Demoralization and Its Relationship with Depression and Hopelessness in Suicidal Patients Attending an Emergency Department
Abstract
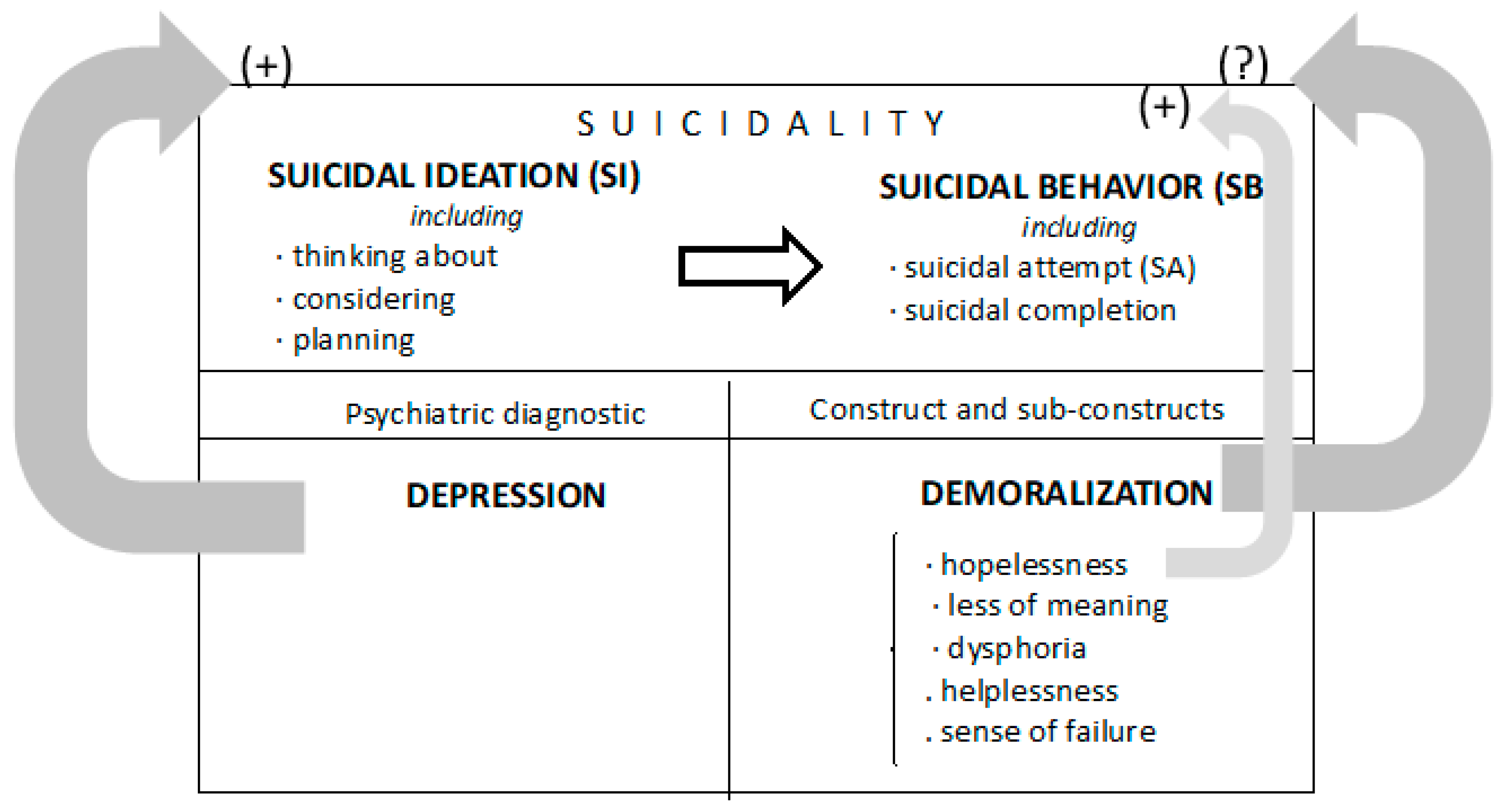
1. Introduction
2. Methods
2.1. Sample
2.2. Procedure
2.3. Instruments
2.4. Statistical Analyses
3. Results
3.1. Descriptive and Sociodemographic Characteristics
3.2. Demoralization and SI/SA, and Demoralization and Depression
3.3. Demoralization and Hopelessness
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Larkin, G.L.; Beautrais, A.L. Emergency Departments Are Underutilized Sites for Suicide Prevention. Crisis 2010, 31, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Ting, S.A.; Sullivan, A.F.; Boudreaux, E.D.; Miller, I.; Camargo, C.A. Trends in US emergency department visits for attempted suicide and self-inflicted injury, 1993–2008. Gen. Hosp. Psychiatry 2012, 34, 557–565. [Google Scholar] [CrossRef] [PubMed]
- Posner, K.; Oquendo, M.A.; Gould, M.; Stanley, B.; Davies, M. Columbia Classification Algorithm of Suicide Assessment (C-CASA): Classification of suicidal events in the FDA’s pediatric suicidal risk analysis of antidepressants. Am. J. Psychiatry 2007, 164, 1035–1043. [Google Scholar] [CrossRef]
- Beautrais, A.L. Further suicidal behavior among medically serious suicide attempters. Suicide Life Threat. Behav. 2004, 34, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Gibb, S.J.; Beautrais, A.L.; Fergusson, D.M. Mortality and further suicidal behaviour after an index suicide attempt: A 10-year study. Aust. N. Z. J. Psychiatry 2005, 39, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Larkin, G.L.; Beautrais, A.L.; Gibb, S.; Laing, N. The epidemiology of presentations for suicidal ideation to the emergency department. Acad. Emerg. Med. 2008, 15, S208–S209. [Google Scholar]
- Arias, S.A.; Miller, I.; Camargo, C.A., Jr.; Sullivan, A.F.; Goldstein, A.B.; Allen, M.H.; Manton, A.P.; Boudreaux, E.D. Factors Associated With Suicide Outcomes 12 Months After Screening Positive for Suicide Risk in the Emergency Department. Psychiat. Serv. 2015, 67, 206–213. [Google Scholar] [CrossRef]
- Claassen, C.A.; Larkin, G.L. Occult suicidality in an emergency department population. Br. J. Psychiatry 2005, 186, 352–353. [Google Scholar] [CrossRef]
- Kemball, R.S.; Gasgarth, R.; Johnson, B.; Patil, M.; Houry, D. Unrecognized suicidal ideation in ED patients: Are we missing an opportunity? Am. J. Emerg. Med. 2008, 26, 701–705. [Google Scholar] [CrossRef]
- Marchesi, C.; Maggini, C. Socio-demographic and clinical features associated with demoralization in medically ill in-patients. Soc. Psychiatry Psychiatr. Epidemiol. 2007, 42, 824–829. [Google Scholar] [CrossRef]
- Tecuta, L.; Tomba, E.; Grandi, S.; Fava, G.A. Demoralization: A systematic review on its clinical characterization. Psychol. Med. 2015, 45, 673–691. [Google Scholar] [CrossRef] [PubMed]
- Frank, J.D. Psychotherapy: The restoration of morale. Am. J. Psychiatry 1974, 131, 271–274. [Google Scholar] [CrossRef] [PubMed]
- De Figueiredo, J.M.; Frank, J.D. Subjective incompetence, the clinical hallmark of demoralization. Compr. Psychiatry 1982, 23, 353–363. [Google Scholar] [CrossRef]
- Engel, E.L. A life setting conducive to illness: The giving-up—Give-up complex. Bull. Menn. Clin. 1968, 32, 355–365. [Google Scholar] [CrossRef] [PubMed]
- Fava, G.A.; Freyberger, H.J.; Bech, P.; Christodoulou, G.; Sensky, T.; Theorell, T.; Wise, T.N. Diagnostic criteria for use in psychosomatic research. Psychother. Psychosom. 1995, 63, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Mangelli, L.; Fava, G.A.; Grandi, S.; Grassi, L.; Ottolini, F.; Porcelli, P.; Rafanelli, C.; Rigatelli, M.; Sonino, N. Assessing demoralization and depression in the setting of medical disease. J. Clin. Psychiatry 2005, 66, 391–394. [Google Scholar] [CrossRef] [PubMed]
- Fava, G.; Fabbri, S.; Sirri, L.; Wise, T. Psychological factors affecting medical condition: A new proposal for DSM-V. Psychosomatics 2007, 48, 103–111. [Google Scholar] [CrossRef]
- Grassi, L.; Caruso, R.; Sabato, S.; Massarenti, S.; Nanni, M.G. The UniFe Psychiatry Working Group Coauthors. Psychosocial screening and assessment in oncology and palliative care settings. Front. Psychol. 2015, 5, 1485. [Google Scholar] [CrossRef]
- Kissane, D.W.; Clarke, D.M.; Street, A.F. Demoralization Syndrome—A relevant psychiatric diagnosis for palliative care. J. Palliat. Care 2001, 17, 12–21. [Google Scholar] [CrossRef]
- Clarke, D.M.; Kissane, D.W. Demoralization: Its phenomenology and importance. Aust. N. Z. J. Psychiatry 2002, 36, 733–742. [Google Scholar] [CrossRef]
- Kissane, D.W.; Wein, S.; Love, A.; Lee, X.; Kee, P.; Clarke, D.M. The Demoralization Scale: A report of its development and preliminary validation. J. Palliat. Care 2004, 20, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Slavney, P.R. Diagnosing demoralization in consultation psychiatry. Psychosomatics 1999, 40, 325–329. [Google Scholar] [CrossRef]
- Slavney, P. Diagnosing demoralization in consultation psychiatry: Reply to Dr. de Figueiredo. Psychosomatics 2000, 41, 449–450. [Google Scholar]
- Kissane, D. Distress, demoralization and depression in palliative care. Curr. Ther. 2000, 41, 14–19. [Google Scholar]
- Kissane, D.W.; Kelly, B.J. Demoralisation, depression and desire for death: Problems with the Dutch guidelines for euthanasia of the mentally ill. Aust. N. Z. J. Psychiatry 2000, 34, 325–333. [Google Scholar] [CrossRef] [PubMed]
- Robinson, S.; Kissane, D.W.; Brooker, J.; Hempton, C.; Burney, S. The relationship between poor quality of life and desire to hasten death: A multiple mediation model examining the contributions of depression, demoralization, loss of control, and low self-worth. J. Pain Symptom Manag. 2017, 53, 243–249. [Google Scholar] [CrossRef]
- Fang, C.K.; Chang, M.C.; Chen, P.J.; Lin, C.C.; Chen, G.S.; Lin, J.; Hsieh, R.K.; Chang, Y.F.; Chen, H.W.; Wu, C.L.; et al. A correlational study of suicidal ideation with psychological distress, depression, and demoralization in patients with cancer. Support. Care Cancer 2014, 22, 3165–3174. [Google Scholar] [CrossRef]
- Tang, P.L.; Wang, H.H.; Chou, F.H. A Systematic Review and Meta-Analysis of Demoralization and Depression in Patients With Cancer. Psychosomatics 2015, 56, 634–643. [Google Scholar] [CrossRef]
- Vehling, S.; Kissane, D.W.; Lo, C.; Glaesmer, H.; Hartung, T.J.; Rodin, G.; Mehnert, A. The association of demoralization with mental disorders and suicidal ideation in patients with cancer. Cancer 2017, 123, 3394–3401. [Google Scholar] [CrossRef]
- Butterworth, P.; Fairweather, K.A.; Anstey, K.J.; Windsor, T.D. Hopelessness, demoralization and suicidal behaviour: The backdrop to welfare reform in Australia. Aust. N. Z. J. Psychiatry 2006, 40, 648–656. [Google Scholar] [CrossRef]
- Drake, R.E.; Gates, C.; Whitaker, A.; Cotton, P.G. Suicide among schizophrenics: A review. Compr. Psychiatry 1985, 26, 90–100. [Google Scholar] [CrossRef]
- Berardelli, I.; Sarubbi, S.; Rogante, E.; Hawkins, M.; Cocco, G.; Erbuto, D.; Lester, D.; Pompili, M. The Role of Demoralization and Hopelessness in Suicide Risk in Schizophrenia: A Review of the Literature. Medicina (Kaunas) 2019, 55, 200. [Google Scholar] [CrossRef] [PubMed]
- Lau, R.; Morse, C.A.; Macfarlane, S. Psychological factors among elderly women with suicidal intentions or attempts to suicide: A controlled comparison. J. Women Aging 2010, 22, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Catanese, A.A.; John, M.S.; Di Battista, J.; Clarke, D.M. Acute Cognitive Therapy in Reducing Suicide Risk Following a Presentation to an Emergency Department. Behav. Chang. 2009, 26, 16–26. [Google Scholar] [CrossRef]
- Schildkraut, J.J.; Klein, D.F. The classification and treatment of depressive disorders. In Manual of Psychiatric Therapeutics; Shader, R.I., Ed.; Little, Brown & Company: New York, NY, USA, 1975; pp. 36–91. [Google Scholar]
- De Figueiredo, J.M. Depression and demoralization: Phenomenologic differences and research perspectives. Compr. Psychiatry 1993, 34, 308–311. [Google Scholar] [CrossRef]
- Clarke, D.M.; Kissane, D.W.; Trauer, T.; Smith, G.C. Demoralization, anhedonia and grief in patients with severe physical illness. World Psychiatry 2005, 4, 96–105. [Google Scholar]
- Angelino, A.F.; Treisman, G.J. Major depression and demoralization in cancer patients: Diagnostic and treatment considerations. Support. Care Cancer 2001, 9, 344–349. [Google Scholar] [CrossRef]
- Jacobsen, J.C.; Vanderwerker, L.C.; Block, S.D.; Friedlander, R.J.; Maciejewski, P.K.; Prigerson, H.G. Depression and demoralization as distinct syndromes: Preliminary data from a cohort of advanced cancer patients. Indian J. Palliat. Care 2006, 12, 8–15. [Google Scholar] [CrossRef]
- Park, E.O.; Lee, H.Y. Factors Influencing Suicidal Ideation Among Korean Adults by Age: Results of the 2010–2011 Korean Health and Nutrition Examination Survey. Community Ment. Health J. 2015, 51, 987–993. [Google Scholar] [CrossRef]
- Robinson, S.; Kissane, D.W.; Brooker, J.; Burney, S. A systematic review of the demoralization syndrome in individuals with progressive disease and cancer: A decade of research. J. Pain Symptom Manag. 2015, 49, 595–610. [Google Scholar] [CrossRef]
- Beck, A.T.; Weissman, A.; Lester, D.; Trexler, L. The measurement of pessimism: The hopelessness scale. J. Consult. Clin. Psychol. 1974, 42, 861–865. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Kovacs, M.; Weissmann, A. Hopelessness and suicidal behavior: An overview. JAMA 1975, 234, 1146–1149. [Google Scholar] [CrossRef] [PubMed]
- Jacobsen, J.C.; Maytal, G.; Stern, T.A. Demoralization in medical practice. Prim. Care Companion J. Clin. Psychiatry 2007, 9, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Sheehan, D.V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Baker, R.; Dunbar, G.C. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 1998, 59, 22–33. [Google Scholar] [PubMed]
- Beck, A.T.; Kovacs, M.; Weissman, A. Assessment of suicidal intention: The Scale for Suicide Ideation. J. Consult. Clin. Psychol. 1979, 47, 343–352. [Google Scholar] [CrossRef] [PubMed]
- De Man, A.F.; Leduc, C.P.; Labrèche-Gauthier, L. A French-Canadian scale for suicide ideation for use with adolescents. Can. J. Behav. Sci. 1993, 25, 126–134. [Google Scholar] [CrossRef]
- Sokero, T.P.; Melartin, T.K.; Rytsala, H.J.; Leskela, U.S.; Lestela-Mielonen, P.S.; Isometsa, E.T. Suicidal ideation and attempts among psychiatric patients with major depressive disorder. J. Clin. Psychiatry 2003, 64, 1094–1100. [Google Scholar] [CrossRef]
- De Beurs, D.P.; Fokkema, M.; O’Connor, R.C. Optimizing the assessement of suicidal behavior: The application of curtailement techniques. J. Affect. Disord. 2016, 196, 218–224. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A. Manual for Beck Scale for Suicide Ideation, 1st ed.; Psychological Corporation: New York, NY, USA, 1991. [Google Scholar]
- Costantini, A.; Picardi, A.; Brunetti, S.; Trabucchi, G.; Bersani, F.S.; Minichino, A.; Marchetti, P. Italian version of Demoralization Scale: A validation study. Riv. Psichiatr. 2013, 48, 234–239. [Google Scholar]
- Hadnagy, Z.; Csikós, Á.; Nagy, L. Introduction of the demoralization scale in Hungary, a study on demoralization and depression among hospice patients. Orv. Hetil. 2012, 153, 737–743. [Google Scholar] [CrossRef]
- Mehnert, A.; Vehling, S.; Höcker, A.; Lehmann, C.; Koch, U. Demoralization and depression in patients with advanced cancer: Validation of the German version of the demoralization scale. J. Pain Symptom Manag. 2011, 42, 768–776. [Google Scholar] [CrossRef] [PubMed]
- Rudilla, D.; Galiana, L.; Oliver, A.; Barreto, P. Demoralization Scale in Spanish-Speaking Palliative Care Patients. J. Pain Symptom Manag. 2016, 51, 769–775. [Google Scholar] [CrossRef] [PubMed]
- Tang, L.; Li, Z.; Pang, Y. The differences and the relationship between demoralization and depression in Chinese cancer patients. Psychooncology 2020, 29, 532–538. [Google Scholar] [CrossRef] [PubMed]
- Baertschi, M.; Costanza, A.; Richard-Lepouriel, H.; Pompili, M.; Sarasin, F.; Weber, K.; Canuto, A. The application of the interpersonal-psychological theory of suicide to a sample of Swiss patients attending a psychiatric emergency department for a non-lethal suicidal event. J. Affect. Disord. 2017, 210, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Baertschi, M.; Costanza, A.; Canuto, A.; Weber, K. The Function of Personality in Suicidal Ideation from the Perspective of the Interpersonal-Psychological Theory of Suicide. Int. J. Environ. Res. Public Health 2018, 15, 636. [Google Scholar] [CrossRef]
- Baertschi, M.; Costanza, A.; Canuto, A.; Weber, K. The dimensionality of suicidal ideation and its clinical implications. Int. J. Methods Psychiatr. Res. 2019, 28, e1755. [Google Scholar] [CrossRef]
- Nordentoft, M. Prevention of suicide and attempted suicide in Denmark. Epidemiological studies of suicide and intervention studies in selected risk groups. Dan. Med. Bull. 2007, 54, 306–369. [Google Scholar]
- Martiello, M.A.; Boncompagni, G.; Lacangellera, D.; Corlito, G. Risk factors for suicide in rural Italy: A case–control study. Soc. Psychiatry Psychiatr. Epidemiol. 2019, 54, 607–616. [Google Scholar] [CrossRef]
| Psychosocial Characteristic (N = 199) | Type | n | Percentage |
|---|---|---|---|
| Gender | Women | 120 | 60.3 |
| Men | 79 | 39.7 | |
| Age | ≤ 50 years | 166 | 83.4 |
| ≥ 50 years | 33 | 16.6 | |
| Citizenship | Swiss | 116 | 58.3 |
| Non-Swiss | 83 | 41.7 | |
| Marital status | In a relationship | 69 | 34.7 |
| Single | 130 | 65.3 | |
| Children | Yes | 78 | 39.2 |
| No | 121 | 60.8 | |
| Professional status | Employed/Student | 115 | 57.8 |
| No activity | 84 | 42.2 | |
| Perceived wealth status | High (categories 1–3) | 36 | 18.1 |
| Low (categories 4–6) | 163 | 81.9 | |
| Inclusion criterion | Suicidal ideations | 131 | 65.8 |
| Suicide attempt | 68 | 34.2 | |
| History of suicide attempt | Yes | 125 | 62.8 |
| No | 74 | 37.2 | |
| Constructs | Sub-constructs | Mean | SD |
| Suicidal ideation (SSI) | Total score | 15.1 | 7.6 |
| Demoralization (DS) | Total score | 61.1 | 15.9 |
| Meaning in life | 11.5 | 4.7 | |
| Hopelessness | 17.2 | 4.7 | |
| Helplessness | 11.1 | 3.4 | |
| Sense of failure | 8.5 | 3.6 | |
| Dysphoria | 12.8 | 4.3 |
| Predictors Entered in Set | Cox-Snell R2 | Nagelkerke R2 | Odds Ratios | Lower CI 95% | Upper CI 95% | p |
|---|---|---|---|---|---|---|
| 1 | ||||||
| 0.017 | 0.024 | |||||
| MINI—major depressive episode | 0.667 | 0.324 | 1.372 | 0.271 | ||
| MINI—number of diagnoses | 1.050 | 0.851 | 1.296 | 0.646 | ||
| Children | 1.209 | 0.634 | 2.305 | 0.565 | ||
| Marital status | 1.474 | 0.763 | 2.850 | 0.248 | ||
| 2 | ||||||
| MINI—major depressive episode | 0.063 | 0.087 | 0.771 | 0.368 | 1.618 | 0.492 |
| MINI—number of diagnoses | 1.115 | 0.899 | 1.384 | 0.322 | ||
| Children | 1.031 | 0.528 | 2.016 | 0.928 | ||
| Marital status | 1.337 | 0.675 | 2.648 | 0.405 | ||
| Demoralization | 0.969 | 0.950 | 0.989 | 0.003 |
| Predictors Entered in Set | F | df | R2 | Adjusted R2 | b | t | p |
|---|---|---|---|---|---|---|---|
| 1 | 6.499 | 4, 194 | 0.118 | 0.100 | 0.000 | ||
| MINI—major depressive episode | 3.861 | 3.054 | 0.003 | ||||
| MINI—number of diagnoses | 0.368 | 0.827 | 0.409 | ||||
| Children | −2.816 | −2.485 | 0.014 | ||||
| Marital status | −1.937 | −1.662 | 0.098 | ||||
| 2 | 20.766 | 5, 193 | 0.350 | 0.333 | 0.000 | ||
| MINI—major depressive episode | 2.624 | 2.389 | 0.018 | ||||
| MINI—number of diagnoses | −0.161 | −0.499 | 0.618 | ||||
| Children | −1.480 | −1.498 | 0.136 | ||||
| Marital status | −1.206 | −1.198 | 0.232 | ||||
| Demoralization | 0.245 | 8.292 | 0.000 | ||||
| 3 | 14.380 | 5, 193 | 0.271 | 0.253 | |||
| MINI—major depressive episode | 2.725 | 2.338 | 0.020 | ||||
| MINI—number of diagnoses | 0.039 | 0.115 | 0.909 | ||||
| Children | −2.127 | −2.049 | 0.042 | ||||
| Marital status | −1.042 | −0.973 | 0.332 | ||||
| Hopelessness | 0.663 | 6.372 | 0.000 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Costanza, A.; Baertschi, M.; Richard-Lepouriel, H.; Weber, K.; Berardelli, I.; Pompili, M.; Canuto, A. Demoralization and Its Relationship with Depression and Hopelessness in Suicidal Patients Attending an Emergency Department. Int. J. Environ. Res. Public Health 2020, 17, 2232. https://doi.org/10.3390/ijerph17072232
Costanza A, Baertschi M, Richard-Lepouriel H, Weber K, Berardelli I, Pompili M, Canuto A. Demoralization and Its Relationship with Depression and Hopelessness in Suicidal Patients Attending an Emergency Department. International Journal of Environmental Research and Public Health. 2020; 17(7):2232. https://doi.org/10.3390/ijerph17072232
Chicago/Turabian StyleCostanza, Alessandra, Marc Baertschi, Hélène Richard-Lepouriel, Kerstin Weber, Isabella Berardelli, Maurizio Pompili, and Alessandra Canuto. 2020. "Demoralization and Its Relationship with Depression and Hopelessness in Suicidal Patients Attending an Emergency Department" International Journal of Environmental Research and Public Health 17, no. 7: 2232. https://doi.org/10.3390/ijerph17072232
APA StyleCostanza, A., Baertschi, M., Richard-Lepouriel, H., Weber, K., Berardelli, I., Pompili, M., & Canuto, A. (2020). Demoralization and Its Relationship with Depression and Hopelessness in Suicidal Patients Attending an Emergency Department. International Journal of Environmental Research and Public Health, 17(7), 2232. https://doi.org/10.3390/ijerph17072232






