Socioeconomic Inequalities in Child Malnutrition in Bangladesh: Do They Differ by Region?
Abstract
1. Introduction
2. Materials and Methods
2.1. Data and Samples
2.2. Measures of Child Malnutrition
2.3. Explanatory Variables
2.4. Data Analysis
2.5. Ethical Approval
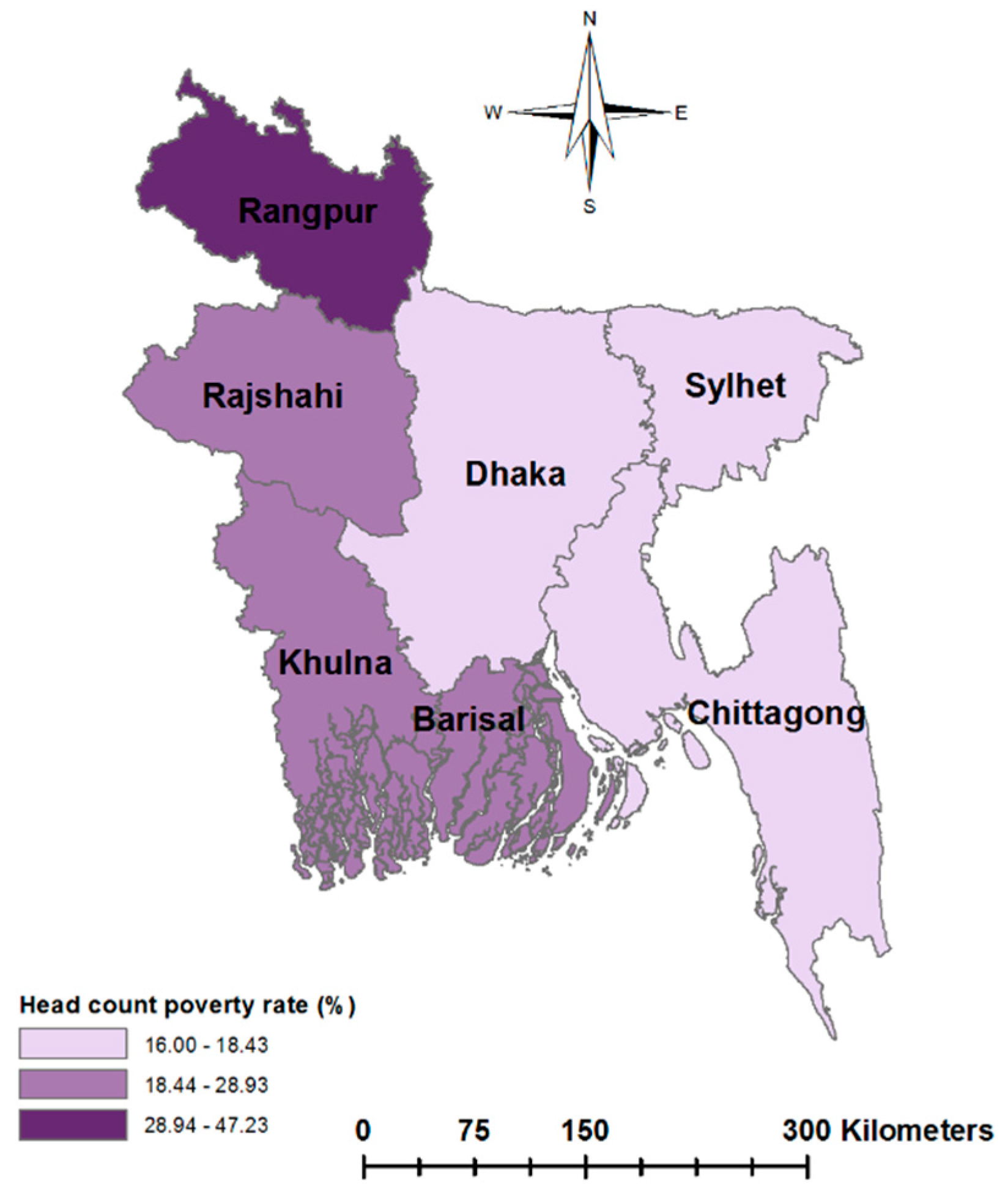
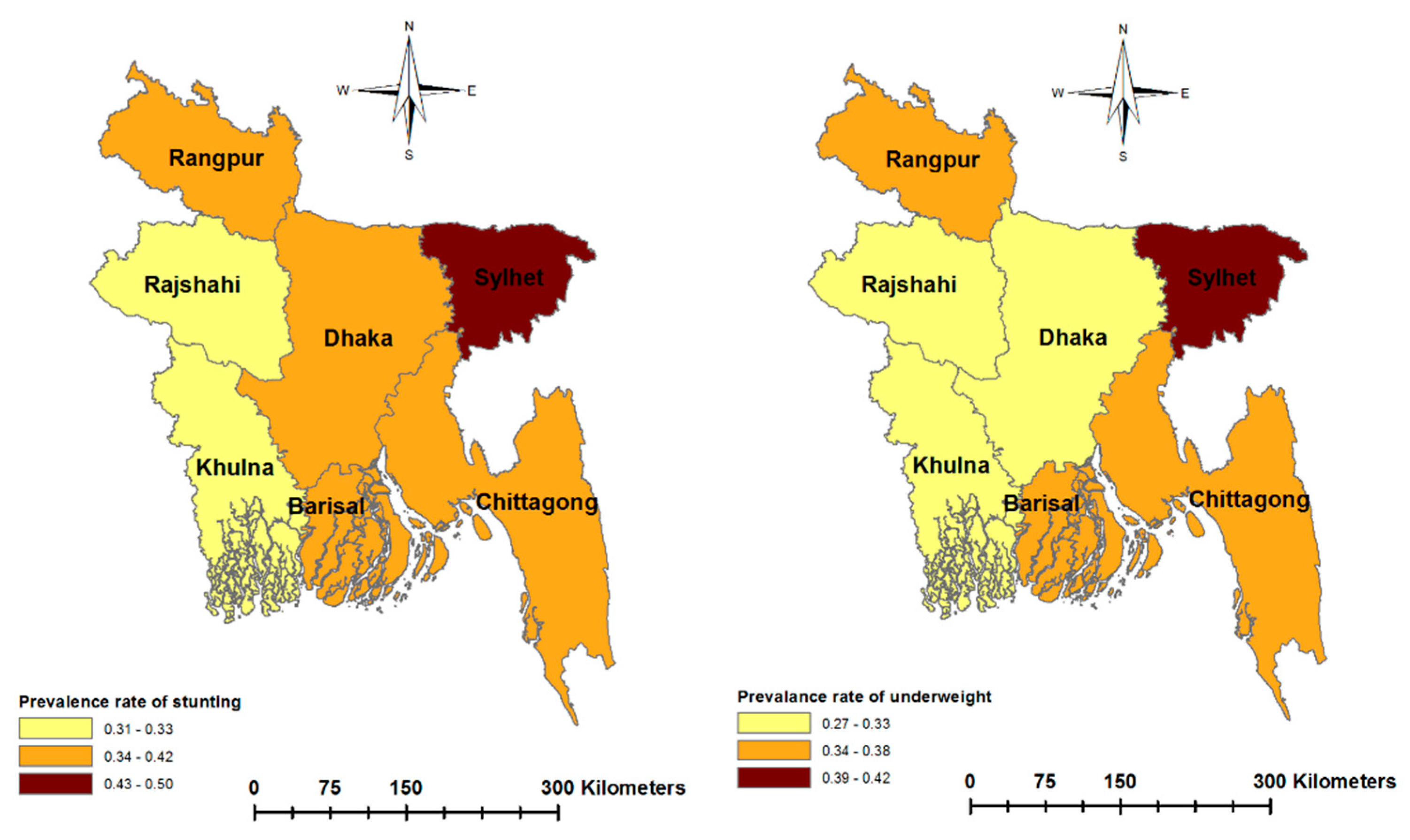
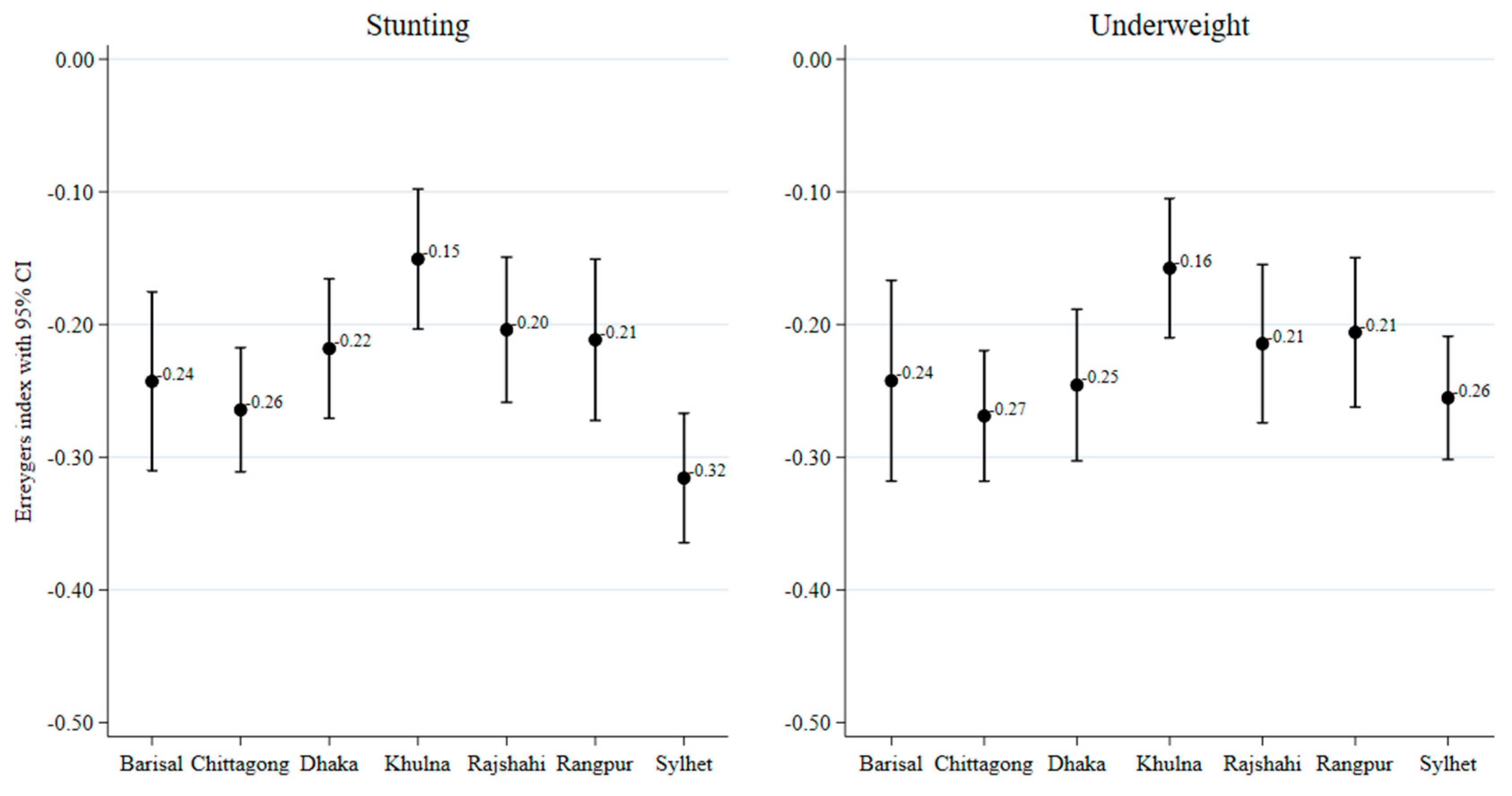
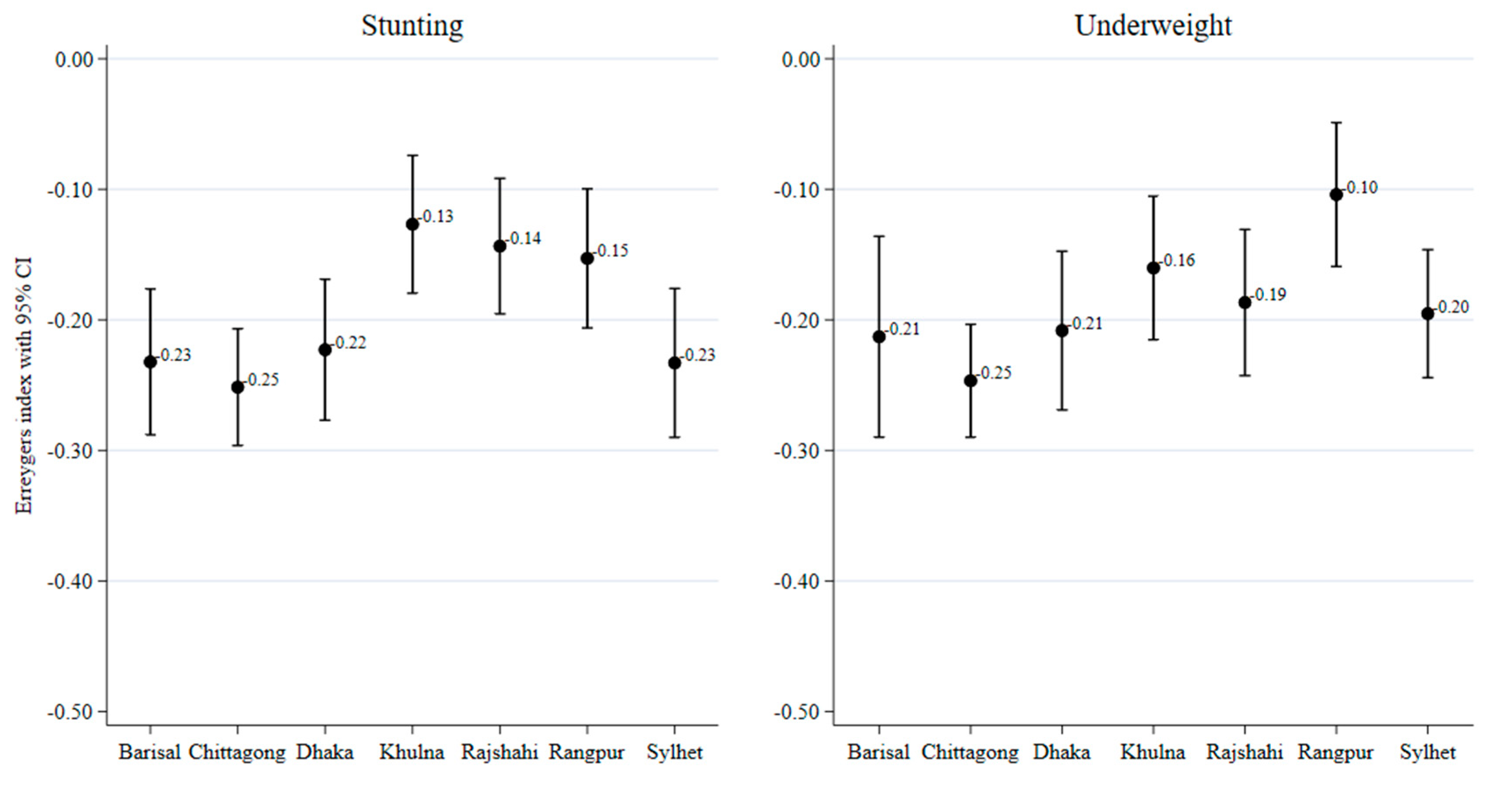
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Black, R.E.; Allen, L.H.; Bhutta, Z.A.; Caulfield, L.E.; de Onis, M.; Ezzati, M.; Mathers, C.; Rivera, J. Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet 2008, 371, 243–260. [Google Scholar] [CrossRef]
- Development Initiatives. 2018 Global Nutrition Report: Shining a Light to Spur Action on Nutrition; Development Initiatives: Bristol, UK, 2018. [Google Scholar]
- Walker, S.P.; Wachs, T.D.; Grantham-McGregor, S.; Black, M.M.; Nelson, C.A.; Huffman, S.L.; Baker-Henningham, H.; Chang, S.M.; Hamadani, J.D.; Lozoff, B.; et al. Inequality in early childhood: Risk and protective factors for early child development. Lancet 2011, 378, 1325–1338. [Google Scholar] [CrossRef]
- Grantham-McGregor, S.; Cheung, Y.B.; Cueto, S.; Glewwe, P.; Richter, L.; Strupp, B. Developmental potential in the first 5 years for children in developing countries. Lancet 2007, 369, 60–70. [Google Scholar] [CrossRef]
- Victora, C.G.; Adair, L.; Fall, C.; Hallal, P.C.; Martorell, R.; Richter, L.; Sachdev, H.S. Maternal and child undernutrition: Consequences for adult health and human capital. Lancet 2008, 371, 340–357. [Google Scholar] [CrossRef]
- Hoddinott, J.; Maluccio, J.A.; Behrman, J.R.; Flores, R.; Martorell, R. Effect of a nutrition intervention during early childhood on economic productivity in Guatemalan adults. Lancet 2008, 371, 411–416. [Google Scholar] [CrossRef]
- Tamiru, D.; Belachew, T. The association of food insecurity and school absenteeism: Systematic review. Agric. Food Secur. 2017, 6, 5. [Google Scholar] [CrossRef]
- Belachew, T.; Hadley, C.; Lindstrom, D.; Gebremariam, A.; Lachat, C.; Kolsteren, P. Food insecurity, school absenteeism and educational attainment of adolescents in Jimma Zone Southwest Ethiopia: A longitudinal study. Nutr. J. 2011, 10, 29. [Google Scholar] [CrossRef]
- Ahmmed, M. Impact of wealth inequality on child nutrition in Bangladesh. Paediatr. Indones 2013, 53, 299. [Google Scholar] [CrossRef]
- Waber, D.P.; Bryce, C.P.; Girard, J.M.; Fischer, L.K.; Fitzmaurice, G.M.; Galler, J.R. Parental history of moderate to severe infantile malnutrition is associated with cognitive deficits in their adult offspring. Nutr. Neurosci. 2018. [Google Scholar] [CrossRef]
- Desie, S. Intergenerational Cycle of Acute Malnutrition among IDPs in Somalia; Emergency Nutrition Network ENN: Oxford, UK, 2016. [Google Scholar]
- UNICEF. The State of the World’s Children 2019. Children, Food and Nutrition: Growing well in a changing world; UNICEF: New York, NY, USA, 2019. [Google Scholar]
- Raj, A.; Saggurti, N.; Winter, M.; Labonte, A.; Decker, M.R.; Balaiah, D.; Silverman, J.G. The effect of maternal child marriage on morbidity and mortality of children under 5 in India: Cross sectional study of a nationally representative sample. BMJ 2010, 340, 353. [Google Scholar] [CrossRef]
- Uddin, J.; Pulok, M.H.; Johnson, R.B.; Rana, J.; Baker, E. Association between child marriage and institutional delivery care services use in Bangladesh: Intersections between education and place of residence. Public Health 2019, 171, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.-K.; Wen, S.W.; Fleming, N.; Demissie, K.; Rhoads, G.G.; Walker, M. Teenage pregnancy and adverse birth outcomes: A large population based retrospective cohort study. Int. J. Epidemiol. 2007, 36, 368–373. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, K.; Malek, M.A.; Faruque, A.S.G.; Salam, M.A.; Ahmed, T. Health and nutritional status of children of adolescent mothers: Experience from a diarrhoeal disease hospital in Bangladesh. Acta Paediatr. 2007, 96, 396–400. [Google Scholar] [CrossRef] [PubMed]
- Khatun, W.; Rasheed, S.; Alam, A.; Huda, T.M.; Dibley, M.J. Assessing the intergenerational linkage between short maternal stature and under-five stunting and wasting in Bangladesh. Nutrients 2019, 11, 1818. [Google Scholar] [CrossRef]
- Braveman, P.; Gottlieb, L. The social determinants of health: It’s time to consider the causes of the causes. Public Health Rep. 2014, 129, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M.; Allen, J.; Bell, R.; Bloomer, E.; Goldblatt, P. WHO European review of social determinants of health and the health divide. Lancet 2012, 380, 1011–1029. [Google Scholar] [CrossRef]
- Link, B.G.; Phelan, J. Social conditions as fundamental causes of disease. J. Health Soc. Behav. 1995, 80–94. [Google Scholar] [CrossRef]
- Das, S.; Rahman, R.M. Application of ordinal logistic regression analysis in determining risk factors of child malnutrition in Bangladesh. Nutr. J. 2011, 10, 124. [Google Scholar] [CrossRef]
- Pulok, M.H.; Sabah, M.N.-U.; Enemark, U. Socioeconomic inequalities of child malnutrition in Bangladesh. Int. J. Soc. Econ. 2016, 43, 1439–1459. [Google Scholar] [CrossRef]
- Rabbani, A.; Khan, A.; Yusuf, S.; Adams, A. Trends and determinants of inequities in childhood stunting in Bangladesh from 1996/7 to 2014. Int. J. Equity Health 2016, 15, 186. [Google Scholar] [CrossRef]
- Subramanyam, M.A.; Kawachi, I.; Berkman, L.F.; Subramanian, S.V. Socioeconomic Inequalities in Childhood Undernutrition in India: Analyzing Trends between 1992 and 2005. PLoS ONE 2010, 5, e11392. [Google Scholar] [CrossRef] [PubMed]
- Vollmer, S.; Bommer, C.; Krishna, A.; Harttgen, K.; Subramanian, S.V. The association of parental education with childhood undernutrition in low- and middle-income countries: Comparing the role of paternal and maternal education. Int. J. Epidemiol. 2017, 46, 312–323. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.B.; Khan, M.H.R. Role of parental education in reduction of prevalence of childhood undernutrition in Bangladesh. Public Health Nutr. 2018, 21, 1845–1854. [Google Scholar] [CrossRef] [PubMed]
- Arsenault, J.E.; Yakes, E.A.; Islam, M.M.; Hossain, M.B.; Ahmed, T.; Hotz, C.; Lewis, B.; Rahman, A.S.; Jamil, K.M.; Brown, K.H. Very Low Adequacy of Micronutrient Intakes by Young Children and Women in Rural Bangladesh Is Primarily Explained by Low Food Intake and Limited Diversity. J. Nutr. 2013, 143, 197–203. [Google Scholar] [CrossRef]
- Urke, H.B.; Bull, T.; Mittelmark, M.B. Socioeconomic status and chronic child malnutrition: Wealth and maternal education matter more in the Peruvian Andes than nationally. Nutr. Res. 2011, 31, 741–747. [Google Scholar] [CrossRef]
- Fotso, J.C.; Kuate-Defo, B. Socioeconomic inequalities in early childhood malnutrition and morbidity: Modification of the household-level effects by the community SES. Health Place 2005, 11, 205–225. [Google Scholar] [CrossRef]
- Van Vuuren, C.L.; Reijneveld, S.A.; van der Wal, M.F.; Verhoeff, A.P. Neighborhood socioeconomic deprivation characteristics in child (0–18 years) health studies: A review. Health Place 2014, 29, 34–42. [Google Scholar] [CrossRef]
- Earls, F.; Carlson, M. The Social Ecology of Child Health and Well-Being. Annu. Rev. Public Health 2001, 22, 143–166. [Google Scholar] [CrossRef]
- Greves Grow, H.M.; Cook, A.J.; Arterburn, D.E.; Saelens, B.E.; Drewnowski, A.; Lozano, P. Child obesity associated with social disadvantage of children’s neighborhoods. Soc. Sci. Med. 2010, 71, 584–591. [Google Scholar] [CrossRef]
- Hong, R.; Banta, J.E.; Betancourt, J.A. Relationship between household wealth inequality and chronic childhood under-nutrition in Bangladesh. Int. J. Equity Health 2006, 5, 15. [Google Scholar] [CrossRef]
- Mia, M.N.; Rahman, M.S.; Roy, P.K. Sociodemographic and geographical inequalities in under- and overnutrition among children and mothers in Bangladesh: A spatial modelling approach to a nationally representative survey. Public Health Nutr. 2018, 21, 2471–2481. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, C.S.; Zanello, G.; Shankar, B. Rural-urban disparities in child nutrition in Bangladesh and Nepal. BMC Public Health 2013, 13, 581. [Google Scholar] [CrossRef] [PubMed]
- Ali, Z.; Yunus, M.; Sen, B. Regional Inequality in Bangladesh in the 2000s: Re-Visiting the East-West Divide Debate; BIDS: Dhaka, Bangladesh, 2015. [Google Scholar]
- NIPORT; Mitra and Associates; ICF International. Bangladesh Demographic and Health Survey 2014; NIPORT; Mitra and Associates; ICF International: Dhaka, Bangladesh, 2016. [Google Scholar]
- Pulok, M.H.; Uddin, J.; Enemark, U.; Hossin, M.Z. Socioeconomic inequality in maternal healthcare: An analysis of regional variation in Bangladesh. Health Place 2018, 52, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Sarker, A.R.; Sultana, M.; Sheikh, N.; Akram, R.; Ali, N.; Mahumud, R.A.; Alam, K.; Morton, A. Inequality of childhood undernutrition in Bangladesh: A decomposition approach. Int. J. Health Plan. Manag. 2019. [Google Scholar] [CrossRef] [PubMed]
- WHO The WHO Child Growth Standards. Available online: https://www.who.int/childgrowth/en/ (accessed on 3 February 2020).
- O’Donnell, O.; van Doorslaer, E.; Wagstaff, A.; Lindelow, M. Analyzing Health Equity Using Household Survey Data: A Guide to Techniques and their Implementation; The World Bank: Washington, DC, USA, 2008; ISBN 0821369342. [Google Scholar]
- Masibo, P.K.; Makoka, D. Trends and determinants of undernutrition among young Kenyan children: Kenya Demographic and Health Survey; 1993, 1998, 2003 and 2008–2009. Public Health Nutr. 2012, 15, 1715–1727. [Google Scholar] [CrossRef]
- Wagstaff, A.; van Doorslaer, E.; Watanabe, N. On decomposing the causes of health sector inequalities with an application to malnutrition inequalities in Vietnam. J. Econom. 2003, 112, 207–223. [Google Scholar] [CrossRef]
- Rutstein, S.O.; Johnson, K. The DHS Wealth Index: DHS; ORC Macro: Calverton, MD, USA, 2004. [Google Scholar]
- Fry, K.; Firestone, R.; Chakraborty, N.M. Measuring Equity with Nationally Representative Wealth Quintiles; Population Services International: Washington, DC, USA, 2014. [Google Scholar]
- Pulok, M.H.; van Gool, K.; Hajizadeh, M.; Allin, S.; Hall, J. Measuring horizontal inequity in healthcare utilisation: A review of methodological developments and debates. Eur. J. Health Econ. 2019, 1–10. [Google Scholar] [CrossRef]
- Wagstaff, A. The bounds of the concentration index when the variable of interest is binary, with an application to immunization inequality. Health Econ. 2005, 14, 429–432. [Google Scholar] [CrossRef]
- Erreygers, G. Correcting the Concentration Index. J. Health Econ. 2009, 28, 504–515. [Google Scholar] [CrossRef]
- DHS. The DHS Program—Data. Available online: https://dhsprogram.com/data/ (accessed on 7 January 2020).
- Husseini, M.; Darboe, M.K.; Moore, S.E.; Nabwera, H.M.; Prentice, A.M. Thresholds of socio-economic and environmental conditions necessary to escape from childhood malnutrition: A natural experiment in rural Gambia. BMC Med. 2018, 16, 199. [Google Scholar] [CrossRef]
- Chowdhury, M.R.K.; Rahman, M.S.; Khan, M.M.H.; Mondal, M.N.I.; Rahman, M.M.; Billah, B. Risk Factors for Child Malnutrition in Bangladesh: A Multilevel Analysis of a Nationwide Population-Based Survey. J. Pediatr. 2016, 172, 194–201.e1. [Google Scholar] [CrossRef] [PubMed]
- Gruebner, O.; Khan, M.; Burkart, K.; Lautenbach, S.; Lakes, T.; Krämer, A.; Subramanian, S.V.; Galea, S. Spatial variations and determinants of infant and under-five mortality in Bangladesh. Health Place 2017, 47, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Sen, B.; Ali, Z. Ending Extreme Poverty in Bangladesh During the Seventh Five Year Plan: Trends, Drivers and Policies; Planning Commission, Government of Bangladesh: Dhaka, Bangladesh, 2015.
- World Bank; World Food Programme; Bangladesh Bureau of Statistics. Poverty Maps of Bangladesh 2010: Key Findings; World Bank: Washington, DC, USA, 2010.
- Fang, P.; Dong, S.; Xiao, J.; Liu, C.; Feng, X.; Wang, Y. Regional inequality in health and its determinants: Evidence from China. Health Policy 2010, 94, 14–25. [Google Scholar] [CrossRef] [PubMed]
- Osorio, A.M.; Bolancé, C.; Madise, N. Community socioeconomic context and its influence on intermediary determinants of child health: Evidence from Colombia. J. Biosoc. Sci. 2015, 47, 1–27. [Google Scholar] [CrossRef]
| Barisal | Chittagong | Dhaka | Khulna | Rajshahi | Rangpur | Sylhet | ||
|---|---|---|---|---|---|---|---|---|
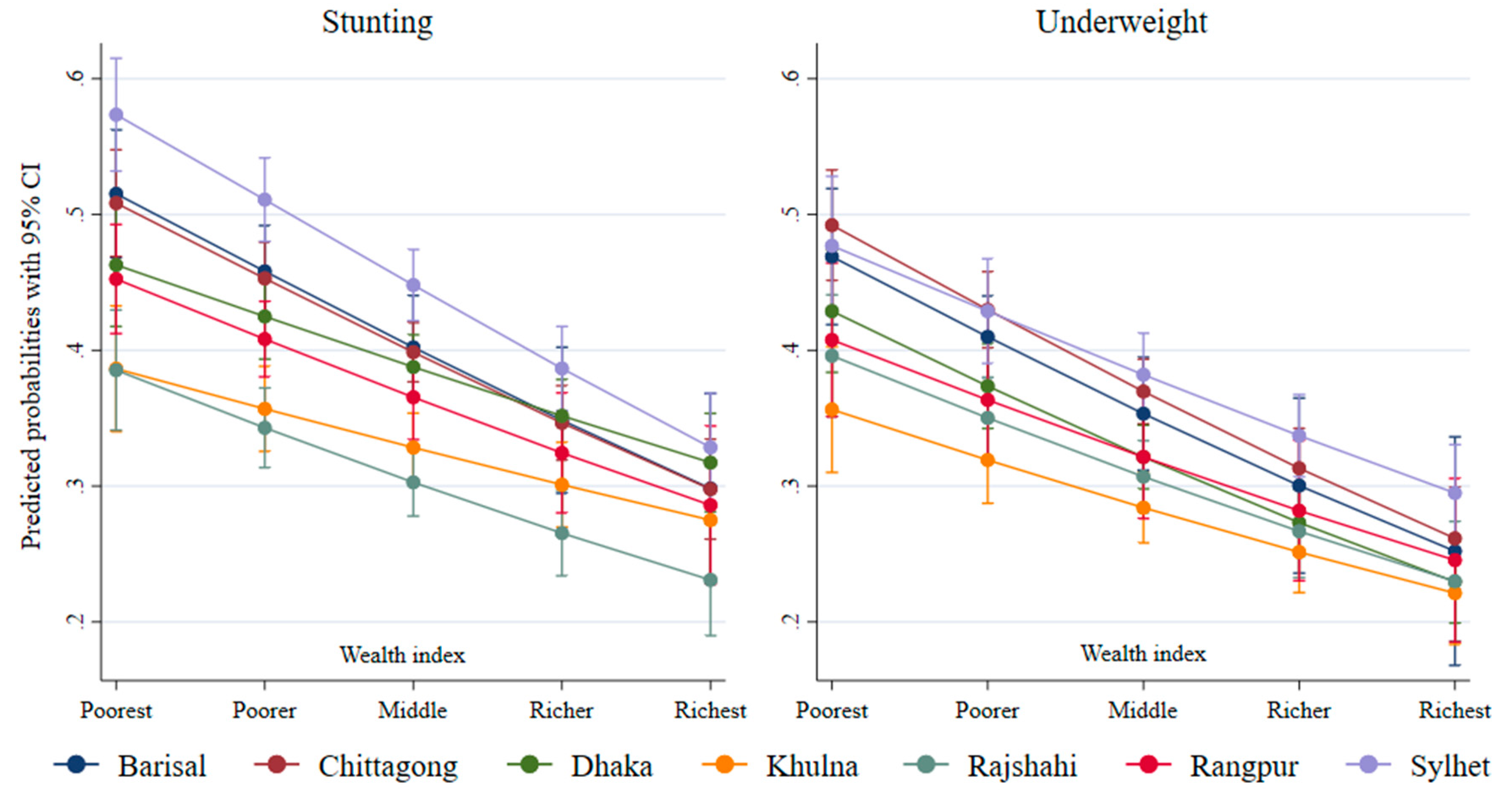
| Stunting | Overall | 0.42 | 0.40 | 0.39 | 0.31 | 0.33 | 0.40 | 0.50 |
| Wealth quintiles | ||||||||
| Poorest | 0.59 | 0.58 | 0.49 | 0.42 | 0.42 | 0.49 | 0.63 | |
| Poorer | 0.40 | 0.48 | 0.46 | 0.32 | 0.40 | 0.43 | 0.56 | |
| Middle | 0.41 | 0.39 | 0.41 | 0.32 | 0.31 | 0.37 | 0.49 | |
| Wealthier | 0.33 | 0.32 | 0.39 | 0.31 | 0.21 | 0.29 | 0.39 | |
| Wealthiest | 0.19 | 0.25 | 0.23 | 0.19 | 0.17 | 0.17 | 0.26 | |
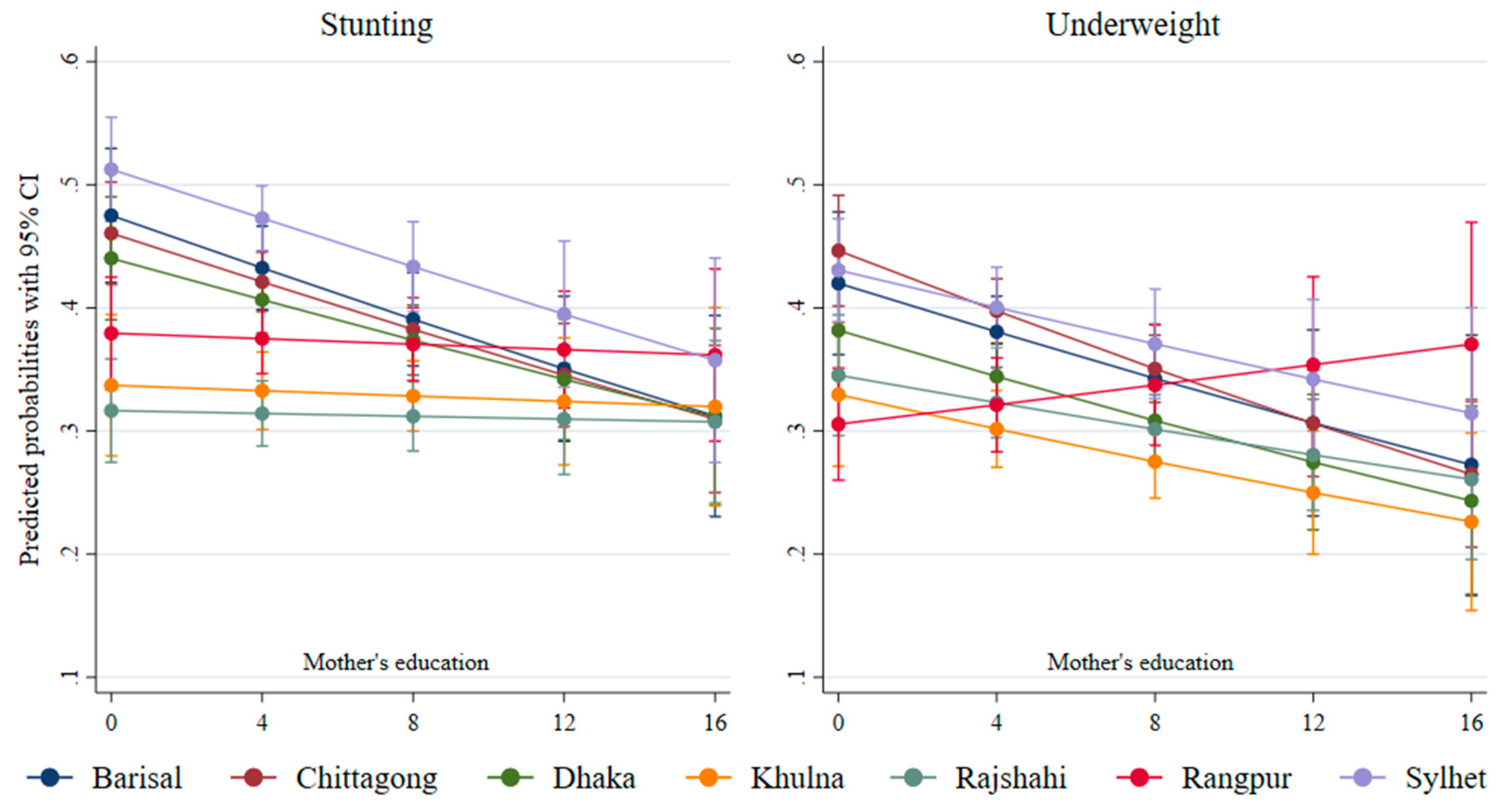
| Mother’s education | ||||||||
| No education | 0.57 | 0.52 | 0.49 | 0.45 | 0.40 | 0.42 | 0.60 | |
| Primary | 0.48 | 0.50 | 0.45 | 0.34 | 0.37 | 0.47 | 0.54 | |
| Secondary | 0.37 | 0.32 | 0.33 | 0.30 | 0.30 | 0.38 | 0.40 | |
| Higher | 0.29 | 0.24 | 0.20 | 0.20 | 0.16 | 0.20 | 0.15 | |
| Underweight | Overall | 0.38 | 0.37 | 0.32 | 0.27 | 0.33 | 0.36 | 0.42 |
| Wealth quintiles | ||||||||
| Poorest | 0.53 | 0.55 | 0.47 | 0.35 | 0.42 | 0.46 | 0.53 | |
| Poorer | 0.39 | 0.45 | 0.39 | 0.34 | 0.40 | 0.37 | 0.46 | |
| Middle | 0.34 | 0.37 | 0.32 | 0.29 | 0.34 | 0.29 | 0.43 | |
| Wealthier | 0.23 | 0.28 | 0.30 | 0.25 | 0.22 | 0.24 | 0.31 | |
| Wealthiest | 0.25 | 0.22 | 0.17 | 0.14 | 0.16 | 0.21 | 0.26 | |
| Mother’s education | ||||||||
| No education | 0.51 | 0.52 | 0.44 | 0.43 | 0.43 | 0.35 | 0.51 | |
| Primary | 0.45 | 0.45 | 0.37 | 0.33 | 0.41 | 0.43 | 0.45 | |
| Secondary | 0.33 | 0.29 | 0.26 | 0.25 | 0.27 | 0.35 | 0.35 | |
| Higher | 0.23 | 0.21 | 0.15 | 0.17 | 0.19 | 0.20 | 0.13 |
| Stunting | Underweight | |||
|---|---|---|---|---|
| Adjusted Odds Ratio | 95% Confidence Interval | Adjusted Odds Ratio | 95% Confidence Interval | |
| Region (Ref: Khulna) | ||||
| Barisal | 1.44 *** | (1.20–1.73) | 1.43 *** | (1.18–1.72) |
| Chittagong | 1.39 *** | (1.19–1.61) | 1.52 *** | (1.29–1.80) |
| Dhaka | 1.34 *** | (1.14–1.56) | 1.23 ** | (1.03–1.45) |
| Rajshahi | 0.89 | (0.75–1.06) | 1.12 | (0.93–1.34) |
| Rangpur | 1.20 ** | (1.02–1.42) | 1.19 | (0.93–1.51) |
| Sylhet | 1.80 *** | (1.52–2.11) | 1.59 *** | (1.31–1.94) |
| Wealth quintiles (Ref: Poorest) | ||||
| Poorer | 0.85 ** | (0.75–0.97) | 0.81 *** | (0.71–0.93) |
| Middle | 0.74 *** | (0.65–0.85) | 0.67 *** | (0.59–0.77) |
| Wealthier | 0.63 *** | (0.54–0.73) | 0.53 *** | (0.45–0.61) |
| Wealthiest | 0.40 *** | (0.33–0.49) | 0.38 *** | (0.32–0.45) |
| Mother’s education (years) | 0.97 *** | (0.95–0.99) | 0.97 *** | (0.95–0.99) |
| Father’s education (years) | 0.96 *** | (0.95–0.98) | 0.97 *** | (0.96–0.99) |
| Mother’s age | 0.97 *** | (0.95–0.98) | 0.98 *** | (0.97–0.99) |
| Rural (Ref: Urban) | 0.83 *** | (0.73–0.95) | 0.98 | (0.87–1.10) |
| Child’s gender (Ref: Male) | 0.99 | (0.91–1.08) | 1.12 ** | (1.02–1.22) |
| Age of child (months) | 1.02 *** | (1.02–1.02) | 1.02 *** | (1.02–1.02) |
| Twin child (Ref: No) | 1.84 *** | (1.21–2.80) | 1.96 *** | (1.27–3.02) |
| Birth order | 1.09 ** | (1.01–1.17) | 1.09 ** | (1.01–1.18) |
| Number of children | 1.04 | (0.96–1.13) | 0.97 | (0.88–1.06) |
| Year—2014 (Ref: 2011) | 0.85 *** | (0.77–0.93) | 0.91 * | (0.81–1.01) |
| Observations | 14,602 | |||
| Stunting | 95% Confidence Interval | Underweight | 95% Confidence Interval | |
|---|---|---|---|---|
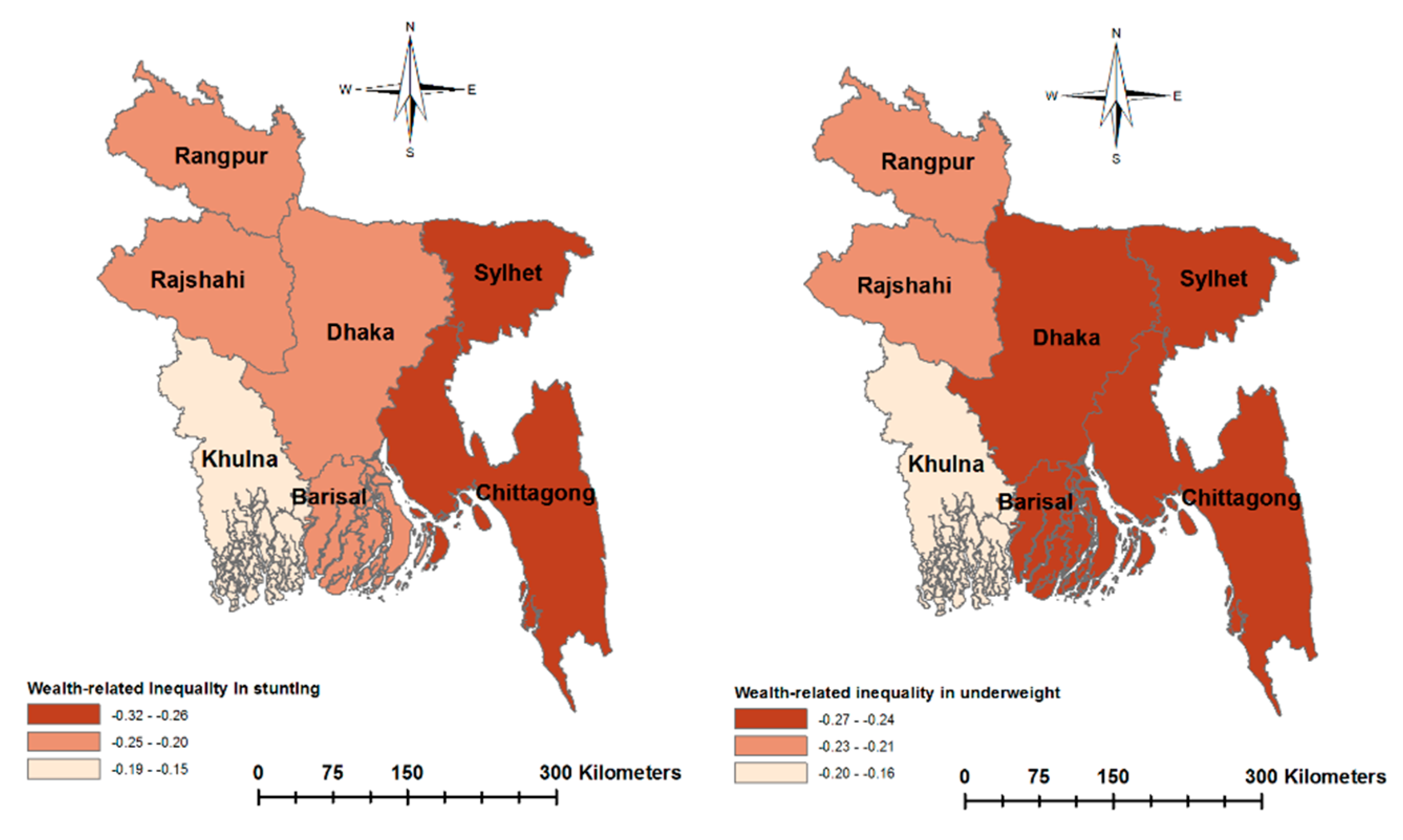
| Wealth-related inequality | ||||
| CI | −0.147 *** | (−0.163, −0.131) | −0.172 *** | (−0.191, −0.154) |
| WI | −0.240 *** | (−0.266, −0.215) | −0.263 *** | (−0.292, −0.235) |
| EI | −0.228 *** | (−0.253, −0.204) | −0.238 *** | (−0.264, −0.212) |
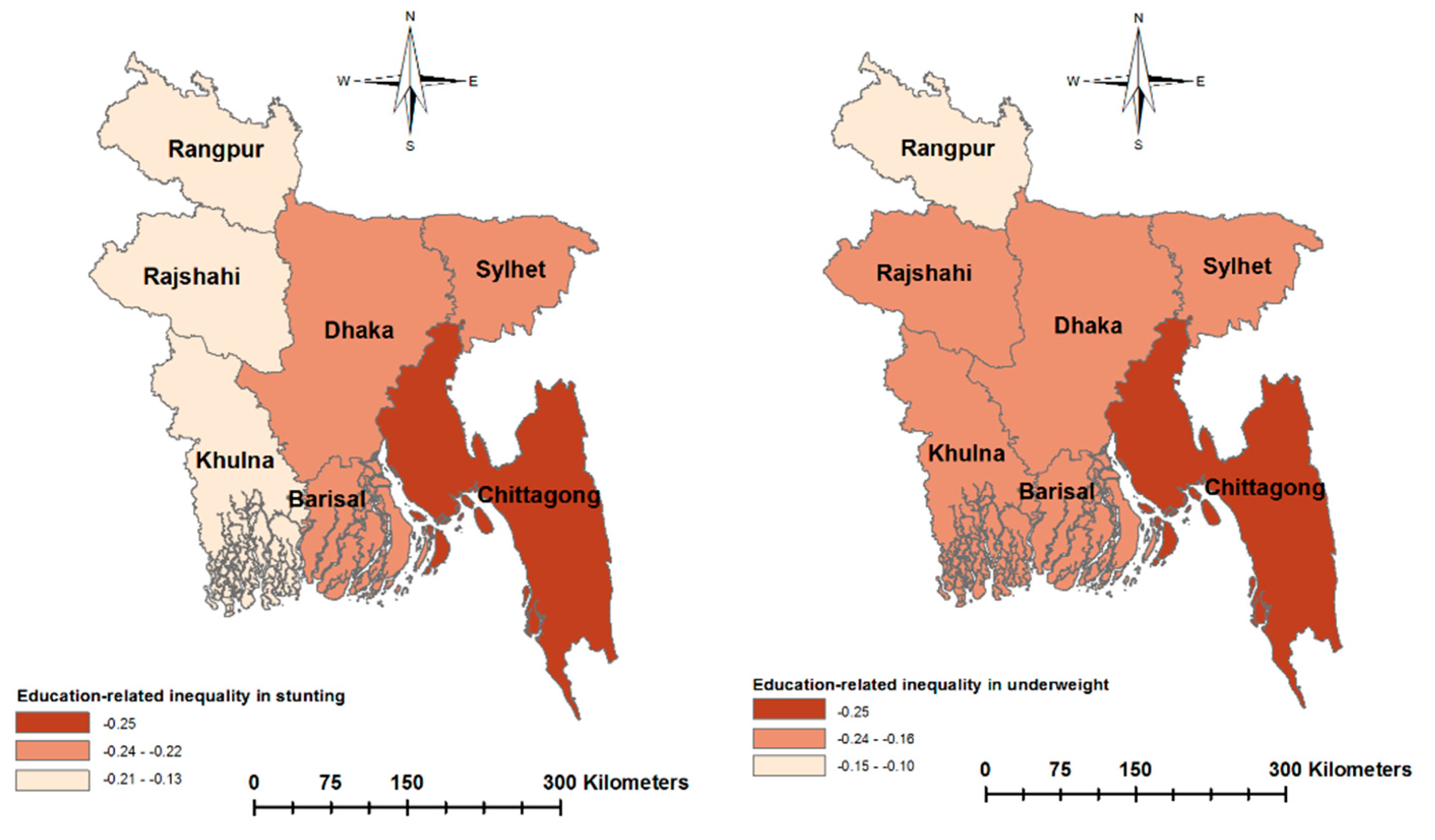
| Education-related inequality | ||||
| CI | −0.139 *** | (−0.154, −0.124) | −0.148 *** | (−0.166,−0.129) |
| WI | −0.227 *** | (−0.251, −0.202) | −0.225 *** | (−0.254, −0.197) |
| EI | −0.215 *** | (−0.239, −0.192) | −0.204 *** | (−0.229, −0.178) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hasan, M.M.; Uddin, J.; Pulok, M.H.; Zaman, N.; Hajizadeh, M. Socioeconomic Inequalities in Child Malnutrition in Bangladesh: Do They Differ by Region? Int. J. Environ. Res. Public Health 2020, 17, 1079. https://doi.org/10.3390/ijerph17031079
Hasan MM, Uddin J, Pulok MH, Zaman N, Hajizadeh M. Socioeconomic Inequalities in Child Malnutrition in Bangladesh: Do They Differ by Region? International Journal of Environmental Research and Public Health. 2020; 17(3):1079. https://doi.org/10.3390/ijerph17031079
Chicago/Turabian StyleHasan, Mohammad Monirul, Jalal Uddin, Mohammad Habibullah Pulok, Nabila Zaman, and Mohammad Hajizadeh. 2020. "Socioeconomic Inequalities in Child Malnutrition in Bangladesh: Do They Differ by Region?" International Journal of Environmental Research and Public Health 17, no. 3: 1079. https://doi.org/10.3390/ijerph17031079
APA StyleHasan, M. M., Uddin, J., Pulok, M. H., Zaman, N., & Hajizadeh, M. (2020). Socioeconomic Inequalities in Child Malnutrition in Bangladesh: Do They Differ by Region? International Journal of Environmental Research and Public Health, 17(3), 1079. https://doi.org/10.3390/ijerph17031079






