Early Discharged Lumbar Spine Fusion Reduced Postoperative Readmissions: A Retrospective Cohort Study
Abstract
1. Introduction
2. Material and Methods
2.1. Data Source and Ethical Concerns
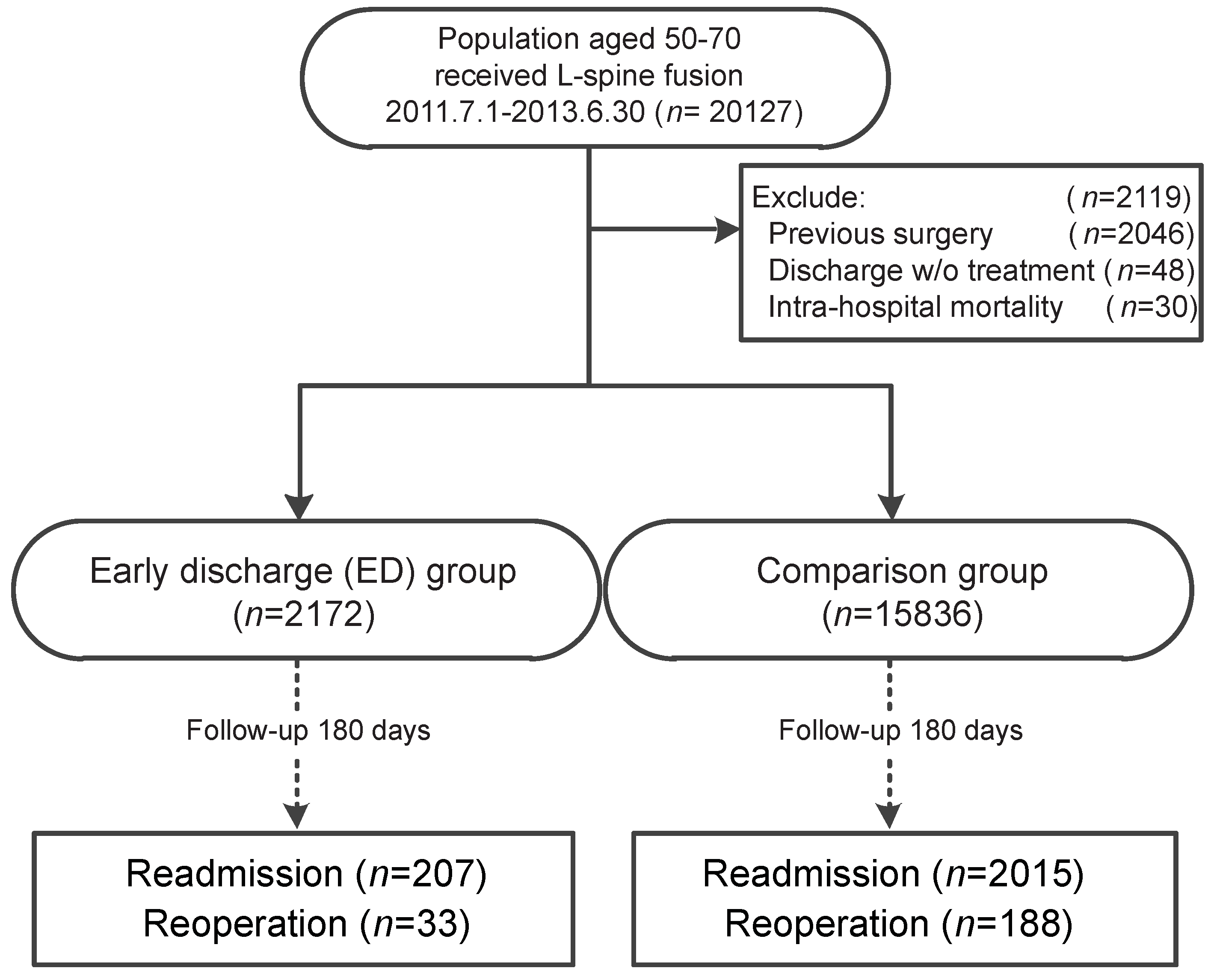
2.2. Study Cohort
2.3. ED Group vs. Comparison Group
2.4. Follow-Up Outcomes and Covariates
2.5. Statistical Analysis
3. Results
3.1. Demographics of the Cohort
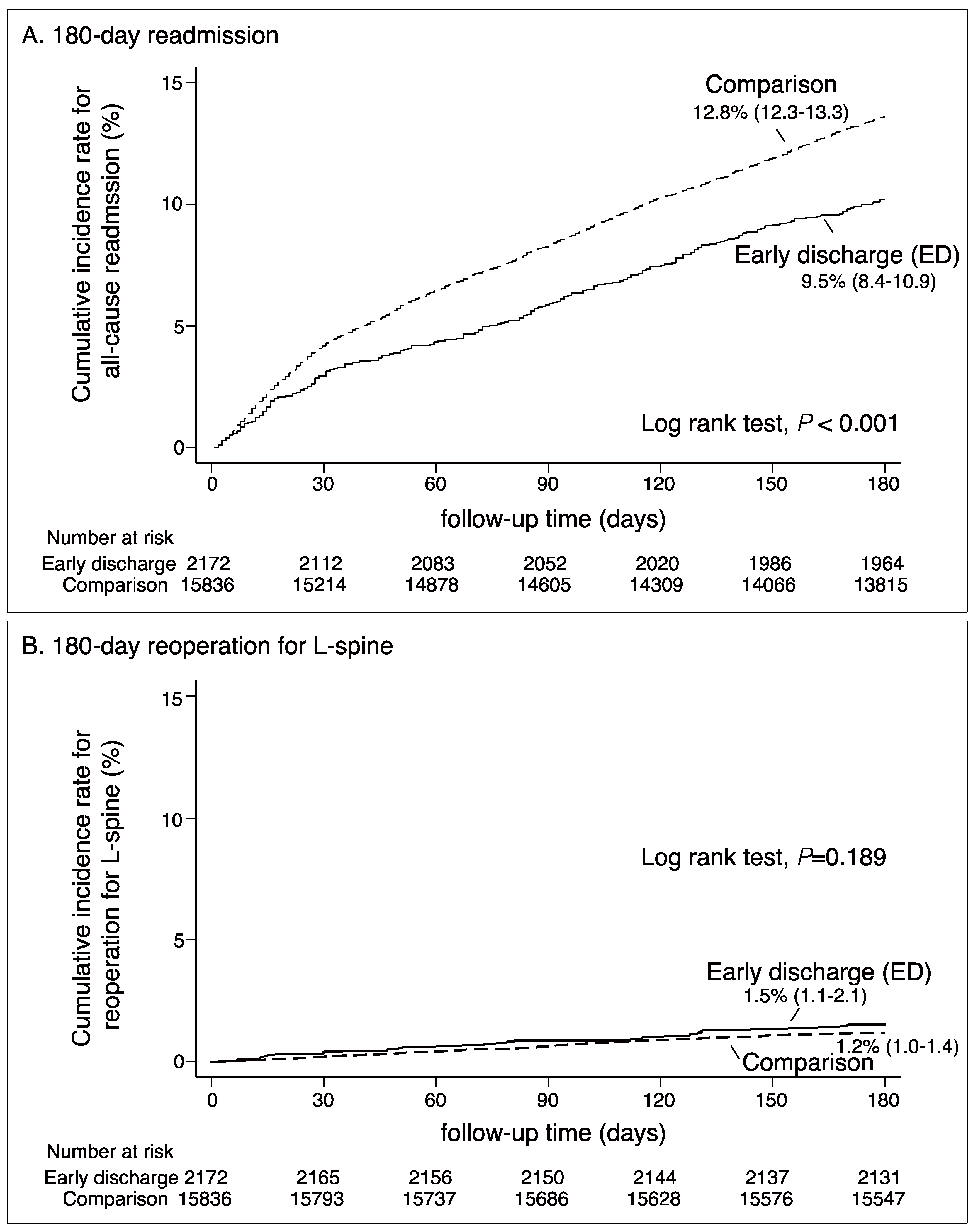
3.2. Readmission Rates
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Cummock, M.D.; Vanni, S.; Levi, A.D.; Yu, Y.; Wang, M.Y. An analysis of postoperative thigh symptoms after minimally invasive transpsoas lumbar interbody fusion. J. Neurosurg. Spine 2011, 15, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Hofstetter, C.P.; Hofer, A.S.; Wang, M.Y. Economic impact of minimally invasive lumbar surgery. World J. Orthop. 2015, 6, 190–201. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.A.; Zfass-Mendez, M.; Lebwohl, N.H.; Wang, M.Y.; Green, B.A.; Levi, A.D.; Vanni, S.; Williams, S.K. Minimally Invasive Versus Open Lumbar Fusion: A Comparison of Blood Loss, Surgical Complications, and Hospital Course. Iowa Orthop. J. 2015, 35, 130–134. [Google Scholar] [PubMed]
- Wang, M.Y.; Cummock, M.D.; Yu, Y.; Trivedi, R.A. An analysis of the differences in the acute hospitalization charges following minimally invasive versus open posterior lumbar interbody fusion. J. Neurosurg. Spine 2010, 12, 694–699. [Google Scholar] [CrossRef]
- Wang, M.Y.; Lerner, J.; Lesko, J.; McGirt, M.J. Acute hospital costs after minimally invasive versus open lumbar interbody fusion: Data from a US national database with 6106 patients. J. Spinal Disord. Tech. 2012, 25, 324–328. [Google Scholar] [CrossRef]
- Wang, M.Y.; Vasudevan, R.; Mindea, S.A. Minimally invasive lateral interbody fusion for the treatment of rostral adjacent-segment lumbar degenerative stenosis without supplemental pedicle screw fixation. J. Neurosurg. Spine 2014, 21, 861–866. [Google Scholar] [CrossRef]
- Chang, H.K.; Kolcun, J.P.G.; Chang, P.Y.; Wang, M.Y. Enhanced Recovery After Surgery Awake Minimally-Invasive Transforaminal Lumbar Interbody Fusion: 2-Dimensional Operative Video. Oper. Neurosurg. 2018. [Google Scholar] [CrossRef]
- Grasu, R.M.; Cata, J.P.; Dang, A.Q.; Tatsui, C.E.; Rhines, L.D.; Hagan, K.B.; Bhavsar, S.; Raty, S.R.; Arunkumar, R.; Potylchansky, Y.; et al. Implementation of an Enhanced Recovery After Spine Surgery program at a large cancer center: A preliminary analysis. J. Neurosurg. Spine 2018. [Google Scholar] [CrossRef]
- Soffin, E.M.; Vaishnav, A.S.; Wetmore, D.; Barber, L.; Hill, P.; Gang, C.H.; Beckman, J.D.; Albert, T.J.; Qureshi, S.A. Design and Implementation of an Enhanced Recovery After Surgery (ERAS) Program for Minimally Invasive Lumbar Decompression Spine Surgery: Initial Experience. Spine 2018. [Google Scholar] [CrossRef]
- Wainwright, T.W.; Immins, T.; Middleton, R.G. Enhanced recovery after surgery (ERAS) and its applicability for major spine surgery. Best Pract. Res. Clin. Anaesthesiol. 2016, 30, 91–102. [Google Scholar] [CrossRef]
- Wang, M.Y.; Chang, H.K.; Grossman, J. Reduced Acute Care Costs With the ERAS(R) Minimally Invasive Transforaminal Lumbar Interbody Fusion Compared with Conventional Minimally Invasive Transforaminal Lumbar Interbody Fusion. Neurosurgery 2018, 83, 827–834. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, N.D.; Andras, L.M.; Lazarus, D.E.; Owen, R.J.; Geddes, B.J.; Cao, J.; Skaggs, D.L.; Oswald, T.S.; Bruce, R.W., Jr. Use of a Novel Pathway for Early Discharge Was Associated With a 48% Shorter Length of Stay After Posterior Spinal Fusion for Adolescent Idiopathic Scoliosis. J. Pediatr. Orthop. 2017, 37, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, N.D.; Shourbaji, N.; Mitchell, P.M.; Oswald, T.S.; Devito, D.P.; Bruce, R.W. Clinical and economic implications of early discharge following posterior spinal fusion for adolescent idiopathic scoliosis. J. Child. Orthop. 2014, 8, 257–263. [Google Scholar] [CrossRef]
- Carreon, L.Y.; Glassman, S.D.; Ghogawala, Z.; Mummaneni, P.V.; McGirt, M.J.; Asher, A.L. Modeled cost-effectiveness of transforaminal lumbar interbody fusion compared with posterolateral fusion for spondylolisthesis using N(2)QOD data. J. Neurosurg. Spine 2016, 24, 916–921. [Google Scholar] [CrossRef]
- Wang, M.Y.; Chang, P.Y.; Grossman, J. Development of an Enhanced Recovery After Surgery (ERAS) approach for lumbar spinal fusion. J. Neurosurg. Spine 2017, 26, 411–418. [Google Scholar] [CrossRef]
- Onyekwelu, I.; Glassman, S.D.; Asher, A.L.; Shaffrey, C.I.; Mummaneni, P.V.; Carreon, L.Y. Impact of obesity on complications and outcomes: A comparison of fusion and nonfusion lumbar spine surgery. J. Neurosurg. Spine 2017, 26, 158–162. [Google Scholar] [CrossRef]
- Ghogawala, Z.; Resnick, D.K.; Glassman, S.D.; Dziura, J.; Shaffrey, C.I.; Mummaneni, P.V. Randomized controlled trials for degenerative lumbar spondylolisthesis: Which patients benefit from lumbar fusion? J. Neurosurg. Spine 2017, 26, 260–266. [Google Scholar] [CrossRef]
- Arrighi-Allisan, A.E.; Neifert, S.N.; Gal, J.S.; Deutsch, B.C.; Caridi, J.M. Discharge Destination as a Predictor of Postoperative Outcomes and Readmission Following Posterior Lumbar Fusion. World Neurosurg. 2018. [Google Scholar] [CrossRef]
- Katz, A.D.; Mancini, N.; Karukonda, T.; Greenwood, M.; Cote, M.; Moss, I. Approach-Based Comparative and Predictor Analysis of 30-Day Readmission, Reoperation, and Morbidity in Patients Undergoing Lumbar Interbody Fusion Using the ACS-NSQIP Dataset. Spine 2018. [Google Scholar] [CrossRef]
- Garcia, R.M.; Khanna, R.; Dahdaleh, N.S.; Cybulski, G.; Lam, S.; Smith, Z.A. Thirty-Day Readmission Risk Factors Following Single-Level Transforaminal Lumbar Interbody Fusion (TLIF) for 4992 Patients From the ACS-NSQIP Database. Glob. Spine J. 2017, 7, 220–226. [Google Scholar] [CrossRef]
- Garcia, R.M.; Choy, W.; DiDomenico, J.D.; Barrington, N.; Dahdaleh, N.S.; Rodriguez, H.E.; Lam, S.; Smith, Z.A. Thirty-day readmission rate and risk factors for patients undergoing single level elective anterior lumbar interbody fusion (ALIF). J. Clin. Neurosci. 2016, 32, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Basques, B.A.; Ibe, I.; Samuel, A.M.; Lukasiewicz, A.M.; Webb, M.L.; Bohl, D.D.; Grauer, J.N. Predicting Postoperative Morbidity and Readmission for Revision Posterior Lumbar Fusion. Clin. Spine Surg. 2017, 30, E770–E775. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.C.; Wu, J.C.; Chen, T.J.; Wetter, T. Reduced access to database. A publicly available database accelerates academic production. BMJ 2011, 342, d637. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.C.; Wu, J.C.; Haschler, I.; Majeed, A.; Chen, T.J.; Wetter, T. Academic impact of a public electronic health database: Bibliometric analysis of studies using the general practice research database. PLoS ONE 2011, 6, e21404. [Google Scholar] [CrossRef]
- Chen, Y.C.; Wu, J.C.; Chang, H.K.; Huang, W.C. Early Discharge for Anterior Cervical Fusion Surgery: Prediction of Readmission and Special Considerations for Older Adults. Int. J. Environ. Res. Public Health 2019, 16, 641. [Google Scholar] [CrossRef]
- Martin, N.; Valero, R.; Hurtado, P.; Gracia, I.; Fernandez, C.; Rumia, J.; Valldeoriola, F.; Carrero, E.J.; Tercero, F.J.; de Riva, N.; et al. Experience with “Fast track” postoperative care after deep brain stimulation surgery. Neurocirugia 2016, 27, 263–268. [Google Scholar] [CrossRef]
- Wang, M.Y.; Grossman, J. Endoscopic minimally invasive transforaminal interbody fusion without general anesthesia: Initial clinical experience with 1-year follow-up. Neurosurg. Focus 2016, 40, E13. [Google Scholar] [CrossRef]
- Gu, J.; Guan, F.; Zhu, L.; Guan, G.; Chi, Z.; Wang, H.; Yu, Z. Risk Factors of Postoperative Low Back Pain for Lumbar Spine Disease. World Neurosurg. 2016, 94, 248–254. [Google Scholar] [CrossRef]
- Kim, J.; Burke, S.M.; Kryzanski, J.T.; Roberts, R.J.; Roguski, M.; Qu, E.; Hwang, S.W.; Liu, P.P.; Desilier, A.; Riesenburger, R.I. The Role of Liposomal Bupivacaine in Reduction of Postoperative Pain After Transforaminal Lumbar Interbody Fusion: A Clinical Study. World Neurosurg. 2016, 91, 460–467. [Google Scholar] [CrossRef]
- Coolsen, M.M.; Wong-Lun-Hing, E.M.; van Dam, R.M.; van der Wilt, A.A.; Slim, K.; Lassen, K.; Dejong, C.H. A systematic review of outcomes in patients undergoing liver surgery in an enhanced recovery after surgery pathways. HPB 2013, 15, 245–251. [Google Scholar] [CrossRef]
| Demographic Characteristics, Comorbidities, and Outcomes | Comparison Group | ED 1 Group | p-Value | |||||
|---|---|---|---|---|---|---|---|---|
| n = 15,836 | (%) | n = 2172 | (%) | |||||
| Gender | <0.001 | |||||||
| Female | 9988 | (63.1) | 1196 | (55.1) | ||||
| Male | 5848 | (36.9) | 976 | (44.9) | ||||
| Age, mean (SD 2) | 60.7 | (5.74) | 59.9 | (5.76) | <0.001 | |||
| Comorbidities | ||||||||
| Anemia | 1041 | (6.6) | 85 | (3.9) | <0.001 | |||
| Chronic pulmonary disease | 2463 | (15.6) | 269 | (12.4) | <0.001 | |||
| Congestive heart failure | 535 | (3.4) | 47 | (2.2) | 0.003 | |||
| Depression | 910 | (5.7) | 103 | (4.7) | 0.057 | |||
| Diabetes | 4406 | (27.8) | 522 | (24.0) | <0.001 | |||
| Hypertension | 7120 | (45.0) | 887 | (40.8) | <0.001 | |||
| Liver disease | 2307 | (14.6) | 279 | (12.8) | 0.032 | |||
| Neurologic disorders | 420 | (2.7) | 44 | (2.0) | 0.084 | |||
| Chronic kidney disease | 270 | (1.7) | 31 | (1.4) | 0.340 | |||
| Chronic peptic ulcer disease | 820 | (5.2) | 107 | (4.9) | 0.620 | |||
| Outcome | ||||||||
| All-cause readmission | ||||||||
| 30-day readmission | 636 | (4.0) | 64 | (2.9) | 0.016 | |||
| 60-day readmission | 962 | (6.1) | 89 | (4.1) | <0.001 | |||
| 180-day readmission | 2015 | (12.7) | 207 | (9.5) | <0.001 | |||
| Re-operation for L-spine | ||||||||
| 30-day re-operation | 33 | (0.2) | 9 | (0.4) | 0.062 | |||
| 60-day re-operation | 66 | (0.4) | 14 | (0.6) | 0.130 | |||
| 180-day re-operation | 188 | (1.2) | 33 | (1.5) | 0.190 | |||
| Readmission during 180-Day-Follow-Up | Comparison Group | ED Group | ||||
|---|---|---|---|---|---|---|
| All-cause readmission | ||||||
| Incidence of readmission (per 1000 person-years) | 275.2 | 201.7 | ||||
| Number of occurrences | 2015 | 207 | ||||
| Observed person-years | 7320.9 | 1026.3 | ||||
| Crude hazard ratio (95% C.I.) 1 | 1.00 | 0.73 | (0.63–0.85) ***,3 | |||
| Adjusted hazard ratio (95% C.I.) 2 | 1.00 | 0.75 | (0.65–0.87) ***,3 | |||
| Reoperation for L-spine | ||||||
| Incidence of reoperation (per 1000 person-years) | 24.0 | 30.7 | ||||
| Number of occurrences | 188 | 33 | ||||
| Observed person-years | 7842.1 | 1075.1 | ||||
| Crude hazard ratio (95% C.I.) 1 | 1.00 | 1.28 | (0.86–1.86) | |||
| Adjusted hazard ratio (95% C.I.) 2 | 1.00 | 1.26 | (0.87–1.83) | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, W.-C.; Wu, J.-C.; Chang, H.-K.; Chen, Y.-C. Early Discharged Lumbar Spine Fusion Reduced Postoperative Readmissions: A Retrospective Cohort Study. Int. J. Environ. Res. Public Health 2020, 17, 1335. https://doi.org/10.3390/ijerph17041335
Huang W-C, Wu J-C, Chang H-K, Chen Y-C. Early Discharged Lumbar Spine Fusion Reduced Postoperative Readmissions: A Retrospective Cohort Study. International Journal of Environmental Research and Public Health. 2020; 17(4):1335. https://doi.org/10.3390/ijerph17041335
Chicago/Turabian StyleHuang, Wen-Cheng, Jau-Ching Wu, Hsuan-Kan Chang, and Yu-Chun Chen. 2020. "Early Discharged Lumbar Spine Fusion Reduced Postoperative Readmissions: A Retrospective Cohort Study" International Journal of Environmental Research and Public Health 17, no. 4: 1335. https://doi.org/10.3390/ijerph17041335
APA StyleHuang, W.-C., Wu, J.-C., Chang, H.-K., & Chen, Y.-C. (2020). Early Discharged Lumbar Spine Fusion Reduced Postoperative Readmissions: A Retrospective Cohort Study. International Journal of Environmental Research and Public Health, 17(4), 1335. https://doi.org/10.3390/ijerph17041335






