Health Care and Productivity Costs of Non-Fatal Traffic Injuries: A Comparison of Road User Types
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting
2.2. Patient and Injury Characteristics
2.3. Health Care Consumption, Productivity Loss and Cost Estimation
2.4. Statistical Data Analysis
3. Results
3.1. Characteristics by Road User Type
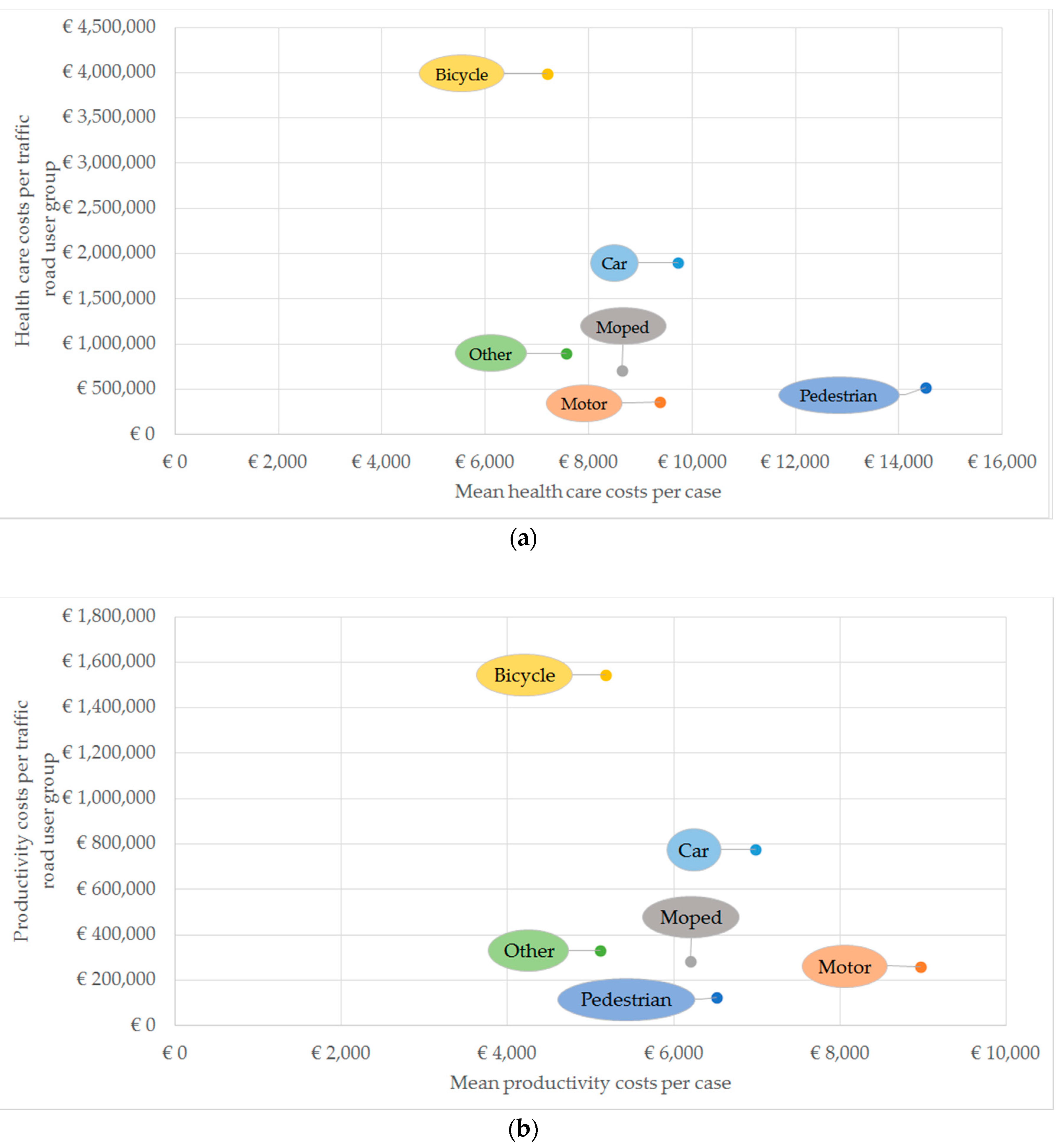
3.2. Health Care and Productivity Costs by Road User Type
3.3. Predictors of Health Care and Productivity Costs
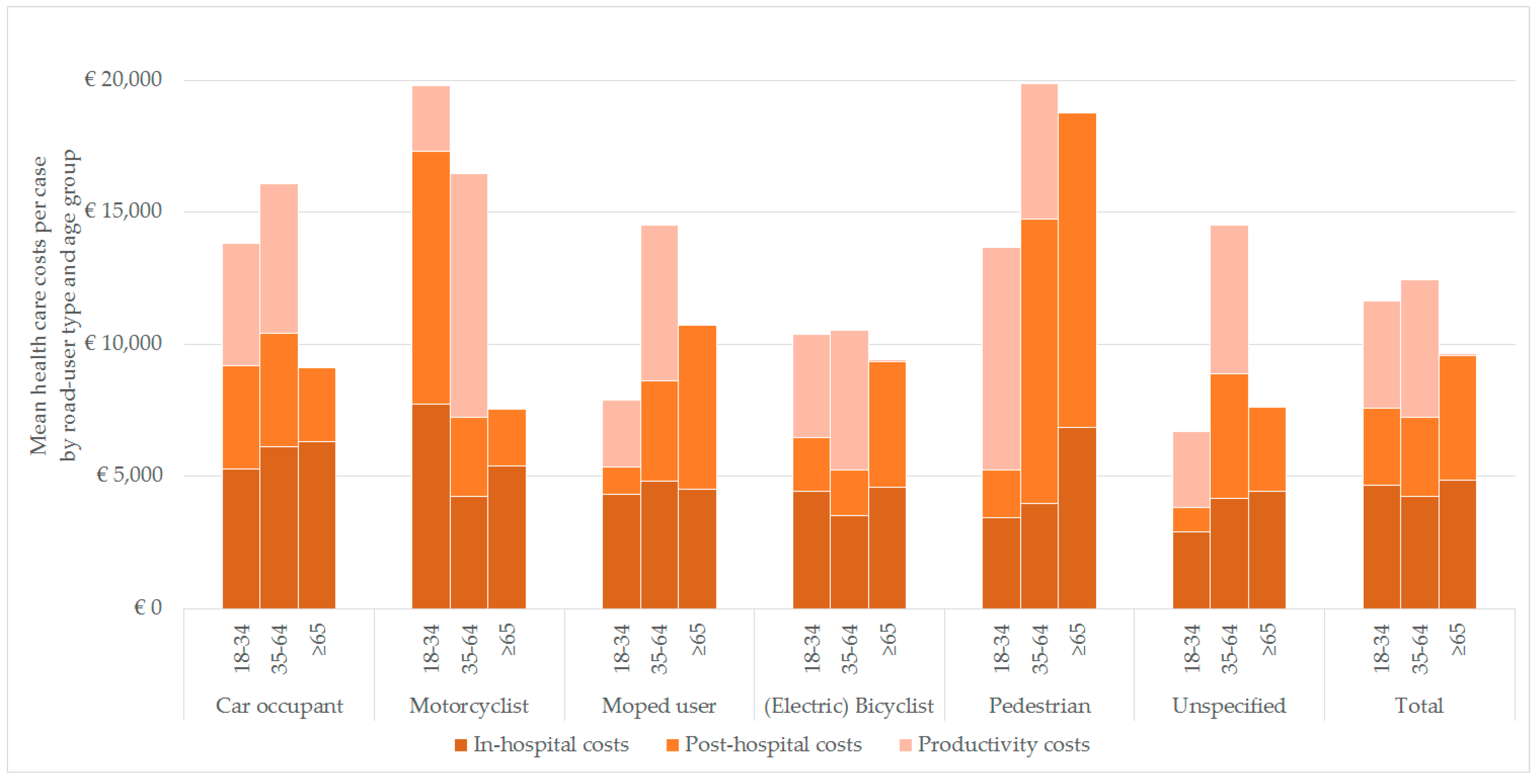
3.4. Health Care Costs by Road User Type and Age Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Unit costs | € |
|---|---|
| Transport | |
| Self-transport, per ride | 4.43 |
| Ambulance transport, per ride | 690 |
| Ambulance transport with support of air medical services, per ride | 5831 |
| Ambulance transport with support of ground medical services, per ride | 5831 |
| Trauma helicopter transport, per ride | 5281 |
| Hospital | |
| Emergency department, per visit | 265 |
| In-hospital day generic hospital, per day | 453 |
| Intensive Care Unit, per day | 1213 |
| Day-treatment hospital, per day | 282 |
| Outpatient clinic general hospital, per visit | 82 |
| Long term care, admission | |
| Nursing home, per day | 172 |
| Rehabilitation, per day | 471 |
| Psychiatric institution, per day | 309 |
| Long term care, day care | |
| Nursing home, per day | 69 |
| Rehabilitation, per hour | 157 |
| Psychiatric institution, per day | 100 |
| Home care | |
| Domestic care, per hour | 22 |
| Help with all day activities, per hour | 55 |
| Nursing, per hour | 75 |
| Health care provider | |
| General practitioner (GP), per visit | 34 |
| Company doctor, per visit | 53 |
| Psychologist, per visit | 65 |
| Social worker, per visit | 67 |
| Physiotherapist, per visit | 34 |
| Occupational therapist, per visit | 34 |
| Speech therapist, per visit | 31 |
| Dietician, per visit | 21 |
| Productivity | |
| Paid labor (male) | 38.78 |
| Paid labor (female) | 32.33 |
| Characteristic | Responders | Non-Responders | p-Value |
|---|---|---|---|
| N (%) | 1024 (44.9) | 1257 (55.1) | |
| Sex, n (%) | 0.07 (chi2 = 3.3) | ||
| Male | 598 (58.4) | 781 (62.1) | |
| Female | 426 (41.6) | 476 (37.9) | |
| Age | |||
| Mean (SD) | 56.6 (18.1) | 51.0 (21.4) | <0.001 |
| 18–34 years, n (%) | 149 (14.6) | 364 (29.0) | |
| 35–64 years, n (%) | 479 (46.8) | 501 (39.9) | |
| >65 years, n (%) | 396 (38.7) | 392 (31.2) | |
| Type of road user | <0.001 (chi2 = 71) | ||
| Car occupant | 195 (19.0) | 360 (28.6) | |
| Motorcyclist | 38 (3.7) | 69 (5.5) | |
| Moped rider | 82 (8.0) | 174 (13.8) | |
| (Electric) Bicyclist | 554 (54.1) | 527 (41.9) | |
| Pedestrian | 36 (3.5) | 38 (3.0) | |
| Unspecified 2 | 119 (11.6) | 89 (7.1) | |
| Injury Severity 1 | |||
| Mean (SD) | 6.9 (6.3) | 6.2 (6.0) | <0.001 |
| ISS 1–3, n (%) | 278 (27.1) | 461 (36.7) | |
| ISS 4–8, n (%) | 371 (36.2) | 407 (32.4) | |
| ISS 9–15, n (%) | 288 (28.1) | 278 (22.1) | |
| ISS ≥16, n (%) | 84 (8.2) | 98 (7.8) | |
| Type of injury | |||
| Pelvic injury | 95 (9.3) | 34 (2.7) | <0.001 (chi2 = 45.7) |
| Hip fracture | 117 (11.4) | 109 (8.7) | 0.03 (chi2 = 4.8) |
| Tibia, complex foot or femur fracture | 143 (14.0) | 182 (14.5) | 0.73 (chi2 = 0.73) |
| Shoulder and upper arm injury | 140 (13.7) | 167 (13.3) | 0.79 (chi2 = 0.1) |
| Radius, ulna or hand fracture | 80 (7.8) | 93 (7.4) | 0.71 (chi2 = 0.1) |
| Head injury | 427 (41.7) | 588 (46.8) | 0.02 (chi2 = 5.9) |
| Facial injury | 99 (9.7) | 128 (10.2) | 0.68 (chi2 = 0.2) |
| Thoracic injury | 69 (6.7) | 79 (6.3) | 0.66 (chi2 = 0.2) |
| Rib fracture | 188 (18.4) | 203 (16.1) | 0.16 (chi2 = 1.9) |
| Abdominal injury | 46 (4.5) | 55 (4.5) | 0.89 (chi2 = 0.02) |
| Stable vertebral fracture or disc injury | 80 (7.8) | 80 (6.4) | 0.18 (chi2 = 1.8) |
References
- World Health Organization. Global Status Report on Road Safety 2018; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Naci, H.; Chisholm, D.; Baker, T.D. Distribution of road traffic deaths by road user group: A global comparison. Inj. Prev. 2009, 15, 55–59. [Google Scholar] [CrossRef] [PubMed]
- Mayou, R.; Bryant, B. Consequences of road traffic accidents for different types of road user. Injury 2003, 34, 197–202. [Google Scholar] [CrossRef]
- Naumann, R.B.; Dellinger, A.M.; Zaloshnja, E.; Lawrence, B.A.; Miller, T.R. Incidence and total lifetime costs of motor vehicle–related fatal and nonfatal injury by road user type, United States, 2005. Traffic Inj. Prev. 2010, 11, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Polinder, S.; Haagsma, J.; Panneman, M.; Scholten, A.; Brugmans, M.J.; Van Beeck, E. The economic burden of injury: Health care and productivity costs of injuries in the Netherlands. Accid. Anal. Prev. 2016, 93, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Vlakveld, W.P.; Twisk, D.; Christoph, M.; Boele, M.; Sikkema, R.; Remy, R.; Schwab, A. Speed choice and mental workload of elderly cyclists on e-bikes in simple and complex traffic situations: A field experiment. Accid. Anal. Prev. 2015, 74, 97–106. [Google Scholar] [CrossRef] [PubMed]
- Central Bureau for Statistics. Traffic Performance Motor Vehicles; Kilometres, Type of Vehicle, Territory. 2019. Available online: https://opendata.cbs.nl/statline/#/CBS/en/dataset/80302eng/table?dl=1431B (accessed on 21 January 2020).
- Kruijer, H.; Den Hertog, P.; Wolt, K.K.; Panneman, M.; Sprik, E. Fietsongevallen in Nederland: Een LIS Vervolgonderzoek Naar Ongevallen Met Gewone en Elektrische Fietsen; VeiligheidNL: Amsterdam, The Netherlands, 2012. [Google Scholar]
- de Jongh, M.A.; Kruithof, N.; Gosens, T.; van de Ree, C.L.; de Munter, L.; Brouwers, L.; Polinder, S.; Lansink, K.W.W. Prevalence, recovery patterns and predictors of quality of life and costs after non-fatal injury: The Brabant Injury Outcome Surveillance (BIOS) study. Inj. Prev. 2017, 23, 59. [Google Scholar] [CrossRef] [PubMed]
- Gennarelli, T.A.; Wodzin, E. AIS 2005: A contemporary injury scale. Injury 2006, 37, 1083–1091. [Google Scholar] [CrossRef] [PubMed]
- Bouwmans, C.; Hakkaart-van Roijen, L.; Koopmanschap, M.; Krol, M.; Severens, H.; Brouwe, W. Handleiding iMTA Medical Cost Questionnaire (iMCQ); iMTA, Erasmus Universiteit Rotterdam: Rotterdam, The Netherlands, 2013. [Google Scholar]
- Hakkaart-van Roijen, L.; van der Linden, N.; Bouwmans, C.; Kanters, T.; Tan, S.S. Kostenhandleiding: Methodologie van Kostenonderzoek en Referentieprijzen Voor Economische Evaluaties in de Gezondheidszorg; Institute for Medical Technology Assessment, Erasmus University Rotterdam: Rotterdam, The Netherlands, 2015. [Google Scholar]
- Erasmus, M.C. Passantenprijslijst 2016. 2016. Available online: https://www6.erasmusmc.nl/cs-patientenzorg/2419534/2419543/3956735/5250821/Internetversie_passantenprijslijst_2016_v3.pdf?view=active (accessed on 6 May 2019).
- Nederlandse Zorgautoriteit. BRCU—2015 Bijlage 2 Medisch Specialistische Behandelingen en Tarieven 2011. 2015. Available online: https://puc.overheid.nl/nza/doc/PUC_11602_22/ (accessed on 6 May 2019).
- Nederlandse Zorgautoriteit. Nederlandse Zorgautoriteit Zorgapplicatie. 2017. Available online: https://puc.overheid.nl/nza/doc/PUC_274147_22/1/ (accessed on 6 May 2019).
- Elkerliek. Standaard Prijslijst Overige Zorgproducten. 2013. Available online: https://www.elkerliek.nl/elkerliek.nl/home/Passantanprijslijst%20Overige%20Zorgproducten%2001042013%20tm%2030062013.pdf (accessed on 6 May 2019).
- Nederlandse Zorgautoriteit. Tarievenlijst Eerstelijnsdiagnostiek. 2014. Available online: https://docplayer.nl/13384312-Tarievenlijst-eerstelijnsdiagnostiek-bijlage-1-bij-tariefbeschikking-tb-cu-7078-02-van-1-juni-2014.html (accessed on 6 May 2019).
- Rivas. Bio-impedantiemeting. 2019. Available online: https://www.rivas.nl/voeding-leefstijl/gezondheidsmetingen/cursus/bio-impedantiemeting/?tx_roqcursussenactiviteiten_cursussen%5Baction%5D=show&tx_roqcursussenactiviteiten_cursussen%5Bcontroller%5D=Course&cHash=094076003728918c33f5113ca52651f1 (accessed on 6 May 2019).
- Zeelandcare. Passanten Prijslijst DBC-OVP Zorgproducten. 2018. Available online: https://zeelandcare.com/sites/default/files/Prijslijst%20Passanten%20DBC-OVP%20zorgproducten%202018.pdf (accessed on 6 May 2019).
- Upatising, B.; Wood, D.L.; Kremers, W.K.; Christ, S.L.; Yih, Y.; Hanson, G.J.; Takahashi, P. Cost comparison between home telemonitoring and usual care of older adults: A randomized trial (Tele-ERA). Telemed. J. E Health 2015, 21, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Bouwmans-Frijters, C.A.; Krol, M.; Severens, H.; Koopmanschap, M.; Brouwer, W.B.F.; Roijen, L.H.-V. The iMTA productivity cost questionnaire: A standardized instrument for measuring and valuing health-related productivity losses. Value Health 2015, 18, 753–758. [Google Scholar] [CrossRef] [PubMed]
- CBS. Working Population; Working Time. 2019. Available online: https://opendata.cbs.nl/statline/#/CBS/nl/dataset/82647NED/table?dl=17FC9 (accessed on 6 May 2019).
- OECD/European Observatory on Health Systems and Policies. Netherlands: Country Health Profile 2019; OECD Publishing: Paris, France, 2019. [Google Scholar]
- Pucher, J.; Buehler, R. Making cycling irresistible: Lessons from the Netherlands, Denmark and Germany. Transp. Rev. 2008, 28, 495–528. [Google Scholar] [CrossRef]
- Connolly, M.P.; Tashjian, C.; Kotsopoulos, N.; Bhatt, A.; Postma, M.J. A comparison of average wages with age-specific wages for assessing indirect productivity losses: Analytic simplicity versus analytic precision. Eur. J. Health Econ. 2017, 18, 697–701. [Google Scholar] [CrossRef] [PubMed]
- Van Wijk, D.; Groeniger, J.O.; Van Lenthe, F.J.; Kamphuis, C.B.M. The role of the built environment in explaining educational inequalities in walking and cycling among adults in the Netherlands. Int. J. Health Geogr. 2017, 16, 10. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Scholten, A.; Polinder, S.; Panneman, M.J.; Van Beeck, E.; Haagsma, J.A. Incidence and costs of bicycle-related traumatic brain injuries in the Netherlands. Accid. Anal. Prev. 2015, 81, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Poos, H.P.A.M.; Lefarth, T.L.; Harbers, J.S.; Wendt, K.W.; El Moumni, M.; Reininga, I.H.F. E-bikers are more often seriously injured in bicycle accidents: Results from the Groningen bicycle accident database. Ned. Tijdschr. Geneeskd. 2017, 161, D1520. [Google Scholar] [PubMed]
- De Guerre, L.E.V.M.; Sadiqi, S.; Leenen, L.P.H.; Oner, C.F.; Van Gaalen, S.M. Injuries related to bicycle accidents: An epidemiological study in The Netherlands. Eur. J. Trauma Emerg. Surg. 2018. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.; Yang, D.; Zhou, J.-B.; Feng, Z.; Yuan, Q. Risk riding behaviors of urban E-Bikes: A literature review. Int. J. Environ. Res. Public Health 2019, 16, 2308. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Car Occupant | Motorcyclist | Moped rider | (Electric) Bicyclist | Pedestrian | Unspecified 4 | Total |
|---|---|---|---|---|---|---|---|
| N | 195 (19) | 38 (3.7) | 82 (8) | 554 (54.1) | 36 (3.5) | 119 (11.6) | 1024 |
| Sex, n (%) | |||||||
| Male | 120 (61.5) | 37 (97.4) | 53 (64.6) | 307 (55.4) | 14 (38.9) | 67 (56.3) | 598 (58.4) |
| Female | 75 (38.5) | 1 (2.6) | 29 (35.4) | 247 (44.6) | 22 (61.1) | 52 (43.7) | 426 (41.6) |
| Age | |||||||
| Median (IQR) | 49.0 (31.0–64.0) | 51.0 (35.0–59.3) | 55.0 (40.8–67.3) | 63.0 (51.0–71.3) | 59.0 (35.8–77.0) | 60.0 (47.0–70.0) | 59.0 (45.0–70.0) |
| 18–34 years, n (%) | 57 (29.2) | 8 (21.1) | 15 (18.3) | 42 (7.6) | 8 (22.2) | 19 (16) | 149 (14.6) |
| 35–64 years, n (%) | 90 (46.2) | 26 (68.4) | 42 (51.2) | 257 (46.4) | 11 (30.6) | 53 (44.5) | 479 (46.8) |
| >65 years, n (%) | 48 (24.6) | 4 (10.5) | 25 (30.5) | 255 (46.0) | 17 (47.2) | 47 (39.5) | 396 (38.7) |
| Type of injury 1 | |||||||
| Pelvic injury, n (%) | 19 (9.7) | 5 (13.2) | 9 (11) | 46 (8.3) | 6 (16.7) | 10 (8.4) | 95 (9.3) |
| Hip fracture, n (%) | 4 (2.1) | 0 (0) | 7 (8.5) | 91 (16.4) | 7 (19.4) | 8 (6.7) | 117 (11.4) |
| Tibia, complex foot or femur fracture, n (%) | 25 (12.8) | 12 (31.6) | 15 (18.3) | 62 (11.2) | 11 (30.6) | 18 (15.1) | 143 (14.0) |
| Shoulder and upper arm injury, n (%) | 21 (10.8) | 7 (18.4) | 16 (19.5) | 81 (14.6) | 5 (13.9) | 10 (8.4) | 140 (13.7) |
| Radius, ulna or hand fracture, n (%) | 14 (7.2) | 8 (21.1) | 8 (9.8) | 40 (7.2) | 3 (8.3) | 7 (5.9) | 80 (7.8) |
| Head injury, n (%) | 83 (42.6) | 6 (15.8) | 36 (43.9) | 242 (43.7) | 16 (44.4) | 44 (37.0) | 427 (41.7) |
| Facial injury, n (%) | 8 (4.1) | 2 (5.3) | 11 (13.4) | 66 (11.9) | 3 (8.3) | 9 (7.6) | 99 (9.7) |
| Thoracic injury, n (%) | 21 (10.8) | 6 (15.8) | 7 (8.5) | 28 (5.1) | 3 (8.3) | 4 (3.4) | 69 (6.7) |
| Rib fracture, n (%) | 65 (33.3) | 10 (26.3) | 20 (24.4) | 69 (12.5) | 3 (8.3) | 21 (17.6) | 188 (18.4) |
| Abdominal injury, n (%) | 22 (11.3) | 4 (10.5) | 7 (8.5) | 10 (1.8) | 2 (5.6) | 1 (0.8) | 46 (4.5) |
| Stable vertebral fracture or disc injury, n (%) | 22 (11.3) | 5 (13.2) | 8 (9.8) | 32 (5.8) | 3 (8.3) | 10 (8.4) | 80 (7.8) |
| Injury Severity 2 | |||||||
| Median (IQR) | 4.0 (2.0–9.0) | 5.5 (4.0–10.0) | 6.0 (4.0–9.3) | 5.0 (4.0–9.0) | 7.5 (4.0–10.0) | 4.0 (4.0–9.0) | 5.0 (3.0–9.0) |
| ISS 1–3, n (%) | 88 (45.1) | 6 (15.8) | 18 (22.0) | 133 (24.0) | 7 (19.4) | 26 (21.8) | 278 (27.1) |
| ISS 4–8, n (%) | 53 (27.2) | 17 (44.7) | 32 (39.0) | 202 (36.5) | 11 (30.6) | 56 (47.1) | 371 (36.2) |
| ISS 9–15, n (%) | 29 (23.7) | 9 (23.7) | 21 (23.6) | 186 (33.6) | 14 (38.9) | 29 (24.4) | 288 (28.1) |
| ISS ≥16, n (%) | 25 (12.8) | 6 (15.8) | 11 (13.4) | 33 (6.0) | 4 (11.1) | 5 (4.2) | 84 (8.2) |
| Days admitted to hospital | |||||||
| Median (IQR) | 3.0 (2.0–6.0) | 4.0 (2.0–11.0) | 4.0 (2.0–8.3) | 4.0 (2.0–6.0) | 6.5 (2.0–11.5) | 3.0 (2.0–6.0) | 3.0 (2.0–7.0) |
| Employment, n (%)3 | |||||||
| Paid employment | 104 (53.3) | 30 (78.9) | 36 (43.9) | 246 (44.4) | 14 (38.9) | 49 (41.2) | 479 (46.8) |
| No paid employment | 28 (14.4) | 3 (7.9) | 19 (23.2) | 87 (15.7) | 6 (16.7) | 26 (21.8) | 169 (16.5) |
| Retired | 45 (23.1) | 3 (7.9) | 20 (24.4) | 199 (35.9) | 15 (41.7) | 37 (31.1) | 319 (31.2) |
| Comorbidity, n (%) | |||||||
| No comorbidities | 111 (56.9) | 29 (76.3) | 35 (42.7) | 250 (45.1) | 21 (58.3) | 54 (45.4) | 500 (48.8) |
| 1 comorbidity | 58 (29.7) | 7 (18.4) | 23 (28.0) | 163 (29.4) | 10 (27.8) | 39 (32.8) | 300 (29.3) |
| 2 or more comorbidities | 26 (13.3) | 2 (5.3) | 24 (29.3) | 141 (25.5) | 5 (13.9) | 26 (21.8) | 224 (21.9) |
| Type of Costs | Car Occupant | Motorcyclist | Moped Rider | (Electric) Bicyclist | Pedestrian | Unspecified 3 | Total |
|---|---|---|---|---|---|---|---|
| N (%) | 195 (19) | 38 (3.7) | 82 (8) | 554 (54.1) | 36 (3.5) | 119 (11.6) | 1024 |
| In-hospital costs | 5900 (8900) | 5100 (5100) | 4600 (3900) | 4100 (3500) | 5200 (3300) | 4100 (2700) | 4500 (5100) |
| Post-hospital costs | 3900 (9100) | 4500 (8800) | 4100 (9400) | 3200 (9700) | 9600 (14,500) | 3700 (11,900) | 3700 (10,100) |
| Productivity costs 1 | 7000 (7300) | 9000 (7700) | 6200 (7700) | 5200 (6000) | 6500 (6800) | 5100 (6700) | 5900 (6700) |
| Total costs 2 | 13,700 (17,700) | 16,200 (15,000) | 12,100 (13,700) | 10,000 (12,100) | 18,000 (16,800) | 10,400 (14,500) | 11,400 (14,100) |
| Characteristic | Health Care Costs | Productivity Costs 3 | ||||
|---|---|---|---|---|---|---|
| Number of Cases N = 1021 | Unadjusted Exp(B) | Adjusted 4 Exp(B) | Number of cases; N = 394 | Unadjusted Exp(B) | Adjusted 4 Exp(B) | |
| Sex | ||||||
| Male (ref) | 597 | 247 | ||||
| Female | 424 | 1.20 (1.06–1.34) | 1.21 (1.09–1.34) | 147 | 0.67 (0.57–0.79) | 0.68 (0.58–0.80) |
| Age | ||||||
| 18–34 years (ref) | 148 | 75 | ||||
| 35–64 years 1 | 478 | 0.96 (0.80–1.14) | 1.21 (1.04–1.42) | 313 | 1.04 (0.84–1.30) | 1.01 (0.81–1.24) |
| >65 years | 395 | 1.27 (1.06–1.51) | 1.63 (1.37–1.93) | 6 | - | - |
| Injury Severity 2 | ||||||
| ISS 1–3 (ref) | 278 | 121 | ||||
| ISS 4–8 | 371 | 1.71 (1.50–1.95) | 1.64 (1.45–1.87) | 143 | 1.64 (1.35–2.01) | 1.55 (1.27–1.89) |
| ISS 9–15 | 288 | 2.51 (2.19–2.89) | 2.34 (2.04–2.67) | 101 | 1.89 (1.51–2.35) | 1.79 (1.44–2.22) |
| ISS ≥16 | 84 | 5.28 (4.30–6.48) | 6.12 (5.00–7.50) | 29 | 2.44 (1.74–3.40) | 2.32 (1.67–3.23) |
| Comorbidity | ||||||
| No comorbidities (ref) | 498 | 264 | ||||
| 1 comorbidity | 300 | 1.29 (1.12–1.47) | 1.11 (0.98–1.25) | 89 | 1.06 (0.86–1.30) | 1.04 (0.86–1.27) |
| 2 or more comorbidities | 223 | 1.32 (1.14–1.54) | 1.19 (1.04–1.37) | 41 | 0.93 (0.70–1.24) | 1.02 (0.78–1.34) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
van der Vlegel, M.; Haagsma, J.A.; de Munter, L.; de Jongh, M.A.C.; Polinder, S. Health Care and Productivity Costs of Non-Fatal Traffic Injuries: A Comparison of Road User Types. Int. J. Environ. Res. Public Health 2020, 17, 2217. https://doi.org/10.3390/ijerph17072217
van der Vlegel M, Haagsma JA, de Munter L, de Jongh MAC, Polinder S. Health Care and Productivity Costs of Non-Fatal Traffic Injuries: A Comparison of Road User Types. International Journal of Environmental Research and Public Health. 2020; 17(7):2217. https://doi.org/10.3390/ijerph17072217
Chicago/Turabian Stylevan der Vlegel, Marjolein, Juanita A. Haagsma, Leonie de Munter, Mariska A. C. de Jongh, and Suzanne Polinder. 2020. "Health Care and Productivity Costs of Non-Fatal Traffic Injuries: A Comparison of Road User Types" International Journal of Environmental Research and Public Health 17, no. 7: 2217. https://doi.org/10.3390/ijerph17072217
APA Stylevan der Vlegel, M., Haagsma, J. A., de Munter, L., de Jongh, M. A. C., & Polinder, S. (2020). Health Care and Productivity Costs of Non-Fatal Traffic Injuries: A Comparison of Road User Types. International Journal of Environmental Research and Public Health, 17(7), 2217. https://doi.org/10.3390/ijerph17072217





