Primary Health Care for Aboriginal Australian Women in Remote Communities after a Pregnancy with Hyperglycaemia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Outcome Measures
2.4. Outcome Variable Definitions
2.5. Statistical Analysis
3. Results
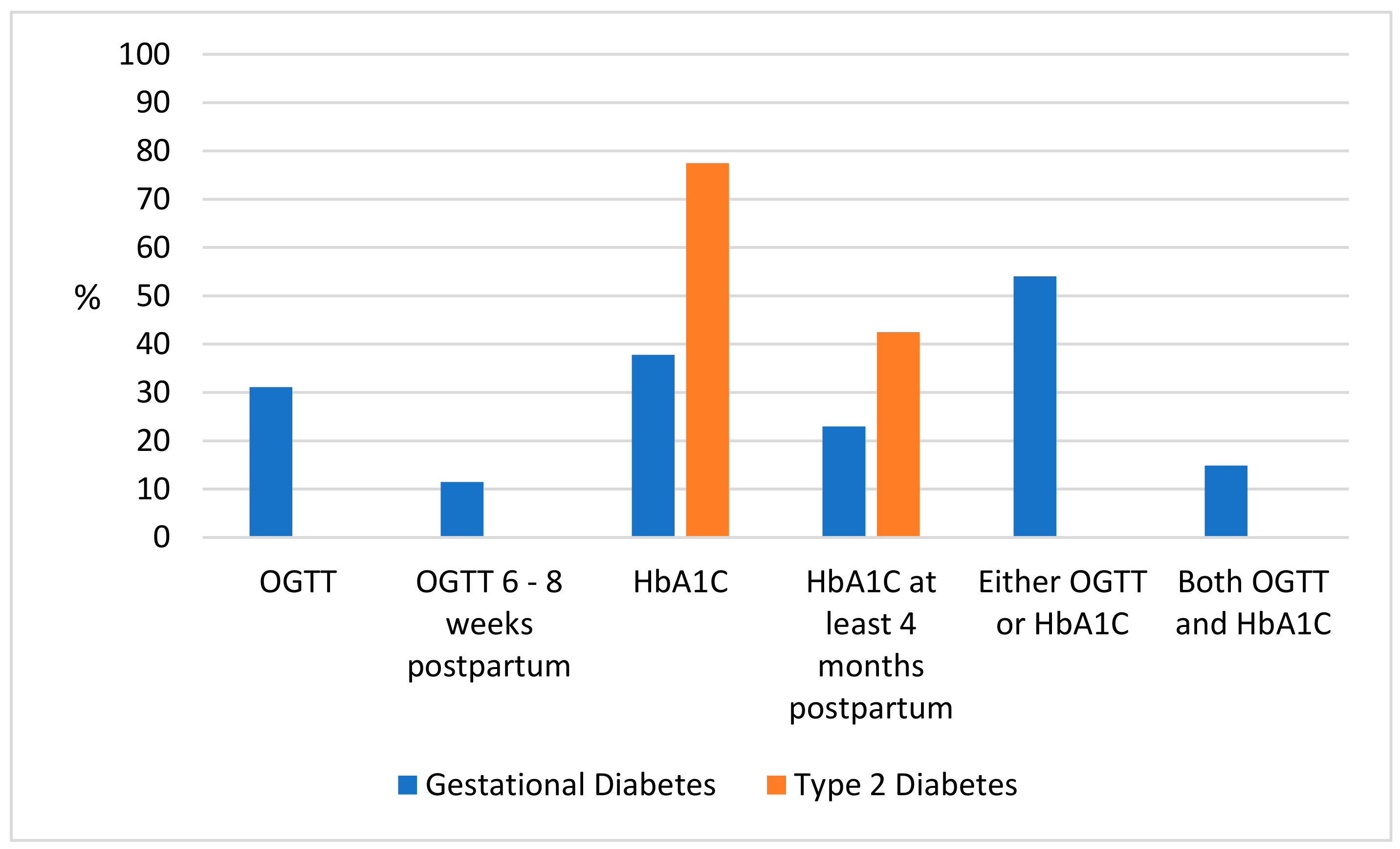
3.1. Postpartum Glycaemic Checks
3.2. Completion of Six-Week Postpartum Check-Up and Health Care Provided within 12 Months Postpartum
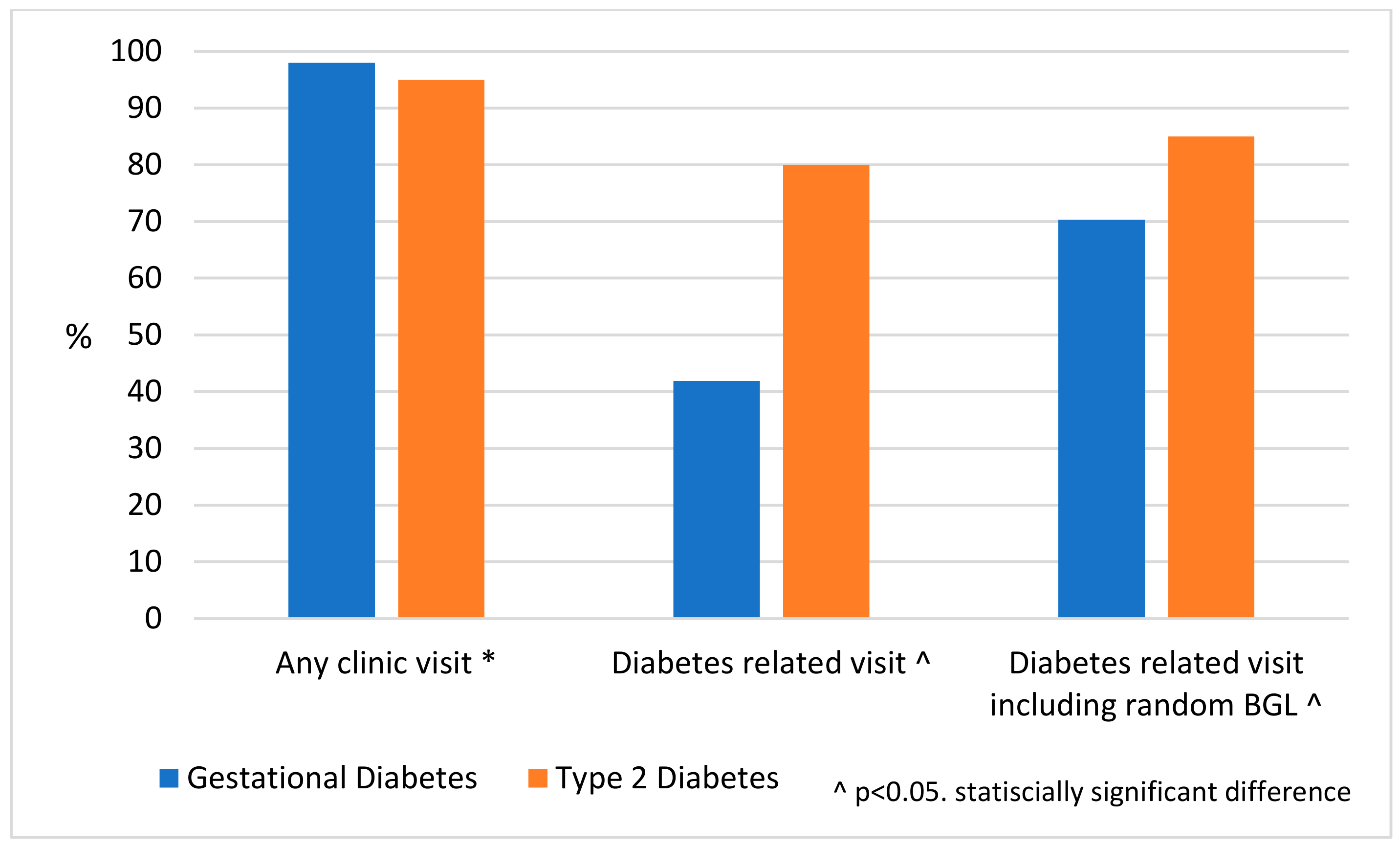
3.3. Visits to Primary Health Centre and Reasons for Visit
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Huffman, M.D.; Galloway, J.M. Cardiovascular health in indigenous communities: Successful programs. Heart Lung Circ. 2010, 19, 351–360. [Google Scholar] [CrossRef]
- World Health Organisation. Obesity and Overweight Fact Sheet Updated February 2019. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 5 November 2019).
- Australian Institute of Health and Welfare. Diabetes in Pregnancy: Its Impact on Australian Women and Their Babies Diabetes Series No. 14. Cat. No. CVD 52. Available online: https://www.aihw.gov.au/getmedia/78c504d6-9b6b-40dc-bf3b-9356f5502409/11837.pdf.aspx?inline=true (accessed on 5 May 2019).
- Osgood, N.D.; Dyck, R.F.; Grassmann, W.K. The inter- and intragenerational impact of gestational diabetes on the epidemic of type 2 diabetes. Am. J. Public Health 2011, 101, 173–179. [Google Scholar] [CrossRef]
- Gluckman, P.D.; Hanson, M.A.; Cooper, C.; Thornburg, K.L. Effect of in utero and early-life conditions on adult health and disease. N. Engl. J. Med. 2008, 359, 61–73. [Google Scholar] [CrossRef]
- Bellamy, L.; Casas, J.P.; Hingorani, A.D.; Williams, D. Type 2 diabetes mellitus after gestational diabetes: A systematic review and meta-analysis. Lancet 2009, 373, 1773–1779. [Google Scholar] [CrossRef]
- Shen, G.X.; Shafer, L.A.; Martens, P.J.; Sellers, E.; Torshizi, A.A.; Ludwig, S.; Phillips-Beck, W.; Heaman, M.; Prior, H.J.; McGavock, J.; et al. Does First Nations ancestry modify the association between gestational diabetes and subsequent diabetes: A historical prospective cohort study among women in Manitoba, Canada. Diabet. Med. J. Br. Diabet. Assoc. 2016, 33, 1245–1252. [Google Scholar] [CrossRef] [PubMed]
- Steinhart, J.R.; Sugarman, J.R.; Connell, F.A. Gestational diabetes is a herald of NIDDM in Navajo women. High rate of abnormal glucose tolerance after GDM. Diabetes Care 1997, 20, 943–947. [Google Scholar] [CrossRef] [PubMed]
- Aljohani, N.; Rempel, B.M.; Ludwig, S.; Morris, M.; McQuillen, K.; Cheang, M.; Murray, R.; Shen, G.X. Gestational diabetes in Manitoba during a twenty-year period. Clin. Invest. Med. 2008, 31, E131–E137. [Google Scholar] [CrossRef] [PubMed]
- Dyck, R.; Klomp, H.; Tan, L.K.; Turnell, R.W.; Boctor, M.A. A comparison of rates, risk factors, and outcomes of gestational diabetes between aboriginal and non-aboriginal women in the Saskatoon health district. Diabetes Care 2002, 25, 487–493. [Google Scholar] [CrossRef] [PubMed]
- Chamberlain, C.R.; Oldenburg, B.; Wilson, A.N.; Eades, S.J.; O’Dea, K.; Oats, J.J.; Wolfe, R. Type 2 diabetes after gestational diabetes: Greater than fourfold risk among Indigenous compared with non-Indigenous Australian women. Diabetes Metab. Res. Rev. 2016, 32, 217–227. [Google Scholar] [CrossRef]
- Edwards, L.; Connors, C.; Whitbread, C.; Brown, A.; Oats, J.; Maple-Brown, L. Improving health service delivery for women with diabetes in pregnancy in remote Australia: Survey of care in the Northern Territory Diabetes in Pregnancy Partnership. Aust. N. Z. J. Obstet. Gynaecol. 2014, 54, 534–540. [Google Scholar] [CrossRef]
- Klein, J.; Boyle, J.A.; Kirkham, R.; Connors, C.; Whitbread, C.; Oats, J.; Barzi, F.; McIntyre, D.; Lee, I.; Luey, M.; et al. Preconception care for women with type 2 diabetes mellitus: A mixed-methods study of provider knowledge and practice. Diabetes Res. Clin. Pract. 2017, 129, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Mathieu, I.P.; Song, Y.; Jagasia, S.M. Disparities in postpartum follow-up in women with gestational diabetes mellitus. Clin. Diabetes 2014, 32, 178–182. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. Standards of medical care in diabetes—2011. Diabetes Care 2011, 34 (Suppl. 1), S11–S61. [Google Scholar] [CrossRef]
- Keely, E. An opportunity not to be missed—How do we improve postpartum screening rates for women with gestational diabetes? Diabetes Metab. Res. Rev. 2012, 28, 312–316. [Google Scholar] [CrossRef] [PubMed]
- Morrison, M.K.; Collins, C.E.; Lowe, J.M. Postnatal testing for diabetes in Australian women following gestational diabetes mellitus. Aust. N. Z. J. Obstet. Gynaecol. 2009, 49, 494–498. [Google Scholar] [CrossRef] [PubMed]
- Chamberlain, C.; McLean, A.; Oats, J.; Oldenburg, B.; Eades, S.; Sinha, A.; Wolfe, R. Low rates of postpartum glucose screening among indigenous and non-indigenous women in Australia with gestational diabetes. Matern. Child Health J. 2015, 19, 651–663. [Google Scholar] [CrossRef] [PubMed]
- McGrath, N.M.; Baldwin, A. Further post-partum follow-up of women with gestational diabetes mellitus from Northland, New Zealand. Diabet. Med. J. Br. Diabet. Assoc. 2012, 29, 415. [Google Scholar] [CrossRef]
- Barclay, L.; Kruske, S.; Bar-Zeev, S.; Steenkamp, M.; Josif, C.; Narjic, C.W.; Wardaguga, M.; Belton, S.; Gao, Y.; Dunbar, T.; et al. Improving Aboriginal maternal and infant health services in the ‘Top End’ of Australia; synthesis of the findings of a health services research program aimed at engaging stakeholders, developing research capacity and embedding change. BMC Health Serv. Res. 2014, 14, 241. [Google Scholar] [CrossRef]
- Kirkham, R. Diabetes care in remote Australia: The antental, postpartum and inter-pregnancy period. BMC Pregnancy Childbirth 2019, 19, 389. [Google Scholar] [CrossRef]
- Morrison, M.K.; Lowe, J.M.; Collins, C.E. Perceived risk of Type 2 diabetes in Australian women with a recent history of gestational diabetes mellitus. Diabet. Med. 2010, 27, 882–886. [Google Scholar] [CrossRef]
- Campbell, S.; Roux, N.; Preece, C.; Rafter, E.; Davis, B.; Mein, J.; Boyle, J.; Fredericks, B.; Chamberlain, C. Paths to improving care of Australian Aboriginal and Torres Strait Islander women following gestational diabetes. Prim. Health Care Res. Dev. 2017, 18, 549–562. [Google Scholar] [CrossRef]
- Van Ryswyk, E.; Middleton, P.; Shute, E.; Hague, W.; Crowther, C. Women’s views and knowledge regarding healthcare seeking for gestational diabetes in the postpartum period: A systematic review of qualitative/survey studies. Diabetes Res. Clin. Pract. 2015, 110, 109–122. [Google Scholar] [CrossRef] [PubMed]
- Bailie, R.; Si, D.; Dowden, M.; O’Donoghue, L.; Connors, C.; Robinson, G.; Cunningham, J.; Weeramanthri, T. Improving organisational systems for diabetes care in Australian Indigenous communities. BMC Health Serv. Res. 2007, 7, 67. [Google Scholar] [CrossRef] [PubMed]
- Australian Institute of Health and Welfare. Spatial Variation in Aboriginal and Torres Strait Islander People’s Access to Primary Health Care; Australian Institute of Health and Welfare: Canberra, Australia, 2017. [Google Scholar]
- Australian Bureau of Statistics. Estimates of Aboriginal and Torres Strait Islander Australians. June 2016. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/mf/3238.0.55.001 (accessed on 5 November 2019).
- Remote Primary Health Care Manuals. Women’s Business Manual, 6th ed.; Centre for Remote Health: Alice Springs, Australia, 2017. [Google Scholar]
- Remote Primary Health Care Manuals. Women’s Business Manual, 4th ed.; Congress Alukura and Nganampa Health Council Inc.: Alice Springs, Australia, 2008. [Google Scholar]
- Remote Primary Health Care Manuals. CARPA Standard Treatment Manual, 5th ed.; Centre for Remote Health: Alice Springs, Australia, 2009. [Google Scholar]
- Diabetes Care. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2018. Diabetes Care 2018, 41, S13–S27. [Google Scholar] [CrossRef]
- American Diabetes Association. Management of Diabetes in Pregnancy: Standards of Medical Care in Diabetes-2018. Diabetes Care 2018, 41, S137–S143. [Google Scholar] [CrossRef] [PubMed]
- Australian Institute of Health and Welfare. Diabetes in Pregnancy 2014–2015. Bulletin 146. Available online: https://www.aihw.gov.au/reports/diabetes/diabetes-in-pregnancy-2014-2015 (accessed on 10 December 2019).
- Carson, M.P.; Frank, M.I.; Keely, E. Original research: Postpartum testing rates among women with a history of gestational diabetes—Systematic review. Prim. Care Diabetes 2013, 7, 177–186. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, A.; Peng, T.; Kim, C. Trends in postpartum diabetes screening and subsequent diabetes and impaired fasting glucose among women with histories of gestational diabetes mellitus: A report from the Translating Research Into Action for Diabetes (TRIAD) Study. Diabetes Care 2009, 32, 269–274. [Google Scholar] [CrossRef]
- Chamberlain, C.; Fredericks, B.; McLean, A.; Oldenburg, B.; Mein, J.; Wolfe, R. Associations with low rates of postpartum glucose screening after gestational diabetes among Indigenous and non-Indigenous Australian women. Aust. N. Z. J. Public Health 2015, 39, 69–76. [Google Scholar] [CrossRef]
- Hunt, K.J.; Conway, D.L. Who returns for postpartum glucose screening following gestational diabetes mellitus? Am. J. Obstet. Gynecol. 2008, 198, e401–e406. [Google Scholar] [CrossRef]
- Kirke, A.B.; Atkinson, D.; Moore, S.; Sterry, K.; Singleton, S.; Roxburgh, C.; Parrish, K.; Porter, C.; Marley, J.V. Diabetes screening in pregnancy failing women in rural Western Australia: An audit of oral glucose tolerance test completion rates. Aust. J. Rural Health 2019, 27, 64–69. [Google Scholar] [CrossRef]
- Duke, A.; Yap, C.; Bradbury, R.; Hng, T.M.; Kim, C.; Wansbrough, A.; Cheung, N.W. The discordance between HbA1c and glucose tolerance testing for the postpartum exclusion of diabetes following gestational diabetes. Diabetes Res. Clin. Pract. 2015, 108, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Picon, M.J.; Murri, M.; Munoz, A.; Fernandez-Garcia, J.C.; Gomez-Huelgas, R.; Tinahones, F.J. Hemoglobin A1c versus oral glucose tolerance test in postpartum diabetes screening. Diabetes Care 2012, 35, 1648–1653. [Google Scholar] [CrossRef] [PubMed]
- Remote Primary Health Care Manuals. CARPA Standard Treatment Manual, 7th ed.; Centre for Remote Health: Alice Springs, Australia, 2017. [Google Scholar]
- Farrell, T.; Neale, L.; Cundy, T. Congenital anomalies in the offspring of women with type 1, type 2 and gestational diabetes. Diabet. Med. J. Br. Diabet. Assoc. 2002, 19, 322–326. [Google Scholar] [CrossRef] [PubMed]
- Schaefer-Graf, U.M.; Buchanan, T.A.; Xiang, A.; Songster, G.; Montoro, M.; Kjos, S.L. Patterns of congenital anomalies and relationship to initial maternal fasting glucose levels in pregnancies complicated by type 2 and gestational diabetes. Am. J. Obstet. Gynecol. 2000, 182, 313–320. [Google Scholar] [CrossRef]
- James, S.; Toombs, M.; Brodribb, W. Barriers and enablers to postpartum contraception among Aboriginal Australian women: Factors influencing contraceptive decisions. Aust. J. Prim. Health 2018, 24, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Stratton, I.M.; Adler, A.I.; Neil, H.A.; Matthews, D.R.; Manley, S.E.; Cull, C.A.; Hadden, D.; Turner, R.C.; Holman, R.R. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): Prospective observational study. BMJ 2000, 321, 405–412. [Google Scholar] [CrossRef] [PubMed]
- Villagra, V.G.; Ahmed, T. Effectiveness of a disease management program for patients with diabetes. Health Aff. Proj. Hope 2004, 23, 255–266. [Google Scholar] [CrossRef][Green Version]
- Li, S.Q.; Guthridge, S.; Lawton, P.; Burgess, P. Does delay in planned diabetes care influence outcomes for aboriginal Australians? A study of quality in health care. BMC Health Serv. Res. 2019, 19, 582. [Google Scholar] [CrossRef]
- Bar-Zeev, S.J.; Kruske, S.G.; Barclay, L.M.; Bar-Zeev, N.H.; Carapetis, J.R.; Kildea, S.V. Use of health services by remote dwelling Aboriginal infants in tropical northern Australia: A retrospective cohort study. BMC Pediatr. 2012, 12, 19. [Google Scholar] [CrossRef]
- Yelland, J.; Weetra, D.; Stuart-Butler, D.; Deverix, J.; Leane, C.; Ah Kit, J.; Glover, K.; Gartland, D.; Newbury, J.; Brown, S. Primary health care for Aboriginal women and children in the year after birth: Findings from a population-based study in South Australia. Aust. N. Z. J. Public Health 2016, 40, 418–423. [Google Scholar] [CrossRef]
- Bar-Zeev, S.J.; Barclay, L.; Farrington, C.; Kildea, S. From hospital to home: The quality and safety of a postnatal discharge system used for remote dwelling Aboriginal mothers and infants in the top end of Australia. Midwifery 2012, 28, 366–373. [Google Scholar] [CrossRef] [PubMed]
- Riskin-Mashiah, S.; Almog, R. Missed opportunities for appropriate postpartum care in women with pregestational diabetes. J. Matern. Fetal Neonatal Med. 2016, 29, 1715–1719. [Google Scholar] [CrossRef] [PubMed]
- Ho, J.; Bachman-Carter, K.; Thorkelson, S.; Anderson, K.; Jaggi, J.; Brown, C.; Nelson, K.; Curley, C.; King, C.; Atwood, S.; et al. Glycemic control and healthcare utilization following pregnancy among women with pre-existing diabetes in Navajo Nation. BMC Health Serv. Res. 2018, 18, 629. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Russell, D.J.; Guthridge, S.; Ramjan, M.; Jones, M.P.; Humphreys, J.S.; Carey, T.A.; Wakerman, J. Long-term trends in supply and sustainability of the health workforce in remote Aboriginal communities in the Northern Territory of Australia. BMC Health Serv. Res. 2017, 17, 836. [Google Scholar] [CrossRef]
- Russell, D.J.; Zhao, Y.; Guthridge, S.; Ramjan, M.; Jones, M.P.; Humphreys, J.S.; Wakerman, J. Patterns of resident health workforce turnover and retention in remote communities of the Northern Territory of Australia, 2013-2015. Hum. Resour. Health 2017, 15, 52. [Google Scholar] [CrossRef]
- McLean, A.; Kirkham, R.; Campbell, S.; Whitbread, C.; Barrett, J.; Connors, C.; Boyle, J.; Brown, A.; Mein, J.; Wenitong, M.; et al. Improving Models of Care for Diabetes in Pregnancy: Experience of Current Practice in Far North Queensland, Australia. Front. Public Health 2019, 7, 192. [Google Scholar] [CrossRef]

| Maternal Characteristics | All Pregnancies | GDM | T2D | p-Value by Diabetes Type |
|---|---|---|---|---|
| Number a | 197 b | 148 | 40 | |
| Age, mean (SD) | 28.7 (6.3) | 27.8 (6.2) | 32 (5) | <0.001 |
| Ethnicity, n (%) | ||||
| Aboriginal | 188 (95.5) | 139 (93.9) | 40 (100) | |
| Torres Strait Islander | 1 (<1) | 1 (0.7) | 0 | |
| Non-Indigenous | 8 (4) | 8 (5.4) | 0 | |
| Geographic location, n (%) | <0.001 | |||
| Top End | 130 (66) | 107 (72.3) | 17 (42.5) | |
| Central Australia | 67 (34) | 41 (27.7) | 23 (57.5) | |
| Glycaemic testing results | n = 46 | |||
| 4.4 [4.1, 5]) | NA | |||
| OGTT fasting mmol/L median (IQR) | 5.6 [5.2, 8.2] | NA | ||
| OGTT 2 h mmol/L median (IQR) | n = 88 | n = 54 | n = 31 | <0.001 |
| HbA1C % mean (SD) | 6.4 (1.5) | 6.0 (1.1) | 7.3 (1.9) | |
| HbA1C mmol/mol mean (SD) | 46.8 (16.5) | 42.1 (11.7) | 56.0 (20.3) | |
| Diabetes treatment, n (%) | <0.001 | |||
| Diet only | 110 (56) | 94 (63) | 8 (20) | |
| Metformin only | 48 (24) | 32 (22) | 15 (37) | |
| Insulin only | 8 (4) | 5 (3) | 3 (8) | |
| Metformin and insulin | 31 (16) | 17 (12) | 14 (35) | |
| Weight kg mean (SD) c | n = 113 | n = 77 | n = 30 | 0.1927 |
| 72.0 (15.5) | 70.9 (17) | 75.3 (10.9) | ||
| BMI kg/m2 mean (SD) | n = 80 | n = 49 | n = 26 | 0.1013 |
| 27.5 (4.9) | 26.9 (5.3) | 28.9 (4) | ||
| Number of women breastfeeding, n (%) d | n = 117 | n = 92 | n = 21 | 0.283 |
| 104 (88.9) | 80 (87) | 20 (95.2) | ||
| Smoking status e | n = 81 | n = 50 | n = 26 | 0.257 |
| 42 (51) | 28 (56) | 11 (42.3) | ||
| Contraception use f | n = 132 | n = 106 | n = 22 | 0.809 |
| No contraception, n (%) | 9 (8) | 7 (6.6) | 2 (9) | |
| Implanon, n (%) | 84 (63) | 70 (66) | 13 (59) | |
| Other g, n (%) | 39 (29) | 29 (27.4) | 7 (31.8) |
| Characteristics | GDM Postpartum Normoglycaemia (n = 48) | GDM Postpartum Dysglycaemia (n = 32) | Comparison (p-Value) |
|---|---|---|---|
| Age years, mean (SD) | 28 (6.0) | 29 (6.5) | 0.456 |
| Prediabetes, n (%) | - | 8 (25) | |
| Diabetes, n (%) | - | 24 (75) | |
| Ethnicity, n (%) | |||
| Aboriginal | 46 (96%) | 31 (97%) | |
| Torres Strait Islander | 0 | 1 (3%) | |
| Non-Indigenous | 2 (4%) | 0 | |
| BMI, kg/m2, mean (SD) | 24.5 (5.3) | 29.0 (5.3) | 0.01 |
| Insulin use during pregnancy, n (%) | 8 (17) | 11 (34) | 0.086 |
| OGTT fasting mmol/L, median (IQR) | 4.4 (4.1–4.9) | 4.8 (4.2–6.8) | 0.146 |
| OGTT 2 h mmol/L, median (IQR) | 5.5 (4.9–6) | 9.1 (8.3–11.4) | <0.01 |
| HbA1C %, mean (SD) | 5.5 (0.30) | 6.5 (1.3) | <0.01 |
| HbA1C mmol/mol, mean (SD) | 36.2 (3.3) | 47.5 (13.9) | <0.01 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wood, A.; MacKay, D.; Fitzsimmons, D.; Derkenne, R.; Kirkham, R.; Boyle, J.A.; Connors, C.; Whitbread, C.; Welsh, A.; Brown, A.; et al. Primary Health Care for Aboriginal Australian Women in Remote Communities after a Pregnancy with Hyperglycaemia. Int. J. Environ. Res. Public Health 2020, 17, 720. https://doi.org/10.3390/ijerph17030720
Wood A, MacKay D, Fitzsimmons D, Derkenne R, Kirkham R, Boyle JA, Connors C, Whitbread C, Welsh A, Brown A, et al. Primary Health Care for Aboriginal Australian Women in Remote Communities after a Pregnancy with Hyperglycaemia. International Journal of Environmental Research and Public Health. 2020; 17(3):720. https://doi.org/10.3390/ijerph17030720
Chicago/Turabian StyleWood, Anna, Diana MacKay, Dana Fitzsimmons, Ruth Derkenne, Renae Kirkham, Jacqueline A. Boyle, Christine Connors, Cherie Whitbread, Alison Welsh, Alex Brown, and et al. 2020. "Primary Health Care for Aboriginal Australian Women in Remote Communities after a Pregnancy with Hyperglycaemia" International Journal of Environmental Research and Public Health 17, no. 3: 720. https://doi.org/10.3390/ijerph17030720
APA StyleWood, A., MacKay, D., Fitzsimmons, D., Derkenne, R., Kirkham, R., Boyle, J. A., Connors, C., Whitbread, C., Welsh, A., Brown, A., Shaw, J. E., & Maple-Brown, L. (2020). Primary Health Care for Aboriginal Australian Women in Remote Communities after a Pregnancy with Hyperglycaemia. International Journal of Environmental Research and Public Health, 17(3), 720. https://doi.org/10.3390/ijerph17030720





