The Role of Physical Activity for the Management of Sarcopenia in People Living with HIV
Abstract
1. Introduction
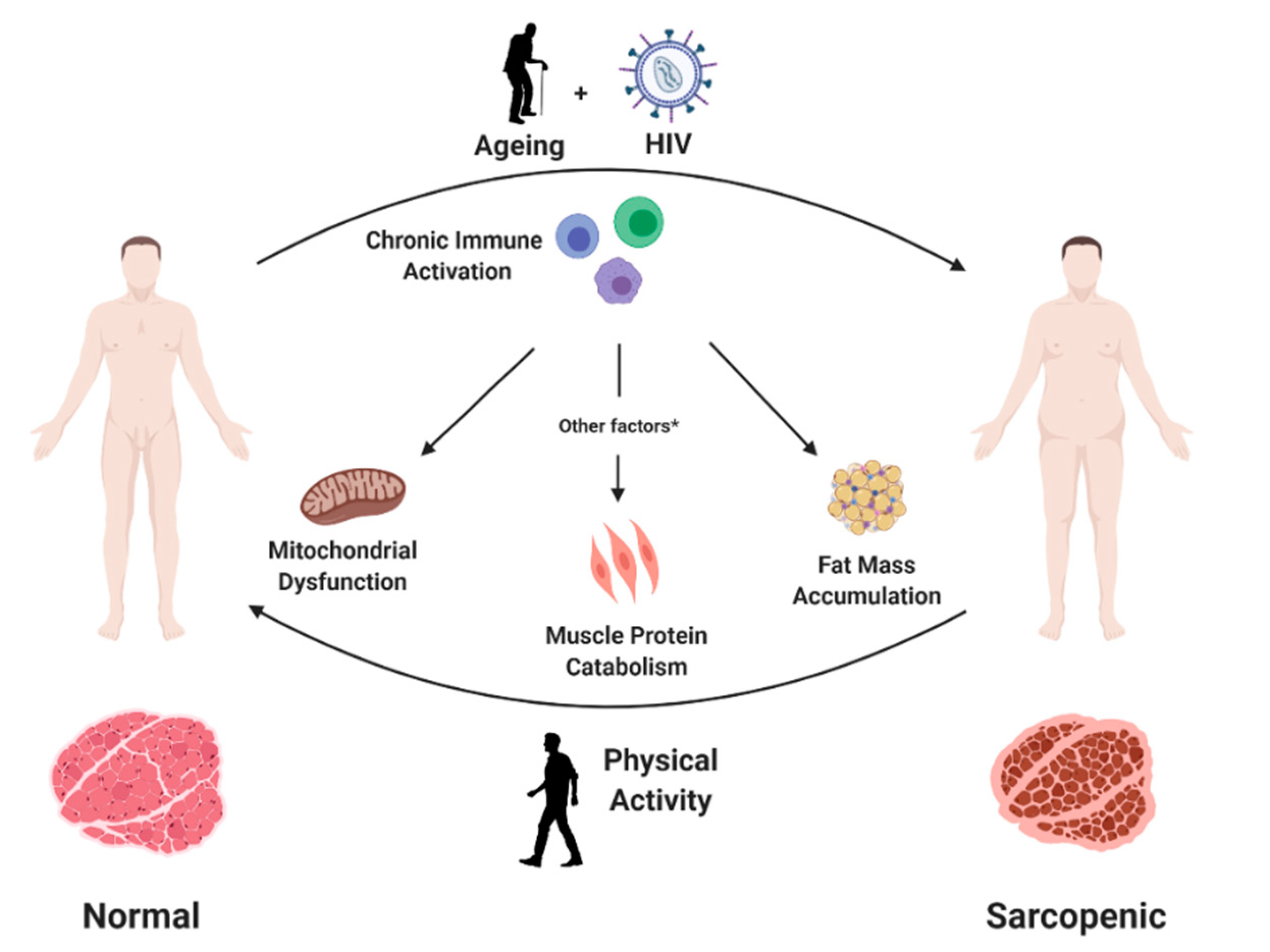
2. Mechanisms of Sarcopenia in People Living with HIV
3. Epidemiological and Clinical Aspects of Sarcopenia in People Living with HIV
4. Exercise Intervention to Counteract Sarcopenia in PLWH
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 601. [Google Scholar] [CrossRef]
- Vitale, J.A.; Bonato, M.; La Torre, A. Banfi. The role of the molecular clock in promoting skeletal muscle growth and protecting against sarcopenia. Int. J. Mol. Sci. 2019, 20, 4318. [Google Scholar] [CrossRef] [PubMed]
- Patel, H.P.; Syddall, H.E.; Jameson, K.; Robinson, S.; Denison, H.; Roberts, H.C.; Edwards, M.; Dennison, E.; Cooper, C.; Aihie Sayer, A. Prevalence of sarcopenia in community-dwelling older people in the UK using the European Working Group on Sarcopenia in Older People (EWGSOP) definition: Findings from the Hertfordshire Cohort Study (HCS). Age Ageing 2013, 42, 378–384. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, R.N.; Koehler, K.M.; Gallagher, D.; Romero, L.; Heymsfield, S.B.; Ross, R.R.; Garry, P.J.; Lindeman, R.D. Epidemiology of sarcopenia among the elderly in New Mexico. Am. J. Epidemiol. 1998, 147, 755–763. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, R.N.; Wayne, S.J.; Waters, D.L.; Janssen, I.; Gallagher, D.; Morley, J.E. Sarcopenic obesity predicts instrumental activities of daily living disability in the elderly. Obes. Res. 2004, 12, 1995–2004. [Google Scholar] [CrossRef] [PubMed]
- Janssen, I.; Heymsfield, S.B.; Wang, Z.M.; Ross, R. Skeletal muscle mass and distribution in 468 men and women aged 18–88 yr. J. Appl. Physiol. (1985) 2000, 89, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Tournadre, A.; Vial, G.; Capel, F.; Soubrier, M.; Boirie, Y. Sarcopenia. Jt. Bone Spine 2019, 86, 309–314. [Google Scholar] [CrossRef]
- Vlietstra, L.; Hendrickx, W.; Waters, D.L. Exercise interventions in healthy older adults with sarcopenia: A systematic review and meta-analysis. Australas. J. Ageing 2018, 37, 169–183. [Google Scholar] [CrossRef]
- Kaplan-Lewis, E.; Aberg, J.A.; Lee, M. Aging with HIV in the ART era. Semin. Diagn. Pathol. 2017, 34, 384–397. [Google Scholar] [CrossRef]
- Avila-Funes, J.A.; Aguilar-Navarro, S.; Melano-Carranza, E. Frailty, an enigmatic and controversial concept in geriatrics. The biological perspective. Gac. Med. Mex. 2008, 144, 255–262. [Google Scholar]
- Guaraldi, G.; Orlando, G.; Zona, S.; Menozzi, M.; Carli, F.; Garlassi, E.; Berti, A.; Rossi, E.; Roverato, A.; Palella, F. Premature age-related comorbidities among HIV-infected persons compared with the general population. Clin. Infect. Dis. 2011, 53, 1120–1126. [Google Scholar] [CrossRef] [PubMed]
- Dhillon, R.J.; Hasni, S. Pathogenesis and Management of Sarcopenia. Clin. Geriatr. Med. 2017, 33, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Sereti, I.; Altfeld, M. Immune activation and HIV: An enduring relationship. Curr. Opin. HIV AIDS 2016, 11, 129–130. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, K.L.; Brown, T.T.; Margolick, J.B.; Erlandson, K.M. Geriatric syndromes: New frontiers in HIV and sarcopenia. AIDS 2017, 31, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Nasi, M.; De Biasi, S.; Gibellini, L.; Bianchini, E.; Pecorini, S.; Bacca, V.; Guaraldi, G.; Mussini, C.; Pinti, M. Ageing and inflammation in patients with HIV infection. Clin. Exp. Immunol. 2017, 187, 44–52. [Google Scholar] [CrossRef]
- Ryall, J.G.; Schertzer, J.D.; Lynch, G.S. Cellular and molecular mechanisms underlying age-related skeletal muscle wasting and weakness. Biogerontology 2008, 9, 213–228. [Google Scholar] [CrossRef]
- Lopez-Otin, C.; Blasco, M.A.; Partridge, L.; Serrano, M.; Kroemer, G. The hallmarks of aging. Cell 2013, 153, 1194–1217. [Google Scholar] [CrossRef]
- Pinto, M.; Moraes, C.T. Mechanisms linking mtDNA damage and aging. Free Radic. Biol. Med. 2015, 85, 250–258. [Google Scholar] [CrossRef]
- Kalinkovich, A.; Livshits, G. Sarcopenic obesity or obese sarcopenia: A cross talk between age-associated adipose tissue and skeletal muscle inflammation as a main mechanism of the pathogenesis. Ageing Res. Rev. 2017, 35, 200–221. [Google Scholar] [CrossRef]
- Bhanji, R.A.; Narayanan, P.; Allen, A.M.; Malhi, H.; Watt, K.D. Sarcopenia in hiding: The risk and consequence of underestimating muscle dysfunction in non-alcoholic steatohepatitis. Hepatology 2017, 66, 2055–2065. [Google Scholar] [CrossRef]
- Garcia, M.; Seelaender, M.; Sotiropoulos, A.; Coletti, D.; Lancha, A.H., Jr. Vitamin D, muscle recovery, sarcopenia, cachexia, and muscle atrophy. Nutrition 2019, 60, 66–69. [Google Scholar] [CrossRef] [PubMed]
- Steffl, M.; Bhannon, R.W.; Petr, M.; Kohlikova, E.; Holmerova, I. Relation between cigarette smoking and sarcopenia: Meta-analysis. Physiol. Res. 2015, 64, 419–426. [Google Scholar] [PubMed]
- Hsieh, E.; Yin, M.T. Continued Interest and Controversy: Vitamin D in HIV. Curr. HIV/AIDS Rep. 2018, 15, 199–211. [Google Scholar] [CrossRef] [PubMed]
- Erlandson, K.M.; Allshouse, A.A.; Jankowski, C.M.; MaWhinney, S.; Kohrt, W.M.; Campbell, T.B. Functional impairment is associated with low bone and muscle mass among persons aging with HIV infection. J. Acquir. Immune Defic. Syndr. 2013, 63, 209–215. [Google Scholar] [CrossRef]
- Frazier, E.L.; Sutton, M.Y.; Brooks, J.T.; Shouse, R.L.; Weiser, J. Trends in cigarette smoking among adults with HIV compared with the general adult population, United States—2009–2014. Prev. Med. 2018, 111, 231–234. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010, 39, 412–423. [Google Scholar] [CrossRef]
- Hawkins, K.L.; Zhang, L.; Ng, D.K.; Althoff, K.N.; Palella, F.J.J.; Kingsley, L.A.; Jacobson, L.P.; Margolick, J.B.; Lake, J.E.; Brown, T.T.; et al. Abdominal obesity, sarcopenia, and osteoporosis are associated with frailty in men living with and without HIV. AIDS 2018, 32, 1257–1266. [Google Scholar] [CrossRef]
- Erlandson, K.M.; Schrack, J.A.; Jankowski, C.M.; Brown, T.T.; Campbell, T.B. Functional impairment, disability, and frailty in adults aging with HIV-infection. Curr. HIV/AIDS Rep. 2014, 11, 279–290. [Google Scholar] [CrossRef]
- Vermeiren, S.; Vella-Azzopardi, R.; Beckwée, D.; Habbig, A.K.; Scafoglieri, A.; Jansen, B.; Bautmans, I.; Gerontopole Brussels Study Group. Frailty and the Prediction of Negative Health Outcomes: A Meta-Analysis. J. Am. Med. Dir. Assoc. 2016, 17, 1163.e1–1163.e17. [Google Scholar] [CrossRef]
- Natsag, J.; Erlandson, K.M.; Sellmeyer, D.E.; Haberlen, S.A.; Margolick, J.; Jacobson, L.P.; Palella, F.J., Jr.; Koletar, S.L.; Lake, J.E.; Post, W.S.; et al. HIV infection is associated with increased fatty infiltration of the thigh muscle with aging independent of fat distribution. PloS ONE 2017, 12, e0169184. [Google Scholar] [CrossRef]
- Grant, P.M.; Kitch, D.; McComsey, G.A.; Collier, A.C.; Bartali, B.; Koletar, S.L.; Erlandson, K.M.; Lake, J.E.; Yin, M.T.; Melbourne, K.; et al. Long-term body composition changes in antiretroviral-treated HIV-infected individuals. AIDS. 2016, 30, 2805–2813. [Google Scholar] [CrossRef] [PubMed]
- Pinto Neto, L.F.; Sales, M.C.; Scaramussa, E.S.; da Paz, C.J.; Morelato, R.L. Human immunodeficiency virus infection and its association with sarcopenia. Braz. J. Infect. Dis. 2016, 20, 99–102. [Google Scholar] [CrossRef] [PubMed]
- Aziz, S.A.A.; Megan, M.; Bashah, N.S.A.; Chong, M.L.; Sasheelaa, P.; Omar, S.F.S.; Sulaiman, H.; Azwa, I.; Tan, P.T.; Kamarulzaman, A.; et al. Assessment of sarcopenia in virally suppressed HIV-infected Asians receiving treatment. AIDS 2019, 33, 769. [Google Scholar] [CrossRef] [PubMed]
- Echeverría, P.; Bonjoch, A.; Puig, J.; Estany, C.; Ornelas, A.; Clotet, B.; Negredo, E. High Prevalence of Sarcopenia in HIV-Infected Individuals. Biomed. Res. Int. 2018, 12, 5074923. [Google Scholar] [CrossRef]
- Landi, F.; Marzetti, E.; Martone, A.M.; Bernabei, R.; Onder, G. Exercise as a remedy for sarcopenia. Curr. Opin. Clin. Nutr. Metab. Care. 2014, 17, 25–31. [Google Scholar] [CrossRef]
- Marzetti, E.; Calvani, R.; Tosato, M.; Cesari, M.; Di Bari, M.; Cherubini, A.; Broccatelli, M.; Savera, G.; D’Elia, M.; Pahor, M.; et al. SPRINTT Consortium. Physical activity and exercise as countermeasures to physical frailty and sarcopenia. Aging Clin. Exp. Res. 2017, 29, 35–42. [Google Scholar] [CrossRef]
- Onen, N.F.; Overton, E.T.; Seyfried, W.; Stumm, E.R.; Snell, M.; Mondy, K.; Tebas, P. Aging and HIV infection: A comparison between older HIV-infected persons and the general population. HIV Clin. Trials 2010, 11, 100–109. [Google Scholar] [CrossRef]
- Ross, R.; Blair, S.N.; Arena, R.; Church, T.S.; Després, J.P.; Franklin, B.A.; Haskell, W.L.; Kaminsky, L.A.; Levine, B.D.; Lavie, C.J.; et al. Importance of Assessing Cardiorespiratory Fitness in Clinical Practice: A Case for Fitness as a Clinical Vital Sign: A Scientific Statement From the American Heart Association. Circulation 2016, 13, e653–e699. [Google Scholar] [CrossRef]
- Roubenoff, R.; Weiss, L.; McDermott, A.; Heflin, T.; Cloutier, G.J.; Wood, M.; Gorbach, S. A pilot study of exercise training to reduce trunk fat in adults with HIV-associated fat redistribution. AIDS 1999, 13, 1373–1375. [Google Scholar] [CrossRef]
- Agin, D.; Gallagher, D.; Wang, J.; Heymsfield, S.B.; Pierson, R.N., Jr.; Kotler, D.P. Effects of whey protein and resistance exercise on body cell mass, muscle strength, and quality of life in women with HIV. AIDS 2001, 15, 2431–2440. [Google Scholar] [CrossRef]
- Yarasheski, K.E.; Tebas, P.; Stanerson, B.; Claxton, S.; Marin, D.; Bae, K.; Kennedy, M.; Tantisiriwat, W.; Powderly, W.G. Resistance exercise training reduces hypertriglyceridemia in HIV-infected men treated with antiviral therapy. J. Appl. Physiol. (1985) 2001, 90, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Roubenoff, R.; Abad, L.W.; Lundgren, N. Effect of acquired immune deficiency syndrome wasting on the protein metabolic response to acute exercise. Metabolism 2001, 50, 288–292. [Google Scholar] [CrossRef] [PubMed]
- Thöni, G.J.; Fedou, C.; Brun, J.F.; Fabre, J.; Renard, E.; Reynes, J.; Varray, A.; Mercier, J. Reduction of fat accumulation and lipid disorders by individualized light aerobic training in human immunodeficiency virus infected patients with lipodystrophy and/or dyslipidemia. Diabetes Metab. 2002, 28, 397–404. [Google Scholar] [PubMed]
- Driscoll, S.D.; Meininger, G.E.; Lareau, M.T.; Dolan, S.E.; Killilea, K.M.; Hadigan, C.M.; Lloyd-Jones, D.M.; Klibanski, A.; Frontera, W.R.; Grinspoon, S.K. Effects of exercise training and metformin on body composition and cardiovascular indices in HIV-infected patients. AIDS 2004, 18, 465–473. [Google Scholar] [CrossRef]
- Driscoll, S.D.; Meininger, G.E.; Ljungquist, K.; Hadigan, C.; Torriani, M.; Klibanski, A.; Frontera, W.R.; Grinspoon, S. Differential effects of metformin and exercise on muscle adiposity and metabolic indices in human immunodeficiency virus-infected patients. J. Clin. Endocrinol. Metab. 2004, 89, 2171–2178. [Google Scholar] [CrossRef]
- Engelson, E.S.; Agin, D.; Kenya, S.; Werber-Zion, G.; Luty, B.; Albu, J.B.; Kotler, D.P. Body composition and metabolic effects of a diet and exercise weight loss regimen on obese, HIV-infected women. Metabolism 2006, 2006 55, 1327–13236. [Google Scholar] [CrossRef]
- Terry, L.; Sprinz, E.; Stein, R.; Medeiros, N.B.; Oliveira, J.; Ribeiro, J.P. Exercise training in HIV-1-infected individuals with dyslipidemia and lipodystrophy. Med. Sci. Sports. Exerc. 2006, 38, 411–417. [Google Scholar] [CrossRef]
- Dolan, S.E.; Frontera, W.; Librizzi, J.; Ljungquist, K.; Juan, S.; Dorman, R.; Cole, M.E.; Kanter, J.R.; Grinspoon, S. Effects of a supervised home-based aerobic and progressive resistance training regimen in women infected with human immunodeficiency virus: A randomized trial. Arch. Intern. Med. 2006, 166, 1225–1231. [Google Scholar] [CrossRef]
- Robinson, F.P.; Quinn, L.T.; Rimmer, J.H. Effects of high-intensity endurance and resistance exercise on HIV metabolic abnormalities: A pilot study. Biol. Res. Nurs. 2007, 8, 177–185. [Google Scholar] [CrossRef]
- Hand, G.A.; Phillips, K.D.; Dudgeon, W.D.; William Lyerly, G.; Larry Durstine, J.; Burgess, S.E. Moderate intensity exercise training reverses functional aerobic impairment in HIV-infected individuals. AIDS Care 2008, 20, 1066–1074. [Google Scholar] [CrossRef]
- Lindegaard, B.; Hansen, T.; Hvid, T.; van Hall, G.; Plomgaard, P.; Ditlevsen, S.; Gerstoft, J.; Pedersen, B.K. The effect of strength and endurance training on insulin sensitivity and fat distribution in human immunodeficiency virus-infected patients with lipodystrophy. J. Clin. Endocrinol. Metab. 2008, 93, 3860–3869. [Google Scholar] [CrossRef] [PubMed]
- Farinatti, P.T.; Borges, J.P.; Gomes, R.D.; Lima, D.; Fleck, S.J. Effects of a supervised exercise program on the physical fitness and immunological function of HIV-infected patients. J. Sports Med. Phys. Fit. 2010, 50, 511–518. [Google Scholar]
- Souza, P.M.; Jacob-Filho, W.; Santarém, J.M.; Zomignan, A.A.; Burattini, M.N. Effect of progressive resistance exercise on strength evolution of elderly patients living with HIV compared to healthy controls. Clinics 2011, 66, 261–266. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dudgeon, W.D.; Jaggers, J.R.; Phillips, K.D.; Durstine, J.L.; Burgess, S.E.; Lyerly, G.W.; Davis, J.M.; Hand, G.A. Moderate-Intensity Exercise Improves Body Composition and Improves Physiological Markers of Stress in HIV-Infected Men. ISRN AIDS 2012, 11, 145127. [Google Scholar] [CrossRef] [PubMed]
- Broholm, C.; Mathur, N.; Hvid, T.; Grøndahl, T.S.; Frøsig, C.; Pedersen, B.K.; Lindegaard, B. Insulin signaling in skeletal muscle of HIV-infected patients in response to endurance and strength training. Physiol. Rep. 2013, 1, e00060. [Google Scholar] [CrossRef] [PubMed]
- Ezema, C.I.; Onwunali, A.A.; Lamina, S.; Ezugwu, U.A.; Amaeze, A.A.; Nwankwo, M.J. Effect of aerobic exercise training on cardiovascular parameters and CD4 cell count of people living with human immunodeficiency virus/acquired immune deficiency syndrome: A randomized controlled trial. Niger. J. Clin. Pract. 2014, 7, 543–548. [Google Scholar]
- Ahmad, B.; Glufke, K.; Grau, M.; Sandig, D.; Rockstroh, J.; Vogel, M.; Wasmuth, J.C.; Bloch, W.; Brixius, K. Influence of endurance training and marathon running on red cell deformability in HIV patients. Clin. Hemorheol. Microcirc. 2014, 57, 355–366. [Google Scholar] [CrossRef]
- Garcia, A.; Fraga, G.A.; Vieira, R.C., Jr.; Silva, C.M.; Trombeta, J.C.; Navalta, J.W.; Prestes, J.; Voltarelli, F.A. Effects of combined exercise training on immunological, physical and biochemical parameters in individuals with HIV/AIDS. J. Sports. Sci. 2014, 32, 785–792. [Google Scholar] [CrossRef]
- Zanetti, H.R.; da Cruz, L.G.; Lourenço, C.L.; Neves, F.F.; Silva-Vergara, M.L.; Mendes, E.L. Does nonlinear resistance training reduce metabolic syndrome in people living with HIV? A randomized clinical trial. J. Sports Med. Phys. Fit. 2017, 57, 678–684. [Google Scholar]
- Bonato, M.; Galli, L.; Passeri, L.; Longo, V.; Pavei, G.; Bossolasco, S.; Bertocchi, C.; Cernuschi, M.; Balconi, G.; Merati, G.; et al. A pilot study of brisk walking in sedentary combination antiretroviral treatement (cART)- treated patients: Benefit on soluble and cell inflammatory markers. BMC Infect. Dis. 2017, 17, 61. [Google Scholar] [CrossRef]
- Pedro, R.E.; Candido, N.; Guariglia, D.A.; Melo, B.P.; Bertolini, D.A.; Peres, S.B.; Franzói de Moraes, S.M. Exercise improves cytokine profile in HIV-infected people: A randomized clinical trial. Cytokine 2017, 99, 18–23. [Google Scholar] [CrossRef]
- Zanetti, H.R.; Cruz, L.G.; Lourenço, C.L.; Neves Fde, F.; Silva-Vergara, M.L.; Mendes, E.L. Non-linear resistance training reduces inflammatory biomarkers in persons living with HIV: A randomized controlled trial. Eur. J. Sport. Sci. 2016, 16, 1232–1239. [Google Scholar] [CrossRef]
- Oursler, K.K.; Sorkin, J.D.; Ryan, A.S.; Katzel, L.I. A pilot randomized aerobic exercise trial in older HIV-infected men: Insights into strategies for successful aging with HIV. PLoS ONE 2018, 13, e0198855. [Google Scholar] [CrossRef] [PubMed]
- Vingren, J.L.; Curtis, J.H.; Levitt, D.E.; Duplanty, A.A.; Lee, E.C.; McFarlin, B.K.; Hill, D.W. Adding Resistance Training to the Standard of Care for Inpatient Substance Abuse Treatment in Men with Human Immunodeficiency Virus Improves Skeletal Muscle Health Without Altering Cytokine Concentrations. J. Strength Cond. Res. 2018, 32, 76–82. [Google Scholar] [CrossRef] [PubMed]
- De Brito-Neto, J.G.; de Andrade, M.F.; de Almeida, V.D.; Paiva, D.C.C.; de Morais, N.M.; Bezerra, C.M.; Fernandes, J.V.; do Nascimento, E.G.C.; Fonseca, I.A.T.; de Medeiros Fernandes, T.A.A. Strength training improves body composition, muscle strength and increases CD4+ T lymphocyte levels in people living with HIV/AIDS. Infect. Dis. Rep. 2019, 11, 7925. [Google Scholar] [CrossRef] [PubMed]
- Zanetti, H.R.; Gonçalves, A.; Paranhos Lopes, L.T.; Mendes, E.L.; Roever, L.; Silva-Vergara, M.L.; Neves, F.F.; Resende, E.S. Effects of exercise training and statin use in people living with HIV with dyslipidemia. Med. Sci. Sports Exerc. 2019. [Google Scholar] [CrossRef]
- Bonato, M.; Turrini, F.; De Zan, V.; Meloni, A.; Plebani, M.; Brambilla, E.; Giordani, A.; Vitobello, C.; Caccia, R.; Piacentini, M.F.; et al. A Mobile Application for Exercise Intervention in People Living with HIV. Med. Sci. Sports Exerc. 2019, 52, 425–433. [Google Scholar] [CrossRef]
| Author | Participants | Age | Intervention | Outcomes | ||
|---|---|---|---|---|---|---|
| Physical Fitness | Body Composition | Inflammatory Markers | ||||
| Roubenoff et al. [39] | 10 subjects with lipodystrophy | 39.2 (23–56) Mean (range) | Duration 16 weeks Frequency: 3 sessions/week Exercise combined - Endurance: 20 min bike - Resistance: 1 h at 80% 1 RM | ↑Leg press; ↑Leg extension; ↑Chest press. | ↓Total Body fat; ↓Trunk fat | n.a. |
| Agin et al. [40] | 37 women allocated in: 12 protein supplementations 12 progressive resistance training 12 combined treatment | 40.8 (29–55) Mean (range) | Duration: 14 weeks Frequency: 3 sessions/week Exercise: - Resistance: 3 × 8/10 at 75% 1RM | Protein supplementation ↑Bench press; ↑Shoulder press; ↑Biceps curl; ↑Triceps extension; ↑Leg extension. Resistance training ↑Bench press; ↑Seated back row; ↑Shoulder press; ↑Biceps curl; ↑Triceps extension; ↑Leg extension; ↑Leg curl Combined treatment ↑Bench press; ↑Seated row; ↑Shoulder press; ↑Biceps curl; ↑Leg extension; ↑Leg curl. | Protein supplementation ↑Body weight; ↑Fat mass; ↑Fat free mass Resistance training ↓Body cell mass; ↑Skeletal muscle; ↓Fat mass; ↓Fat free mass. Combined treatment ↓Body cell mass; ↑Fat free mass | n.a. |
| Yarasheski et al. [41] | 18 subjects with hypertriglyceridemia | 42 ± 2 Mean ± SD | Duration: 16 weeks Frequency: 4 sessions/week Exercise: - Resistance: 3 × 5/8 at 75/85% 1 RM | ↑in muscle strength. | ↑Body weight; ↑Lean mass; ↓Fat mass; ↓Thigh muscle area | n.a. |
| Roubenoff et al. [42] | 10 HIV-seropositive wasted 12 HIV-seropositive nonwasted | 38.9 (30–53) Mean (range) | Duration: 8 weeks Frequency: 3 sessions/week Exercise: - Resistance: 3 × 8 from 50% to 80% 1RM | HIV wasting syndrome ↑Chest press; ↑Leg press; ↑Leg extension; ↑Upper back. No HIV wasting syndrome ↑Chest press; ↑Leg press; ↑Leg extension; ↑Upper back. | HIV wasting syndrome ↑Fat free mass No HIV wasting syndrome ↑Fat free mass | n.a. |
| Thöni et al. [43] | 17 subjects with lipodystrophy and 2 with dyslipidaemia | 44.2 ± 2.3 Mean ± SD | Duration: 16 weeks Frequency: 2 sessions/week Exercise: Endurance: cycling 45 min at VT | ↑O2max | ↓Abdominal adipose tissue; ↓Visceral adipose tissue | n.a. |
| Driscoll et al. [44,45] | 37 subjects with hyperinsulinemia and fat redistribution allocated in: 19 metformin and exercise 18 metformin only | 42 (35–27) Median (IQR) | Duration: 12 weeks Frequency: 2 sessions/week Exercise: combined - Endurance: 20/30 min cycling at 60%–75% HRmax - Resistance: 3 × 10 at 60%–80% 1RM | Metformin and exercise ↑Exercise time | Metformin and exercise ↓Waist-to-hip ratio; ↓Abdominal subcutaneous fat; ↑Thigh muscle area. | n.a. |
| Engelson et al. [46] | 39 obese women | 41.8 ± 7.5 Mean ± SD | Duration: 12 weeks Frequency: 3 sessions/week Exercise: combined - Endurance: 30 min running at 70%–80% HRmax - Resistance: 3 × 8/10 at 70% 1RM | ↑Pectoral; ↑Latissimus dorsi; ↑Quadriceps; ↑Time to fatigue. | ↓Body mass; ↓BMI; ↓Waist circumference; ↓Chest circumference; ↓Biceps skinfold; ↓Abdominal skinfold; ↓Thigh skinfold; ↑Skeletal muscle; ↓Visceral adipose tissue; ↓Subcutaneous adipose tissue; ↓Total adipose tissue; ↓Fat mass | n.a. |
| Terry et al. [47] | 42 subjects with dyslipidaemia and lipodystrophy allocated in: 21 diet and exercise group 21 diet group | 36 ± 6 Mean ± SD | Duration: 12 weeks Frequency: 3 sessions/week Exercise: - Endurance: 30 min running at 70%–85% HRmax | Exercise and diet ↑O2max | In both groups ↓Body mass; ↓BMI; ↓Waist-to-hip ratio; ↓Body fat | n.a. |
| Dolan et al. [48] | 40 women with fat redistribution allocated in: 20 exercise group 20 control group | 42 ± 2 Mean ± SEM | Duration: 16 weeks Frequency: 3 sessions/week Exercise: combined - Endurance: 20/30 min cycling at 60%–75% HRmax - Resistance: 3/4 × 8/10 at 60%–80% 1RM | Exercise ↑O2max; ↑Time to exercise; ↑Strength; ↑6MWT; ↑Knee extensor; ↑Knee flexor; ↑Pectoralis; Shoulder abductors; ↑Ankle plantar flexor; ↑Elbow flexors | Exercise ↓Waist circumference; ↓Total muscle area | n.a. |
| Robinson et al. [49] | 9 subjects with HIV metabolic abnormalities | 44.0 ± 3.8 Mean ± SD | Duration: 16 weeks Frequency: 3 sessions/week Exercise: combined - Endurance: 20 min bike at 70%–80% O2max - Resistance: 1 × 10 at 60%–80% 1RM | ↑1RM in all strength exercises | ↓Trunk fat | n.a. |
| Hand et al. [50] | 74 subjects allocated in: 44 exercise group 30 control group | 41.8 ± 3.7 Mean ± SD | Duration: 6 weeks Frequency: 3 sessions/week Exercise: combined - Endurance: 30 min at 50%–70% O2max - Resistance: 20 min at 60% 3RM | Exercise training ↑Time to fatigue; ↑Estimated O2max; ↓Functional aerobic impairment; ↑HRpeak during exercise; ↓Submaximal exercise | n.a. | n.a. |
| Lindegaard et al. [51] | 20 men with lipodystrophy allocated in: 10 endurance group 10 strength group | 49.5 ± 8.2 Mean ± SD | Duration:16 weeks Frequency: 3 sessions/week Exercise: - Endurance: 35 min at 65%–75% O2max - Resistance: 3 × 8 at 50%–80% 3RM | Endurance training ↑O2max; ↑3RM Strength training ↑3RM | Strength training ↓Body mass; ↑Total lean mass; ↓Total fat mass; ↓Trunk fat mass; ↓Limb fat mass | Endurance training ↓hsCRP; ↓TNF-α; ↓IL6; ↓IL18 Strength training ↓IL18; ↔hsCRP; ↔TNF-α; ↔IL6. |
| Farinatti et al. [52] | 27 subjects allocated in: 19 experimental group 8 control group | 44 ± 4 Mean ± SD | Duration: 12 weeks Frequency: 3 sessions/week Exercise: combined - Endurance: 30 min at 150 bpm - Resistance: 3 × 12 at 60–80 12RM - Flexibility: 3 × 30 s | Exercise training ↑Flexibility; ↑Leg press; ↑Seated row; ↓HR during exercise | Exercise training ↔ Body Mass; BMI | n.a. |
| Souza et al. [53] | 26 women subjects allocated in: 11 living with HIV 21 controls | 65.65 ± 3.06 Mean ± SD | Duration: 48 weeks Frequency: 2 sessions/week Exercise: - Resistance: 3 × 8/12 | Exercise with HIV ↓Sit standing; ↑2.4 miles walking; ↑Leg press; ↑Chest press; ↑Lumbar extension; ↑Seated row; ↑Seated abdominal. | Exercise with HIV ↔ Body Mass; BMI | n.a. |
| Dudgeon et al. [54] | 111 men allocated in: 59 exercise group 59 control group | 44.9 ± 1.4 Mean ± SD | Duration: 6 weeks Frequency: 2 sessions/week Exercise: combined - Endurance: 30 min at 60%–75% HRmax - Resistance: 3 × 12 circuit training | n.a. | Exercise ↑Total lean mass ↔ Body mass; ↔ BMI; ↔ Total body fat; %Trunk fat; ↔ Arm fat; ↔ Leg fat; ↔ Arm/leg/trunk lean mass | Exercise ↓Salivary cortisol; ↔ IL6; ↔ IL1; ↔ sTNFrII; ↔ IGF1; ↔ IGFBP3; ↔ GH; ↔ Salivary testosterone |
| Broholom et al. [55] | 20 subjects with lipodystrophy allocated in: 10 endurance group 10 strength group | 49.5 ± 10.3 Mean ± SD | Duration: 16 weeks Frequency: 3 sessions/week Exercise: - Endurance: 35 min interval training - Resistance: 3 × 8/10 rep at 50–80 3 RM | Endurance ↑O2max; ↑3RM Strength ↑3RM | n.a. | |
| Ezema et al. [56] | 33 subjects allocated in: 17 exercise 16 control | 36.27 ± 10.06 Mean ± SD | Duration: 8 weeks Frequency: 3 sessions/week Exercise: - Endurance: 45–60 min at 60%–79% HRmax | Exercise ↑O2max | Exercise ↔ BMI | |
| Ahmad et al. [57] | 8 subjects | 38 ± 9 Mean ± SD | Individual marathon running plan | ↑Maximal running velocity; ↑VT | ↔ BMI | |
| Garcia et al. [58] | 10 subjects | 44.7 ± 8.9 Mean ± SD | Duration: 20 weeks Frequency: 3 sessions/week Duration: combined - Endurance: 30 min at 60%–75% O2max - Resistance: circuit training | n.a. | ↑Lean mass; ↔ Body mass; ↔ BMI; ↔ Fat mass; | |
| Zanetti et al. [59] | 30 subjects allocated in 15 non-linear resistance training 15 control | 42.4 ± 10.5 Mean ± SD | Duration: 12 weeks Frequency: 3 times/week Exercise: - Resistance: 3/4 sets from 4 to 20 reps | Non-linear resistance training ↑Squat; ↑Bench press; ↑Hamstring curls; ↑Frontal pull; ↑Seated calf raise; ↑Shoulder press | Non-linear resistance training ↓Central subcutaneous fat; ↓Peripheral subcutaneous fat; ↓Total subcutaneous fat; ↓Neck circumference; ↓Abdomen circumference; ↓Waist circumference; ↓Waist-to-hip ratio | Non-linear resistance training ↓IL-1β; ↓IL6; ↓IL8; ↓IL10; ↓TNF-α |
| Bonato et al. [60] | 49 subjects allocated in: 29 walk 20 strength-walk | 48 (44–54) Median (IQR) | Duration: 12 weeks Frequency: 3 sessions/week Duration: combined - Endurance: 60 min at 65%–75% HRmax - Resistance: 3 × 12 circuit training | Walk ↑6MWT Strength-walk ↑6MWT; ↑1RM strength in all circuit training exercises | Walk ↓Body mass; ↓Body mass index | Walk ↓CRP; ↓IL6; ↓D-dimer Strength-walk ↓CRP |
| Pedro et al. [61] | 28 subjects allocated in: 11 training group 17 control group | 45.1 ± 7.7 Mean ± SD | Duration: 16 weeks Frequency: 3 sessions/week Exercise: combined - Endurance: 20 min at 50%–70% HRR - Resistance: 2/3 sets × 8/12 rep | Concurrent training ↑Leg press; ↑Bench press | n.a. | Concurrent training ↓IL8 |
| Zanetti et al. [62] | 21 subjects with metabolic syndrome allocated in: 10 non-linear resistance training 11 control | 41.1 ± 10.1 Mean ± SD | Duration: 12 weeks Frequency: 3 times/week Exercise: - Resistance: 3/4 sets from 4 to 20 reps | n.a. | Non-linear resistance training ↓Fat mass; ↑Lean mass; ↓Waist circumference; | n.a. |
| Oursler et al. [63] | 22 subjects allocated in: 11 moderate-intensity 11 high-intensity | 57.4 ± 9.5 Mean ± SD | Duration: 16 weeks Frequency: 3 sessions/week Exercise: endurance - Moderate-intensity training: 45 min self-paced walking - high-intensity training: 45 min at 75%–90% HRR. | Moderate-intensity training ↑Time on treadmill; ↑6MWT High-intensity training ↑O2peak; ↑Time on treadmill; ↑6MWT | Moderate-intensity training ↔ Body mass; ↔ Lean Mass; ↔ Fat mass; ↔ Body fat percent; ↔ Visceral fat area; ↔ Subcutaneous fat area High-intensity training ↔ Body mass; ↔ Lean Mass; ↔ Fat mass; ↔ Body fat percent; ↔ Visceral fat area; ↔ Subcutaneous fat area | n.a. |
| Vingren et al. [64] | 16 men with substance abuse treatment 8 resistance training 8 control | 42 ± 11 Mean ± SD | Duration: 6 weeks Frequency: 3 sessions/week Exercise: - Resistance: 3/5 × 5/12 reps | Resistance training group ↑1RM strength at bench press; ↑Iso squat peak; ↑Vertical power | Resistance training group ↑Muscle mass; ↑Upper-arm circumference; ↑Forearm circumference | Resistance training group ↔ IFN, ↔ IL1β, ↔ IL2, ↔ IL4, ↔ IL6, ↔ IL10, ↔ TNF-α |
| De Brito-Neto et al. [65] | 19 subjects allocated in 9 exercise group 10 control group | 39.16 ± 5.11 Mean ± SD | Duration: 12 weeks Frequency: 2 sessions/week Exercise: - Resistance: 3 × 18/10 reps at subjective perception of effort | Exercise group ↓Bench press; ↓Lat pulldown; ↓Triceps pulley; ↓Elbow flexion; ↓Squat; ↓Leg press; ↓Knee flexion; ↓Ankle extension. | Exercise group ↓Body fat; ↑Lean body mass | n.a. |
| Zanetti et al. [66] | 82 subjects allocated in: 21 placebo 21 statins 21 placebo + exercise training 20 statins + exercise training | 41.9 ± 10.4 Mean ± SD | Duration: 12 weeks Frequency: 3 sessions/week Exercise: - Endurance: periodized polarized training - Resistance: periodized nonlinear resistance training | Placebo + exercise training ↑O2max; ↑Bench press; ↑Hamstring curl; ↑Frontal pull; ↑Seated calf raise; ↑Shoulder press Statins + exercise training ↑O2max; ↑Bench press; ↑Hamstring curl; ↑Frontal pull; ↑Seated calf raise; ↑Shoulder press | Placebo + exercise training ↑Lean body mass; ↓Fat mass Statins + exercise training ↑Lean body mass; ↓Fat mass | Statins ↓IL-1β; ↓IL6; ↓hsCRP; ↓FIBR; Placebo + exercise training ↓IL-1β; ↓IL6; ↓IL10; ↓CRP; ↓FIBR; Statins + exercise training ↓IL1β; ↓IL6; ↓IL8; ↓IL10; ↓CRP; ↓FIBR; |
| Bonato et al. [67] | 38 subjects allocated in: 20 APP 18 No-APP | 51 (44–54) Median (IQR) | Duration: 16 weeks Frequency: 3 sessions/week Exercise: - Endurance: 60 min at 65%–75% HRmax | APP ↑O2peak | APP ↓Fat mass; ↑Fat free mass | n.a. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bonato, M.; Turrini, F.; Galli, L.; Banfi, G.; Cinque, P. The Role of Physical Activity for the Management of Sarcopenia in People Living with HIV. Int. J. Environ. Res. Public Health 2020, 17, 1283. https://doi.org/10.3390/ijerph17041283
Bonato M, Turrini F, Galli L, Banfi G, Cinque P. The Role of Physical Activity for the Management of Sarcopenia in People Living with HIV. International Journal of Environmental Research and Public Health. 2020; 17(4):1283. https://doi.org/10.3390/ijerph17041283
Chicago/Turabian StyleBonato, Matteo, Filippo Turrini, Laura Galli, Giuseppe Banfi, and Paola Cinque. 2020. "The Role of Physical Activity for the Management of Sarcopenia in People Living with HIV" International Journal of Environmental Research and Public Health 17, no. 4: 1283. https://doi.org/10.3390/ijerph17041283
APA StyleBonato, M., Turrini, F., Galli, L., Banfi, G., & Cinque, P. (2020). The Role of Physical Activity for the Management of Sarcopenia in People Living with HIV. International Journal of Environmental Research and Public Health, 17(4), 1283. https://doi.org/10.3390/ijerph17041283







