Factors Predicting Treatment of World Trade Center-Related Lung Injury: A Longitudinal Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Source Population and Data Sources
2.2. ICS/LABA Treatment
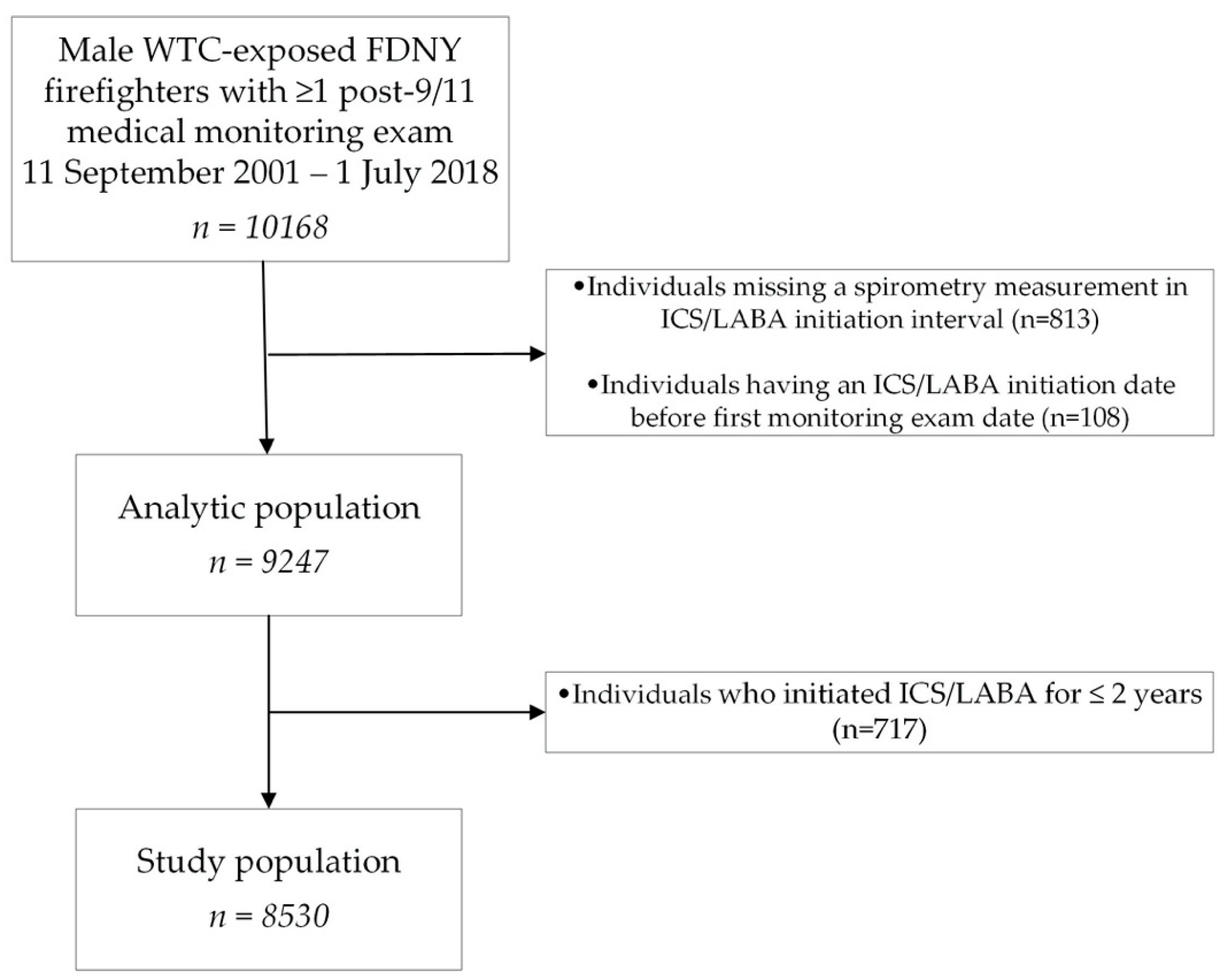
2.3. Dataset Structure and Exclusions
2.4. Statistical Analyses
3. Results
3.1. Concurrent Symptoms and ICS/LABA Treatment Duration
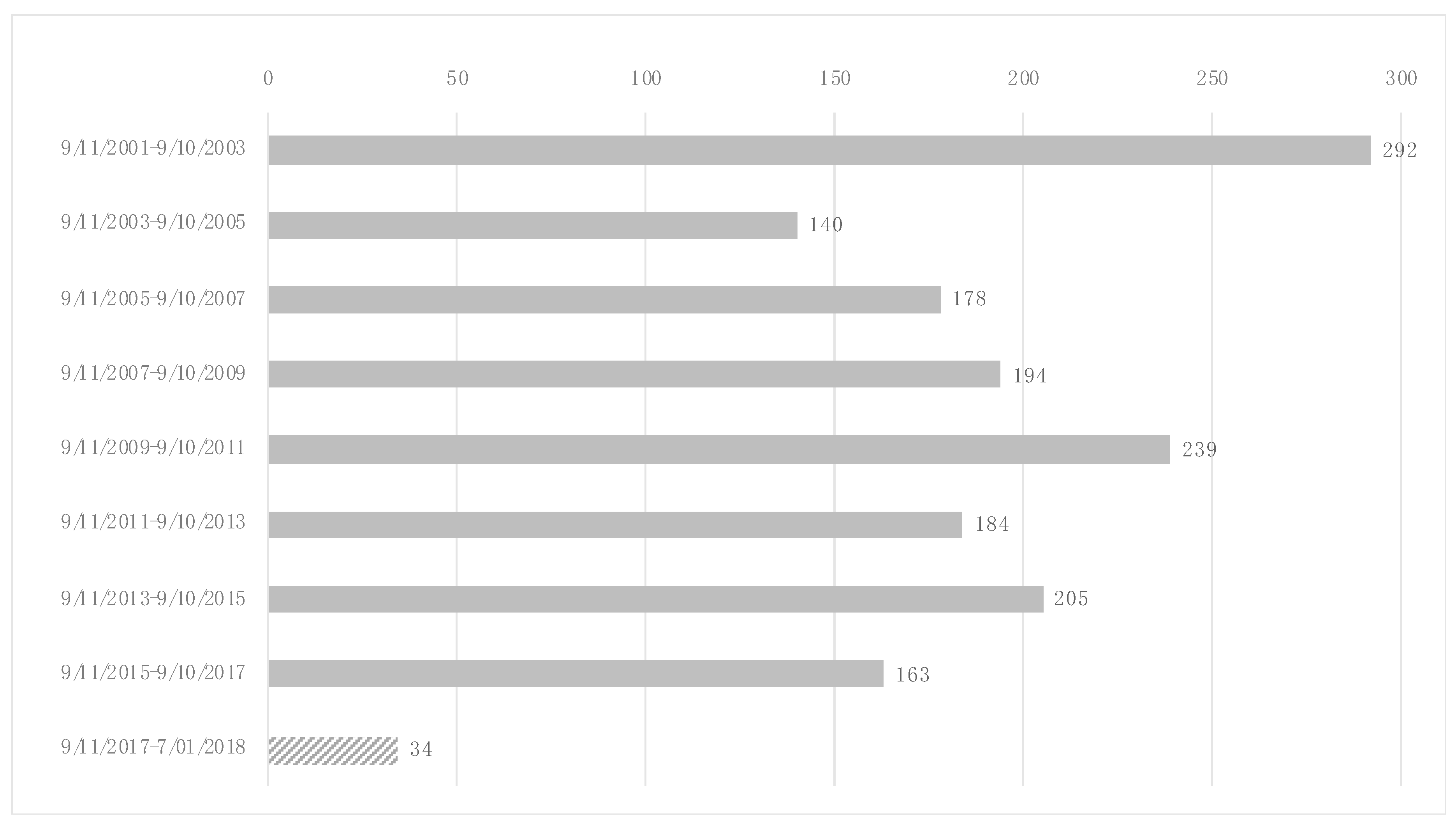
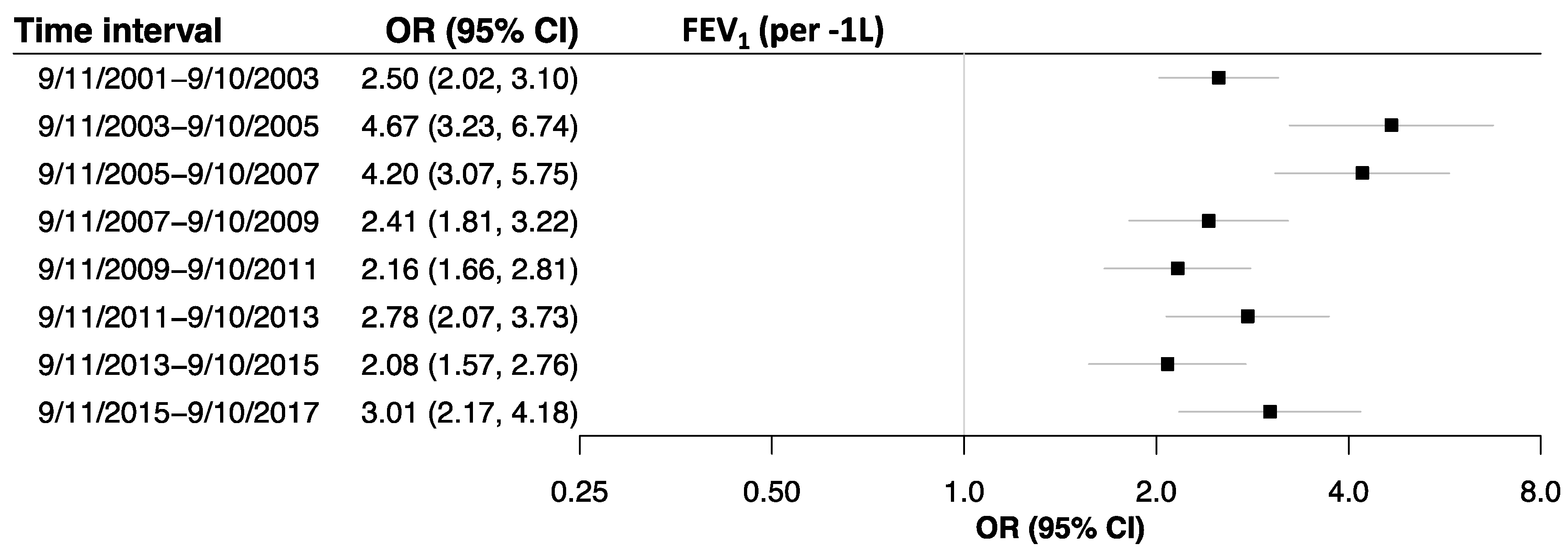
3.2. Initiation of Prolonged ICS/LABA Treatment Over Time
3.3. Sensitivity Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lioy, P.J.; Weisel, C.P.; Millette, J.R.; Eisenreich, S.; Vallero, D.; Offenberg, J.; Buckley, B.; Turpin, B.; Zhong, M.; Cohen, M.D.; et al. Characterization of the dust/smoke aerosol that settled east of the World Trade Center (WTC) in lower Manhattan after the collapse of the WTC 11 September 2001. Environ. Health Perspect. 2002, 110, 703–714. [Google Scholar] [CrossRef] [PubMed]
- Prezant, D.J.; Weiden, M.; Banauch, G.I.; McGuinness, G.; Rom, W.N.; Aldrich, T.K.; Kelly, K.J. Cough and Bronchial Responsiveness in Firefighters at the World Trade Center Site. N. Engl. J. Med. 2002, 347, 806–815. [Google Scholar] [CrossRef] [PubMed]
- Webber, M.P.; Gustave, J.; Lee, R.; Niles, J.K.; Kelly, K.; Cohen, H.W.; Prezant, D.J. Trends in Respiratory Symptoms of Firefighters Exposed to the World Trade Center Disaster: 2001–2005. Environ. Health Perspect. 2009, 117, 975–980. [Google Scholar] [CrossRef] [PubMed]
- Aldrich, T.K.; Gustave, J.; Hall, C.B.; Cohen, H.W.; Webber, M.P.; Zeig-Owens, R.; Cosenza, K.; Christodoulou, V.; Glass, L.; Al-Othman, F.; et al. Lung Function in Rescue Workers at the World Trade Center after 7 Years. N. Engl. J. Med. 2010, 362, 1263–1272. [Google Scholar] [CrossRef] [PubMed]
- Weiden, M.D.; Ferrier, N.; Nolan, A.; Rom, W.N.; Comfort, A.; Gustave, J.; Zeig-Owens, R.; Zheng, S.; Goldring, R.M.; Berger, K.I.; et al. Obstructive Airways Disease With Air Trapping Among Firefighters Exposed to World Trade Center Dust. Chest 2010, 137, 566–574. [Google Scholar] [CrossRef] [PubMed]
- Weakley, J.; Webber, M.P.; Gustave, J.; Kelly, K.; Cohen, H.W.; Hall, C.B.; Prezant, D.J. Trends in respiratory diagnoses and symptoms of firefighters exposed to the World Trade Center disaster: 2005–2010. Prev. Med. 2011, 53, 364–369. [Google Scholar] [CrossRef] [PubMed]
- Zeig-Owens, R.; Singh, A.; Aldrich, T.K.; Hall, C.B.; Schwartz, T.; Webber, M.P.; Cohen, H.W.; Kelly, K.J.; Nolan, A.; Prezant, D.J.; et al. Blood Leukocyte Concentrations, FEV1 Decline, and Airflow Limitation. A 15-Year Longitudinal Study of World Trade Center–exposed Firefighters. Ann. Am. Thorac. Soc. 2018, 15, 173–183. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Liu, C.; Putman, B.; Zeig-Owens, R.; Hall, C.B.; Schwartz, T.; Webber, M.P.; Cohen, H.W.; Berger, K.I.; Nolan, A.; et al. Predictors of Asthma/COPD Overlap in FDNY Firefighters With World Trade Center Dust Exposure. Chest 2018, 154, 1301–1310. [Google Scholar] [CrossRef] [PubMed]
- Yip, J.; Webber, M.P.; Zeig-Owens, R.; Vossbrinck, M.; Singh, A.; Kelly, K.; Prezant, D.J. FDNY and 9/11: Clinical services and health outcomes in World Trade Center-exposed firefighters and EMS workers from 2001 to 2016: FDNY WTC Health Program. Am. J. Ind. Med. 2016, 59, 695–708. [Google Scholar] [CrossRef] [PubMed]
- Putman, B.; Lahousse, L.; Singh, A.; Zeig-Owens, R.; Hall, C.B.; Fazzari, M.J.; Schwartz, T.; Webber, M.P.; Cohen, H.W.; Prezant, D.J.; et al. Dyspnea and Inhaled Corticosteroid and Long-acting β-Agonist Therapy in an Occupational Cohort: A Longitudinal Study. Ann. Am. Thorac. Soc. 2020, 17, 770–773. [Google Scholar] [CrossRef] [PubMed]
- Reddel, H.K.; Bateman, E.D.; Becker, A.; Boulet, L.-P.; Cruz, A.A.; Drazen, J.M.; Haahtela, T.; Hurd, S.S.; Inoue, H.; de Jongste, J.C.; et al. A summary of the new GINA strategy: A roadmap to asthma control. Eur. Respir. J. 2015, 46, 622–639. [Google Scholar] [CrossRef] [PubMed]
- Calverley, P.M.A.; Anderson, J.A.; Celli, B.; Ferguson, G.T.; Jenkins, C.; Jones, P.W.; Yates, J.C.; Vestbo, J. Salmeterol and Fluticasone Propionate and Survival in Chronic Obstructive Pulmonary Disease. N. Engl. J. Med. 2007, 356, 775–789. [Google Scholar] [CrossRef] [PubMed]
- The Global Strategy for Asthma Management and Prevention. 2020 GINA Report. Available online: https://ginasthma.org/wp-content/uploads/2020/04/GINA-2020-full-report_-final-_wms.pdf (accessed on 20 August 2020).
- Global Initiative for Chronic Obstructive Lung Disease. 2020 Global Strategy for Prevention, Diagnosis and Management of COPD. Available online: https://goldcopd.org/wp-content/uploads/2019/12/GOLD-2020-FINAL-ver1.2-03Dec19_WMV.pdf (accessed on 20 August 2020).
- Aliverti, A. Wearable technology: Role in respiratory health and disease. Breathe 2017, 13, e27–e36. [Google Scholar] [CrossRef] [PubMed]
- Ambrosino, N.; Fracchia, C. The role of tele-medicine in patients with respiratory diseases. Expert Rev. Respir. Med. 2017, 11, 893–900. [Google Scholar] [CrossRef] [PubMed]
- Hall, C.B.; Liu, X.; Zeig-Owens, R.; Webber, M.P.; Aldrich, T.K.; Weakley, J.; Schwartz, T.; Cohen, H.W.; Glaser, M.S.; Olivieri, B.L.; et al. The Duration of an Exposure Response Gradient between Incident Obstructive Airways Disease and Work at the World Trade Center Site: 2001–2011. PLoS Curr. 2015. [Google Scholar] [CrossRef] [PubMed]
- Zhang, O.; Minku, L.L.; Gonem, S. Detecting asthma exacerbations using daily home monitoring and machine learning. J. Asthma 2020, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Weldring, T.; Smith, S.M.S. Patient-Reported Outcomes (PROs) and Patient-Reported Outcome Measures (PROMs). Health Serv. Insights 2013, 6, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Parimi, M.; Svedsater, H.; Ann, Q.; Gokhale, M.; Gray, C.M.; Hinds, D.; Nixon, M.; Boxall, N. Persistence and Adherence to ICS/LABA Drugs in UK Patients with Asthma: A Retrospective New-User Cohort Study. Adv. Ther. 2020, 37, 2916–2931. [Google Scholar] [CrossRef] [PubMed]

| Variable | Study Population N = 8530 | ICS/LABA non-Treated N = 6901 | ICS/LABA Treated >2 y N = 1629 | ICS/LABA Treated ≤2 y N = 717 |
|---|---|---|---|---|
| Age on 9/11 | 40.5 ± 7.5 | 40.4 ± 7.7 | 40.8 ± 6.8 | 39.8 ± 7.3 |
| Height (cm) | 177.1 ± 6.4 | 177.0 ± 6.4 | 177.2 ± 6.6 | 177.5 ± 6.6 |
| Smoker, ever * | 2195 (25.7) | 1754 (25.4) | 441 (27.1) | 199 (27.8) |
| Race | ||||
| White | 8008 (93.9) | 6464 (93.7) ‡ | 1544 (94.8) ‡ | 677 (94.4) |
| Black | 221 (2.6) | 198 (2.9) ‡ | 23 (1.4) ‡ | 12 (1.7) |
| Other | 301 (3.5) | 239 (3.5) ‡ | 62 (3.8) ‡ | 28 (3.9) |
| WTC exposure level | ||||
| Morning of 9/11 | 1352 (15.9) | 1034 (15.0) ‡ | 318 (19.5) ‡ | 128 (17.9) |
| Afternoon of 9/11 or 12 September 2001 | 6065 (71.1) | 4908 (71.1) ‡ | 1157 (71.0) ‡ | 524 (73.1) |
| 13-24 September 2001 | 1113 (13.1) | 959 (13.9) ‡ | 154 (9.5) ‡ | 65 (9.1) |
| Baseline * FEV1 (L) | 4.01 ± 0.68 | 4.06 ± 0.66 ‡ | 3.80 ± 0.68 ‡ | 3.97 ± 0.68 |
| Baseline * FEV1 % predicted | 97.3 ± 13.6 | 98.6 ± 13.1 ‡ | 91.8 ± 14.1 ‡ | 95.2 ± 14.2 |
| Baseline * wheeze | 1797 (21.1) | 1210 (17.6) ‡ | 587 (36.0) ‡ | 216 (30.2) |
| Baseline * dyspnea | 2454 (28.9) | 1720 (25.0) ‡ | 734 (45.1) ‡ | 272 (38.0) |
| ICS/LABA Treated > 2y N = 1570 * | ICS/LABA Treated ≤ 2y N = 690 * | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | OR | 95% CI | p Value | OR | 95% CI | p Value | ||
| FEV1 absolute #, per -1 L | 2.36 | 2.10 | 2.67 | <0.001 | 1.52 | 1.31 | 1.77 | <0.001 |
| Respiratory symptoms ±, 1 vs. 0 | 3.68 | 3.06 | 4.42 | <0.001 | 2.57 | 2.07 | 3.20 | <0.001 |
| Respiratory symptoms ±, 2 vs. 0 | 10.04 | 8.37 | 12.05 | <0.001 | 5.47 | 4.38 | 6.83 | <0.001 |
| Respiratory symptoms ±, 3 vs. 0 | 28.80 | 23.19 | 35.76 | <0.001 | 10.06 | 7.60 | 13.32 | <0.001 |
| Probability * on ICS/LABA Treatment | Predicting | HR | 95% CI | p Value | |
|---|---|---|---|---|---|
| 9/11/2005–9/10/2007 | 9/10/2007–9/11/2011 | 3.32 | 2.58 | 4.26 | <0.001 |
| 9/11/2005–9/10/2007 | 9/10/2015–7/1/2018 | 2.13 | 1.37 | 3.32 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Putman, B.; Lahousse, L.; Goldfarb, D.G.; Zeig-Owens, R.; Schwartz, T.; Singh, A.; Vaeth, B.; Hall, C.B.; Lancet, E.A.; Webber, M.P.; et al. Factors Predicting Treatment of World Trade Center-Related Lung Injury: A Longitudinal Cohort Study. Int. J. Environ. Res. Public Health 2020, 17, 9056. https://doi.org/10.3390/ijerph17239056
Putman B, Lahousse L, Goldfarb DG, Zeig-Owens R, Schwartz T, Singh A, Vaeth B, Hall CB, Lancet EA, Webber MP, et al. Factors Predicting Treatment of World Trade Center-Related Lung Injury: A Longitudinal Cohort Study. International Journal of Environmental Research and Public Health. 2020; 17(23):9056. https://doi.org/10.3390/ijerph17239056
Chicago/Turabian StylePutman, Barbara, Lies Lahousse, David G. Goldfarb, Rachel Zeig-Owens, Theresa Schwartz, Ankura Singh, Brandon Vaeth, Charles B. Hall, Elizabeth A. Lancet, Mayris P. Webber, and et al. 2020. "Factors Predicting Treatment of World Trade Center-Related Lung Injury: A Longitudinal Cohort Study" International Journal of Environmental Research and Public Health 17, no. 23: 9056. https://doi.org/10.3390/ijerph17239056
APA StylePutman, B., Lahousse, L., Goldfarb, D. G., Zeig-Owens, R., Schwartz, T., Singh, A., Vaeth, B., Hall, C. B., Lancet, E. A., Webber, M. P., Cohen, H. W., Prezant, D. J., & Weiden, M. D. (2020). Factors Predicting Treatment of World Trade Center-Related Lung Injury: A Longitudinal Cohort Study. International Journal of Environmental Research and Public Health, 17(23), 9056. https://doi.org/10.3390/ijerph17239056





