Correlation between Kind of Cesarean Section and Posttraumatic Stress Disorder in Greek Women
Abstract
:1. Introduction
1.1. PTSD after Childbirth
1.2. PTSD after Cesarean(AC)
1.3. PTSD- AC in Greek Women
2. Materials and Methods
2.1. Participants
2.2. Data and Measures
2.2.1. Socio-Demographic Questionnaire
2.2.2. Life Events Checklist-5 (LEC-5) of DSM-V
2.2.3. Criterion A of DSM-V
2.2.4. Post-Traumatic Stress Checklist (PCL-5)of DSM-V
2.3. Statistical Analysis
3. Results
3.1. Pregnancy and Delivery Characteristics
3.2. ΤhePrevalence of PTSD Criteria among Women after CS
3.3. Risk Factors for PTSD-AC
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- DePierro, J.; D’Andrea, W.; Spinazzola, J.; Stafford, E.; van Der Kolk, B.; Saxe, G.; Stolbach, B.; McKernan, S.; Ford, J.D. Beyond PTSD: Client Presentations of Developmental Trauma Disorder from a National Survey of Clinicians. Psychol. Trauma Theory Res. Pract. Policy 2019. [Google Scholar] [CrossRef] [PubMed]
- Stein, M.B.; Jang, K.L.; Taylor, S.; Vernon, P.A.; Livesley, W.J. Genetic and Environmental Influences on Trauma Exposure and Posttraumatic Stress Disorder Symptoms: A Twin Study. Am. J. Psychiatry 2002, 159, 1675–1681. [Google Scholar] [CrossRef] [PubMed]
- Breslau, N.; Lucia, V.C.; Davis, G.C. Partial PTSD versus Full PTSD: An Empirical Examination of Associated Impairment. Psychol. Med. 2004, 34, 1205–1214. [Google Scholar] [CrossRef] [PubMed]
- Mylle, J.; Maes, M. Partial Posttraumatic Stress Disorder Revisited. J. Affect. Disord. 2004, 78, 37–48. [Google Scholar] [CrossRef]
- Ayers, S.; Pickering, A.D. Do Women Get Posttraumatic Stress Disorder as a Result of Childbirth? A Prospective Study of Incidence. Birth Issues Perinat. Care 2001, 28, 111–118. [Google Scholar] [CrossRef] [Green Version]
- Czarnocka, J.; Slade, P. Prevalence and Predictors of Post-Traumatic Stress Symptoms Following Childbirth. Br. J. Clin. Psychol. 2000, 39, 35–51. [Google Scholar] [CrossRef]
- Sentilhes, L.; Maillard, F.; Brun, S.; Madar, H.; Merlot, B.; Goffinet, F.; Deneux-Tharaux, C. Risk Factors for Chronic Post-Traumatic Stress Disorder Development One Year after Vaginal Delivery: A Prospective, Observational Study. Sci. Rep. 2017, 7, 8724. [Google Scholar] [CrossRef]
- Van Heumen, M.A.; Hollander, M.H.; van Pampus, M.G.; van Dillen, J.; Stramrood, C.A.I. Psychosocial Predictors of Postpartum Posttraumatic Stress Disorder in Women With a Traumatic Childbirth Experience. Front. Psychiatry 2018, 9, 348. [Google Scholar] [CrossRef] [Green Version]
- Kessler, R.C.; Sonnega, A.; Bromet, E.; Hughes, M.; Nelson, C.B. Posttraumatic Stress Disorder in the National Comorbidity Survey. Arch. Gen. Psychiatry 1995, 52, 1048–1060. [Google Scholar] [CrossRef]
- James, S. Women’s Experiences of Symptoms of Posttraumatic Stress Disorder (PTSD) after Traumatic Childbirth: A Review and Critical Appraisal. Arch. Women’s Ment. Health 2015, 18, 761–771. [Google Scholar] [CrossRef] [Green Version]
- Shaban, Z.; Dolatian, M.; Shams, J.; Alavi-Majd, H.; Mahmoodi, Z.; Sajjadi, H. Post-Traumatic Stress Disorder (PTSD) Following Childbirth: Prevalence and Contributing Factors. Iran. Red Crescent Med. J. 2013, 15, 177–182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwab, W.; Marth, C.; Bergant, A.M. Post-Traumatic Stress Disorder Post Partum. Geburtshilfe Frauenheilkd. 2012, 72, 56–63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andersen, L.B.; Melvaer, L.B.; Videbech, P.; Lamont, R.F.; Joergensen, J.S. Risk Factors for Developing Post-Traumatic Stress Disorder Following Childbirth: A Systematic Review. Acta Obstet. Gynecol. Scand. 2012, 91, 1261–1272. [Google Scholar] [CrossRef] [PubMed]
- Ryding, E.L.; Wijma, K.; Wijma, B. Psychological Impact of Emergency Cesarean Section in Comparison with Elective Cesarean Section, Instrumental and Normal Vaginal Delivery. J. Psychosom. Obstet. Gynecol. 1998, 19, 135–144. [Google Scholar] [CrossRef]
- Mahmoodi, Z.; Dolatian, M.; Shaban, Z.; Shams, J.; Alavi-Majd, H.; Mirabzadeh, A. Correlation between Kind of Delivery and Posttraumatic Stress Disorder. Ann. Med. Health Sci. Res. 2016, 6, 356–361. [Google Scholar] [CrossRef] [Green Version]
- Cohen, M.M.; Ansara, D.; Schei, B.; Stuckless, N.; Stewart, D.E. Posttraumatic Stress Disorder after Pregnancy, Labor, and Delivery. J. Women’s Health 2004, 13, 315–324. [Google Scholar] [CrossRef]
- Sorenson, D.S.; Tschetter, L. Prevalence of Negative Birth Perception, Disaffirmation, Perinatal Trauma Symptoms, and Depression among Postpartum Women. Perspect. Psychiatr. Care 2010, 46, 14–25. [Google Scholar] [CrossRef]
- Ford, E.; Ayers, S.; Bradley, R. Exploration of a Cognitive Model to Predict Post-Traumatic Stress Symptoms Following Childbirth. J. Anxiety Disord. 2010, 24, 353–359. [Google Scholar] [CrossRef] [Green Version]
- Lopez, U.; Meyer, M.; Loures, V.; Iselin-Chaves, I.; Epiney, M.; Kern, C.; Haller, G. Post-Traumatic Stress Disorder in Parturients Delivering by Caesarean Section and the Implication of Anaesthesia: A Prospective Cohort Study. Health Qual. Life Outcomes 2017, 15, 118. [Google Scholar] [CrossRef] [Green Version]
- Söderquist, J.; Wijma, B.; Thorbert, G.; Wijma, K. Risk Factors in Pregnancy for Post-Traumatic Stress and Depression after Childbirth. BJOG Int. J. Obstet. Gynaecol. 2009, 116, 672–680. [Google Scholar] [CrossRef]
- Ryding, E.L.; Wijma, B.; Wijma, K. Posttraumatic Stress Reactions after Emergency Cesarean Section. Acta Obstet. Gynecol. Scand. 1997, 76, 856–861. [Google Scholar] [CrossRef] [PubMed]
- Tham, V.; Christensson, K.; Ryding, E.L. Sense of Coherence and Symptoms of Post-Traumatic Stress after Emergency Caesarean Section. Acta Obstet. Gynecol. Scand. 2007, 86, 1090–1096. [Google Scholar] [CrossRef] [PubMed]
- Ayers, S.; Bond, R.; Bertullies, S.; Wijma, K. The Aetiology of Post-Traumatic Stress Following Childbirth: A Meta-Analysis and Theoretical Framework. Psychol. Med. 2016, 46, 1121–1134. [Google Scholar] [CrossRef] [PubMed]
- O’Donovan, A.; Alcorn, K.L.; Patrick, J.C.; Creedy, D.K.; Dawe, S.; Devilly, G.J. Predicting Posttraumatic Stress Disorder after Childbirth. Midwifery 2014, 30, 935–941. [Google Scholar] [CrossRef] [Green Version]
- Population and Social Conditions—ELSTAT. Available online: https://www.statistics.gr/en/statistics/pop (accessed on 16 January 2020).
- WHO|WHO Statement on Caesarean Section Rates. Available online: http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/cs-statement/en/ (accessed on 28 December 2019).
- Modarres, M.; Afrasiabi, S.; Rahnama, P.; Montazeri, A. Prevalence and Risk Factors of Childbirth-Related Post-Traumatic Stress Symptoms. BMC Pregnancy Childbirth 2012, 12, 88. [Google Scholar] [CrossRef] [Green Version]
- Leonardou, A.A.; Zervas, Y.M.; Papageorgiou, C.C.; Marks, M.N.; Tsartsara, E.C.; Antsaklis, A.; Christodoulou, G.N.; Soldatos, C.R. Validation of the Edinburgh Postnatal Depression Scale and Prevalence of Postnatal Depression at Two Months Postpartum in a Sample of Greek Mothers. J. Reprod. Infant Psychol. 2009, 27, 28–39. [Google Scholar] [CrossRef]
- Papamarkou, M.; Sarafis, P.; Kaite, C.P.; Malliarou, M.; Tsounis, A.; Niakas, D. Investigation of the Association between Quality of Life and Depressive Symptoms during Postpartum Period: A Correlational Study. BMC Women’s Health 2017, 17, 115. [Google Scholar] [CrossRef] [Green Version]
- Diagnostic and Statistical Manual of Mental Disorders (DSM-5)—ProQuest. Available online: https://search.proquest.com/openview/6b548968301e74806949f2f8bbf5559c/1?pq-origsite=gscholar&cbl=34821 (accessed on 29 December 2019).
- Life Events Checklist for DSM-5 (LEC-5)—PTSD: National Center for PTSD. Available online: https://www.ptsd.va.gov/professional/assessment/te-measures/life_events_checklist.asp (accessed on 29 December 2019).
- Gray, M.J.; Litz, B.T.; Hsu, J.L.; Lombardo, T.W. Psychometric Properties of the Life Events Checklist. Assessment 2004, 11, 330–341. [Google Scholar] [CrossRef] [Green Version]
- PTSD and DSM-5—PTSD: National Center for PTSD. Available online: https://www.ptsd.va.gov/professional/treat/essentials/dsm5_ptsd.asp (accessed on 30 December 2019).
- McFarlane, A.C. PTSD and DSM-5: Unintended Consequences of Change. Lancet Psychiatry 2014, 1, 246–247. [Google Scholar] [CrossRef]
- PTSD Checklist for DSM-5 (PCL-5—PTSD: National Center for PTSD. Available online: https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp (accessed on 31 December 2019).
- Wortmann, J.H.; Jordan, A.H.; Weathers, F.W.; Resick, P.A.; Dondanville, K.A.; Hall-Clark, B.; Foa, E.B.; Young-McCaughan, S.; Yarvis, J.S.; Hembree, E.A.; et al. Psychometric Analysis of the PTSD Checklist-5 (PCL-5) among Treatment-Seeking Military Service Members. Psychol. Assess. 2016, 28, 1392–1403. [Google Scholar] [CrossRef]
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. J. Trauma. Stress 2015, 28, 489–498. [Google Scholar] [CrossRef] [PubMed]
- Xie, R.; Lei, J.; Wang, S.; Xie, H.; Walker, M.; Wen, S.W. Cesarean Section and Postpartum Depression in a Cohort of Chinese Women with a High Cesarean Delivery Rate. J. Women’s Health 2011, 20, 1881–1886. [Google Scholar] [CrossRef] [PubMed]
- Boyce, P.M.; Todd, A.L. Increased Risk of Postnatal Depression after Emergency Caesarean Section. Med. J. Aust. 1992, 157, 172–174. [Google Scholar] [CrossRef] [PubMed]
- Karlström, A. Women’s Self-Reported Experience of Unplanned Caesarean Section: Results of a Swedish Study. Midwifery 2017, 50, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Sgayer, I.; Frank Wolf, M. induction of labor at 39 weeks of gestation versus expectant management. Harefuah 2019, 158, 802–806. [Google Scholar] [PubMed]
- Holditch-Davis, D.; Bartlett, T.R.; Blickman, A.L.; Miles, M.S. Posttraumatic Stress Symptoms in Mothers of Premature Infants. J. Obstet. Gynecol. Neonatal Nurs. 2003, 32, 161–171. [Google Scholar] [CrossRef]
- Shaw, R.J.; Brecht, C.J.; St. John, N.; Lilo, E.; Corcoran, J.; Jo, B.; Howell, S.; Benitz, W.; Feinstein, N.F.; Melnyk, B.; et al. Prevention of postpartum traumatic stress in mothers with preterm infants: Manual development and evaluation. Issues Ment. Health Nurs. 2013, 34, 578–586. [Google Scholar] [CrossRef] [Green Version]
- Staver, M.A.; Moore, T.A.; Hanna, K.M. Maternal Distress in the Neonatal Intensive Care Unit: A Concept Analysis. Adv. Neonatal Care Off. J. Natl. Assoc. Neonatal Nurses 2019, 19, 394–401. [Google Scholar] [CrossRef]
- Bonacquisti, A.; Geller, P.A.; Patterson, C.A. Maternal Depression, Anxiety, Stress, and Maternal-Infant Attachment in the Neonatal Intensive Care Unit. J. Reprod. Infant Psychol. 2019, 1–14. [Google Scholar] [CrossRef]
- Klein, M.; Vanderbilt, D.; Kendall-Tackett, K. PTSD and Breastfeeding: Let It Flow. ICAN Infant ChildAdolesc. Nutr. 2014, 6, 211–215. [Google Scholar] [CrossRef]
- Hoff, C.E.; Movva, N.; Rosen Vollmar, A.K.; Pérez-Escamilla, R. Impact of Maternal Anxiety on Breastfeeding Outcomes: A Systematic Review. Adv. Nutr. 2019, 10, 816–826. [Google Scholar] [CrossRef] [PubMed]
- Groër, M.W. Differences between Exclusive Breastfeeders, Formula-Feeders, and Controls: A Study of Stress, Mood, and Endocrine Variables. Biol. Res. Nurs. 2005, 7, 106–117. [Google Scholar] [CrossRef] [PubMed]
- Berkman, L.F. The Role of Social Relations in Health Promotion. Psychosom. Med. 1995, 57, 245–254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Total Sample (N = 160) | Type of C-Section | p | ||
|---|---|---|---|---|
| Emergency (N = 63; 39.4%) | Planned (N = 97; 60.6%) | |||
| N (%) | N (%) | N (%) | ||
| Parity | ||||
| 0 | 79 (49.4) | 46 (73) | 33 (34) | <0.001 + |
| 1 | 61 (38.1) | 13 (20.6) | 48 (49.5) | |
| >1 | 20 (12.5) | 4 (6.3) | 16 (16.5) | |
| Type of previous labor | ||||
| Vaginal | 16 (19.8) | 8 (47.1) | 8 (12.5) | 0.010 ++ |
| C-section | 62 (76.5) | 9 (52.9) | 53 (82.8) | |
| Both | 3 (3.7) | 0 (0.0) | 3 (4.7) | |
| Psychiatric history | 21 (13.1) | 8 (12.7) | 8 (8.2) | 0.337 + |
| Number of traumatic events, median (IQR) | 1 (0–2) | 2 (0–4) | 1 (0–3) | 0.012 ‡‡ |
| Medical history | 54 (33.8) | 23 (36.5) | 31 (32) | 0.552 + |
| Title | Total Sample (N = 160) | Type of C-Section | p | |
|---|---|---|---|---|
| Emergency (N = 63; 39.4%) | Planned (N = 97; 60.6%) | |||
| N (%) | N (%) | N (%) | ||
| Conception | ||||
| Normal | 145 (90.6) | 58 (92.1) | 87 (89.7) | 0.615 + |
| IVF | 15 (9.4) | 5 (7.9) | 10 (10.3) | |
| Problems during pregnancy | 70 (43.8) | 35 (55.6) | 35 (36.1) | 0.015 + |
| Gestational week, mean (SD) | 37.7 (2.1) | 37.4 (3) | 38 (1.2) | 0.066 ‡ |
| Preterm labor | 133 (83.1) | 48 (76.2) | 85 (87.6) | 0.059 + |
| NICU | 30 (18.8) | 19 (30.2) | 11 (11.3) | 0.003 + |
| Support from spouse | 132 (82.5) | 46 (73) | 86 (88.7) | 0.011 + |
| Expectations | 89 (55.6) | 16 (25.4) | 73 (75.3) | <0.001 + |
| Traumatic c-section | 64 (40) | 45 (71.4) | 19 (19.6) | <0.001 + |
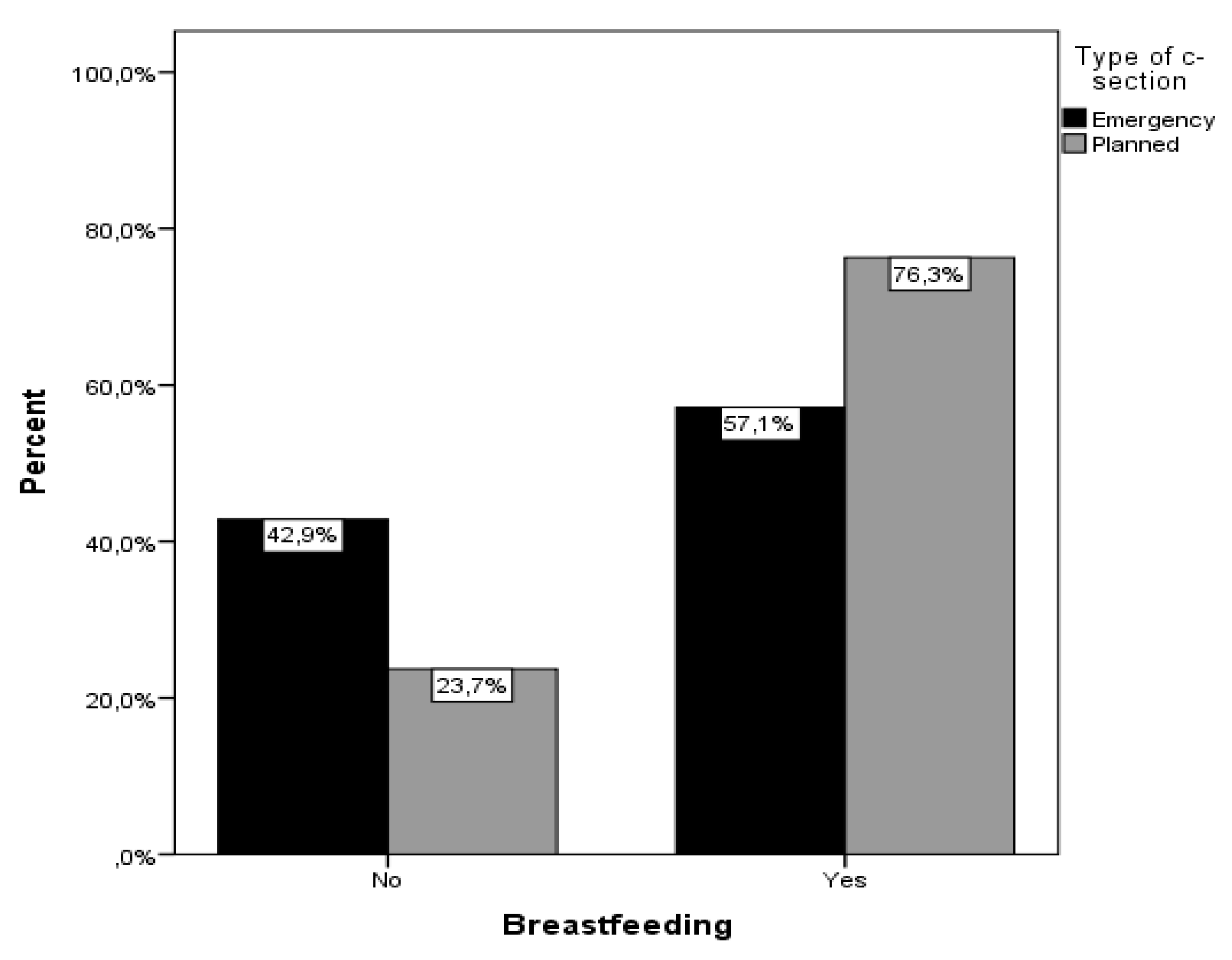
| Breastfeeding | 110 (68.8) | 36 (57.1) | 74 (76.3) | 0.011 + |
| Total Sample (N = 160) | Type of C-Section | p | ||
|---|---|---|---|---|
| Emergency (N = 63; 39.4%) | Planned (N = 97; 60.6%) | |||
| N (%) | N (%) | N (%) | ||
| Criterion Α | 41 (25.6) | 34 (54) | 7 (7.2) | <0.001 + |
| Criterion B | 42 (26.3) | 33 (52.4) | 9 (9.3) | <0.001 + |
| Criterion C | 42 (26.3) | 32 (50.8) | 10 (10.3) | <0.001 + |
| Criterion D | 43 (26.9) | 33 (52.4) | 10 (10.3) | <0.001 + |
| Criterion E | 31 (19.4) | 23 (36.5) | 8 (8.2) | <0.001 + |
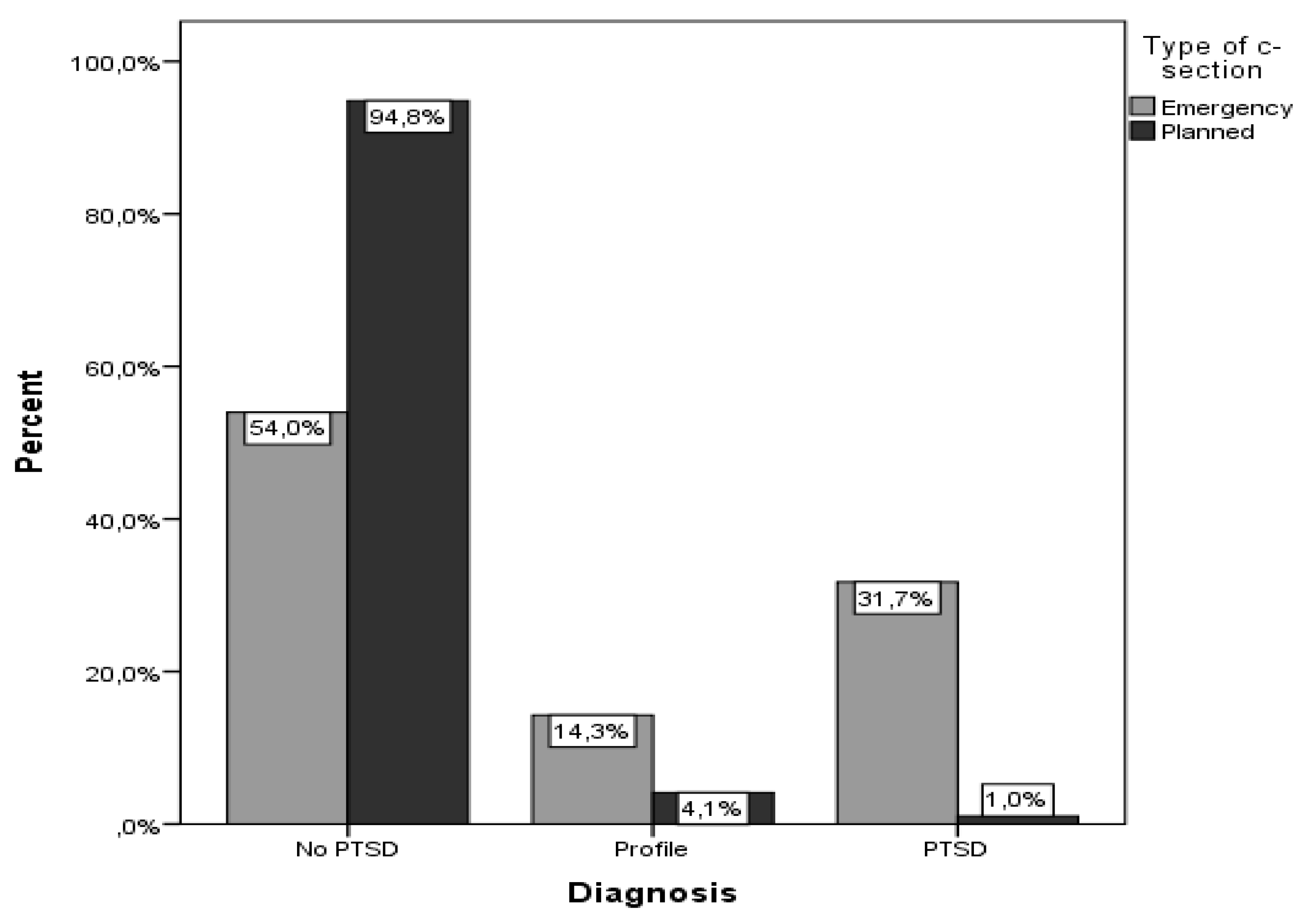
| Diagnosis | ||||
| No PTSD | 126 (78.8) | 34 (54) | 92 (94.8) | <0.001 + |
| Profile | 13 (8.1) | 9 (14.3) | 4 (4.1) | |
| PTSD | 21 (13.1) | 20 (31.7) | 1 (1.0) | |
| PTSD score, median (IQR) | 2 (0–17) | 17 (2–32) | 0 (0–4) | <0.001 ‡‡ |
| Τotal Sample (N=160) | Diagnosis | Unadjusted OR (95% CI) | p | Adjusted OR (95% CI) | p | ||
|---|---|---|---|---|---|---|---|
| No PTSD/Profile | PTSD | ||||||
| N (%) | N (%) | ||||||
| Age | 33.3 (5.7) | 32 (7.3) | 0.97 (0.90–1.04) | 0.380 | 0.89 (0.77–1.03) | 0.105 | |
| Married/Engaged/In a relationship | No | 5 (83.3) | 1 (16.7) | 1.00+ | 1.00 | ||
| Yes | 134 (87.0) | 20 (13.0) | 0.75 (0.08–6.72) | 0.794 | 0.53 (0.01–54.52) | 0.787 | |
| Educational level | Primary/Middle/High school graduate | 70 (86.4) | 11 (13.6) | 1.00 | 1.00 | ||
| University alumni/MSc/PhD | 69 (87.3) | 10 (12.7) | 0.92 (0.37–2.31) | 0.863 | 1.43 (0.33–6.13) | 0.630 | |
| Financial status | Low | 14 (77.8) | 4 (22.2) | 1.00 | 1.00 | ||
| Middle/High | 125 (88.0) | 17 (12.0) | 0.48 (0.14–1.61) | 0.234 | 2.26 (0.16–32.05) | 0.548 | |
| Nationality | Greek | 129 (86.6) | 20 (13.4) | 1.00 | 1.00 | ||
| Other | 10 (90.9) | 1 (9.1) | 0.65 (0.08–5.31) | 0.684 | 0.16 (0.01–3.11) | 0.225 | |
| Parity | 0 | 66 (83.5) | 13 (16.5) | 1.00 | 1.00 | ||
| ≥1 | 73 (90.1) | 8 (9.9) | 0.56 (0.22–1.43) | 0.222 | 1.36 (0.11–16.79) | 0.810 | |
| Previous c-section | No | 79 (83.2) | 16 (16.8) | 1.00 | 1.00 | ||
| Yes | 60 (92.3) | 5 (7.7) | 0.41 (0.14–1.19) | 0.100 | 0.9 (0.05–15.07) | 0.944 | |
| Psychiatric history | No | 126 (90.6) | 13 (9.4) | 1.00 | 1.00 | ||
| Yes | 13 (61.9) | 8 (38.1) | 5.96 (2.09–17.04) | 0.001 | 2.79 (0.55–14.17) | 0.216 | |
| Number of traumatic events, median (IQR) | 1(0–3) | 3(1-5) | 1.29(1.06–1.57) | 0.013 | 1.34(0.84–2.18) | 0.211 | |
| Full-term labor | No | 18 (66.7) | 9 (33.3) | 1.00 | 1.00 | ||
| Yes | 121 (91) | 12 (9) | 0.19 (0.07–0.54) | 0.001 | 0.34 (0.06–1.83) | 0.208 | |
| Type of c-section | Planned | 96 (99.0) | 1 (1.0) | 1.00 | 1.00 | ||
| Emergency | 43 (68.3) | 20 (31.7) | 44.65 (5.80–343.50) | <0.001 | 46.55 (6.00–360.81) | <0.001 | |
| NICU | No | 121 (93.1) | 9 (6.9) | 1.00 | 1.00 | ||
| Yes | 18 (60.0) | 12 (40) | 8.96 (3.31–24.27) | <0.001 | 9.00 (3.31–24.49) | <0.001 | |
| Support from spouse | No | 20 (71.4) | 8 (28.6) | 1.00 | 1.00 | ||
| Yes | 119 (90.2) | 13 (9.8) | 0.27 (0.10–0.74) | 0.011 | 0.27 (0.10–0.74) | 0.011 | |
| Expectations | No | 50 (70.4) | 21 (29.6) | ||||
| Yes | 89 (100.0) | 0 (0.0) | ++ | - | - | - | |
| Traumatic c-section | No | 96 (100.0) | 0 (0.0) | ||||
| Yes | 43 (67.2) | 21 (32.8) | ++ | - | - | - | |
| Breastfeeding | No | 34 (68.0) | 16 (32.0) | 1.00 | 1.00 | ||
| Yes | 105 (95.5) | 5 (4.5) | 0.10 (0.03–0.30) | <0.001 | 0.08 (0.02–0.25) | <0.001 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Orovou, E.; Dagla, M.; Iatrakis, G.; Lykeridou, A.; Tzavara, C.; Antoniou, E. Correlation between Kind of Cesarean Section and Posttraumatic Stress Disorder in Greek Women. Int. J. Environ. Res. Public Health 2020, 17, 1592. https://doi.org/10.3390/ijerph17051592
Orovou E, Dagla M, Iatrakis G, Lykeridou A, Tzavara C, Antoniou E. Correlation between Kind of Cesarean Section and Posttraumatic Stress Disorder in Greek Women. International Journal of Environmental Research and Public Health. 2020; 17(5):1592. https://doi.org/10.3390/ijerph17051592
Chicago/Turabian StyleOrovou, Eirini, Maria Dagla, Georgios Iatrakis, Aikaterini Lykeridou, Chara Tzavara, and Evangelia Antoniou. 2020. "Correlation between Kind of Cesarean Section and Posttraumatic Stress Disorder in Greek Women" International Journal of Environmental Research and Public Health 17, no. 5: 1592. https://doi.org/10.3390/ijerph17051592








