Parent and Clinician Perspectives on the Participation of Children with Cerebral Palsy in Community-Based Football: A Qualitative Exploration in a Regional Setting
Abstract
1. Introduction
1.1. Frameworks of PA Participation
1.2. Factors Influencing Participation: Current Knowledge and Gaps in Knowledge
2. Materials and Methods
2.1. Participants
2.1.1. Clinician Focus Groups
2.1.2. Parent Focus Groups
2.2. Procedure
2.3. Data Analysis
2.4. Credibility and Qualitative Rigor
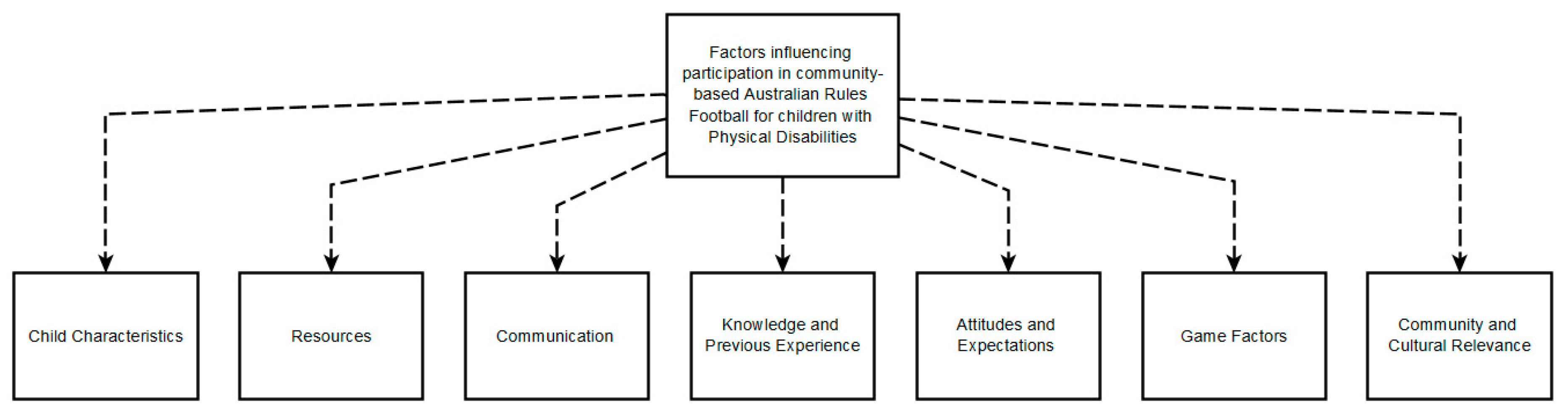
3. Results
3.1. Child Characteristics
“... You might have a child in a wheelchair, you might have some in a walking frame, and you might have some that can... walk independently… often the speed of sport can be too fast for the kids”—Clinician
“Kids who have CP have such a broad range of cognitive capacities and their communication”—Clinician
“I think, he’s just that in that age group yet like, where he is, you know six, he’s still not that interested in a lot of things”—Father of a six-year-old boy
“…some of it is the mental bit, “oh the balls wet”, you know “I don’t want to touch it”, things like that”—Father of a six-year-old boy
“…well for Brad (name anonymised to protect participant identity), I don’t think it’s that he doesn’t know he can’t do it, I think he just hasn’t got that confidence yet…”—Father of a six-year-old boy
“… I think it’s almost as if the kids that are more physical able, your GMFCS I’s and high functioning II’s, that notice it. Like they’re the ones that realise their different cause they’re almost there”—Clinician
3.2. Resources
“not that we need to go and adapt and modify everything but for the club to be aware of what works within their environment or what kind of access is possible in terms of...you know the toilet access, or parking, and all those sorts of things....”—Clinician
“…if they do have a one-off, I know it’s again, it’s like anything, trying to find the day and people to come, but umm they can see that kids of all ages and all levels of disabilities can participate. And if they like it”—Father of a six-year-old boy
3.3. Communication
“…that might help with the education, wider (repeated) reaching education, if clubs are encouraged to have that inclusion officer and they attend a day of education…”—Clinician
“...instead of me giving Rebecca (name anonymised to protect participant identity) strategies of how to deal with that, but the coach giving her strategies as well. So that she’s getting, you know, the same message but from different people and not just getting it from me and disregarding it…”.—Mother of an eight-year-old girl
“So if this child comes and these are the additional strategies or things that we’re using that supports that child to be here, that information is consistent and passed on to anybody who’s running the group that day”—Clinician
“Like you know it comes down to the parents as well and having that confidence and being the advocate…”.—Clinician
“…When she starts something new… I just go and speak to the coach and say this is it, you know. Have a go. If you have any issues, let me know. We’ll talk to the physio and we’ll work through... If you’re finding that she can’t do something, talk to me about it and let’s talk about her CP and how it’s affecting that.”—Mother of an eight-year-old girl
3.4. Knowledge and Previous Experience
“…he was there, and he had fun and you know he said he had fun…”
“…the parents aren’t playing, so the kids don’t play and then that whole cycle…”—Clinician
“but I think that it would get a ‘ohhhh what do we do...’ because I reckon there is a lack of experience…”—Clinician
“…it’s that concern for the child’s safety or you know, worried they might knocked by someone else or they might get urm so you know that’s genuine concern but having the knowledge to know that’s ok and [repeated], yeah what the risks are or alleviating some of that concern can go a long way to…helping with just general confidence.”—Clinician
“…even having training for clubs in general about what inclusive practice looks like and what that means for... yeah that individual child and family...”—Clinician
“…if I said to them. ‘Do you wanna play footy?’ or ‘do you wanna play sport?’…and actually more actively encouraging either their parents or the child to think of it as an option and encouraging it for those reasons you know... you have your green prescription from the doctor... this will be the green prescription from your therapist... Find a sports team and go and play”.
3.5. Attitudes and Expectations
“There’s a lot of worry for the child’s experience of rejection, or failure, or you know perhaps not failure but not success”—Clinician
“I think having the culture of enjoyment without the competitiveness [is] the primary thing. So, I guess within the club culture, promoting participation as the main thing. Let’s still win, we don’t have to take scoring out of the equation, everyone knows who wins I guess a shift in that culture”—Clinician
“…the coach was very welcoming. And so, you know, that’s fine, we don’t have an issue with children with disabilities coming and joining in and yeah”.
“…her gymnastics coach…has CP and that was, she had a first session last week… walked away from that and said, ‘Oh that’s so good mum, she gets me, she understands me’. So, having that kind of mentor and role model who has a disability and is quite capable and has competed in umm like Paralympics type stuff has kind of given her inspiration, ‘yes I can do this’, and confidence”—Mother of an eight-year-old girl
3.6. Game Factors
“So what if the ball is kicked off and then they have... you know no-one’s allowed to move for three seconds and that child gets a bit of extra time...urm or if it’s thrown to them, you can’t tackle them or take the ball off them until you know three second, five seconds or whatever so that they have an opportunity to do something with it before it’s... they’ve lost the ball or yeah...”—Clinician
“... and for some kids, having a [repeated] picture to represent a word or to represent communication can be so incredibly valuable, especially in a busy, chaotic, distracting environment where the speech comes and goes and its gone, but if an umpire or a coach could hold up a symbol that said what the call was, or what the thing they’re doing was, just something very simple and clear. You know umpires could wear a lanyard that had 10 symbols...”—Clinician
“If urm environmental issues became a problem but there was openness to consider adapting the environment, so whether it be the surfaces or the size of the ground or whatever comes urm comes with that might need to be considered that there was a willingness to consider other options within the sport”—Clinician
“…if it was offered on a Monday or Tuesday night, earlier in the week before she is tired from the week at school”.
“Children with disabilities or young adults with disabilities tend to be given more of the role of a helper or run the bench or statistician or you’re an umpire or something like that. So, you’re still involved but with a different role typically…I think it’s becoming a little bit more open”—Clinician
“I also like pairing up kids, I think that works nicely and having sort of a buddy system where everybody is, if you get the ball, you have to pass to your buddy before the next person goes…pair someone whose sort of better skilled than someone who is less skilled, so one of the people that gets the ball all the time then has to pass the ball to the person that doesn’t get the ball …”—Clinician
3.7. Community and Cultural Relevance
“One of the big standouts for me for any team or club is about that, you’re involved in the community, you’re part of something, there’s a relationship and there’s connections being made”—Clinician
“Families would go down and hang out at the footy and kick alongside the ground.”—Clinician
“The parents love the fact that they’re (the child) getting that sense of connectedness”—Clinician
“I’ve got a number of kids that would love to be just part of a club, but maybe have their own team with altered rules and then but still you know still come to the club rooms after and still get best on ground and still do all that sort of stuff but it’s sort of an all-abilities group—Clinician
“I think the love of football is very strong in Geelong…”—Clinician
4. Discussion
4.1. Limitations
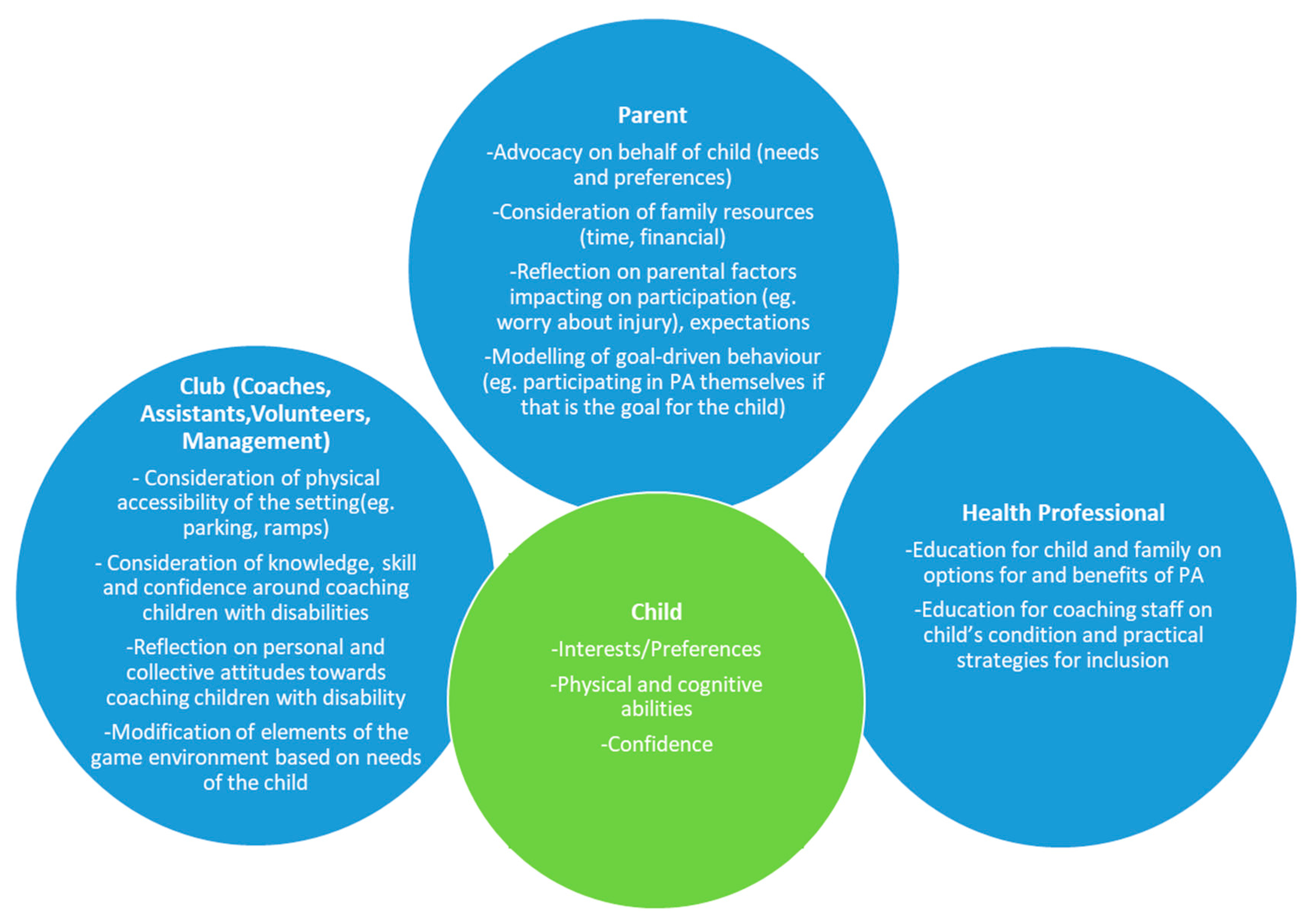
4.2. The Need for A Holistic Approach
Communicate: For parents, clinicians and club staff to develop a system of communication that is appropriate for the whole system, prior to the child commencing participation (e.g., developing a shared summary document of the child’s preferences, strengths and weaknesses that can be modified throughout the season). The role of the parent within the care-team in advocating for the child is particularly relevant in this instance.
Consider: For each party within the care-team to engage in self-reflection about their individual contributions to the system in facilitating community-based PA participation for the child. This entails reflection on strengths they can bring (e.g., expert knowledge on a sport or disability, mentoring players with disability as a coach with a disability), as well as any challenges they may anticipate with regards to facilitating participation for the child and how they can work with the care-team to problem-solve this (e.g., attitudes towards disability, or the physical club facilities not being wheelchair accessible).
Collaborate: For parents, clinicians and club staff to develop opportunities for knowledge-sharing and joint decision-making on tailored adaptations for inclusive practices (e.g., tip-sheets by clinicians with disability-specific information, introducing a buddy system). The clinician’s provision of disability-specific information and how it may impact on the child’s participation, alongside the club’s input on centre specific information (e.g., club expectations, facilities), will facilitate the development of tailored interventions based on the child’s needs and preferences and the consistent use of strategies across contexts.
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Purpose | Questions/Prompts |
|---|---|
| Introductions and explanation of the purpose of the session | Purpose: to discuss perspectives on the participation of children with physical challenges in football within the local community. |
| Opening questions | What is the age group of children that you work with? |
| Importance of football within local community | How important is it to play football for the children you work with living in the local community? |
| What would playing football mean to children you work with and their families? | |
| Would the children you work with enjoy football? | |
| Access to organised football activities within the local community | Do you feel that the children you work with have access to the football community in Geelong? Why or why not? |
| Type of organised activity for children with physical challenges | Have you found integrated or segregated physical activities to be more beneficial for the children you work with? |
| Acceptance of children with physical challenges in the football community | How do you think the children you work with are received in the football community? |
| How accepting are coaches, other children and families towards children with CP? | |
| Benefits | What do you think the children you work with would get out of playing football? |
| Barriers | From your experience, what have been some of the challenges or barriers to a child with additional physical challenges participating in football? |
| Facilitators | What supports would help the children you work with to participate in football? |
| Strategies to increase engagement | Have you come across any strategies so far that might be helpful in getting more kids to participate? |
| What key recommendations would you make for including children with physical disabilities in football? |
| Purpose | Questions/Prompts |
|---|---|
| Introductions and explanation of the purpose of the session | Purpose: to discuss perspectives on the participation of children with physical challenges in football within the local community. |
| Opening questions | Tell us briefly about your child and what their experience of football has been to date. |
| Child’s current engagement in football. | Does your child currently play football? |
| If yes, do they enjoy it? | |
| If no, do they want to play football? | |
| Importance of football within local community and within family network | How important is it to play football for your child in the Geelong community? |
| What would playing footy mean to your child and for your family? | |
| Access to organised football activities within the local community | Do you feel that your child has access to the football community in Geelong? Why or why not? |
| Have you found integrated or segregated activities to be more beneficial for your child? | |
| Acceptance of children with physical challenges in the football community | How do you think your child is received in the football community? |
| How accepting are coaches, other children and families towards children with CP getting involved in sport? | |
| Benefits | What are some of the benefits of participating in football for your child? |
| What does/would your child get out of playing football? | |
| Barriers | What have been some of the challenges or barriers to your child participating in football? |
| Strategies to increase engagement | What supports are available to help your child participate in football? |
| What supports/strategies would you recommend increasing the likelihood that your child will participate in football? |
References
- Smith, L.B. Cognition as a dynamic system: Principles from embodiment. Dev. Rev. 2005, 25, 278–298. [Google Scholar] [CrossRef]
- May, T.; Rinehart, N.; Barnett, L.; Hinkley, T.; McGillivray, J.; Skouteris, H.; Stephens, D.; Goldfinch, D. ‘We’re Doing AFL Auskick as Well’: Experiences of an Adapted Football Program for Children with Autism. J. Motor Learn. Dev. 2018, 6, 130–146. [Google Scholar] [CrossRef]
- Howells, K.; Sivaratnam, C.; May, T.; Lindor, E.; McGillivray, J.; Rinehart, N. Efficacy of Group-Based Organised Physical Activity Participation for Social Outcomes in Children with Autism Spectrum Disorder: A Systematic Review and Meta-analysis. J. Autism Dev. Disord. 2019, 49, 3290–3308. [Google Scholar] [CrossRef] [PubMed]
- Epstein, A.; Whitehouse, A.; Williams, K.; Murphy, N.; Leonard, H.; Davis, E.; Reddihough, D.; Downs, J. Parent-observed thematic data on quality of life in children with autism spectrum disorder. Autism 2019, 23, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Imms, C.; Reilly, S.; Carlin, J.; Dodd, K.J. Characteristics influencing participation of Australian children with cerebral palsy. Disabil. Rehabil. 2009, 31, 2204–2215. [Google Scholar] [CrossRef] [PubMed]
- Orlin, M.N.; Palisano, R.J.; Chiarello, L.A.; Kang, L.J.; Polansky, M.; Almasri, N.; Maggs, J. Participation in home, extracurricular, and community activities among children and young people with cerebral palsy. Dev. Med. Child Neurol. 2010, 52, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Keawutan, P.; Bell, K.; Davies, P.S.; Boyd, R.N. Systematic review of the relationship between habitual physical activity and motor capacity in children with cerebral palsy. Res. Dev. Disabil. 2014, 35, 1301–1309. [Google Scholar] [CrossRef]
- Mitchell, L.E.; Ziviani, J.; Boyd, R.N. Habitual physical activity of independently ambulant children and adolescents with cerebral palsy: Are they doing enough? Phys. Ther. 2015, 95, 202–211. [Google Scholar] [CrossRef]
- Ryan, J.M.; Hensey, O.; McLoughlin, B.; Lyons, A.; Gormley, J. Reduced moderate-to-vigorous physical activity and increased sedentary behavior are associated with elevated blood pressure values in children with cerebral palsy. Phys. Ther. 2014, 94, 1144–1153. [Google Scholar] [CrossRef]
- Svestkova, O.; Sladkova, P.; Kotkova, K. Application of International Classification of Functioning, Disability and Health (ICF), Functional Health and Disability. Cent. Eur. J. Public Health 2016, 24, 83–85. [Google Scholar] [CrossRef]
- Martin Ginis, K.A.; Ma, J.K.; Latimer-Cheung, A.E.; Rimmer, J.H. A systematic review of review articles addressing factors related to physical activity participation among children and adults with physical disabilities. Health Psychol. Rev. 2016, 10, 478–494. [Google Scholar] [CrossRef] [PubMed]
- Imms, C.; Granlund, M.; Wilson, P.H.; Steenbergen, B.; Rosenbaum, P.L.; Gordon, A.M. Participation, both a means and an end: A conceptual analysis of processes and outcomes in childhood disability. Dev. Med. Child Neurol. 2017, 59, 16–25. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Functioning, Disability and Health: ICF; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Shields, N.; Synnot, A.J.; Barr, M. Perceived barriers and facilitators to physical activity for children with disability: A systematic review. Br. J. Sports Med. 2012, 46, 989–997. [Google Scholar] [CrossRef] [PubMed]
- Bloemen, M.A.; Backx, F.J.; Takken, T.; Wittink, H.; Benner, J.; Mollema, J.; de Groot, J.F. Factors associated with physical activity in children and adolescents with a physical disability: A systematic review. Dev. Med. Child Neurol. 2015, 57, 137–148. [Google Scholar] [CrossRef]
- Li, R.; Sit, C.H.P.; Yu, J.J.; Duan, J.Z.J.; Fan, T.C.M.; McKenzie, T.L.; Wong, S.H.S. Correlates of physical activity in children and adolescents with physical disabilities: A systematic review. Prev. Med. 2016, 89, 184–193. [Google Scholar] [CrossRef]
- Ajzen, I.; Fishbein, M. The influence of attitudes on behavior. In The Handbook of Attitudes; Albarracín, D., Johnson, B., Zanna, M., Eds.; Erlbaum: Mahwah, NJ, USA, 2005; pp. 173–221. [Google Scholar]
- Hagger, M.; Chatzisarantis, N. Intrinsic Motivation and Self-Determination in Exercise and Sport; Human Kinetics: Leeds, UK, 2007. [Google Scholar]
- Barr, M.; Shields, N. Identifying the barriers and facilitators to participation in physical activity for children with Down syndrome. J. Intellect. Disabil. Res. 2011, 55, 1020–1033. [Google Scholar] [CrossRef]
- Law, M.; King, G.; King, S.; Kertoy, M.; Hurley, P.; Rosenbaum, P.; Young, N.; Hanna, S. Patterns of participation in recreational and leisure activities among children with complex physical disabilities. Dev. Med. Child Neurol. 2006, 48, 337–342. [Google Scholar] [CrossRef]
- Majnemer, A.; Shevell, M.; Law, M.; Birnbaum, R.; Chilingaryan, G.; Rosenbaum, P.; Poulin, C. Participation and enjoyment of leisure activities in school-aged children with cerebral palsy. Dev. Med. Child Neurol. 2008, 50, 751–758. [Google Scholar] [CrossRef]
- Wright, A.; Roberts, R.; Bowman, G.; Crettenden, A. Barriers and facilitators to physical activity participation for children with physical disability: Comparing and contrasting the views of children, young people, and their clinicians. Disabil. Rehabil. 2019, 41, 1499–1507. [Google Scholar] [CrossRef]
- Verschuren, O.; Darrah, J.; Novak, I.; Ketelaar, M.; Wiart, L. Health-enhancing physical activity in children with cerebral palsy: More of the same is not enough. Phys. Ther. 2014, 94, 297–305. [Google Scholar] [CrossRef]
- Morris, A.; Imms, C.; Kerr, C.; Adair, B. Sustained participation in community-based physical activity by adolescents with cerebral palsy: A qualitative study. Disabil. Rehabil. 2018, 1–9. [Google Scholar] [CrossRef]
- Fauconnier, J.; Dickinson, H.O.; Beckung, E.; Marcelli, M.; McManus, V.; Michelsen, S.I.; Parkes, J.; Parkinson, K.N.; Thyen, U.; Arnaud, C.; et al. Participation in life situations of 8–12 year old children with cerebral palsy: Cross sectional European study. BMJ 2009, 338, b1458. [Google Scholar] [CrossRef]
- Hammal, D.; Jarvis, S.N.; Colver, A.F. Participation of children with cerebral palsy is influenced by where they live. Dev. Med. Child Neurol. 2004, 46, 292–298. [Google Scholar] [CrossRef]
- Anaby, D.; Hand, C.; Bradley, L.; DiRezze, B.; Forhan, M.; DiGiacomo, A.; Law, M. The effect of the environment on participation of children and youth with disabilities: A scoping review. Disabil. Rehabil. 2013, 35, 1589–1598. [Google Scholar] [CrossRef]
- Colver, A.F.; Dickinson, H.O.; Parkinson, K.; Arnaud, C.; Beckung, E.; Fauconnier, J.; Marcelli, M.; McManus, V.; Michelsen, S.I.; Parkes, J.; et al. Access of children with cerebral palsy to the physical, social and attitudinal environment they need: A cross-sectional European study. Disabil. Rehabil. 2011, 33, 28–35. [Google Scholar] [CrossRef]
- Walker, A.; Colquitt, G.; Elliott, S.; Emter, M.; Li, L. Using participatory action research to examine barriers and facilitators to physical activity among rural adolescents with cerebral palsy. Disabil. Rehabil. 2019, 1–12. [Google Scholar] [CrossRef]
- Reedman, S.; Boyd, R.N.; Sakzewski, L. The efficacy of interventions to increase physical activity participation of children with cerebral palsy: A systematic review and meta-analysis. Dev. Med. Child Neurol. 2017, 59, 1011–1018. [Google Scholar] [CrossRef]
- Trainor, A.A. Diverse Approaches to Parent Advocacy During Special Education Home-School Interactions Identification and Use of Cultural and Social Capital. Remedial Spec. Educ. 2010, 31, 34–47. [Google Scholar] [CrossRef]
- Brunton, L.K. Clinicians Are the Missing Link to Sustainable Community-Based Physical Activity Participation for Children with Disabilities. Phys. Occup. Ther. Pediatrics 2017, 37, 359–361. [Google Scholar] [CrossRef]
- Palisano, R.J.; Chiarello, L.A.; King, G.A.; Novak, I.; Stoner, T.; Fiss, A. Participation-based therapy for children with physical disabilities. Disabil. Rehabil. 2012, 34, 1041–1052. [Google Scholar] [CrossRef]
- Imms, C.; Adair, B.; Keen, D.; Ullenhag, A.; Rosenbaum, P.; Granlund, M. ‘Participation’: A systematic review of language, definitions, and constructs used in intervention research with children with disabilities. Dev. Med. Child Neurol. 2016, 58, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Thomas, E.; Magilvy, J.K. Qualitative Rigor or Research Validity in Qualitative Research. J. Spec. Pediatric Nurs. 2011, 16, 151–155. [Google Scholar] [CrossRef] [PubMed]
- Lauruschkus, K.; Nordmark, E.; Hallstrom, I. Parents’ experiences of participation in physical activities for children with cerebral palsy—Protecting and pushing towards independence. Disabil. Rehabil. 2017, 39, 771–778. [Google Scholar] [CrossRef]
- King, G.; McDougall, J.; Dewit, D.; Petrenchik, T.; Hurley, P.; Law, M. Predictors of Change Over Time in the Activity Participation of Children and Youth with Physical Disabilities. Children’s Health Care 2009, 38, 321–351. [Google Scholar] [CrossRef]
- Hays, K.; Thomas, O.; Maynard, I.; Bawden, M. The role of confidence in world-class sport performance. J. Sport Sci. 2009, 27, 1185–1199. [Google Scholar] [CrossRef]
- Anderson, D.; Dumont, S.; Jacobs, P.; Azzaria, L. The personal costs of caring for a child with a disability: A review of the literature. Public Health Rep. 2007, 122, 3–16. [Google Scholar] [CrossRef]
- Maxwell, G.; Alves, I.; Granlund, M. Participation and environmental aspects in education and the ICF and the ICF-CY: Findings from a systematic literature review. Dev. Neurorehabilit. 2012, 15, 63–78. [Google Scholar] [CrossRef]
- Benito, K.G.; Walther, M. Therapeutic Process During Exposure: Habituation Model. J. Obs. Compuls. Related Disord. 2015, 6, 147–157. [Google Scholar] [CrossRef]
- Bigby, C.; Fyffe, C.; Ozanne, E. Planning and Support for People with Intellectual Disabilities: Issues for Case Managers and Other Professionals; UNSW Press: Sydney, Australia, 2007. [Google Scholar]
- Rosenbaum, P.; Gorter, J.W. The ‘F-words’ in childhood disability: I swear this is how we should think! Child Care Health Dev. 2012, 38, 457–463. [Google Scholar] [CrossRef]
- Foley, K.R.; Blackmore, A.M.; Girdler, S.; O’Donnell, M.; Glauert, R.; Llewellyn, G.; Leonard, H. To Feel Belonged: The Voices of Children and Youth with Disabilities on the Meaning of Wellbeing. Child Indic. Res. 2012, 5, 375–391. [Google Scholar] [CrossRef]
- Vasileiou, K.; Barnett, J.; Thorpe, S.; Young, T. Characterising and justifying sample size sufficiency in interview-based studies: Systematic analysis of qualitative health research over a 15-year period. BMC Med. Res. Methodol. 2018, 18. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sivaratnam, C.; Howells, K.; Stefanac, N.; Reynolds, K.; Rinehart, N. Parent and Clinician Perspectives on the Participation of Children with Cerebral Palsy in Community-Based Football: A Qualitative Exploration in a Regional Setting. Int. J. Environ. Res. Public Health 2020, 17, 1102. https://doi.org/10.3390/ijerph17031102
Sivaratnam C, Howells K, Stefanac N, Reynolds K, Rinehart N. Parent and Clinician Perspectives on the Participation of Children with Cerebral Palsy in Community-Based Football: A Qualitative Exploration in a Regional Setting. International Journal of Environmental Research and Public Health. 2020; 17(3):1102. https://doi.org/10.3390/ijerph17031102
Chicago/Turabian StyleSivaratnam, Carmel, Katherine Howells, Nicole Stefanac, Kelly Reynolds, and Nicole Rinehart. 2020. "Parent and Clinician Perspectives on the Participation of Children with Cerebral Palsy in Community-Based Football: A Qualitative Exploration in a Regional Setting" International Journal of Environmental Research and Public Health 17, no. 3: 1102. https://doi.org/10.3390/ijerph17031102
APA StyleSivaratnam, C., Howells, K., Stefanac, N., Reynolds, K., & Rinehart, N. (2020). Parent and Clinician Perspectives on the Participation of Children with Cerebral Palsy in Community-Based Football: A Qualitative Exploration in a Regional Setting. International Journal of Environmental Research and Public Health, 17(3), 1102. https://doi.org/10.3390/ijerph17031102





