Rise and Recharge: Effects on Activity Outcomes of an e-Health Smartphone Intervention to Reduce Office Workers’ Sitting Time
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Recruitment of Organisations
2.3. Recruitment of Office Workers
2.4. Eligibility and Selection
2.5. Intervention
2.5.1. Theoretical Basis and Intervention Development
2.5.2. Group Allocation and Application Installation
2.5.3. Intervention Application
2.6. Data Collection
2.7. Outcomes
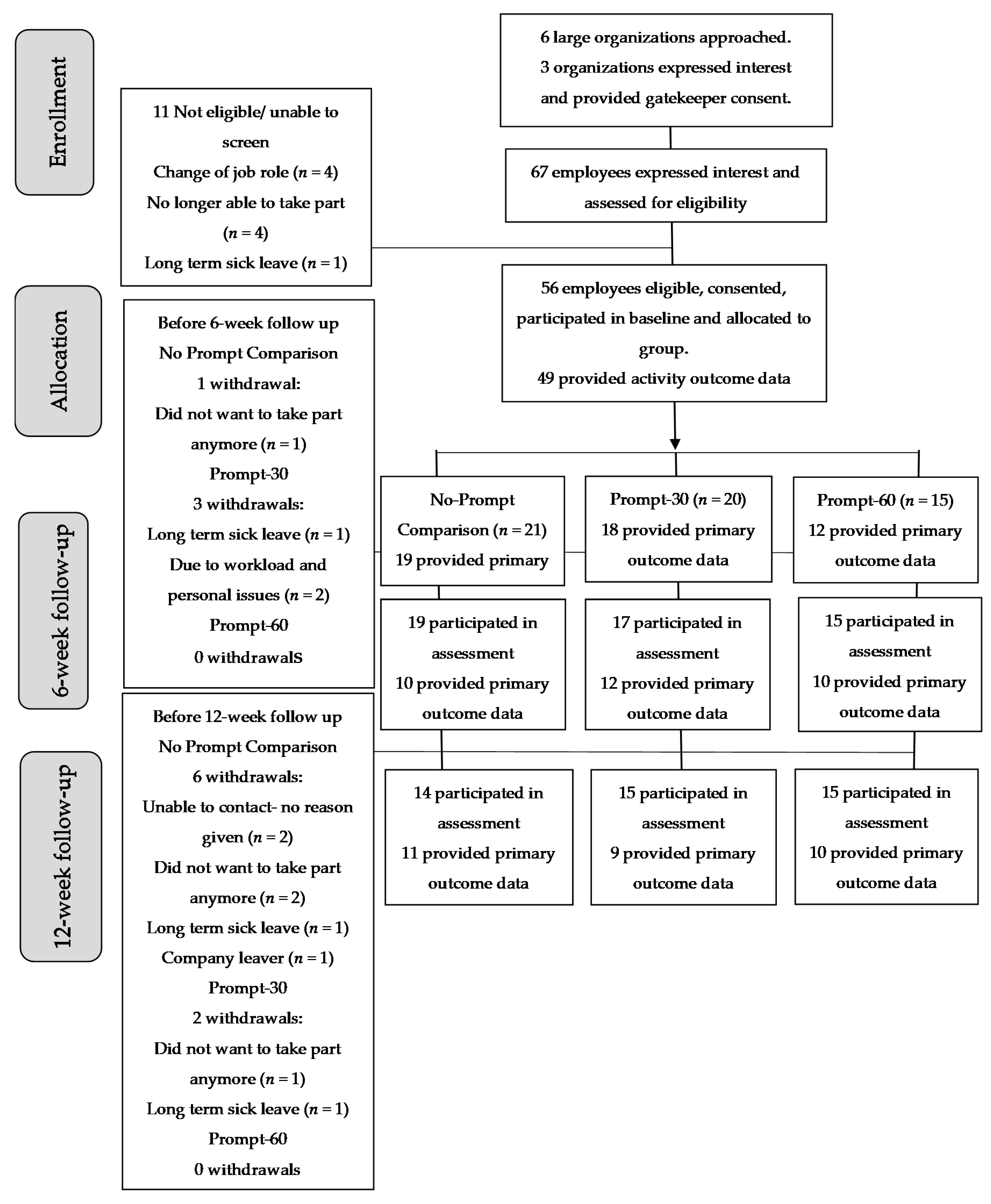
Recruitment, Retention and Attrition
2.8. Behavioural Outcomes
2.8.1. Sitting, Standing and Moving Time
2.8.2. Anthropometry: Stature, Body Mass and Body Composition
2.8.3. Cardiometabolic Markers
2.8.4. Survey Measures and Outcomes
2.9. Analyses
2.9.1. Behavioural Outcomes
2.9.2. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Behavioural Outcomes
3.3. Secondary Outcomes
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Patterson, R.; McNamara, E.; Tainio, M.; de Sá, T.H.; Smith, A.D.; Sharp, S.J.; Edwards, P.; Woodcock, J.; Brage, S.; Wijndaele, K. Sedentary Behaviour and Risk of All-Cause, Cardiovascular and Cancer Mortality, and Incident Type 2 Diabetes: A Systematic Review and Dose Response Meta-Analysis; Springer: Berlin/Heidelberg, Germany, 2018; pp. 811–829. [Google Scholar]
- Gov.UK. Physical Activity Guidelines: UK Chief Medical Officers’ Report; Department of Health and Social Care: London, UK, 2019. [Google Scholar]
- Ryan, C.G.; Dall, P.M.; Granat, M.H.; Grant, P.M. Sitting patterns at work: Objective measurement of adherence to current recommendations. Ergonomics 2011, 54, 531–538. [Google Scholar] [CrossRef]
- World Health Organization. World Health Organisation Global Strategy on Diet, Physical Activity and Health. Global Recommendations on Physical Activity for Health; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Clemes, S.A.; O’Connell, S.E.; Edwardson, C.L. Office workers’ objectively measured sedentary behaviour and physical activity during and outside work hours. J. Occup. Environ. Med. 2014, 56, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Coenen, P.; Willenberg, L.; Parry, S.; Shi, J.W.; Romero, L.; Blackwood, D.M.; Maher, C.G.; Healy, G.N.; Dunstan, D.W.; Straker, L.M. Associations of occupational standing with musculoskeletal symptoms: A systematic review with meta-analysis. Br. J. Sports Med. 2016, 52, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Thorp, A.A.; Kingwell, B.A.; Owen, N.; Dunstan, D.W. Breaking up workplace sitting time with intermittent standing bouts improves fatigue and musculoskeletal discomfort in overweight/obese office workers. Occup. Environ. Med. 2014, 71, 765–771. [Google Scholar] [CrossRef]
- Healy, G.N.; Dunstan, D.W.; Salmon, J.; Cerin, C.; Shaw, J.; Zimmet, P. Breaks in sedentary time: Beneficial association with metabolic risk. Diabetes Care 2008, 31, 661–666. [Google Scholar] [CrossRef]
- Bellettiere, J.; Carlson, J.A.; Rosenberg, D.; Singhania, A.; Natarajan, L.; Berardi, V.; LaCroix, A.Z.; Sears, D.D.; Moran, K.; Crist, K. Gender and age differences in hourly and daily patterns of sedentary time in older adults living in retirement communities. PLoS ONE 2015, 10, e0136161. [Google Scholar] [CrossRef]
- Carter, S.E.; Draijer, R.; Holder, S.M.; Brown, L.; Thijssen, D.H.; Hopkins, N.D. Regular walking breaks prevent the decline in cerebral blood flow associated with prolonged sitting. J. Appl. Physiol. 2018, 125, 790–798. [Google Scholar] [CrossRef]
- Brakenridge, C.; Chong, Y.Y.; Winkler, E.A.H.; Hadgraft, N.; Fjeldsoe, B.; Johnston, V.; Straker, L.; Healy, G.; Clark, B.J. Evaluating short-term musculoskeletal pain changes in desk-based workers receiving a workplace sitting-reduction intervention. Int. J. Environ. Res. Public Health 2018, 15, 1975. [Google Scholar] [CrossRef]
- Benatti, F.; Larsden, S.; Kofoed, K.; Nielsen, S.; Harder-Lauridsen, N.; Lyngbæk, M.; Eriksen, D.; Karstoft, K.; Krogh-Madsen, R.; Pedersen, B. Intermittent standing but not a moderate exercise bout reduces postprandial glycemia. Med. Sci. Sports Exerc. 2017, 49, 2305–2314. [Google Scholar] [CrossRef]
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.F.M.; Altenburg, T.M.; Chinapaw, M.J.M.; Altenburg, T.M.; et al. Sedentary Behavior Research Network (SBRN)—Terminology Consensus Project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 75. [Google Scholar] [CrossRef]
- Edwardson, C.L.; Yates, T.; Biddle, S.J.; Davies, M.J.; Dunstan, D.W.; Esliger, D.W.; Gray, L.J.; Jackson, B.; O’Connell, S.E.; Waheed, G. Effectiveness of the Stand More AT (SMArT) Work intervention: Cluster randomised controlled trial. BMJ 2018, 363, k3870. [Google Scholar] [CrossRef] [PubMed]
- Healy, G.N.; Eakin, E.G.; Owen, N.; LaMontagne, A.D.; Moodie, M.; Winkler, E.; Fjeldsoe, B.; Wiesner, G.; Willenberg, L.; Dunstan, D.W. A Cluster Randomised Controlled Trial to Reduce Office Workers’ Sitting Time: Impact on Activity Outcomes. Med. Sci. Sports Exerc. 2016, 48, 1787–1797. [Google Scholar] [CrossRef] [PubMed]
- Mackenzie, K.; Goyder, E.; Eves, F. Acceptability and feasibility of a low-cost, theory-based and co-produced intervention to reduce workplace sitting time in desk-based university employees. BMC Public Health 2015, 15, 1294. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, N.; Kukkonen-Harjula, K.T.; Verbeek, J.H.; Ijaz, S.; Hermans, V.; Pedisic, Z. Workplace interventions for reducing sitting at work. Cochrane Database Syst. Rev. 2018, 20. [Google Scholar] [CrossRef]
- Bort-Roig, J.; Chirveches-Perez, E.; Gine-Garriga, M.; Navarro-Blasco, L.; Bausa-Peris, R.; Iturrioz-Rosell, P.; Gonzalez-suarez, A.M.; Martinez-Lemos, I.; Puigoriol-Juvanteny, E.; Dowd, K. An m-health workplace-based ‘sit less, move more’ program: Impact on employees’ sedentary and physical activity patterns. In Journal of Physical Activity and Health 2018; Human Kinetics Publisl Inc.: Champaign, IL, USA, 2018. [Google Scholar]
- Peachey, M.M.; Richardson, J.; Tang, A.V.; Haas, V.D.-B.; Gravesande, J. Environmental, behavioural and multicomponent interventions to reduce adults’ sitting time: A systematic review and meta-analysis. Br. J. Sports Med. 2020, 54, 315–325. [Google Scholar] [CrossRef] [PubMed]
- Gao, L.; Flego, A.; Dunstan, D.W.; Winkler, E.A.; Healy, G.N.; Eakin, E.G.; Willenberg, L.; Owen, N.; LaMontagne, A.D.; Lal, A. Economic evaluation of a randomized controlled trial of an intervention to reduce office workers’ sitting time: The’Stand Up Victoria’trial. Scand. J. Work Environ. Health 2018, 44, 503–511. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, A.; McDonough, S.M.; Murphy, M.H.; Nugent, C.D.; Mair, J.L. Using computer, mobile and wearable technology enhanced interventions to reduce sedentary behaviour: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 105. [Google Scholar] [CrossRef]
- Ofcom. Communications Market Report. Available online: https://www.ofcom.org.uk/__data/assets/pdf_file/0022/117256/CMR-2018-narrative-report.pdf (accessed on 6 June 2020).
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and evaluating complex interventions: The new Medical Research Council guidance. BMJ 2008, 337, a1655. [Google Scholar] [CrossRef]
- Moore, G.F.; Audrey, S.; Barker, M.; Bond, L.; Bonell, C.; Hardeman, W.; Moore, L.; O’Cathain, A.; Tinati, T.; Wight, D. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015, 350, h1258. [Google Scholar] [CrossRef]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014, 348, g1687. [Google Scholar] [CrossRef]
- Billingham, S.A.; Whitehead, A.L.; Julious, S.A. An audit of sample sizes for pilot and feasibility trials being undertaken in the United Kingdom registered in the United Kingdom Clinical Research Network database. BMC Med. Res. Methodol. 2013, 13, 104. [Google Scholar] [CrossRef] [PubMed]
- Sim, J.; Lewis, M. The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency. J. Clin. Epidemiol. 2012, 65, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Julious, S.A. Sample size of 12 per group rule of thumb for a pilot study. Pharm. Stat. J. Appl. Stat. Pharm. Ind. 2005, 4, 287–291. [Google Scholar] [CrossRef]
- Klasnja, P.; Hekler, E.B.; Shiffman, S.; Boruvka, A.; Almirall, D.; Tewari, A.; Murphy, S.A. Microrandomized trials: An experimental design for developing just-in-time adaptive interventions. Health Psychol. 2015, 34, 1220. [Google Scholar] [CrossRef] [PubMed]
- Clemes, S.A.; Bingham, D.D.; Pearson, N.; Chen, Y.-L.; Edwardson, C.L.; McEachan, R.R.; Tolfrey, K.; Cale, L.; Richardson, G.; Fray, M. Stand Out in Class: Restructuring the classroom environment to reduce sitting time–findings from a pilot cluster randomised controlled trial. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Bronfenbrenner, U. Toward an experimental ecology of human development. Am. Psychol. 1977, 32, 513. [Google Scholar] [CrossRef]
- Sallis, J.F.; Owen, N.; Fisher, E.B. Ecological models of health behavior. Health Behav. Health Educ. Theory Res. Pract. 2008, 4, 465–486. [Google Scholar]
- Michie, S.; Fixsen, D.; Grimshaw, J.M.; Eccles, M.P. Specifying and reporting complex behaviour change interventions: The need for a scientific method. Implement. Sci. 2009, 4, 1–6. [Google Scholar] [CrossRef]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The Behavior Change Technique Taxonomy (v1) of 93 Hierarchically Clustered Techniques: Building an International Consensus for the Reporting of Behavior Change Interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef]
- Higgins, J.P.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2008. [Google Scholar]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gøtzsche, P.C.; Devereaux, P.J. CONSORT 2010 Explanation and Elaboration: Updated guidelines for reporting parallel group randomised trials. Int. J. Surg. 2012, 10, 28–55. [Google Scholar] [CrossRef]
- Edwardson, C.L.; Winkler, E.A.; Bodicoat, D.H.; Yates, T.; Davies, M.J.; Dunstan, D.W.; Healy, G.N. Considerations when using the activPAL monitor in field-based research with adult populations. J. Sport Health Sci. 2017, 6, 162–178. [Google Scholar] [CrossRef] [PubMed]
- Lohman, T.G.; Roche, A.F.; Martorell, R. Anthropometric Standardization Reference Manual; Human kinetics books Champaign: Champaign, IL, USA, 1988; Volume 177. [Google Scholar]
- Molarius, A.; Seidell, J.; Sans, S.; Tuomilehto, J.; Kuulasmaa, K. Waist and hip circumferences, and waist-hip ratio in 19 populations of the WHO MONICA Project. Int. J. Obes. 1999, 23, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Frese, E.M.; Fick, A.; Sadowsky, H.S. Blood pressure measurement guidelines for physical therapists. Cardiopulm. Phys. Ther. J. 2011, 22, 5. [Google Scholar] [CrossRef] [PubMed]
- Graves, L.; Murphy, R.; Shepherd, S.O.; Cabot, J.; Hopkins, N.D. Evaluation of sit-stand workstations in an office setting: A randomised controlled trial. BMC Public Health 2015, 15, 1145. [Google Scholar] [CrossRef]
- Winkler, E.A.; Bodicoat, D.H.; Healy, G.N.; Bakrania, K.; Yates, T.; Owen, N.; Dunstan, D.W.; Edwardson, C.L. Identifying adults’ valid waking wear time by automated estimation in activPAL data collected with a 24 h wear protocol. Physiol. Meas. 2016, 37, 1653. [Google Scholar] [CrossRef]
- Chu, A.H.; Ng, S.H.; Tan, C.S.; Win, A.M.; Koh, D.; Muller-Riemenschneider, F.J.O.R. A systematic review and meta-analysis of workplace intervention strategies to reduce sedentary time in white-collar workers. Obes. Rev. 2016, 17, 467–481. [Google Scholar] [CrossRef]
- Rowlands, A.V.; Yates, T.; Davies, M.; Khunti, K.; Edwardson, C.L. Raw Accelerometer Data Analysis with GGIR R-package: Does Accelerometer Brand Matter? Med. Sci. Sports Exerc. 2016, 48, 1935–1941. [Google Scholar] [CrossRef]
- Hildebrand, M.; van Hees, V.T.; Hansen, B.H.; Ekelund, U. Age group comparability of raw accelerometer output from wrist-and hip-worn monitors. Med. Sci. Sports Exerc. 2014, 46, 1816–1824. [Google Scholar] [CrossRef]
- Matthews, C.E.; Hagströmer, M.; Pober, D.M.; Bowles, H.R. Best practices for using physical activity monitors in population-based research. Med. Sci. Sports Exerc. 2012, 44 (Suppl. S1), S68. [Google Scholar] [CrossRef]
- Vickers, A.J.; Altman, D.G.J.B. Analysing controlled trials with baseline and follow up measurements. BMJ 2001, 323, 1123–1124. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Academic Press: Cambridge, MA, USA, 2013. [Google Scholar]
- Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.K. Alternatives to P value: Confidence interval and effect size. Korean J. Anesthesiol. 2016, 69, 555. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence. Obesity: Identification, Classification and Management; National Institute for Health and Care Excellence: London, UK, 2014. [Google Scholar]
- World Health Organization. World Health Statistics 2016: Monitoring Health for the SDGs Sustainable Development Goals; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Clemes, S.A.; Patel, R.; Mahon, C.; Griffiths, P.L. Sitting time and step counts in office workers. Occup. Med. 2014, 64, 188–192. [Google Scholar] [CrossRef] [PubMed]
- Chastin, S.F.M.; Egerton, T.; Leask, C.; Stamatakis, E. Meta-analysis of the relationship between breaks in sedentary behavior and cardiometabolic health. Obesity 2015, 23, 1800–1810. [Google Scholar] [CrossRef] [PubMed]
- Teychenne, M.; Costigan, S.A.; Parker, K. The association between sedentary behaviour and risk of anxiety: A systematic review. BMC Public Health 2015, 15, 513. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef] [PubMed]
- Buckley, J.P.; Hedge, A.; Yates, T.; Copeland, R.J.; Loosemore, M.; Hamer, M.; Bradley, G.; Dunstan, D.W. The sedentary office: An expert statement on the growing case for change towards better health and productivity. Br. J. Sports Med. 2015, 49, 1357–1362. [Google Scholar] [CrossRef]
- Dempsey, P.C.; Larsen, R.N.; Sethi, P.; Sacre, J.W.; Straznicky, N.E.; Cohen, N.D.; Cerin, E.; Lambert, G.W.; Owen, N.; Kingwell, B.A. Benefits for type 2 diabetes of interrupting prolonged sitting with brief bouts of light walking or simple resistance activities. Diabetes Care 2016, 39, 964–972. [Google Scholar] [CrossRef]
- Henson, J.; Davies, M.J.; Bodicoat, D.H.; Edwardson, C.L.; Gill, J.M.; Stensel, D.J.; Tolfrey, K.; Dunstan, D.W.; Khunti, K.; Yates, T.E. Breaking up prolonged sitting with standing or walking attenuates the postprandial metabolic response in postmenopausal women: A randomized acute study. Diabetes Care 2016, 39, 130–138. [Google Scholar] [CrossRef]
- Winkler, E.A.; Chastin, S.; Eakin, E.G.; Owen, N.; LaMontagne, A.D.; Moodie, M.; Dempsey, P.C.; Kingwell, B.A.; Dunstan, D.W.; Healy, G.N.; et al. Cardiometabolic Impact of Changing Sitting, Standing, and Stepping in the Workplace. Med. Sci. Sports Exerc. 2018, 50, 516–524. [Google Scholar] [CrossRef]
- Hadgraft, N.T.; Brakenridge, C.L.; LaMontagne, A.D.; Fjeldsoe, B.S.; Lynch, B.M.; Dunstan, D.W.; Owen, N.; Healy, G.N.; Lawler, S.P. Feasibility and acceptability of reducing workplace sitting time: A qualitative study with Australian office workers. BMC Public Health 2016, 16, 933. [Google Scholar] [CrossRef] [PubMed]
- De Cocker, K.; Veldeman, C.; De Bacquer, D.; Braeckman, L.; Owen, N.; Cardon, G.; De Bourdeaudhuij, I. Acceptability and feasibility of potential intervention strategies for influencing sedentary time at work: Focus group interviews in executives and employees. Int. J. Behav. Nutr. Phys. Act. 2015, 12. [Google Scholar] [CrossRef] [PubMed]
- Hadgraft, N.T.; Brakenridge, C.L.; Dunstan, D.W.; Owen, N.; Healy, G.N.; Lawler, S.P.J.I.J.o.B.N.; Activity, P. Perceptions of the acceptability and feasibility of reducing occupational sitting: Review and thematic synthesis. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 90. [Google Scholar] [CrossRef] [PubMed]
- Brakenridge, C.; Fjeldsoe, B.; Young, D.; Winkler, E.; Dunstan, D.; Straker, L.; Healy, G.J. Evaluating the effectiveness of organisational-level strategies with or without an activity tracker to reduce office workers’ sitting time: A cluster-randomised trial. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 115. [Google Scholar] [CrossRef]
- Goode, A.D.; Hadgraft, N.T.; Neuhaus, M.; Healy, G.N. Perceptions of an online “train-the-champion” approach to increase workplace movement. Health Promot. Int. 2018, 34, 1179–1190. [Google Scholar] [CrossRef]
- Hadgraft, N.T.; Winkler, E.; Climie, R.E.; Grace, M.S.; Romero, L.; Owen, N.; Dunstan, D.; Healy, G.; Dempsey, P.C. Effects of sedentary behaviour interventions on biomarkers of cardiometabolic risk in adults: Systematic review with meta-analyses. Br. J. Sports Med. 2020. [Google Scholar] [CrossRef]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Campbell, M.K.; Elbourne, D.R.; Altman, D.G. CONSORT statement: Extension to cluster randomised trials. BMJ 2004, 328, 702–708. [Google Scholar] [CrossRef]
| All (n = 56) | Comparison Attrition (n = 20) | Prompt-30 (n = 21) | Prompt-60 (n = 15) | |
|---|---|---|---|---|
| Female | 36.0 (64) | 14.0 (70) | 13.0 (62) | 9.0 (60) |
| Age (years) | 39.8 ± 11.4 | 43.5 ± 10.5 | 39.3 ± 13.5 | 35.9 ± 8.4 |
| White British | 47.0 (84) | 17.0 (85) | 16.0 (76) | 14.0 (93) |
| Married | 30.0 (54) | 10.0 (50) | 15.0 (71) | 5.0 (33) |
| Full-time employee | 47.0 (84) | 16.0 (80) | 16.0 (76) | 15.0 (100) |
| Tenure in current role ≥ 3 years | 34.0 (61) | 14.0 (70) | 12.0 (57) | 8.0 (53) |
| Tertiary education | 45.0 (80) | 17.0 (85) | 13.0 (62) | 15.0 (100) |
| Management job role | 16.0 (29) | 6.0 (30) | 6.0 (29) | 4.0 (27) |
| Clerical, sales, or admin job role | 29.0 (52) | 11.0 (55) | 9.0 (43) | 9.0 (60) |
| Daily hours worked (h/day) | 7.6 ± 0.6 | 7.5 ± 0.5 | 8.0 ± 1.0 | 7.5 ± 0.5 |
| Weekly hours worked (h/week) | 36.4 ± 4.1 | 35.5 ± 6.0 | 37.2 ± 2.8 | 36.3 ± 5.4 |
| Stature (m) | 1.7 ± 0.1 | 1.7 ± 0.1 | 1.7 ± 0.1 | 1.7 ± 0.1 |
| Body mass (kg) | 83.0 ± 19.9 | 87.4 ± 18.3 | 81.3 ± 18.1 | 79.8 ± 24.5 |
| Body mass index (kg·m−2) | 29.0 ± 6.3 | 31.0 ± 6.8 | 28.4 ± 5.9 | 26.9 ± 5.7 |
| Waist circumference (cm) | 89.8 ± 16.3 | 95.4 ± 16.7 | 88.8 ± 15.4 | 83.8 ± 15.7 |
| Hip circumference (cm) | 107.3 ± 13.3 | 108.8 ± 16.0 | 107.4 ± 10.0 | 105.3 ± 14.3 |
| Systolic blood pressure (mmHg) | 135.7 ± 19.2 | 139.3 ± 16.0 | 137.7 ± 17.7 | 132.3 ± 14.5 |
| Diastolic blood pressure (mmHg) | 87.3 ± 17.3 | 91.1 ± 14.8 | 89.8 ± 7.2 | 87.5 ± 10.1 |
| Glycated haemoglobin HbA1C (%) | 5.6 ± 0.3 | 5.7 ± 0.4 | 5.4 ± 0.3 | 5.6 ± 0.3 |
| Glucose (mmol·L−1) | 5.16 ± 1.0 | 5.8 ± 1.0 | 4.7 ± 0.7 | 4.9 ± 0.9 |
| Total cholesterol (mmol·L−1) | 4.26 ± 1.0 | 4.5 ± 1.2 | 4.0 ± 0.8 | 4.2 ± 1.1 |
| High-density lipoprotein (HDL) cholesterol (mmol·L−1) | 1.16 ± 0.5 | 1.0 ± 0.3 | 1.2 ± 0.5 | 1.2 ± 0.4 |
| Low-density lipoprotein (LDL) cholesterol (mmol·L−1) | 3.10 ± 1.1 | 3.4 ± 1.2 | 2.8 ± 0.8 | 3.0 ± 1.0 |
| Cholesterol ratio (total cholesterol:HDL) | 4.16 ± 2.0 | 4.8 ± 1.9 | 3.7 ± 1.6 | 3.8 ± 2.2 |
| Behavioural worktime (ActivPAL) | ||||
| Valid wear (days) | 3.3 ± 1.7 | 3.5 ± 1.6 | 3.9 ± 1.8 | 3.5 ± 1.7 |
| Sitting time (min/8 hday) | 330.1 ± 89.8 | 329.4 ± 83.1 | 320.7 ± 110.5 | 345.2 ± 67.8 |
| Standing time (min/8 hday) | 115.3 ± 87.1 | 115.4 ± 75.5 | 125.5 ± 110.4 | 100.0 ± 67.2 |
| Stepping time (min/8 hday) | 34.6 ± 13.9 | 35.2 ± 14.5 | 33.79 ± 14.8 | 34.7 ± 12.5 |
| Prolonged sitting time (≥30 min/8 hday) | 211.0 ± 95.3 | 235.4 ± 96.0 | 184.3 ± 100.8 | 212.3 ± 81.5 |
| Steps (number/8 hday) | 3138.8 ± 1279.7 | 3130.6 ± 1178.8 | 3131.0 ± 1484.3 | 3163.8 ± 1211.0 |
| Sit–upright transitions (number/8 hworkday) | 27.6 ± 12.1 | 25.3 ± 8.0 | 30.5 ± 17.4 | 26.6 ± 6.3 |
| Behavioural whole day (ActivPAL) | ||||
| Valid wear (days) | 6.0 ± 1.5 | 5.9 ± 1.6 | 6.3 ± 1.4 | 5.8 ± 1.6 |
| Sitting time (min/16 hday) | 612.4 ± 101.8 | 629.9 ± 78.7 | 589.2 ± 112.6 | 623.2 ± 96.6 |
| Standing time (min/16 hday) | 241.9 ± 81.6 | 227.1 ± 65.53 | 266.9 ± 96.4 | 224.5 ± 73.0 |
| Stepping time (min/16 hday) | 105.6 ± 37.2 | 103.0 ± 33.3 | 103.9 ± 42.9 | 112.4 ± 35.0 |
| Prolonged sitting time (≥30 min/16 hday) | 325.9 ± 113.4 | 355.1 ± 103.3 | 295.8 ± 123.3 | 329.6 ± 107.4 |
| Steps (steps/day) | 4380.6 ± 1743.6 | 8681.6 ± 3349.1 | 8413.3 ± 3715.6 | 9446.0 ± 3493.9 |
| No-Prompt Comparison | Prompt-30 | Prompt-60 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | 6 Weeks | 12 Weeks | Baseline | 6 Weeks | 12 Weeks | Baseline | 6 Weeks | 12 Weeks | |
| Worktime (ActivPAL) (min/8 h workday) | |||||||||
| Sitting Time | 329.4 ± 83.1 | 331.6 ± 97.2 | 369.5 ± 86.0 | 320.7 ± 110.5 | 343.2 ± 81.2 | 326.0 ± 119.3 | 345.2 ± 67.8 | 314.6 ± 112.3 | 302.4 ± 117.4 |
| Standing Time | 115.4 ± 75.5 | 120.3 ± 96.5 | 83.1 ± 80.5 | 125.5 ± 110.4 | 104.3 ± 74.4 | 123.1 ± 119.1 | 100.0 ± 67.2 | 129.7 ± 115.8 | 140.9 ± 116.7 |
| Stepping Time | 35.2 ± 14.5 | 28.1 ± 9.6 | 27.4 ± 10.6 | 33.8 ± 14.8 | 32.4 ± 20.6 | 30.9 ± 14.7 | 34.8 ± 12.5 | 35.7 ± 16.9 | 36.7 ± 17.9 |
| Prolonged Sitting Time (≥30 min) | 235.4 ± 96.1 | 160.1 ± 118.5 | 218.6 ± 116.2 | 184.3 ± 100.8 | 141.5 ± 75.2 | 139.8 ± 105.2 | 212.3 ± 81.5 | 179.7 ± 107.8 | 153.6 ± 116.9 |
| Steps (number) | 3130.6 ± 1178.8 | 2616.4 ± 946.4 | 2581.4 ± 1040.6 | 3131.0 ± 1484.3 | 2874.2 ± 1600.2 | 2737.9 ± 1339.7 | 3163.8 ± 1211.0 | 3192.2 ± 1481.8 | 3359.1 ± 1703.9 |
| Whole day (min/16 h day) | |||||||||
| Sitting Time | 629.9 ± 78.7 | 633.2 ± 91.1 | 694.8 ± 92.7 | 589.2 ± 122.6 | 601.4 ± 110.7 | 612.5 ± 116.5 | 623.2 ± 96.6 | 613.8 ± 147.9 | 622.1 ± 122.2 |
| Standing Time | 227.1 ± 65.3 | 245.2 ± 90.9 | 188.4 ± 78.4 | 266.9 ± 96.4 | 259.2 ± 79.4 | 257.1 ± 116.7 | 224.5 ± 73.0 | 245.4 ± 140.2 | 244.5 ± 110.8 |
| Stepping Time | 103.0 ± 33.1 | 81.6 ± 13.0 | 76.8 ± 22.9 | 103.9 ± 42.9 | 99.4 ± 38.1 | 90.4 ± 24.8 | 112.4 ± 35.0 | 100.8 ± 30.4 | 93.5 ± 28.5 |
| Prolonged Sitting Time (≥30 min) | 355.1 ± 103.3 | 350.5 ± 132.9 | 420.3 ± 144.2 | 295.8 ± 123.3 | 297.2 ± 107.5 | 331.1 ± 106.9 | 329.6 ± 107.3 | 342.3 ± 144.1 | 379.3 ± 126.6 |
| Steps (number) | 8681.6 ± 3349.1 | 6725.5 ± 1268.2 | 6320.3 ± 1930.5 | 8413.3 ± 3715.6 | 7962.4 ± 325.5 | 7142.0 ± 2086.3 | 9946.0 ± 3493.9 | 8007.7 ± 2353.6 | 7656.3 ± 2694.6 |
| Adjusted Mean Change 0–6 Weeks | Adjusted Mean Change 0–12 Weeks | |||||||
|---|---|---|---|---|---|---|---|---|
| Prompt-30 Coefficient (95% CI) | Cohen’s d (95% CI) | Prompt-60 Coefficient (95% CI) | Cohen’s d (95% CI) | Prompt-30 Coefficient (95% CI) | Cohen’s d (95% CI) | Prompt-60 Coefficient (95% CI) | Cohen’s d (95% CI) | |
| Worktime (ActivPAL) (min/8 h workday) | ||||||||
| Sitting Time | −35.5 (−73.8, 3.0) | −0.4 (−1.0, −1.6) | −46.7 (−86.4, −6.6) * | 5.6 (5.2, 6.0) | −37.0 (−78.0, 4.2) | −0.5 (−1.3, −2.2) | −69.8 (−111.0, −28.2) ** | −20.5 (−20.8, −19.3) |
| Standing Time | 29.4 (−7.2, 66.0) | 0.6 (0.3, 0.7) | 40.8 (34.8, 8.6) * | −4.7 (−5.0, −4.3) | 34.8 (−3.6, 73.8) | 0.3 (−0.1, 0.0) | 64.8 (25.8, 103.8) ** | 10.0 (9.4, 10.6) |
| Stepping Time | 6.0 (−6.6, 18.6) | 0.4 (0.3, 0.7) | 7.1 (−6.0, 20.4) | −2.9 (−3.0, −2.8) | 3.0 (−10.2, 16.2) | 0.0 (−0.1, 0.1) | 7.2 (−6.0, 20.4) | 0.8 (0.7, 0.8) |
| Prolonged Sitting Time (≥30 min) | −7.8 (60.0, 76.2) | 0.5 (−0.1, 0.1) | 23.4 (−48.0, 95.4) | 4.2 (3.6, 4.8) | −27.0 (−99.0, 45.0) | 0.0 (−0.7, 1.0) | −25.8 (−98.4, 47.4) | 7.2 (6.3, 8.2) |
| Whole day (min/16 h day) | ||||||||
| Sitting Time | −7.2 (−63.0, 49.2) | −0.2 (−0.6, −0.9) | −10.2 (−67.8, 47.4) | 0.3 (−0.4, 0.9) | −42.0 (−100.8, 16.8) | −0.5 (−1.1, −1.8) | −28.2 (−90.0, 3.8) | 3.9 (3.3, 4.5) |
| Standing Time | −7.2 (−54.6, 40.2) | −0.2 (−0.5, −0.8) | 7.2 (−41.4, 55.8) | −0.3 (−0.9, 0.3) | 29.4 (−20.4, 79.2) | 0.4 (0.0, 0.2) | 33.6 (−19.8, 87.6) | −13.5 (−13.9, −13.0) |
| Stepping Time | 14.4 (−48.0, 33.6) | 0.8 (0.6, 1.2) | 3.0 (−16.8, 22.8) | 2.2 (2.0, 2.3) | 12.6 (−7.8, 32.4) | 0.7 (0.5, 1.1) | −4.8 (−26.4, 16.8) | 0.7 (0.5, 0.9) |
| Prolonged Sitting Time (≥30 min) | −7.2 (−78.6, 64.2) | −0.2 (−0.7, −1.1) | 31.2 (−42.0, 44.4) | −0.9 (−1.7, −0.2) | −23.4 (−98.4, 51.6) | −0.5 (−1.1, −1.9) | 17.4 (−63.0, 98.4) | −29.0 (−29.9, −28.2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morris, A.S.; Mackintosh, K.A.; Dunstan, D.; Owen, N.; Dempsey, P.; Pennington, T.; McNarry, M.A. Rise and Recharge: Effects on Activity Outcomes of an e-Health Smartphone Intervention to Reduce Office Workers’ Sitting Time. Int. J. Environ. Res. Public Health 2020, 17, 9300. https://doi.org/10.3390/ijerph17249300
Morris AS, Mackintosh KA, Dunstan D, Owen N, Dempsey P, Pennington T, McNarry MA. Rise and Recharge: Effects on Activity Outcomes of an e-Health Smartphone Intervention to Reduce Office Workers’ Sitting Time. International Journal of Environmental Research and Public Health. 2020; 17(24):9300. https://doi.org/10.3390/ijerph17249300
Chicago/Turabian StyleMorris, Abigail S., Kelly A. Mackintosh, David Dunstan, Neville Owen, Paddy Dempsey, Thomas Pennington, and Melitta A. McNarry. 2020. "Rise and Recharge: Effects on Activity Outcomes of an e-Health Smartphone Intervention to Reduce Office Workers’ Sitting Time" International Journal of Environmental Research and Public Health 17, no. 24: 9300. https://doi.org/10.3390/ijerph17249300
APA StyleMorris, A. S., Mackintosh, K. A., Dunstan, D., Owen, N., Dempsey, P., Pennington, T., & McNarry, M. A. (2020). Rise and Recharge: Effects on Activity Outcomes of an e-Health Smartphone Intervention to Reduce Office Workers’ Sitting Time. International Journal of Environmental Research and Public Health, 17(24), 9300. https://doi.org/10.3390/ijerph17249300







