A Hybrid Effectiveness-Implementation Study of a Multi-Component Lighting Intervention for Hospital Shift Workers
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
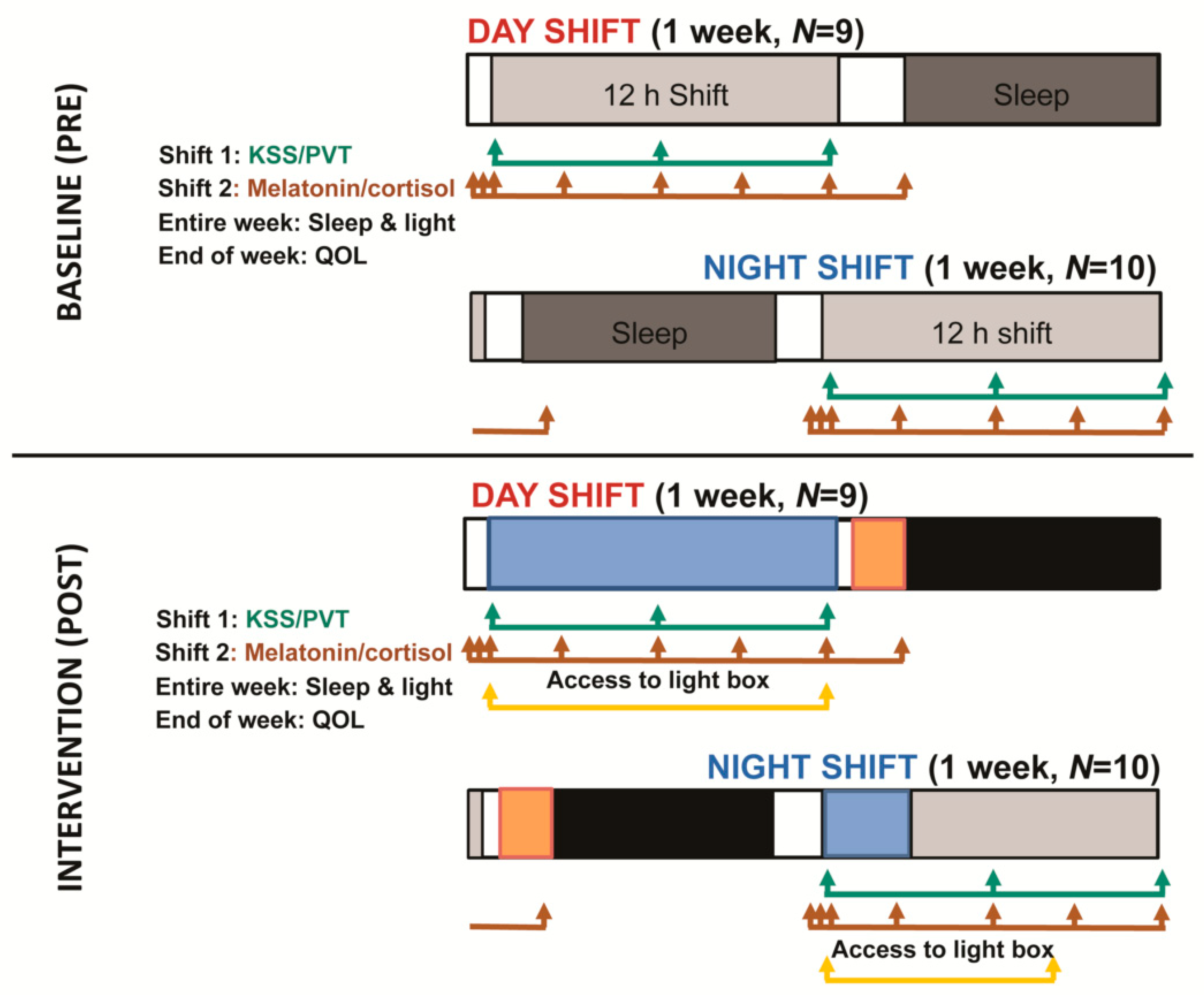
2.2. Protocol
2.3. Measures
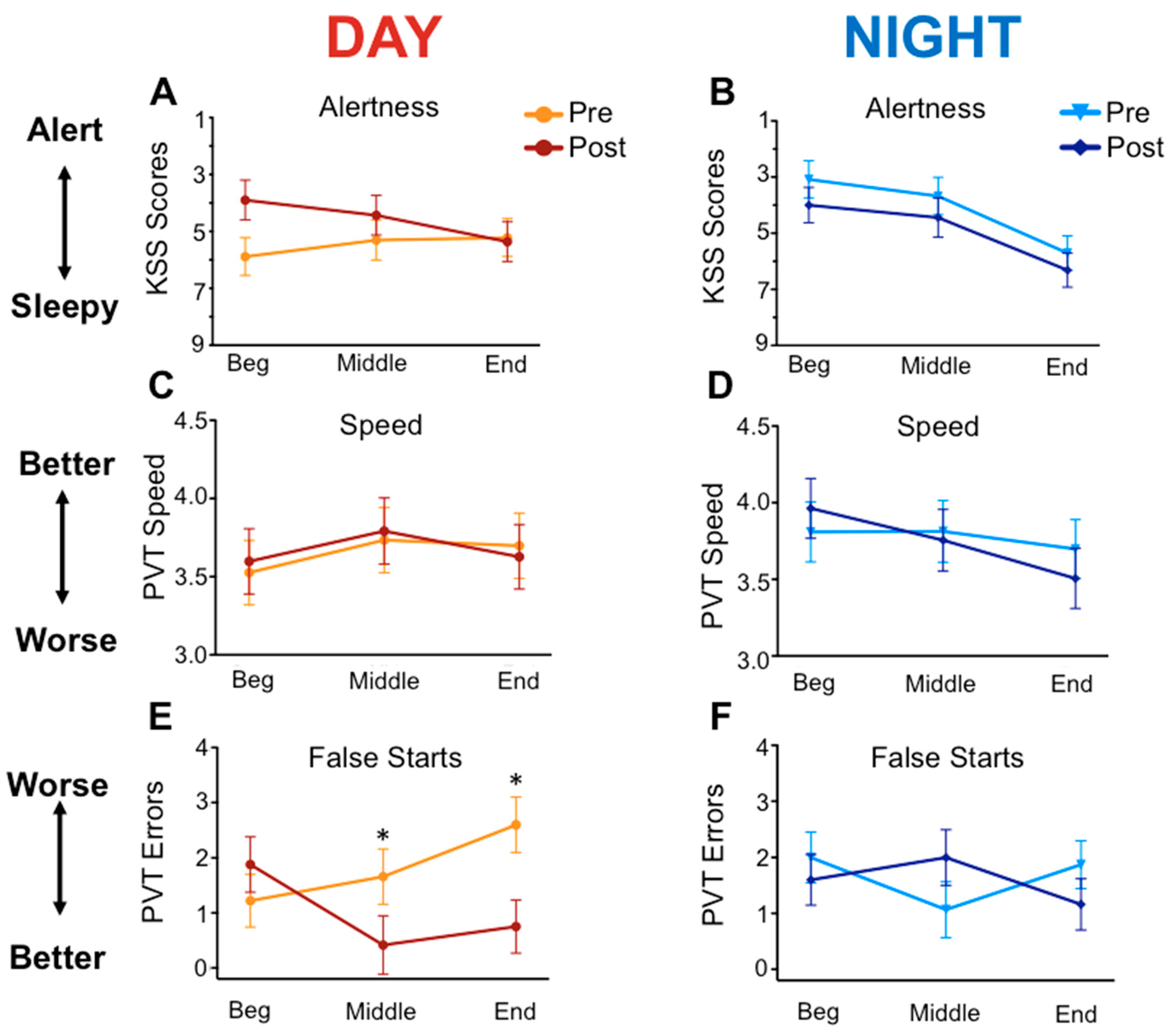
3. Results
3.1. Intervention Use
3.2. Effectiveness Measures
3.3. Implementation Measures
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Disclaimer
References
- Kecklund, G.; Axelsson, J. Health consequences of shift work and insufficient sleep. BMJ 2016, 355, i5210. [Google Scholar] [CrossRef] [PubMed]
- Neil-Sztramko, S.E.; Pahwa, M.; Demers, P.A.; Gotay, C.C. Health-related interventions among night shift workers: A critical review of the literature. Scand. J. Work Environ. Health 2014, 543–556. [Google Scholar] [CrossRef] [PubMed]
- Chellappa, S.L.; Steiner, R.; Blattner, P.; Oelhafen, P.; Götz, T.; Cajochen, C. Non-visual effects of light on melatonin, alertness and cognitive performance: Can blue-enriched light keep us alert? PLoS ONE 2011, 6, e16429. [Google Scholar] [CrossRef] [PubMed]
- Parthasarathy, S.; Carskadon, M.A.; Jean-Louis, G.; Owens, J.; Bramoweth, A.; Combs, D.; Honaker, S.M. Implementation of sleep and circadian science: Recommendations from the Sleep Research Society and National Institutes of Health workshop. Sleep 2016, 39, 2061–2075. [Google Scholar] [CrossRef]
- Harrison, E.M.; Schmied, E.A.; Yablonsky, A.M.; Glickman, G.L. Implementation of interventions designed to enhance the circadian health of shiftworkers. Chronobiol. Int. 2020, 37, 573–591. [Google Scholar]
- Landes, S.J.; McBain, S.A.; Curran, G.M. Reprint of: An introduction to effectiveness-implementation hybrid designs. Psychiatry Res. 2019, 283, 112630. [Google Scholar] [CrossRef]
- Schmied, E.A.; Harrison, E.M.; Powell, A.L.; Yablonsky, A.M.; Glickman, G.L. Engagement and satisfaction with a multi-component lighting intervention for enhancing sleep, circadian health and performance in military hospital staff. In Proceedings of the Illuminating Engineering Society Conference Annual Symposium Proceedings (extended abstract), Louisville, KY, USA, 8–10 August 2018. [Google Scholar]
- Smith, M.R.; Eastman, C.I. Shift work: Health, performance and safety problems, traditional countermeasures, and innovative management strategies t reduce circadian misalignment. Nat. Sci. Sleep 2012, 4, 111–132. [Google Scholar]
- Lockley, S.W. Safety considerations for the use of blue-light blocking glasses in shift-workers. J. Pineal Res. 2007, 42, 210–211. [Google Scholar] [CrossRef]
- Harrison, E.M.; Yablonsky, A.M.; Powell, A.L.; Ancoli-Israel, S.; Glickman, G.L. Reported light in the sleep environment: Enhancement of the sleep diary. Nat. Sci. Sleep 2019, 11, 11. [Google Scholar] [CrossRef]
- Basner, M.; Mollicone, D.; Dinges, D.F. Validity and sensitivity of a brief psychomotor vigilance test (PVT-B) to total and partial sleep deprivation. Acta Astronaut. 2011, 69, 949–959. [Google Scholar] [CrossRef]
- Ferrans, C.E.; Powers, M.J. Psychometric assessment of the Quality of Life Index. Res. Nurs. Health 1992, 15, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Rannestad, T.; Eikeland, O.; Helland, H.; Qvarnstrom, U. The quality of life in women suffering from gynecological disorders is improved by means of hysterectomy. Acta Obstet. Gynecol. Scand. 2001, 80, 46–51. [Google Scholar] [CrossRef]
- Taylor, R. Quality of life and symptom severity for individuals with Chronic Fatigue Syndrome: Findings from a clinical trial. Am. J. Occup. Ther. 2004, 58, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Ghadam, M.S.; Poorgholami, F.; Jahromi, Z.B.; Parandavar, N.; Kalani, N.; Rahmanian, E. Effect of self-care education by face-to-face method on the quality of life in hemodialysis patients. Glob. J. Health Sci. 2016, 8, 121–127. [Google Scholar] [CrossRef][Green Version]
- Damschroder, L.J.; Aron, D.C.; Keith, R.E.; Kirsh, S.R.; Alexander, J.A.; Lowery, J.C. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement. Sci. 2009, 4, 50. [Google Scholar] [CrossRef]
- Åkerstedt, T. Shift work and disturbed sleep/wakefulness. Sleep Med. Rev. 1998, 2, 117–128. [Google Scholar] [CrossRef]
- Flynn-Evans, E.E.; Arsintescu, L.; Gregory, K.; Mulligan, J.; Nowinski, J.; Feary, M. Sleep and neurobehavioral performance vary by work start time during non-traditional day shifts. Sleep Health 2018, 4, 476–484. [Google Scholar] [CrossRef] [PubMed]
- Harrison, E.M.; Walbeek, T.J.; Maggio, D.G.; Herring, A.A.; Gorman, M.R. Circadian profile of an emergency medicine department: Scheduling practices and their effects on sleep and performance. J. Emerg. Med. 2020, 58, 130–140. [Google Scholar] [CrossRef]
- Boivin, D.B.; James, F.O. Circadian adaptation to night-shift work by judicious light and darkness exposure. J. Biol. Rhythm. 2002, 17, 556–567. [Google Scholar] [CrossRef]
- Yoon, I.; Jeong, D.; Kwon, K.; Kang, S.; Song, B. Bright light exposure at night and light attenuation in the morning improve adaptation of night shift workers. Sleep 2002, 25, 351–356. [Google Scholar]
- Sasseville, A.; Hebert, M. Using blue-green light at night and blue-blockers during the day to improve adaptation to night work: A pilot study. Prog. Neuro Psychopharm. Biol. Psychiatry 2010, 34, 1236–1242. [Google Scholar] [CrossRef] [PubMed]
- Thorne, H.C.; Hampton, S.M.; Morgan, L.M.; Skene, D.J.; Arendt, J. Returning from night shift to day life: Beneficial effects of light on sleep. Sleep Biol. Rhythm. 2010, 8, 212–221. [Google Scholar] [CrossRef]
- Boivin, D.B.; Boudreau, P.; Tremblay, G.M. Phototherapy and orange-tinted goggles for night-shift adaptation of police officers on patrol. Chronobiol. Int. 2012, 29, 629–640. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Tsai, M.; Chen, C.; Hsu, S. The effectiveness of light/dark exposure to treat insomnia in female nurses undertaking shift work during the evening/night shift. J. Clin. Sleep Med. 2013, 9, 641–646. [Google Scholar] [CrossRef] [PubMed]
- Edwardson, C.L.; Yates, T.; Biddle, S.J.H.; Davies, M.J.; Dunstan, D.W.; Esliger, D.W.; Gray, L.J.; Jackson, B.; O’connell, S.E.; Waheed, G.; et al. Effectiveness of the Stand More AT (SMArT) Work intervention: Cluster randomised controlled trial. BMJ 2018, 363, k3870. [Google Scholar] [CrossRef]
- Fessel, M.M.; Mann, M.; Miyawaki, C.E.; Rosenberg, D.E. Multi-Component Interventions and Cognitive Health: A Scoping Review. J. Gerontol. Nurs. 2017, 43, 39–48. [Google Scholar] [CrossRef]
- Wang, Y.; Cai, L.; Wu, Y.; Wilson, R.F.; Weston, C.; Fawole, O.; Bleich, S.N.; Cheskin, L.J.; Showell, N.N.; Lau, B.D.; et al. What childhood obesity prevention programmes work? A systematic review and meta-analysis. Obes. Rev. 2015, 16, 547–565. [Google Scholar] [CrossRef]
- Wilfling, D.; Junghans, A.; Marshall, L.; Eisemann, N.; Meyer, G.; Möhler, R.; Köpke, S. Non-pharmacological interventions for sleep disturbances in people with dementia (Protocol). Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef]
| Day | Night | |||||
|---|---|---|---|---|---|---|
| Baseline (SEM) | Intervention (SEM) | p Value | Baseline (SEM) | Intervention (SEM) | p Value | |
| Sleep Quality | 3.22 (0.16) | 3.80 (0.16) | <0.001 | 3.30 (0.16) | 3.12 (0.16) | 0.33 |
| Total Sleep Time (m) | 416.03 (32.27) | 421.29 (32.23) | 0.82 | 401.29 (25.90) | 380.48 (26.16) | 0.44 |
| Sleep Onset Latency (m) | 31.29 (11.80) | 26.91 (11.84) | 0.59 | 23.34 (5.85) | 16.08 (6.05) | 0.37 |
| WASO (m) | 9.10 (2.47) | 6.55 (2.54) | 0.23 | 22.08 (6.39) | 14.39 (6.40) | 0.18 |
| Caffeine (drinks/day) | 1.57 (0.25) | 1.26 (0.25) | <0.05 | 1.05 (0.17) | 0.96 (0.17) | 0.55 |
| Overall QOL | 20.01 (1.46) | 22.48 (1.69) | <0.05 | 22.13 (1.10) | 23.36 (1.01) | <0.05 |
| Health QOL | 20.07 (1.52) | 22.79 (1.88) | <0.05 | 20.30 (1.24) | 22.01 (0.98) | <0.05 |
| Family QOL | 20.09 (2.18) | 22.21 (2.03) | <0.05 | 24.19 (1.02) | 24.25 (1.22) | 0.96 |
| Socio-Economic QOL | 21.08 (1.37) | 22.62 (1.89) | 0.16 | 24.06 (1.29) | 24.98 (1.13) | 0.17 |
| Psych-Spiritual QOL | 18.65 (2.16) | 21.77 (1.80) | 0.10 | 22.27 (1.88) | 23.58 (1.53) | 0.10 |
| Lighting Satisfaction | 2.78 (0.22) | 3.13 (0.28) | 0.35 | 3.50 (0.53) | 4.91 (0.58) | <0.05 |
| Ease of Use | Somewhat—Very Easy | Somewhat—Very Difficult | No Opinion | Somewhat—Very Easy | Somewhat—Very Difficult | No Opinion |
| Lightbox | 80.0% | 20.0% | 0% | 77.8% | 22.2% | 0% |
| Eyemasks | 83.3% | 0% | 16.7% | 87.5% | 12.5% | 0% |
| Blue-blockers | 100.0% | 0% | 0% | 100.0% | 0% | 0% |
| Future Use | Somewhat—Very Likely | Somewhat—Very Unlikely | No Opinion | Somewhat—Very Likely | Somewhat—Very Unlikely | No Opinion |
| Lightbox | 44.4% | 44.4% | 11.1% | 80.0% | 10.0% | 10.0% |
| Eyemasks | 55.5% | 33.3% | 11.1% | 60.0% | 40.0% | 0% |
| Blue-blockers | 55.5% | 33.3% | 11.1% | 80.0% | 10.0% | 10.0% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harrison, E.M.; Schmied, E.A.; Easterling, A.P.; Yablonsky, A.M.; Glickman, G.L. A Hybrid Effectiveness-Implementation Study of a Multi-Component Lighting Intervention for Hospital Shift Workers. Int. J. Environ. Res. Public Health 2020, 17, 9141. https://doi.org/10.3390/ijerph17239141
Harrison EM, Schmied EA, Easterling AP, Yablonsky AM, Glickman GL. A Hybrid Effectiveness-Implementation Study of a Multi-Component Lighting Intervention for Hospital Shift Workers. International Journal of Environmental Research and Public Health. 2020; 17(23):9141. https://doi.org/10.3390/ijerph17239141
Chicago/Turabian StyleHarrison, Elizabeth M., Emily A. Schmied, Alexandra P. Easterling, Abigail M. Yablonsky, and Gena L. Glickman. 2020. "A Hybrid Effectiveness-Implementation Study of a Multi-Component Lighting Intervention for Hospital Shift Workers" International Journal of Environmental Research and Public Health 17, no. 23: 9141. https://doi.org/10.3390/ijerph17239141
APA StyleHarrison, E. M., Schmied, E. A., Easterling, A. P., Yablonsky, A. M., & Glickman, G. L. (2020). A Hybrid Effectiveness-Implementation Study of a Multi-Component Lighting Intervention for Hospital Shift Workers. International Journal of Environmental Research and Public Health, 17(23), 9141. https://doi.org/10.3390/ijerph17239141







