -arm CohortRCT | Employees with smoke, pre-existing disease (hypertension, diabetes), and medication use | 2 Medical center worksites | Exp = 84 Con = 67 | Overall 45 ± 9/ Gender = Male Intervention: 23.5%, Control:21.9% | I: Assessment + physical activity and dietary intervention, individual goal setting, group discussion, etc. C: Assessment only | Not reported/ On-site | Not reported | 12 months/ Baseline, 6 months, 12 months | BMI, Wt, BP (S/D), TC, HDL/LDL– C, Body fat, glucose | + |
| Salinardi [21] (2013); USA | 2 -arm RCT | Employees with BMI ≥ 25 kg/m2 | 4 worksites Office-based company | Exp = 94 Wait-listed group = 39 | Exp 45 ± 1 Con 39 ± 1/ Gender = Male Intervention: 22%, Control:51% | I: Group-based multi-component lifestyle intervention on weight loss and CVD risk factors prevention C: Wait-list weight loss | 19/ On-site | 60 | 6 months/ Baseline, 6 months | Primary: Wt Secondary: BP (S/D), BMI BP, TC, TG, glucose HDL/LDL– C | + |
| Ursua [22] (2018); USA | 2 -arm RCT | Filipino Americans with hypertension (BP ≥ 140 or ≥ 90) | A metropolitan | Exp = 112 Con = 128 | Exp 54 ± 10 Con 54 ± 10/ Gender = Male Intervention: 39.3%, Control:31.5% | I: CHW led education by Filipino immigrants. Mixed individual and group activities C: Wallet card information | 8 (4 group and 4 individual education)/on-site | 90 | 4 months/ Baseline, 4, 8 months | BP (S/D) | + |
| Outcomes | Final Time Point | T1 (12 months <) | T2 (12 months ≥) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Effect Size | Heterogeneity | Effect Size | Heterogeneity | Effect Size | Heterogeneity | ||||||||||
| No. of Studies | Hedges’ | 95% CI | I2 | P | No. of Studies | Hedges’ | 95% CI | I2 | P | No. of Studies | Hedges’ | 95% CI | I2 | P | |
| SBP | 10 | 0.66 | 0.27, 1.60 | 94.20 | 0.000 | 6 | 1.02 | 0.33, 1.70 | 96.63 | 0.000 | 7 | 0.20 | 0.10, 0.31 | 2.92 | 0.41 |
| DBP | 9 | 0.63 | 0.21, 1.06 | 93.73 | 0.000 | 6 | 0.91 | 0.27, 1.54 | 96.12 | 0.000 | 6 | 0.23 | 0.11, 0.35 | 0.00 | 0.60 |
| BMI | 6 | 0.71 | 0.15, 1.26 | 94.61 | 0.000 | 4 | 1.11 | 0.22, 2.01 | 97.08 | 0.000 | 4 | 0.37 | 0.25, 0.51 | 45.39 | 0.120 |
| Weight | 6 | 0.19 | −0.78, 0.46 | 78.45 | 0.000 | 4 | 0.16 | −0.29, 0.61 | 87.80 | 0.000 | 6 | 0.19 | −0.08, 0.46 | 78.45 | 0.000 |
| LDL | 5 | 0.46 | −0.02, 0.93 | 90.83 | 0.000 | 2 | 1.28 | −0.96, 3.52 | 97.78 | 0.000 | 4 | 0.10 | −0.04, 0.23 | 0.94 | 0.000 |
| Outcomes | At the Final Point | ||
|---|---|---|---|
| No. of Studies | Egger’s Regression | ||
| t | p-Value | ||
| SBP | 10 | 2.54 | 0.029 |
| DBP | 9 | 2.24 | 0.052 |
| BMI | 6 | 1.17 | 0.292 |
| Weight | 6 | 1.52 | 0.178 |
| LDL | 5 | 1.82 | 0.143 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hwang, W.J.; Kang, S.J. Interventions to Reduce the Risk of Cardiovascular Disease among Workers: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 2267. https://doi.org/10.3390/ijerph17072267
Hwang WJ, Kang SJ. Interventions to Reduce the Risk of Cardiovascular Disease among Workers: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2020; 17(7):2267. https://doi.org/10.3390/ijerph17072267
Chicago/Turabian StyleHwang, Won Ju, and Soo Jin Kang. 2020. "Interventions to Reduce the Risk of Cardiovascular Disease among Workers: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 17, no. 7: 2267. https://doi.org/10.3390/ijerph17072267
APA StyleHwang, W. J., & Kang, S. J. (2020). Interventions to Reduce the Risk of Cardiovascular Disease among Workers: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 17(7), 2267. https://doi.org/10.3390/ijerph17072267






