A Hierarchical Age–Period–Cohort Analysis of Breast Cancer Mortality and Disability Adjusted Life Years (1990–2015) Attributable to Modified Risk Factors among Chinese Women
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Outcomes
2.3. Predictors
2.4. Statistical Analysis
3. Results
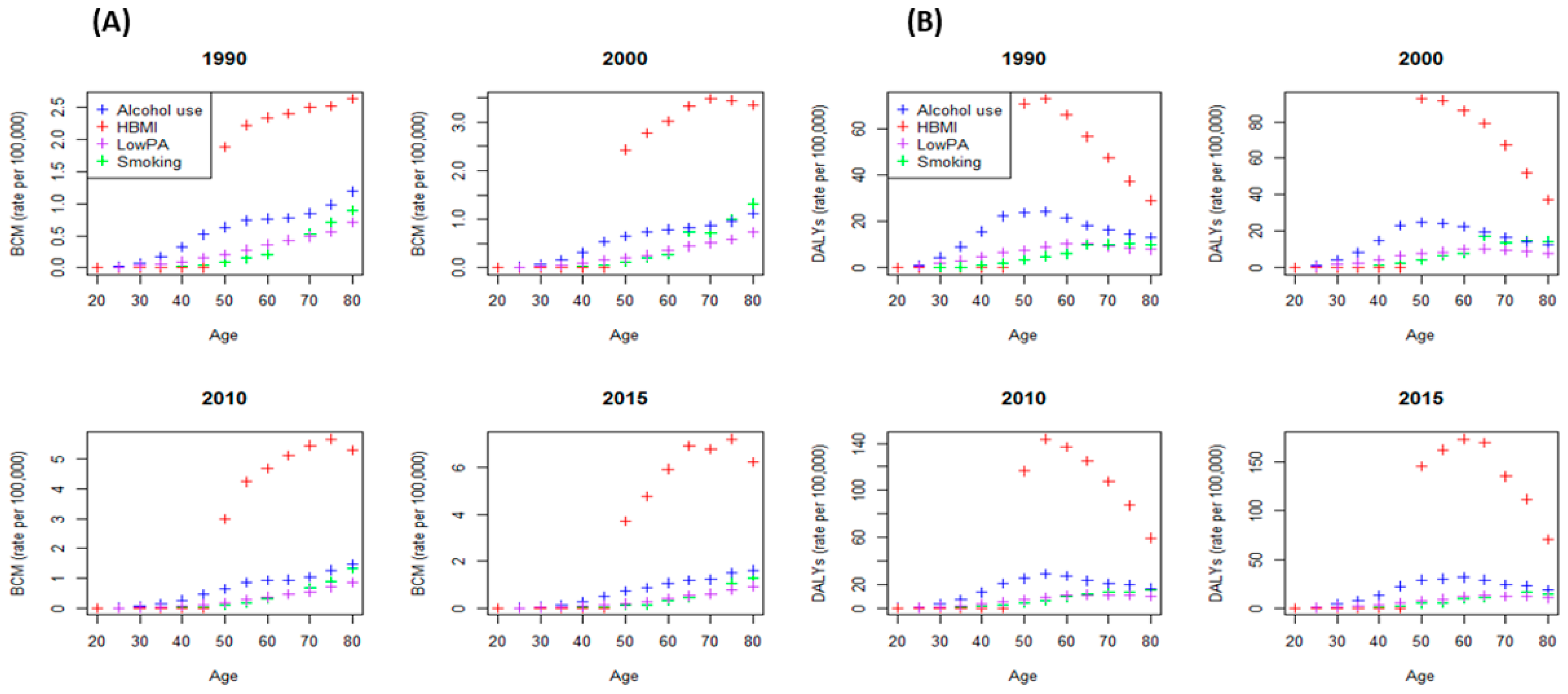
3.1. Mortality Rates (MRs)
3.2. Disability-Adjusted Life Years (DALYs)
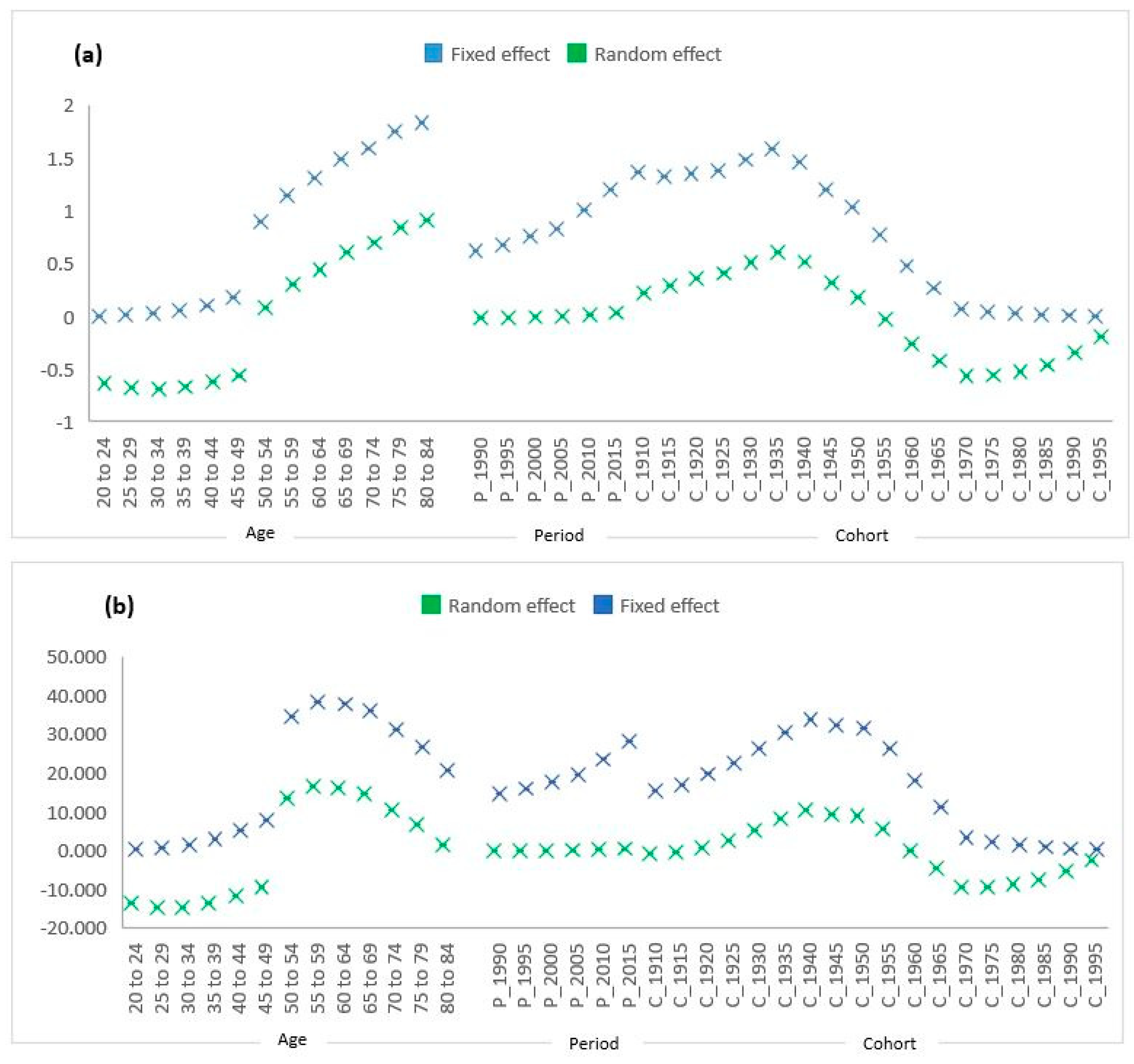
3.3. Random Effects of Age, Period, Cohort, and Interaction with Risk Factors
3.4. Fixed and Random Effects Comparison
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Torre, L.A.; Trabert, B.; DeSantis, C.E.; Miller, K.D.; Samimi, G.; Runowicz, C.D.; Gaudet, M.M.; Jemal, A.; Siegel, R.L. Ovarian cancer statistics, 2018. CA Cancer J. Clin. 2018, 68, 284–296. [Google Scholar] [CrossRef] [PubMed]
- Malik, S.S.; Mubarik, S.; Masood, N.; Khadim, M.T. An insight into clinical outcome of XPG polymorphisms in breast cancer. Mol. Biol. Rep. 2018, 45, 2369–2375. [Google Scholar] [CrossRef] [PubMed]
- Fitzmaurice, C.; Akinyemiju, T.F.; Al Lami, F.H.; Alam, T.; Alizadeh-Navaei, R.; Allen, C.; Alsharif, U.; Alvis-Guzman, N.; Amini, E.; Anderson, B.O. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2016: A systematic analysis for the global burden of disease study. JAMA Oncol. 2018, 4, 1553–1568. [Google Scholar] [PubMed]
- Lin, Y.; Chen, J.; Shen, B. Interactions between genetics, lifestyle, and environmental factors for healthcare. In Translational Informatics in Smart Healthcare; Springer: Berlin/Heidelberg, Germany, 2017; pp. 167–191. [Google Scholar]
- Demark-Wahnefried, W.; Rogers, L.Q.; Alfano, C.M.; Thomson, C.A.; Courneya, K.S.; Meyerhardt, J.A.; Stout, N.L.; Kvale, E.; Ganzer, H.; Ligibel, J.A. Practical clinical interventions for diet, physical activity, and weight control in cancer survivors. CA Cancer J. Clin. 2015, 65, 167–189. [Google Scholar] [CrossRef] [PubMed]
- Anders, C.K.; Johnson, R.; Litton, J.; Phillips, M.; Bleyer, A. Breast cancer before age 40 years. Semin. Oncol. 2009, 36, 237–249. [Google Scholar] [CrossRef] [PubMed]
- Malik, S.S.; Baig, M.; Khan, M.B.; Masood, N. Survival analysis of breast cancer patients with different treatments: A multi-centric clinicopathological study. JPMA 2019, 69, 976–980. [Google Scholar]
- Picon-Ruiz, M.; Morata-Tarifa, C.; Valle-Goffin, J.J.; Friedman, E.R.; Slingerland, J.M. Obesity and adverse breast cancer risk and outcome: Mechanistic insights and strategies for intervention. CA Cancer J. Clin. 2017, 67, 378–397. [Google Scholar] [CrossRef]
- González, N.; Moreno-Villegas, Z.; González-Bris, A.; Egido, J.; Lorenzo, Ó. Regulation of visceral and epicardial adipose tissue for preventing cardiovascular injuries associated to obesity and diabetes. Cardiovasc. Diabetol. 2017, 16, 44. [Google Scholar] [CrossRef]
- Eckel, R.H.; Kahn, S.E.; Ferrannini, E.; Goldfine, A.B.; Nathan, D.M.; Schwartz, M.W.; Smith, R.J.; Smith, S.R. Obesity and type 2 diabetes: What can be unified and what needs to be individualized? J. Clin. Endocrinol. Metab. 2011, 96, 1654–1663. [Google Scholar] [CrossRef]
- La Vecchia, C.; Giordano, S.H.; Hortobagyi, G.N.; Chabner, B. Overweight, obesity, diabetes, and risk of breast cancer: Interlocking pieces of the puzzle. Oncologist 2011, 16, 726. [Google Scholar] [CrossRef]
- Vance, V.; Mourtzakis, M.; McCargar, L.; Hanning, R. Weight gain in breast cancer survivors: Prevalence, pattern and health consequences. Obes. Rev. 2011, 12, 282–294. [Google Scholar] [CrossRef] [PubMed]
- Demark-Wahnefried, W.; Campbell, K.L.; Hayes, S.C. Weight management and its role in breast cancer rehabilitation. Cancer 2012, 118, 2277–2287. [Google Scholar] [CrossRef] [PubMed]
- Playdon, M.C.; Bracken, M.B.; Sanft, T.B.; Ligibel, J.A.; Harrigan, M.; Irwin, M.L. Weight gain after breast cancer diagnosis and all-cause mortality: Systematic review and meta-analysis. JNSI J. Natl. Cancer Inst. 2015, 107. [Google Scholar] [CrossRef] [PubMed]
- Nelson, S.H.; Marinac, C.R.; Patterson, R.E.; Nechuta, S.J.; Flatt, S.W.; Caan, B.J.; Kwan, M.L.; Poole, E.M.; Chen, W.Y.; Shu, X.-O. Impact of very low physical activity, BMI, and comorbidities on mortality among breast cancer survivors. Breast Cancer Res. Treat. 2016, 155, 551–557. [Google Scholar] [CrossRef]
- Calle, E.E.; Rodriguez, C.; Walker-Thurmond, K.; Thun, M.J. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of US adults. N. Engl. J. Med. 2003, 348, 1625–1638. [Google Scholar] [CrossRef]
- Lu, Y.; Ma, H.; Malone, K.E.; Norman, S.A.; Sullivan-Halley, J.; Strom, B.L.; Marchbanks, P.A.; Spirtas, R.; Burkman, R.T.; Deapen, D. Obesity and survival among black women and white women 35 to 64 years of age at diagnosis with invasive breast cancer. J. Clin. Oncol. 2011, 29, 3358. [Google Scholar] [CrossRef]
- Kwan, M.L.; John, E.M.; Caan, B.J.; Lee, V.S.; Bernstein, L.; Cheng, I.; Gomez, S.L.; Henderson, B.E.; Keegan, T.H.; Kurian, A.W. Obesity and mortality after breast cancer by race/ethnicity: The California Breast Cancer Survivorship Consortium. Am. J. Epidemiol. 2014, 179, 95–111. [Google Scholar] [CrossRef]
- Kyu, H.H.; Bachman, V.F.; Alexander, L.T.; Mumford, J.E.; Afshin, A.; Estep, K.; Veerman, J.L.; Delwiche, K.; Iannarone, M.L.; Moyer, M.L. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: Systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013. BMJ 2016, 354, i3857. [Google Scholar] [CrossRef]
- Loprinzi, P.D.; Cardinal, B.J.; Smit, E.; Winters-Stone, K.M. Physical activity and breast cancer risk. J. Exerc. Sci. Fit. 2012, 10, 1–7. [Google Scholar] [CrossRef]
- Maliniak, M.L.; Patel, A.V.; McCullough, M.L.; Campbell, P.T.; Leach, C.R.; Gapstur, S.M.; Gaudet, M.M. Obesity, physical activity, and breast cancer survival among older breast cancer survivors in the Cancer Prevention Study-II Nutrition Cohort. Breast Cancer Res. Treat. 2018, 167, 133–145. [Google Scholar] [CrossRef]
- Burden of cancer in the Eastern Mediterranean Region, 2005–2015: Findings from the Global Burden of Disease 2015 Study. Int. J. Public Health 2018, 63, 151–164. [CrossRef] [PubMed]
- Mubarik, S.; Malik, S.S.; Wang, Z.; Li, C.; Fawad, M.; Yu, C. Recent insights into breast cancer incidence trends among four Asian countries using age-period-cohort model. Cancer Manag. Res. 2019, 11, 8145. [Google Scholar] [CrossRef] [PubMed]
- Gakidou, E.; Afshin, A.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abdulle, A.M.; Abera, S.F.; Aboyans, V. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1345–1422. [Google Scholar] [CrossRef]
- Zhou, M.; Wang, H.; Zeng, X.; Yin, P.; Zhu, J.; Chen, W.; Li, X.; Wang, L.; Wang, L.; Liu, Y. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019. [Google Scholar] [CrossRef]
- Yang, Y.; Lee, L.C. Dynamics and heterogeneity in the process of human frailty and aging: Evidence from the US older adult population. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2009, 65, 246–255. [Google Scholar] [CrossRef]
- Yang, Y.; Lee, L.C. Sex and race disparities in health: Cohort variations in life course patterns. Soc. Forces 2009, 87, 2093–2124. [Google Scholar] [CrossRef]
- Bell, A.; Jones, K. The hierarchical age–period–cohort model: Why does it find the results that it finds? Qual. Quant. 2018, 52, 783–799. [Google Scholar] [CrossRef]
- Yang, Y.; Land, K.C. A mixed models approach to the age-period-cohort analysis of repeated cross-section surveys, with an application to data on trends in verbal test scores. Sociol. Methodol. 2006, 36, 75–97. [Google Scholar] [CrossRef]
- Yang, Y. Is old age depressing? Growth trajectories and cohort variations in late-life depression. J. Health Soc. Behav. 2007, 48, 16–32. [Google Scholar] [CrossRef]
- Pinheiro, J. Nlme: Linear and Nonlinear Mixed Effects Models. R Package Version 3.1-96. Available online: http://cran.r-project.org/web/packages/nlme/2009 (accessed on 20 February 2020).
- Gordon-Larsen, P.; Wang, H.; Popkin, B.M. Overweight dynamics in Chinese children and adults. Obes. Rev. 2014, 15, 37–48. [Google Scholar] [CrossRef]
- Momenimovahed, Z.; Salehiniya, H. Epidemiological characteristics of and risk factors for breast cancer in the world. Breast Cancer 2019, 11, 151–164. [Google Scholar] [CrossRef] [PubMed]
- DeSantis, C.E.; Ma, J.; Goding Sauer, A.; Newman, L.A.; Jemal, A. Breast cancer statistics, 2017, racial disparity in mortality by state. CA Cancer J. Clin. 2017, 67, 439–448. [Google Scholar] [CrossRef] [PubMed]
- India State-Level Disease Burden Initiative Cancer Collaborators. The burden of cancers and their variations across the states of India: The Global Burden of Disease Study 1990–2016. Lancet Oncol. 2018, 19, 1289–1306. [Google Scholar] [CrossRef]
- Youlden, D.R.; Cramb, S.M.; Yip, C.H.; Baade, P.D. Incidence and mortality of female breast cancer in the Asia-Pacific region. Cancer Biol. Med. 2014, 11, 101–115. [Google Scholar]
- Silva, D.A.S.; Tremblay, M.S.; de Souza, M.D.F.M.; Guerra, M.R.; Mooney, M.; Naghavi, M.; Malta, D.C. Mortality and years of life lost due to breast cancer attributable to physical inactivity in the Brazilian female population (1990–2015). Sci. Rep. 2018, 8, 11141. [Google Scholar] [CrossRef]
- Conroy, S.M.; Maskarinec, G.; Wilkens, L.R.; White, K.K.; Henderson, B.E.; Kolonel, L.N. Obesity and breast cancer survival in ethnically diverse postmenopausal women: The Multiethnic Cohort Study. Breast Cancer Res. Treat. 2011, 129, 565–574. [Google Scholar] [CrossRef]


| Predictors | GLM | Mixed Effect Models | ||||
| Model Estimate | Model 1 Estimate | Model 2 Estimate | Model 3 Estimate | |||
| (Intercept) | −0.164 (0.591) | −1.733 (0.000) | −1.128 (0.006) | −0.164 (0.662) | ||
| Age | 0.011 (0.046) | 0.042 (0.000) | 0.030 (0.001) | 0.010 (0.0450) | ||
| Period (Reference 1990) | ||||||
| 1995 | 0.074 (0.840) | 0.057 (0.576) | 0.074 (0.797) | 0.074 (0.798) | ||
| 2000 | 0.209 (0.568) | 0.135 (0.186) | 0.209 (0.468) | 0.209 (0.471) | ||
| 2005 | 0.344 (0.349) | 0.215 (0.036) | 0.344(0.233) | 0.344 (0.236) | ||
| 2010 | 0.663 (0.072) | 0.392 (0.000) | 0.662 (0.022) | 0.663 (0.023) | ||
| 2015 | 0.950 (0.010) | 0.587 (0.000) | 0.950 (0.001) | 0.950 (0.001) | ||
| Risk (Reference: alcohol use) | ||||||
| HBMI | 2.155 (0.000) | 1.438 (0.000) | 1.437 (0.000) | 2.154 (0.000) | ||
| Low PA | 0.096 (0.744) | −0.394 (0.191) | −0.394 (0.195) | −0.096 (0.848) | ||
| Smoking | −0.354 (0.277) | −0.435 (0.160) | −0.435 (0.164) | −0.354 (0.526) | ||
| Age × 1995 | 0.003 (0.705) | 0.002 (0.630) | 0.003 (0.632) | |||
| Age × 2000 | 0.007 (0.321) | 0.006 (0.207) | 0.007 (0.210) | |||
| Age × 2005 | 0.011 (0.108) | 0.010 (0.041) | 0.011 (0.042) | |||
| Age × 2010 | 0.020 (0.003) | 0.020 (0.000) | 0.020 (0.000) | |||
| Age × 2015 | 0.030 (0.000) | 0.029 (0.000) | 0.030 (0.000) | |||
| Age × HBMI | 0.072 (0.000) | 0.072 (0.000) | ||||
| Age × Low PA | −0.008 (0.120) | −0.008 (0.365) | ||||
| Age × Smoking | 0.000 (0.962) | 0.000 (0.978) | ||||
| Model Selection Parameter Estimates among GLM and Mixed-Effect Models | ||||||
| Model | AIC | BIC | Log Likelihood | Test | L Ratio | p-Value |
| GLM | 545.1321 | 615.1202 | −253.566 | |||
| Model 1 | 573.7778 | 621.6644 | −273.889 | GLM vs. 1 | 40.64567 | <0.0001 |
| Model 2 | 538.8635 | 605.0037 | −251.432 | 1 vs. 2 | 44.86496 | <0.0001 |
| Model 3 | 485.8985 | 563.2537 | −221.949 | 2 vs. 3 | 59.0393 | <0.0001 |
| Predictors | GLM | Mixed Effect Models | ||||
| Model Estimate | Model 1 Estimate | Model 2 Estimate | Model 3 Estimate | |||
| (Intercept) | 5.143 (0.635) | −24.939 (0.020) | −13.866 (0.232) | 5.143 (0.735) | ||
| Age | 0.103 (0.040) | 0.698 (0.002) | 0.483 (0.029) | 0.104 (0.042) | ||
| Period (Reference: 1990) | ||||||
| 1995 | 0.836 (0.949) | 1.381 (0.565) | 0.836 (0.905) | 0.836 (0.905) | ||
| 2000 | 3.020 (0.817) | 3.098 (0.197) | 3.019 (0.667) | 3.019 (0.669) | ||
| 2005 | 5.591 (0.669) | 4.953 (0.039) | 5.590(0.426) | 5.591 (0.429) | ||
| 2010 | 10.290 (0.043) | 8.934 (0.000) | 10.290 (0.0144) | 10.290 (0.015) | ||
| 2015 | 14.734(0.026) | 13.600 (0.000) | 14.734 (0.036) | 14.734 (0.037) | ||
| Risk (Reference: alcohol use) | ||||||
| HBMI | 37.666 (0.000) | 31.728 (0.000) | 31.728 (0.000) | 37.666 (0.006) | ||
| Low PA | −2.368 (0.822) | −10.199 (0.247) | −10.198 (0.251) | −2.440 (0.909) | ||
| Smoking | −10.349 (0.374) | −11.891 (0.190) | −11.891 (0.194) | −11.162 (0.641) | ||
| Age × 1995 | 0.043 (0.858) | 0.042 (0.738) | 0.043 (0.739) | |||
| Age × 2000 | 0.118 (0.621) | 0.118 (0.357) | 0.118 (0.360) | |||
| Age × 2005 | 0.204 (0.394) | 0.203 (0.113) | 0.204 (0.115) | |||
| Age × 2010 | 0.372 (0.121) | 0.371 (0.004) | 0.372 (0.004) | |||
| Age × 2015 | 0.548 (0.023) | 0.547 (0.000) | 0.548 (0.000) | |||
| Age × HBMI | 1.388 (0.000) | 1.388 (0.000) | ||||
| Age × Low PA | −0.131 (0.497) | −0.129 (0.741) | ||||
| Age × Smoking | 0.007 (0.975) | 0.0193 (0.963) | ||||
| Models Selection Parameters Estimates among GLM and Mixed Effect Models | ||||||
| Model | AIC | BIC | Log Likelihood | Test | L. Ratio | p-Value |
| GLM | 2646.76 | 2716.74 | −1304.38 | |||
| Model 1 | 2451.29 | 2499.18 | −1212.64 | GLM vs. 1 | 183.46 | <0.0001 |
| Model 2 | 2434.55 | 2500.86 | −1199.27 | 1 vs. 2 | 26.73 | <0.0001 |
| Model 3 | 2422.40 | 2499.76 | −1190.20 | 2 vs. 3 | 18.14 | <0.0004 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mubarik, S.; Wang, F.; Malik, S.S.; Shi, F.; Wang, Y.; Nawsherwan; Yu, C. A Hierarchical Age–Period–Cohort Analysis of Breast Cancer Mortality and Disability Adjusted Life Years (1990–2015) Attributable to Modified Risk Factors among Chinese Women. Int. J. Environ. Res. Public Health 2020, 17, 1367. https://doi.org/10.3390/ijerph17041367
Mubarik S, Wang F, Malik SS, Shi F, Wang Y, Nawsherwan, Yu C. A Hierarchical Age–Period–Cohort Analysis of Breast Cancer Mortality and Disability Adjusted Life Years (1990–2015) Attributable to Modified Risk Factors among Chinese Women. International Journal of Environmental Research and Public Health. 2020; 17(4):1367. https://doi.org/10.3390/ijerph17041367
Chicago/Turabian StyleMubarik, Sumaira, Fang Wang, Saima Shakil Malik, Fang Shi, Yafeng Wang, Nawsherwan, and Chuanhua Yu. 2020. "A Hierarchical Age–Period–Cohort Analysis of Breast Cancer Mortality and Disability Adjusted Life Years (1990–2015) Attributable to Modified Risk Factors among Chinese Women" International Journal of Environmental Research and Public Health 17, no. 4: 1367. https://doi.org/10.3390/ijerph17041367
APA StyleMubarik, S., Wang, F., Malik, S. S., Shi, F., Wang, Y., Nawsherwan, & Yu, C. (2020). A Hierarchical Age–Period–Cohort Analysis of Breast Cancer Mortality and Disability Adjusted Life Years (1990–2015) Attributable to Modified Risk Factors among Chinese Women. International Journal of Environmental Research and Public Health, 17(4), 1367. https://doi.org/10.3390/ijerph17041367






