Promotion of Elementary School Students’ Health Literacy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Physical Activity Program
2.3. Measures
2.4. Ethics
2.5. Statistical Analysis
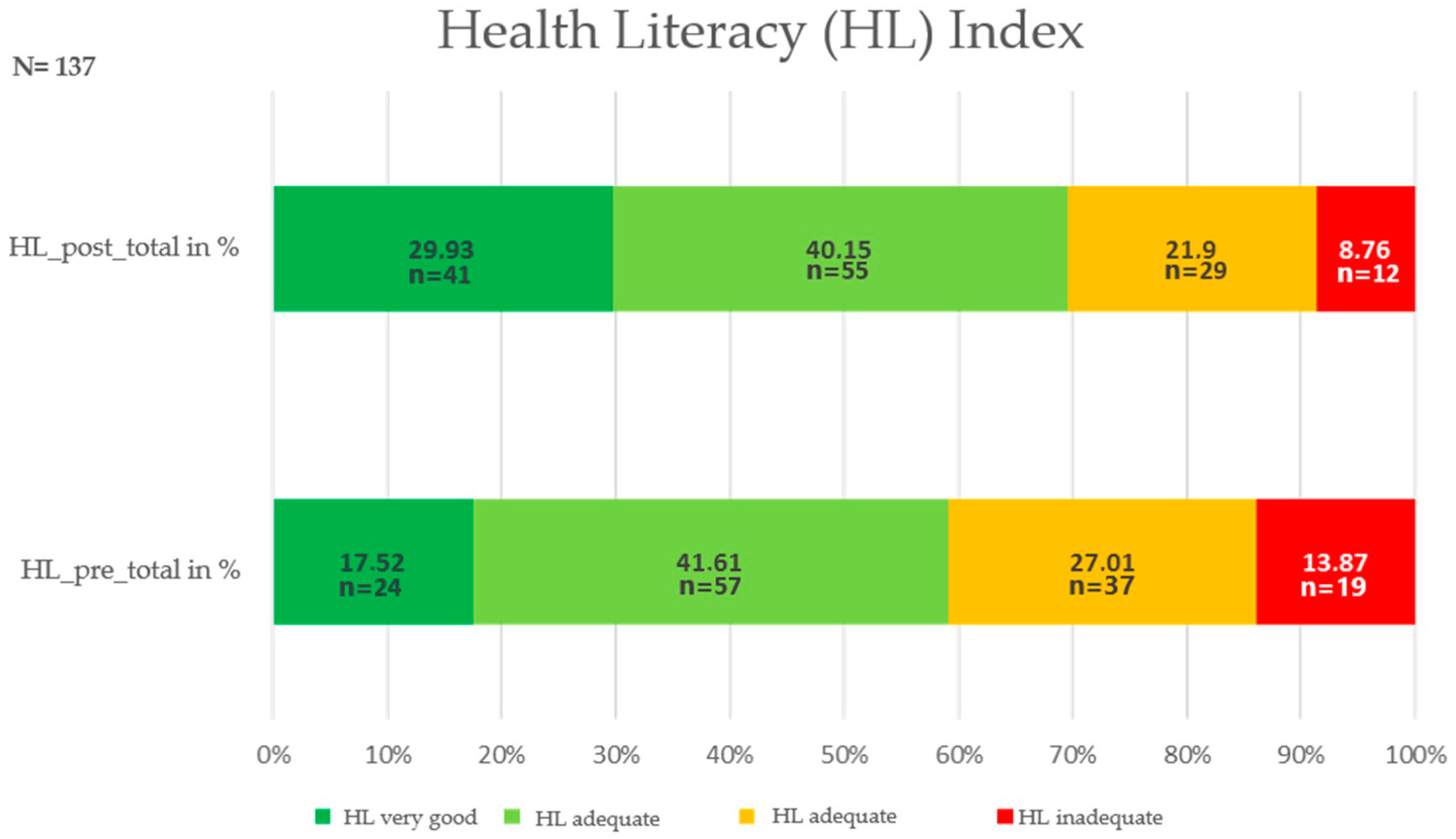
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Knisel, E.; Kleiner, K.; Bronikowski, M.; González Gross, M.; Parry Martínková, I.; Erdmann, R. Health Promotion at School: Pedagogical Aspects and Practical Implications; De Gruyter Open: Warsaw, Poland, 2017; p. ix. [Google Scholar] [CrossRef]
- Töpfer, C. Sportbezogene Gesundheitskompetenz: Kompetenzmodellierung und Testentwicklung für den Sportunterricht; [Sport-Related Health Competence: A Competence Model and Test Instrument for Physical Education]. Ph.D. Thesis, Friedrich-Alexander-Universität Erlangen-Nürnberg, Erlangen, Germany, 2017. [Google Scholar]
- Bollweg, T.M.; Okan, O. Measuring children’s health literacy. Current approaches and challenges. In International Handbook of Health Literacy. Research, Practice and Policy Across the Life-Span; Okan, O., Bauer, U., Levin-Zamir, D., Pinheiro, P., Sørensen, K., Eds.; Policy Press: Bristol, UK, 2019; ISBN 978-1-4473-4452-0. [Google Scholar]
- LeBlanc, A.G.; Katzmarzyk, P.T.; Barreira, T.V.; Broyles, S.T.; Chaput, J.-P.; Church, T.S.; Fogelholm, M.; Harrington, D.M.; Hu, G.; Kuriyan, R.; et al. Correlates of total sedentary time and screen time in 9–11 year-old children around the world: The International Study of Childhood Obesity, Lifestyle and the Environment. PLoS ONE 2015, 10, e0129622. [Google Scholar] [CrossRef] [PubMed]
- Borzekowski, D.L. Considering children and health literacy: A theoretical approach. Pediatrics 2009, 124 (Suppl. 3), 282–288. [Google Scholar] [CrossRef]
- Bröder, J.; Okan, O.; Bauer, U.; Bruland, D.; Schlupp, S.; Bollweg, T.M.; Saboga-Nunes, L.; Bond, E.; Sørensen, K.; Bitzer, E.-M.; et al. Health literacy in childhood and youth: A systematic review of definitions and models. BMC Public Health 2017, 17, 361. [Google Scholar] [CrossRef]
- Guo, S.; Armstrong, R.; Waters, E.; Sathish, T.; Alif, S.M.; Browne, G.R.; Yu, X. Quality of health literacy instruments used in children and adolescents: A systematic review. BMJ Open 2018, 8, e020080. [Google Scholar] [CrossRef] [PubMed]
- Malloy-Weir, L.J.; Charles, C.; Gafni, A.; Entwistle, V. A review of health literacy: Definitions, interpretations, and implications for policy initiatives. J. Public Health Policy 2016, 37, 334–352. [Google Scholar] [CrossRef]
- Okan, O.; Pinheiro, P.; Zamora, P.; Bauer, U. Health literacy bei Kindern und Jugendlichen. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz 2015, 58. [Google Scholar] [CrossRef]
- Saboga-nunes, L.; Bittlingmayer, U.; Okan, O. Salutogenesis and health literacy: The health promotion simplex! In International Handbook of Health Literacy. Research, Practice and Policy Across the Life-Span.; Okan, O., Bauer, U., Levin-Zamir, D., Pinheiro, P., Sørensen, K., Eds.; Policy Press: Bristol, UK, 2019; pp. 649–664. ISBN 978-1-4473-4452-0. [Google Scholar]
- Demetriou, Y.; Sudeck, G.; Thiel, A.; Höner, O. The effects of school-based physical activity interventions on students’ health-related fitness knowledge: A systematic review. Educ. Res. Rev. 2015, 16, 19–40. [Google Scholar] [CrossRef]
- Linnebur, L.A.; Linnebur, S.A. Self-administered assessment of health literacy in adolescents using the newest Vital Sign. Health Promot. Pract. 2018, 19, 119–124. [Google Scholar] [CrossRef]
- Paakkari, L.; Paakkari, O. Health literacy as a learning outcome in schools. Health Educ. 2012, 112, 133–152. [Google Scholar] [CrossRef]
- Sørensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Consortium Health Literacy Project European. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef]
- Sørensen, K.; Van den Broucke, S.; Pelikan, J.M.; Fullam, J.; Doyle, G.; Slonska, Z.; Kondilis, B.; Stoffels, V.; Osborne, R.H.; Brand, H. Measuring health literacy in populations: Illuminating the design and development process of the European Health Literacy Survey Questionnaire (HLS-EU-Q). BMC Public Health 2013, 13, 948. [Google Scholar] [CrossRef]
- Van den Broucke, S. Health literacy: A critical concept for public health. Arch. Public Health 2014, 72, 10. [Google Scholar] [CrossRef]
- Rubene, Z.; Stars, I.; Goba, L. Health literate child: Transforming teaching in school health education. Soc. Integr. Educ. 2015, 1, 10. [Google Scholar] [CrossRef][Green Version]
- Nutbeam, D. Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promot. Int. 2000, 15, 259–267. [Google Scholar] [CrossRef]
- Bruselius-Jensen, M.; Høstgaard Bonde, A.H.; Hellesøe Christensen, J.H. Promoting health literacy in the classroom. Health Educ. J. 2016, 76, 156–168. [Google Scholar] [CrossRef]
- Aghazadeh, S.A.; Aldoory, L. ‘Health literacy for all’: Exploring the feasibility of an intervention to reduce health disparities among rural children. J. Appl. Commun. Res. 2020, 48, 478–495. [Google Scholar] [CrossRef]
- Manganello, J.A. Health literacy and adolescents: A framework and agenda for future research. Health Educ. Res. 2008, 23, 840–847. [Google Scholar] [CrossRef]
- Paakkari, L.; Torppa, M.; Mazur, J.; Boberova, Z.; Sudeck, G.; Kalman, M.; Paakkari, O. A Comparative Study on Adolescents’ Health Literacy in Europe: Findings from the HBSC Study. Int. J. Environ. Res. Public Health 2020, 17, 3543. [Google Scholar] [CrossRef]
- Sukys, S.; Trinkuniene, L.; Tilindiene, I. Subjective Health Literacy among School-Aged Children: First Evidence from Lithuania. Int. J. Environ. Res. Public Health 2019, 16, 3397. [Google Scholar] [CrossRef]
- Paakkari, L.; Kokko, S.; Villberg, J.; Paakkari, O.; Tynjälä, J. Health literacy and participation in sports club activities among adolescents. Scand. J. Public Health 2017, 45, 854–860. [Google Scholar] [CrossRef]
- Okan, O.; Bollweg, T.M. Development process of a health literacy measurement instrument for fourth grade schoolchildren. A mixed-method study. In Health Literacy Across the Life Span; Mayer, A.-K., Ed.; Pabst Science Publisher: Lengerich, Germany, 2018; pp. 87–110. ISBN 978-3-95853-449-0. [Google Scholar]
- Ormshaw, M.; Paakkari, L.; Kannas, L. Measuring child and adolescent health literacy: A systematic review of literature. Health Educ. 2013, 113. [Google Scholar] [CrossRef]
- Perry, E.L. Health literacy in adolescents: An integrative review. J. Spec. Pediatr. Nurs. 2014, 19, 210–218. [Google Scholar] [CrossRef] [PubMed]
- Weiss, B.D.; Mays, M.Z.; Martz, W.; Castro, K.M.; DeWalt, D.A.; Pignone, M.P.; Mockbee, J.; Hale, F.A. Quick assessment of literacy in primary care: The newest vital sign. Ann. Fam. Med. 2005, 3, 514–522. [Google Scholar] [CrossRef] [PubMed]
- Fretian, A.; Bollweg, T.M.; Okan, O.; Pinheiro, P.; Bauer, U. Exploring Associated Factors of Subjective Health Literacy in School-Aged Children. Int. J. Environ. Res. Public Health 2020, 17, 1720. [Google Scholar] [CrossRef]
- Bollweg, T.M.; Okan, O.; Fretian, A.; Bröder, J.; Domanska, O.; Jordan, S.; Bruland, D.; Pinheiro, P.; Bauer, U. Adapting the European Health Literacy Survey Questionnaire for Fourth-Grade Students in Germany: Validation and Psychometric Analysis. Health Lit. Res. Pract. 2020, 4, e144–e159. [Google Scholar] [CrossRef]
- Diamond, C.; Saintonge, S.; August, P.; Azrack, A. The development of Building Wellness™, a Youth health literacy program. J. Health Commun. 2011, 16 (Suppl. 3), 103–118. [Google Scholar] [CrossRef]
- Robinson, L.; Calmes, D.; Bazargan, M. The impact of literacy enhancement on asthma-related outcomes among underserved children. J. Natl. Med. Assoc. 2008, 100, 892–896. [Google Scholar] [CrossRef]
- Franze, M.; Fendrich, K.; Schmidt, C.; Ruth, A.; Fahland, J.; René, T.; Plachta-Danielzik, S.; Seiberl, J.; Hoffmann, W.; Splieth, C.; et al. Implementation and evaluation of the population-based programme “Health Literacy in School-aged Children” (GeKo KidS). J. Public Health 2011, 19, 339–347. [Google Scholar] [CrossRef][Green Version]
- Schmidt, C.O.; Fahland, R.A.; Franze, M.; Splieth, C.; Thyrian, J.R.; Plachta-Danielzik, S.; Hoffmann, W.; Kohlmann, T. Health-related behaviour, knowledge, attitudes, communication and social status in school children in Eastern Germany. Health Educ. Res. 2010, 25, 542–551. [Google Scholar] [CrossRef]
- Deal, T.B.; Jenkins, J.M.; Deal, L.O.; Byra, A. The impact of professional development to infuse health and reading in elementary schools. Am. J. Health Educ. 2010, 41, 155–166. [Google Scholar] [CrossRef]
- Okan, O. Gesundheitskompetenz im Kindes- und Jugendalter: Bestandsaufnahme und Analyse der konzeptionellen und Methodischen Erforschung. Ph.D. Thesis, Universität Bielefeld, Bielefeld, Germany, 2019. [Google Scholar] [CrossRef]
- Lee, A. Health-promoting schools: Evidence for a holistic approach to promoting health and improving health literacy. Appl. Health Econ. Health Policy 2009, 7, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Okan, O.; Lopes, E.; Bollweg, T.M.; Bröder, J.; Messer, M.; Bruland, D.; Bond, E.; Carvalho, G.S.; Sørensen, K.; Saboga-Nunes, L.; et al. Generic health literacy measurement instruments for children and adolescents: A systematic review of the literature. BMC Public Health 2017, 18, 166. [Google Scholar] [CrossRef] [PubMed]
- Bollweg, T.M.; Okan, O. Gesundheitskompetenz messen bei Kindern: Aktuelle Ansätze und Herausforderungen. In Health Literacy im Kindes- und Jugendalter: Ein- und Ausblicke; Bollweg, T.M., Bröder, J., Pinheiro, P., Eds.; Springer Fachmedien: Wiesbaden, Germany, 2020; pp. 73–98. [Google Scholar]
- Woolson, R.F. Wilcoxon Signed-Rank Test. In Wiley Encyclopedia of Clinical Trials; Wiley Online Library: Hoboken, NJ, USA, 2008; pp. 1–3. [Google Scholar] [CrossRef]
- Cohen, J. Statistical power analysis. Curr. Dir. Psychol. Sci. 1992, 1, 98–101. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; L. Erlbaum Associates: Hillsdale, NJ, USA, 1988; ISBN 0-8058-0283-5. [Google Scholar]
- Sørensen, K.; Pelikan, J.M.; Röthlin, F.; Ganahl, K.; Slonska, Z.; Doyle, G.; Fullam, J.; Kondilis, B.; Agrafiotis, D.; Uiters, E.; et al. Health literacy in Europe: Comparative results of the European Health Literacy Survey (HLS-EU). Eur. J. Public Health 2015, 25, 1053–1058. [Google Scholar] [CrossRef]
- Brown, S.L.; Teufel, J.A.; Birch, D.A. Early adolescents perceptions of health and health literacy. J. Sch. Health 2007, 77, 7–15. [Google Scholar] [CrossRef]
- St. Leger, L.; Nutbeam, D. Research into health promotings Schools. J. Sch. Health 2000, 70, 257. [Google Scholar] [CrossRef]
- Paakkari, L.; Okan, O. Health literacy—Talking the language of (school) education. HLRP Health Lit. Res. Pract. 2019, 3, e161–e164. [Google Scholar] [CrossRef]
- Antonovsky, A. The salutogenic model as a theory to guide health promotion. Health Promot. Int. 1996, 11, 11–18. [Google Scholar] [CrossRef]
- McCuaig, L.; Quennerstedt, M.; Macdonald, D. A salutogenic, strengths-based approach as a theory to guide HPE curriculum change. Asia-Pac. J. HealthSport Phys. Educ. 2013, 4, 109–125. [Google Scholar] [CrossRef]
- Saboga-Nunes, L.; Bittlingmayer, U.H.; Okan, O. Salutogenesis and health literacy: The health promotion simplex! In International Handbook of Health Literacy; Policy Press: Bristol, UK, 2019; pp. 649–664. ISBN 978-1-4473-4451-3. [Google Scholar]
- Bhagat, K.; Howard, D.E.; Aldoory, L. The relationship between health literacy and health conceptualizations: An exploratory study of elementary school-aged children. Health Commun. 2018, 33, 131–138. [Google Scholar] [CrossRef]
- Pulgarón, E.R.; Sanders, L.M.; Patiño-Fernandez, A.M.; Wile, D.; Sanchez, J.; Rothman, R.L.; Delamater, A.M. Glycemic control in young children with diabetes: The role of parental health literacy. Patient Educ. Couns. 2014, 94, 67–70. [Google Scholar] [CrossRef] [PubMed]
- Sanders, L.M.; Shaw, J.S.; Guez, G.; Baur, C.; Rudd, R. Literacy and child health: A sysetmatic review. Pediatrics 2009, 124 (Suppl. 3), 306–314. [Google Scholar] [CrossRef]
- DeWalt, D.A.; Berkman, N.D.; Sheridan, S.; Lohr, K.N.; Michael, P.; Pignone, M.P. Literacy and health outcomes. J. Gen. Intern. Med. 2004, 19, 1228–1239. [Google Scholar] [CrossRef] [PubMed]
- Kumar, D.; Sanders, L.; Perrin, E.M.; Lokker, N.; Patterson, B.; Gunn, V.; Finkle, J.; Franco, V.; Choi, L.; Rothman, R.L. Parental understanding of infant health information: Health literacy, numeracy, and the Parental Health Literacy Activities Test (PHLAT). Acad. Pediatrics 2010, 10, 309–316. [Google Scholar] [CrossRef] [PubMed]
- DeWalt, D.A.; Hink, A. Health literacy and child health outcomes: A systematic review of the literature. Pediatrics 2009, 124 (Suppl. 3), S265–S274. [Google Scholar] [CrossRef]
- Yu, X.; Yang, T.; Wang, S.; Zhang, X. Study on student health literacy gained through health education in elementary and middle schools in China. Health Educ. J. 2012, 71, 452–460. [Google Scholar] [CrossRef]
- Brozo, W.G.; Sulkunen, S.; Shiel, G.; Garbe, C.; Pandian, A.; Valtin, R. Reading, gender, and engagement: Lessons from five PISA countries. J. Adolesc. Adult Lit. 2014, 57, 584–593. [Google Scholar] [CrossRef]
- Organisation for Economic Co-operation and Development. PISA 2009 Results: Overcoming Social Background: Equity in Learning Opportunities and Outcomes (Volume II); OECD Publishing: Paris, France, 2010. [Google Scholar] [CrossRef]
- Klecker, B.M. The ”Gender Gap” in NAEP Fourth-, Eighth-, and Twelfth-Grade Reading Scores Across Years; Online Submission; ERIC: Morehead, KY, USA, 2005.
- Driessnack, M.; Chung, S.; Perkhounkova, E.; Hein, M. Using the “Newest Vital Sign” to assess health literacy in children. J. Pediatric Health Care 2014, 28, 165–171. [Google Scholar] [CrossRef]
- Kraft, M.A. Interpreting effect sizes of education interventions. Educ. Res. 2020, 49, 241–253. [Google Scholar] [CrossRef]
- Latkin, C.A.; Edwards, C.; Davey-Rothwell, M.A.; Tobin, K.E. The relationship between social desirability bias and self-reports of health, substance use, and social network factors among urban substance users in Baltimore, Maryland. Addict. Behav. 2017, 73, 133–136. [Google Scholar] [CrossRef]
- Lane, H.G.; Aldoory, L. Recommendations for measurement of child health literacy: A Pragmatic Approach. HLRP Health Lit. Res. Pract. 2019, 3, e165–e169. [Google Scholar] [CrossRef] [PubMed]
| All | Girls | Boys | First/Second Graders | Third and Fourth Graders |
|---|---|---|---|---|
| Mpre = 3.04 | Mpre = 3.01 | Mpre = 3.06 | Mpre = 2.93 | Mpre = 3.21 |
| SD = 0.48 | SD = 0.43 | SD = 0.51 | SD = 0.48 | SD = 0.41 |
| Mpost = 3.22 | Mpost = 3.21 | Mpost = 3.21 | Mpost = 3.1 | Mpost = 3.4 |
| SD = 0.49 | SD = 0.47 | SD = 0.51 | SD = 0.49 | SD = 0.44 |
| z = 4.929 | z = −3.214 | z = −3.734 | z = −3.69 | z = 3.26 |
| p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 |
| n = 137 | n = 57 | n = 80 | n = 83 | n = 54 |
| Health Care | Disease Prevention | Health Promotion |
|---|---|---|
| Mpre = 2.95 | Mpre = 3.04 | Mpre = 3.12 |
| SD = 0.57 | SD = 0.69 | SD = 0.48 |
| Mpost = 3.12 | Mpost = 3.26 | Mpost = 3.27 |
| SD = 0.6 | SD = 0.62 | SD = 0.5 |
| z = 3.45 | z = 4.22 | z = 3.71 |
| p = 0.001 | p < 0.001 | p < 0.001 |
| r = 0.32 | r = 0.36 | r = 0.32 |
| n = 137 | n = 137 | n = 137 |
| Access | Understanding | Appraising | Applying |
|---|---|---|---|
| Mpre = 2.99 | Mpre = 3.0 | Mpre = 2.9 | Mpre = 3.22 |
| SD = 0.52 | SD = 0.64 | SD = 0.82 | SD = 0.58 |
| Mpost = 3.24 | Mpost = 3.14 | Mpost = 3.0 | Mpost = 3.37 |
| SD = 0.56 | SD = 0.54 | SD = 0.86 | SD = 0.59 |
| z = 5.02 | z = 2.769 | z = 1.16 | z = 2.809 |
| p = 0.000 | p = 0.006 | p = 0.245 | p = 0.005 |
| r = 0.43 | r = 0.24 | r = 0.1 | r = 0.24 |
| n = 137 | n = 137 | n = 137 | n = 137 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Knisel, E.; Rupprich, H.; Wunram, A.; Bremer, M.; Desaive, C. Promotion of Elementary School Students’ Health Literacy. Int. J. Environ. Res. Public Health 2020, 17, 9560. https://doi.org/10.3390/ijerph17249560
Knisel E, Rupprich H, Wunram A, Bremer M, Desaive C. Promotion of Elementary School Students’ Health Literacy. International Journal of Environmental Research and Public Health. 2020; 17(24):9560. https://doi.org/10.3390/ijerph17249560
Chicago/Turabian StyleKnisel, Elke, Helge Rupprich, Annika Wunram, Markus Bremer, and Christiane Desaive. 2020. "Promotion of Elementary School Students’ Health Literacy" International Journal of Environmental Research and Public Health 17, no. 24: 9560. https://doi.org/10.3390/ijerph17249560
APA StyleKnisel, E., Rupprich, H., Wunram, A., Bremer, M., & Desaive, C. (2020). Promotion of Elementary School Students’ Health Literacy. International Journal of Environmental Research and Public Health, 17(24), 9560. https://doi.org/10.3390/ijerph17249560





